Abstract
Infants with tetralogy of Fallot (ToF) presenting with desaturation may require augmentation of the pulmonary blood flow, usually in the form of a Blalock–Taussig shunt. Shunts may result in a preferential increase in blood flow to one lung. They also may be associated with significant morbidity and possibly mortality of premature infants. Balloon dilation of the pulmonary valve is reported to improve saturation in early infancy. This report describes two premature infants (weighing, respectively, 1.8 and 1.6 kg) with ToF and desaturation for whom balloon dilation of the pulmonary valve showed good results. Neither infant required palliative surgery. At this writing, one infant has already undergone complete repair.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
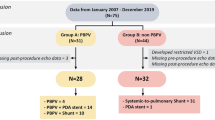
Children with tetralogy of Fallot (ToF) presenting with significant desaturation during early infancy require a Blalock–Taussig (BT) shunt as a palliative measure. Shunt surgery may be associated with significant morbidity, and neonatal shunts may be associated with a higher mortality rate [3]. Balloon dilation of the pulmonary valve as an alternative to a shunt is reported to improve and palliate a significant number of patients with ToF and desaturation [13]. We report two premature infants with ToF accompanied by significant desaturation who were palliated successfully by balloon pulmonary valvuloplasty.
Case 1
Infant S, a 25-day-old preterm infant born at 29 weeks gestation and weighing 1.4 kg at birth was referred to us for management of ToF, prematurity, and severe desaturation. The infant weighed 1.8 kg at the time of admission. The oxygen saturation was 55% to 60% in room air.
An echocardiographic study showed ToF with predominantly valvular pulmonary stenosis (valve annulus of 4 mm) and confluent right and left branch pulmonary arteries measuring 3 and 3.3 mm, respectively. Augmentation of the pulmonary blood flow by balloon pulmonary valvuloplasty was planned (Fig. 1a).
(a) Parasternal short-axis view of case 1 showing the right ventricular outflow tract (RVOT) and pulmonary annulus measurement. The obstruction is mainly at the valvular level. (b) Subcostal view of case 2 showing color flow mapping of the RVOT and branch pulmonary arteries. Note the turbulence starting at the level of the valve. AO, aorta; RV, right ventricle; VSD, ventricular septal defect
Procedure
The child was electively intubated. Right femoral venous access was obtained using a 4-Fr sheath. A right ventricular angiogram showed a hypertrophied right ventricle with severe pulmonary valvular stenosis (Fig. 2a). The pulmonary annulus measured 4.2 mm. The pulmonary valve was crossed with a 0.014-in. coronary wire.
After a stable position had been obtained, a 4 × 20-mm balloon was tracked over the wire across the pulmonary valve and inflated twice to 8 atmospheres.
Results
A repeat angiogram showed an improved antegrade flow (Fig. 2b). The child was gradually weaned from the ventilator. At the time of discharge, the saturations were 95%.
Follow-up Evaluation
The patient was subsequently followed up at the referring center and reevaluated a year later. An echocardiogram at the age of 13 months showed a pulmonary annulus of 9 mm (z-score, –1) and confluent right and left branch pulmonary arteries measuring 4.6 and 4.5 mm, respectively (z-score, −3). The patient underwent complete repair including ventricular septal defect closure, infundibular resection, and a small transannular patch.
Case 2
Baby E was born by cesarean section (indication, twin delivery at 32 weeks gestation) and weighed 1.6 kg at both birth and presentation to our center at the age of 28 days. At evaluation, the infant was found to have ToF with an oxygen saturation of 60%. Echocardiogram showed the right ventricular outflow tract (RVOT) obstruction to be predominantly at the pulmonary valvular level (Fig. 1b). The pulmonary valve annulus measured 2.6 mm, and the branch pulmonary artery measured 3 to 3.5 mm.
After informed consent was obtained, balloon pulmonary valvuloplasty was undertaken. The child also was noted to have apneic episodes. As part of the workup for apnea, blood cultures were performed.
Procedure
The procedure was planned within 24 h of hospital admission because of the low saturations. The newborn was electively intubated before the procedure. Injection esmolol and phenylepherine were prepared before the procedure and kept ready for use in case of desaturation unresponsive to volume and sodium bicarbonate. In-house surgical backup was available in case an emergency BT shunt needed to be placed.
