Abstract
Infants with an unbalanced atrioventricular septal defect (AVSD) frequently present with comorbidities that may have an impact on their medical course and outcome. This study aimed to assess outcomes and explore possible prognostic indicators for patients undergoing surgical palliation for an unbalanced AVSD. The medical records of all infants presenting to the authors’ institution with an unbalanced AVSD over a 5-year period were retrospectively reviewed for assessment of outcomes and comorbidities. The study group consisted of 44 patients with an overall survival rate of 51% for the entire follow-up period. The majority of these patients (88%) underwent single-ventricle palliation, with an 83% rate of survival to initial hospital discharge and an overall long-term survival rate of 50%. The midterm outcome was significantly worse than that for a cohort of hypoplastic left heart syndrome patients undergoing single-ventricle palliation during the same period (P = 0.03). In addition, 30% of the patients required either repair or replacement of their systemic atrioventricular valve at initial palliation or during subsequent follow-up evaluation. Of the patients with an unbalanced AVSD, 75% had associated congenital anomalies. In conclusion, infants with an unbalanced AVSD are a high-risk population with diminished midterm survival compared with palliated patients who have more classic forms of hypoplastic heart syndromes. This may be due to the higher incidence of both severe atrioventricular valve regurgitation and important associated congenital anomalies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Complete atrioventricular septal defect (AVSD), also known as common atrioventricular canal or endocardial cushion defect, occurs in 7.3% of all congenital heart disease cases [8]. Among patients with an AVSD, other noncardiac diagnoses are common. According to the data from the Baltimore–Washington Infant Study, 76% of patients with an AVSD had an associated chromosome abnormality, syndrome, or laterality defect [8].
The majority of patients with an AVSD are balanced, with the common atrioventricular (AV) valve equally positioned over both ventricles. In a smaller percentage of patients with an AVSD (~10%), the common AV valve is unequally positioned over the right or left ventricle and described as unbalanced [6]. The degree of ventricular hypoplasia is variable among patients with an unbalanced AVSD, and there may be an associated aortic or pulmonary outflow tract obstruction. In addition, the common AV valve typically has some degree of regurgitation of [4, 10, 17, 18].
The surgical options for patients with an unbalanced AVSD depend on the underlying anatomy and range from two ventricular repairs to a single-ventricle palliation [5]. For patients requiring single-ventricle palliation, the initial procedure may be a Norwood procedure, an isolated aortopulmonary shunt, or pulmonary arterial banding. Due to the high incidence of associated risk factors, we hypothesized that neonates with an unbalanced AVSD undergoing single-ventricle palliation may have worse outcomes than patients with more classic hypoplastic left heart lesions undergoing similar surgical procedures.
Materials and Methods
A retrospective chart review was performed for all infants presenting with an unbalanced AVSD at our institution from June 1998 to June 2003. An unbalanced defect was defined as one with more than 60% of the atrioventricular valve area committed to one ventricle, as determined by echocardiography and confirmed by two independent echocardiographers. Information was gathered regarding specific cardiac anatomic and functional details, associated noncardiac diagnoses, surgical interventions performed, and both short- and long-term outcomes. Follow-up data were obtained until December 2005.
A cohort of patients with classic hypoplastic left heart syndrome (HLHS) consisting of mitral and aortic hypoplasia or atresia who underwent surgical palliation at our institution during a similar period and had similar follow-up time was used for comparison analysis [19]. Both cohorts had similar general characteristics such as gestational age (AVSD 38.3 vs HLHS 39 weeks), weight (AVSD 3.1 vs HLHS 3.3 kg), fetal diagnosis (AVSD 69% vs HLHS 55%), and follow-up time (AVSD 25 months; range, 0.1–88 months vs HLHS 23 months; range, 0.1–53 months).
A two-tailed Fisher’s exact test was used to examine for differences in frequency data between the two groups. Logistic regression analysis was used to identify predictors associated with mortality. Statistical significance was defined as a P value less than 0.05.
Results
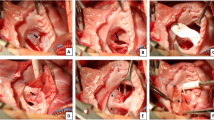
Unbalanced AVSD was diagnosed for 44 patients at our institution during the specified time frame. Figure 1 displays the overall outcomes for the study group. Two in utero deaths occurred (one terminated), and two patients died before surgical intervention after decisions were made to withdraw support secondary to multiple congenital anomalies.
