Abstract
The aim of the study was to evaluate the left ventricular systolic function of newborns with asphyxia using tissue Doppler imaging (TDI). Newborns with a history of asphyxia were divided into severe and mild groups based on their Apgar scores; normal newborns without asphyxia served as the controls. Left ventricular ejection fraction (LVEF), fraction shortening (FS), and stroke volume (SV) were measured by M-mode echocardiography at 24, 48, and 72 h after birth. The peak systolic velocity of the anterior mitral valve leaflet (Sm wave) was measured with TDI. Cardiac troponin I (CTnI) was measured. The results revealed that the LVEF and FS of the severe asphyxia group at 24 h were significantly lower than those at later time points (P < 0.01). These parameters were also significantly lower than those of the mild and control groups (P < 0.01). SV was not significantly different among the three groups. Sm wave of asphyxia groups was significantly lower than that of control group (P < 0.001). In the severe asphyxia group, Sm wave at 24 h was significantly lower than that at 48 or 72 h (P < 0.001). CTnI values of the severe asphyxia group were remarkably higher than those of the other two groups (P < 0.01). The findings of this study indicate decreased left ventricular systolic function of newborn children after asphyxia. Sm by TDI is a more sensitive indicator of left ventricular systolic function than LVEF, FS, or SV by M-mode echocardiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Asphyxia is a serious problem presented during the neonatal period. It was estimated that in 2001 complications such as asphyxia and birth trauma accounted for 29% of neonatal mortality [3]. The death toll reaches about 1 million newborns per year [11]. In China, neonatal asphyxia is one of the main causes of perinatal death, with an incidence ranging from 4.7 to 8.9% [6]. Asphyxia can impact organ systems such as the cardiovascular system, brain, liver, kidney, and gastrointestinal tract. Cardiovascular malfunction occurs often, which in turn can compromise the function of other organs and lead to irreversible sequels. Therefore, it is imperative to accurately and objectively assess the cardiac function in asphyxial newborns. Color Doppler echocardiography has been used to evaluate cardiac function of newborns after asphyxia. Parameters used in clinical practice include left ventricular ejection fraction (LVEF), cardiac output (CO), left ventricular pre-ejection period/left ventricular ejection time (LPEP/LVET), right ventricular pre-ejection period/right ventricular ejection time (RPE/RVET), left ventricular acceleration time/left ventricular ejection time (LVAT/LVET), right ventricular acceleration time/right ventricular ejection time (RVAT/RVET), mitral value early diastolic peak flow velocity (E), mitral value late diastolic peak flow velocity (A), tricuspid value early diastolic peak flow velocity (E), and tricuspid value late diastolic peak flow velocity(A) [5, 15]. While tissue Doppler imaging (TDI) has not been reported as a method of evaluating cardiac function after neonatal asphyxia, this study addresses the use of TDI and M-mode echocardiography in accessing cardiac function of neonates with a history of asphyxia.
Materials and Methods
Patients
Sixty two full-term newborns with histories of asphyxia were selected from the Department of Pediatrics, Jin Hua Hospital, from October 2003 to December 2005. Newborns with a history of asphyxia were divided into severe and mild groups based on their Apgar scores at 1 min. The severe asphyxial group (31 cases; Apgar scores ≤3) included 17 males and 14 females. Of the 31 severe cases, 9 patients presented with tachypnea and respiratory distress; 7 with edema of both lower limbs, ochrodermia, and chills in all extremities; and 11 with ECG changes including occasional premature ventricular contraction in 4 cases and depressed ST-T in 7 cases. Of the 31 mild asphyxia cases (Apgar 4–7), 12 were males and 19 females. Five of the cases presented transient tachypnea and another with transient lower ST-T. Thirty normal full-term newborns (13 male, 17 female) were also recruited from the newborn nursery of the Department of Obstetrics at the same hospital during the study period. There were no significant differences in birth weight, gender, or gestational age among the three groups. Control members displayed no cardiac malformations detectable by ultrasonograph. The study was approved by the hospital’s internal review board, and written informed consent was obtained from the parents of all subjects.