Figure 2 shows the breakdown of the initial surgical procedures performed. The majority of patients who underwent surgery had single-ventricle palliation (35/40). Three patients had biventricular repairs, all of whom survived. One patient had a one and a half ventricular repair (comprising an initial pulmonary arterial band and coarctation repair at 1 week of life and subsequent right bidirectional Glenn) and died of complications after the second surgery. One patient underwent repair of obstructed total anomalous pulmonary venous return on day 1 of life and died shortly thereafter.
In addition, most patients were unbalanced to the right side, resulting in a hypoplastic left ventricle (39/44). Of the 39 patients in this group, 16 had left ventricular outflow tract obstruction, and 13 had associated aortic coarctation. Two of the five patients unbalanced to the left with a hypoplastic right ventricle had right ventricular outflow tract obstruction, and three had coarctation.
Table 1 lists the rates of survival to hospital discharge for different subcategories of the patient population. The rate of survival to initial hospital discharge was 83% among the 40 patients who underwent surgery. There were no significant differences in survival to hospital discharge based on type of surgery performed. In addition, no significant difference in survival to hospital discharge was found between unbalanced AVSD patients undergoing single-ventricle palliation with the Norwood procedure (83% survival) or a systemic to pulmonary artery shunt alone (92% survival) and the HLHS cohort (74% survival) (Table 1). Among the surgically treated patients, survival to hospital discharge was not significantly affected by fetal diagnosis, chromosomal anomalies, or heterotaxy association.
Table 2 delineates the midterm survival rates for the different subcategories of patients. The overall survival rate for the entire postnatal cohort was 51% (20/39, with 3 patients lost to follow-up evaluation) during a median follow-up period of 25 months (range, 0.1–88 months). Patients undergoing single-ventricle palliation had a midterm survival rate of 50%. Within this group, those who underwent a Norwood procedure had a 40% midterm survival rate, compared with 64% for those who underwent an aortopulmonary shunt. The comparison HLHS cohort had an overall midterm survival rate of 74% during a median follow-up period of 23 months (range, 0.1–53 months). Compared with the HLHS cohort, a significantly worse survival rate was found not only among the AVSD patients undergoing the Norwood procedure but also among all unbalanced AVSD patients undergoing single-ventricle palliation (50% vs 74%; P = 0.03). Patients undergoing aortopulmonary shunt alone showed no difference in survival compared with the HLHS group (64% vs 74%, respectively; P = 0.5). Of the 16 patients who survived with single-ventricle palliation, 13 underwent successful Fontan completion, 2 were considered poor Fontan candidates and remained at the hemi-Fontan stage, and 1 never advanced beyond repeated aortopulmonary shunts.
More than two-thirds of the patients (69%) had a prenatal diagnosis. However, when the midterm survival rate for the patients with the prenatal diagnosis (17/29) was compared with that for the patients with the postnatal diagnosis (3/11) who underwent surgery, no significant difference was found (P = 0.16), although the number of patients with the postnatal diagnosis was quite small.
Extracardiac anomalies were present in 73% (32/44) of the patients. Table 3 lists the various anomalies found. Heterotaxy syndrome was present in 41% (18/44) of the patients. Right isomerization occurred in 11 patients and left isomerization in 4 patients (3 had undetermined sidedness). The patients with heterotaxy association had an overall survival rate of 56%. The overall survival rate for the patients with extracardiac anomalies was 45%, similar to that for patients without extracardiac anomalies (P = 0.5).
Of the patients who underwent initial operations, 12 (30%) subsequently underwent AV valve repair or replacement. As shown in Table 4, the overall survival rate for the patients requiring valve surgery was 25% compared with 64% for the patients not requiring AV valve repair or replacement (P = 0.03). Four patients underwent multiple attempts at repair or replacement of the AV valve. Three patients required repair of total anomalous pulmonary venous return. Two of these patients ultimately died, whereas the third patient was lost to follow-up evaluation.
Multivariable logistic regression analysis identified only the need for AV valve intervention as a predictor of mortality, with an odds ratio of 5.3 (95% confidence interval [CI], 1.14–24.90). There were no interactions or predictive odds ratios with other variables such as fetal diagnosis, heterotaxy association, or other congenital anomalies (Table 4).