Procedures
Newborns were asleep or lightly sedated by oral administration of chloral hydrate (0.5 ml/kg) for all examinations. Patients were monitored by the NICU staff at the same time. An HP5500 color Doppler echocardiography diagnostic apparatus (Hewlett Packard, Palo Alto, CA, USA) was used, at 5-MHz feeler frequency. Left ventricular systolic functional indexes such as left ventricular ejection fraction (LVEF), fractional shortening (FS), and stroke volume (SV) were detected at 24, 48, and 72 h after birth using M-mode echocardiography based on the left ventricular end-diastolic diameter and the left ventricular end-systolic diameter. TDI mode was then applied to measure the peak systolic velocity of the anterior mitral valve leaflet (Sm) through an apical four-chamber view. The mean value of three measurements was used for calculation. Two-milliliter blood samples were taken before each echocardiography, and CTnI levels were determined by the chemiluminescence method as described [2]. All equipments and reagents were purchased from Beckman Instruments, Inc. (Fullerton, CA, USA).
Statistical Analysis
All data are expressed as mean ± SE. Analysis of variance (ANOVA) was used to compare the data among the three groups or three time intervals. When significance of the above comparison was identified, post hoc testing was used to further determine the difference between two individual groups. SPSS10.0 software was used. P < 0.05 is defined as statistically significant. Correlation between two valuables was calculated using the Pearson product-moment correlation method.
Results
LVEF Is Reduced at 24 h in Newborns with Asphyxia
LVEF measurements were taken from newborns with severe and mild asphyxia as well as the control group at 24, 48, and 72 h after birth. As shown in Fig. 1, at 24 h after birth, the LVEF of newborns with severe asphyxia was 62.00 ± 3.67%, which was significantly lower than that of the same group at 48 and 72 h (65.72 ± 4.76% and 64.8 ± 5.47%, respectively; P < 0.01). The value at this time period was also significantly lower than that of the mild asphyxial (64.04 ± 7.05%) and control (68.01 ± 8.23%; P < 0.01) groups. However, no difference was noted between newborns with mild asphyxia and the control group at 24 h or among the three groups at 48 and 72 h (P > 0.05), indicating a recovery of LVEF after 2 days of management in NICU.
The effect of asphyxia on LVEF. Echocardiography was performed in study subjects at 24, 48, and 72 h after birth as described under Materials and Methods. Data presented as mean ± SE for each group (n = 31 for severe and mild asphyxia groups, n = 30 for control group). * P < 0.01 compared to control group
FS Is Reduced Only in Patients with Severe Asphyxia at an Early Stage
Next, we measured the FS in all patients at the three time intervals after birth (Fig. 2). At 24 h, the FS measurements were 31.58 ± 3.32%, 32.03 ± 4.82%, and 34.87 ± 5.79%, for the severe asphyxial, mild asphyxial, and control groups, respectively. Results demonstrated statistical significance of FS among the three groups at 24 h (P < 0.01). Further calculation revealed a difference between the severe asphyxial and the control group (90% of control). There was no significant difference in FS between patients with mild asphyxia and the control group at 24 h. As in LVEF, by 48 h this difference was no longer present among the three groups, and no difference was noticed at the 72-h time point either (P > 0.05).
FS is reduced only in newborns with severe asphyxia at early time points. FS values for the three groups were determined as described under “Materials and Methods”. Data presented as mean ± SE for each group (n = 31 for severe and mild asphyxial groups, n = 30 for control group). * P < 0.01 compared to control group
No Change in SV in Newborns with Asphyxia
Although there was a trend toward a decrease in SV in newborns with asphyxia at 24 h (6.25 ± 0.24 ml in severe and 6.26 ± 0.23 ml in mild asphyxia), in comparison to the control group (6.77 ± 0.27 ml), no statistic significant difference was detected (P = 0.25). No significant difference was noticed among the three groups at the intervals of 48 and 72 h (P = 0.14 and P = 0.08 respectively), as indicated in Fig. 3, implying that SV may be a less sensitive parameter for assessing cardiac function in newborns with asphyxia.
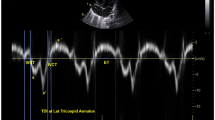
TDI Sm Is Decreased in Patients with Asphyxia
The Sm wave was determined for all groups at different times after birth. The control group showed 6.45 ± 0.14, 6.18 ± 0.14, and 6.46 ± 0.15 cm/s at 24, 48, and 72 h, respectively. As clearly illustrated in Fig. 4, the asphyxial groups had significantly lower Sm values than the control group at 24 h (61 and 75% of control), 48 h (85 and 80% of control), and 72 h (77 and 78% of control), indicating a sustained effect. Also notable is the observation that at 24 h children with severe asphyxia demonstrated a significantly lower Sm than the group with mild asphyxia (3.92 ± 0.07%, and 4.87 ± 0.13%, respectively; P < 0.001). However, this variation was not noticed at the 48- or 72-h time periods (P > 0.05).