Discussion
The reports on outcomes for patients with unbalanced AVSDs undergoing biventricular repair are few and even fewer for those undergoing single-ventricle palliation. Drinkwater and Laks [7] reported on 45 unbalanced AVSD patients, most of whom underwent pulmonary arterial banding as an initial procedure. Of these patients, 34 subsequently received modified Glenn shunts, with a hospital survival rate of 91%. Five patients reportedly underwent Fontan palliation, but the overall survival rate for this cohort was not reported. Other smaller studies have reported mortality rates ranging from 50% to 100% [3, 6, 15].
Our results further demonstrate that patients with an unbalanced AVSD, specifically those undergoing single-ventricle palliation, are a high-risk population with comparable short-term but diminished midterm survival rates in relation to patients with more classic hypoplastic left heart lesions undergoing similar surgical procedures at our institution and others [9, 13, 19, 20]. The outcomes for unbalanced AVSD patients undergoing an aortopulmonary shunt alone (our institution prefers aortopulmonary shunts to pulmonary arterial banding to generate restrictive pulmonary blood flow) were comparable with those for the HLHS Norwood cohort, suggesting that these patients may have a better outcome than unbalanced AVSD patients requiring a Norwood procedure. This could serve as important data for counseling families with such infants. Furthermore, although not statistically significant, extracardiac anomalies such as chromosomal derangements and heterotaxy syndrome likely contribute to the poor outcome for these patients. Given that 73% of our patients had extracardiac anomalies (compared with 11% of the HLHS cohort [19]), it is possible that with continued addition to the cohort, this characteristic may prove to be an important determinant of outcome. It also is possible that anomalies in patients who did not survive were not discovered, hence confounding the data.
Significant AV valve regurgitation occurs frequently among patients with an unbalanced AVSD [10, 18], and our data showed a 30% incidence of AV valve regurgitation requiring intervention. The need for AV valve repair or replacement resulted in a statistically significant increase in mortality among our patients, indicating that this characteristic is a significant risk factor for survival. Findings also show atrioventricular valve regurgitation to be a risk factor for HLHS patients undergoing single-ventricle palliation [1, 14, 16]. The need for repair of anomalous pulmonary venous drainage, found more frequently among patients with an unbalanced AVSD, is almost certainly a major risk factor, although our study cohort was too small to show statistically significant differences in outcomes.
Our cohort did show a high rate of single-ventricle palliation compared with two-ventricle repair. This likely represents a significant referral bias because many patients were transferred specifically for such palliation, and many had severely hypoplastic left-sided structures. Because a two-ventricle repair is preferable when feasible, new surgical techniques and diagnostic criteria to determine suitability for two-ventricle repair for patients with borderline anatomy are important endeavors currently underway [4, 5, 11].
Prenatal diagnosis of an unbalanced AVSD was determined for 69% of the patients in our cohort. However, no statistically significant difference in outcome was found between prenatally and postnatally diagnosed patients. Varied findings of benefit from a prenatal diagnosis have been reported for transposition of the great arteries [2], hypoplastic left heart syndrome [21], pulmonary atresia [22], and other disorders [12]. In our cohort of patients with an unbalanced AVSD, although survival was perhaps similar between those diagnosed pre- and postnatally, other perinatal and postnatal morbidities may have occurred without in utero diagnoses that could have been avoided with prenatal knowledge of this lesion. Furthermore, the psychological benefit of prenatal counseling for families about probable outcomes and arrangements for labor and delivery are undoubtedly valuable.
In summary, patients with an unbalanced AVSD are a unique group with a wide variety of associated cardiac and noncardiac lesions. Due to relatively poor midterm survival rates for single-ventricle palliation, families should be counseled appropriately, with particular emphasis on the difference in survival rates between the more classic hypoplastic heart lesions and the negative effects of any known associated anomalies such as AV valve regurgitation.