Change of Serum CTnI Levels in Patients with Asphyxia
Sera from all subjects at different time points were collected for determination of CTnI levels. As shown in Fig. 5, CTnI was highest in newborns with severe asphyxia at 24 h (0.59 ± 0.08 ng/ml), which is 12- and 30-fold higher than that of newborns with mild asphyxia and the control group, indicating acute cardiac ischemia as result of the asphyxia. This value decreased to 0.15 ± 0.03 and 0.04 ± 0.01 ng/ml, respectively at 48 and 72 h. Nonetheless, these values were still significantly higher than those of newborns with mild asphyxia and the control group (0.023 and 0.015 ng/ml for control group at 48 and 72 h). No significant difference was detected between mild asphyxial and control groups throughout the three time intervals, indicating that CTnI is probably a less sensitive parameter of cardiac malfunction in newborns with a history of asphyxia.
Serum CTnI levels of asphyxial and control patients. Sera were collected at 24, 48, and 72 h after birth. CTnI levels were measured by the chemiluminescence method as summarized under “Materials and Methods”. Data presented as mean ± SE for each group (n = 31 for severe and mild asphyxial groups, n = 30 for control group). * P < 0.001 compared to control group
Correlation of Sm with CTnI and of Sm with FS
The correlation between Sm and CTnl, as well as between Sm and FS, was calculated based on individual values at the 24-h time period among all subjects (Fig. 6). Sm showed a better correlation (negatively) with CTnl, with a correlation coefficient of −0.713, than with FS, with correlation coefficient of 0.302. The data indicate that Sm is a better parameter than FS to reflect ischemic change of the left ventricle after asphyxia.
Correlation of Sm with CTnl and of Sm with FS. The values of Sm vs. CTnl and Sm vs. FS for each subject at 24 h were plotted with Sm on the Y axis, and CTnl and FS on the X axes. Correlation coefficients were calculated using Pearson product-moment correlation method. P = 0.0001 and P = 0.03 for Sm vs. CTnl and Sm vs. FS, respectively
Discussion
Severe hypoxemia and acidosis induced by asphyxia during delivery may lead to multiorgan malfunction. The heart is often affected, which results in reduction of left ventricular systolic function and cardiac output [4, 16]. Mild cases of cardiac involvement are manifested as transient cardiac dysfunction, while severe cases may develop heart failure. Cardiac abnormalities other than asphyxia may present with similar clinic manifestations, resulting in difficulty in pinpointing the diagnosis. It is usually difficult, if not impossible, to make a correct judgment regarding cardiac function based on clinical presentation alone. Echocardiography may provide a more sensitive modality to detect a defect of left ventricular function in newborns with asphyxia [10, 12]. M-mode echocardiography is widely used and can reflect cardiac systolic function more accurately. Our data, similar to what has been published previously, show a significant reduction of LVEF and FS in the group with severe asphyxia at 24 h after birth. However, these parameters are still within normal range ( >50 and >30%, respectively). This may be due to patients’ recovery of cardiac function in the first 24 h after vigorous resuscitation and clinical management thereafter. However, a sustained elevation of CTnI is still present in these patients.
TDI was initially introduced by McDicken and coworkers in 1992 [8]. According to the principle of Doppler, the reflected Doppler signal correlates with the movement of cardiac tissue and the velocity of the bloodstream. Optimal signals are collected using a low-pass filter and adjusting the level of enhancement. A proper threshold is defined, which is followed by autocorrelation, speed calculation, and color-coding. Real-time information regarding the movement of cardiac tissue is then displayed after digital-to-nalog conversion. The Sm wave of mitral annulus is created by movement of the mitral annulus toward the ventricle during left ventricular contraction. Sm gives the estimation of the global systolic function of the left ventricle. TDI has been widely used as a robust and reproducible echocardiographic tool for assessing cardiac function in adults, especially to show segmental changes in cardiac function and to avoid the disadvantages of observer-dependent interpretation [1, 7]. However, to the best of our knowledge, its use to assess cardiac function in neonatal asphyxia has not been reported.
The reduced Sm wave of patients in the current study suggests compromised left ventricular systolic function in newborns with asphyxia, particularly at the earlier time interval (24 h). The Sm wave has the advantage of direct detection of the velocity of cardiac muscle movement, and illustrates the irrelevancy of mechanical systolic movement of cardiac muscle fiber to the heart rate and ventricular pre- and postload. In newborns with asphyxia, infarction of papillary muscles causes anoxic necrosis of cardiac muscles, which in turn leads to functional disorder of the mitral valve, requiring a long recovery time [9]. This may explain why the Sm wave was significantly depressed in asphyxial patients up to 72 h after birth, while LVEF and FS had recovered by that time. Asphyxia had no evident effect on SV; this is probably due to the fact that cardiac muscle injury and decreased left ventricular contractility are mainly mediated by anoxia and acidosis [14]. As resuscitation starts, anoxia and acidosis are corrected, which results in increased heart rate and cardiac output [13]. The end point of this process is the rapid recovery of cardiac blood-pumping function, which is reflected by the normalized LVEF and FS.