References
Barber G, Helton JG, Aglira BA, Chin AJ, Murphy JD, Pigott JD, Norwood WI (1988) The significance of tricuspid regurgitation in hypoplastic left-heart syndrome. Am Heart J 116(6 Pt 1):1563–1567
Bartlett JM, Wypij D, Bellinger DC, Rappaport LA, Heffner LJ, Jonas RA, Newburger JW (2004) Effect of prenatal diagnosis on outcomes in D-transposition of the great arteries. Pediatrics 113(4):e335–e340
Bharati S, Lev M (1973) The spectrum of common atrioventricular orifice (canal). Am Heart J 86:553–561
Cohen MS, Jacobs ML, Weinberg PM, Rychik J (1996) Morphometric analysis of unbalanced common atrioventricular canal using two-dimensional echocardiography. J Am Coll Cardiol 28(4):1017–1023
Cohen MS, Spray TL (2005) Surgical management of unbalanced atrioventricular canal defect. Semin Thorac Cardiovasc Surg Pediatr Card Surg Ann 8:135–144
Corno A, Marino B, Catena G, Marcelletti C (1988) Atrioventricular septal defects with severe left ventricular hypoplasia. J Thorac Cardiovasc Surg 96:249–252
Drinkwater D, Laks H (1997) Unbalanced atrioventricular septal defects. Semin Thorac Cardiovasc Surg 9(1):21–25
Ferencz C, Loffredo CA, Correa-Villasenor A, Wilson PD (1997) Genetic and environmental risk factors of major cardiovascular malformations: the Baltimore-Washington infant study 1981–1989. Futura Publishing Co, Armonk, NY, pp 103–122
Gaynor JW, Mahle WT, Cohen MI, Ittenbach RF, DeCampli WM, Steven JM, Nicolson SC, Spray TL (2002) Risk factors for mortality after the Norwood procedure. Eur J Cardiothorac Surg 22(1):82–89
Geva T, Ayres NA, Pignatelli RH, Gajarski RJ (1996) Echocardiographic evaluation of common atrioventricular canal defects: a study of 206 consecutive patients. Echocardiography 13(4):387–400
Kim WH, Lee TY, Kim SC (2000) Unbalanced atrioventricular septal defect with parachute valve. Ann Thorac Surg 70(5):1711–1712
Kovalchin JP, Silverman NH (2004) The impact of fetal echocardiography. Pediatr Cardiol 25(3):299–306
Lloyd TR (1996) Prognosis of the hypoplastic left heart syndrome. Prog Pediatr Cardiol 5:57–64
Mahle WT, Cohen MS, Spray TL, Rychik J (2001) Atrioventricular valve regurgitation in patients with single ventricle: impact of the bidirectional cavopulmonary anastomosis. Ann Thorac Surg 72(3):831–835
Mehta S, Hirschfeld S, Riggs T, Liebman J (1979) Echocardiographic estimation of ventricular hypoplasia in complete atrioventricular canal. Circulation 59:888–893
Ohye RG, Gomez CA, Goldberg CS, Graves HL, Devaney EJ, Bove EL (2006) Repair of the tricuspid valve in hypoplastic left heart syndrome. Cardiol Young 16(Suppl 3):21–26
Pierpomt ME, Markwald RR, Lin AE (2000) Genetic aspects of atrioventricular septal defects. Am J Med Genet Winter 97(4):289–296
Silverman NH, Zuberbuhler JR, Anderson RH (1986) Atrioventricular septal defects: cross-sectional echocardiographic and morphologic comparisons. Int J Cardiol 13(3):309–331
Stasik CN, Gelehrter S, Goldberg CS, Bove EL, Devaney EJ, Ohye RG (2006) Current outcomes and risk factors for the Norwood procedure. J Thorac Cardiovasc Surg 131(2):412–417
Tweddell JS, Hoffman GM, Mussatto KA, Fedderly RT, Berger S, Jaquiss RD, Ghanayem NS, Frisbee SJ, Litwin SB (2002) Improved survival of patients undergoing palliation of hypoplastic left heart syndrome: lessons learned from 115 consecutive patients. Circulation 106(12 Suppl 1):I82–I89
Tworetzky W, McElhinney DH, Reddy VM, Brook MM, Hanley FL, Silverman NH (2001) Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation 103(9):1269–1273
Tzifa A, Barker C, Tibby SM, Simpson JM (2007) Prenatal diagnosis of pulmonary atresia: impact on clinical presentation and early outcome. Arch Dis Child Fetal Neonatal Ed 92(3):F199–F203
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Owens, G.E., Gomez-Fifer, C., Gelehrter, S. et al. Outcomes for Patients with Unbalanced Atrioventricular Septal Defects. Pediatr Cardiol 30, 431–435 (2009). https://doi.org/10.1007/s00246-008-9376-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9376-z