Myocardial cells are the only source of CTnI; therefore, its change can specifically reflect cardiac muscular impairment. However, CTnI does not directly correlate with cardiac contractility. CTnI in serum peaks at 24 h before falling gradually to baseline around 7 days after birth [17]. Data presented here show that the CTnI and TDI Sm wave change in parallel in patients with asphyxia.
In summary, our study has demonstrated that left ventricular systolic function decreases in newborns with asphyxia as measured by M-mode echocardiography and TDI. TDI Sm is more sensitive than the parameters of M-mode echocardiography (LVEF, FS, SV) for evaluating left ventricular systolic function. Therefore, TDI may provide earlier diagnostic values in assessing cardiac function of newborns with a history of asphyxia.
References
Alam M, Witt N, Nordlander R et al (2007) Detection of abnormal left ventricular function by Doppler tissue imaging in patients with a first myocardial infarction and showing normal function assessed by conventional echocardiography. Eur J Echocardiogr 8:37–41
Ammann P, Naegeli B, Schuiki E et al (2003) Long-term outcome of acute myocarditis is independent of cardiac enzyme release. Int J Cardiol 89:217–222
Atasay B, Arsan S (2003) Organization of neonatal care services and its importance. J Perinat Med 31:292–294
Bai XL, Han YK, Xu CX (1994) Early evaluation of heart function after neonatal asphyxia. Chin J Pract Pediatr 9:93–95 (In Chinese)
Cao HY, Meng FH, Li JG (2000) Study of multiple organs hemodynamics and cardiac functions of neonates with asphyxia. Chin J Ultrasound Med 16:37–39 (in Chinese)
Cao Y (2004) Resuscitation of neonatal asphyxia. New Med 38:46–48 (in Chinese)
Gorcsan J, Gulati VK, Mandarino WA et al (1996) Color-coded measures of myocardial velocity throughout the cardiac cycle by tissue Doppler imaging to quantify regional left ventricular function. Am Heart J 131:1203–1213
McDicken WN, Sutherland GR, Moran CM et al (1992) Colour Doppler velocity imaging of the myocardium. Ultrasound Med Biol 18:651–654
Gill AB, Weindling AM (1993) Echocardiographic assessment of cardiac function in shocked very low birth weight infants. Arch Dis Child 68:17–21
Ichihashi K, Yada Y, Takahashi N et al (2005) Utility of a Doppler-derived index combining systolic and diastolic performance (Tei index) for detecting hypoxic cardiac damage in newborns. J Perinat Med 33:549–552
Lawn JE, Wilczynska-Ketende K, Cousens SN (2006) Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol 35:706–718
Liu X, Qiu YP, You SR (2000) Echocardiography evaluation of right ventricular function for post-asphyxia newborn infants. China JMIT 16:454–455 (in Chinese)
Moraru L, Cimponeriu L, Tong S et al (2004) Characterization of heart rate variability changes following asphyxia in rats. Methods Inf Med 43:118–121
Ranjit MS (2000) Cardiac abnormalities in birth asphyxia. Indian J Pediatr 67:S26–S29
Waggoner AD, Bierig SM (2001) Tissue Doppler imaging: a useful echocardiographic method for the cardiac sonographer to assess systolic and diastolic ventricular function. J Am Soc Echocardiogr 14:1143–1152
Walther FJ, Siassi B, Ramddam NA (1998) Cardiac output in newborn infant with transient myocardial dysfunction. J Pediatr 107:781–785
Zhu XP, Zhang RX, Huang YP (1999) Clinic value of cTn1 in evaluation of myocardial damage after asphyxial newborn. Chin J Pract Pediatr 14:667–668 (in Chinese)
Acknowledgments
This work was performed at Jin Hua Municipal Central Hospital, Jin Hua City, Zhejiang Province, China. The work was sponsored by health department grants from Zhejiang Province.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, Y., Xu, J., Xu, T. et al. Left Ventricular Systolic Function of Newborns with Asphyxia Evaluated by Tissue Doppler Imaging. Pediatr Cardiol 30, 741–746 (2009). https://doi.org/10.1007/s00246-009-9421-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-009-9421-6