Right femoral venous access was obtained, and a 3-Fr sheath was inserted. An angiogram was performed over the wire using a cut 3-Fr pigtail in the RVOT. The pulmonary annulus measured 2.6 mm. The pulmonary valve was crossed using a 0.014-in. coronary wire positioned in the right pulmonary artery for stabilization. A coronary balloon measuring 2.5 × 15 mm was taken over the wire across the pulmonary valve. After confirmation of its position on fluoroscopy, the balloon was inflated to a pressure of 9 atmospheres twice. Subsequently, a 3 × 18-mm balloon was inflated to 14 atmospheres.
Results
Immediately after the procedure, the pulse oximetry dipped to 50% to 55%. The child was given a 5-ml/kg normal saline bolus directly into the right ventricle and injection sodium bicarbonate intravenously. After these measures, the saturation gradually improved to 80%.
The child was shifted to the neonatal intensive care unit, where the saturations persisted at low levels (60%) for a few hours. Hemoglobin was optimized. Other possibilities considered included reperfusion lung injury and infundibular reaction. A chest X-ray ruled out the first possibility. A postprocedure echocardiogram showed an open RVOT (Fig. 3).
The saturations improved to 90% several hours after the procedure. The child was weaned from the ventilator. Preprocedure apnea workup showed a positive fungal blood culture, which was treated with antifungals for 4 weeks, especially in view of the cardiac intervention. At the time of the child’s discharge from the hospital, the saturations were between 85% and 90% with room air.
An echocardiogram done at discharge showed a RVOT with a gradient of 40 mmHg mainly at the infundibular level. The follow-up assessment 6 months after the procedure showed the child’s saturations to be 82%. At this writing, reparative surgery is planned in the near future.
Discussion
Patients with ToF presenting in early infancy with low saturations require augmentation of their pulmonary blood flow, which usually is performed using a BT shunt. A central increase in the pulmonary blood flow, as happens with balloon dilation of the pulmonary valve, has been shown to obviate the need for a BT shunt and to allow acceptable saturations until final reparative surgery can be performed [7, 10, 16].
Several issues are related to palliative surgical procedures for premature infants. The infants may outgrow the shunt and require a repeat procedure. If a larger shunt is implanted in anticipation of growth, the child may be symptomatic due to heart failure. In addition, a surgical mortality rate of 10–18% has been reported for low-birth-weight and premature neonates (weight, <2,500 grams) with congenital heart disease undergoing cardiac surgery [1, 12, 14, 15]. Balloon dilation in selected cases with dominant valvular stenosis may provide advantages over BT shunt including a shorter recovery period, a shorter in-hospital stay, and a more evenly distributed bilateral flow to the pulmonary arteries.
After balloon dilation, several parameters have been studied including the pulmonary annulus z-score, the pulmonary artery z-score, the requirement for shunt surgery, and the need for a transannular patch at the time of total correction. A review of the available literature shows an improvement in the pulmonary artery z-score, the branch pulmonary artery size, and saturation [4–6, 9]. Complications are reported mainly for older children in whom the infundibular component is greater or for newborns in whom crossing the valve was difficult [4–6, 9].
Challenges related to interventions for premature infants are similar to those for newborns and include issues related to maintaining temperature and glucose homeostasis. Other reports of interventions for premature and low-birth-weight infants have resulted in reports of a high success and a low complication rate, with palliative surgery postponed or not needed [2, 8, 11].
The importance of preprocedural preparedness, namely, maintaining the 3-Fr sheath and catheter in stock, having drugs such as esmolol and phenylepherine available, and providing for surgical backup, are highlighted in these cases. We had to use a pigtail catheter (with the tip cut off) for the angiogram because it was the only 3-Fr catheter available.
The issues related to postprocedure desaturation, starting an hour after the procedure (case 2), highlight the potential problems. Possible etiologies we had to consider included transient infundibular reaction, reperfusion injury to the lung, decreased hemoglobin resulting in decreased oxygen-carrying capacity, pulmonary issues such as atelectasis, and preexisting systemic infection. Comorbidities including apnea and preprocedure fungemia in case 2 highlight the noncardiac problems that may alter the postprocedure course.
In conclusion, balloon dilation of the pulmonary valve to palliate low-birth-weight desaturated infants with ToF appears to be a safe alternative to a BT shunt. Confirming the etiology of obstruction (valvular) ensures a better outcome. Postprocedure desaturation for a few hours may be anticipated. Findings have shown the procedure to be safe for a small number of patients. Comorbidities related to prematurity may affect the outcome, and the long-term result is encouraging.
References
Bove T, Francois K, De Groote K, Suys B, De Wolf D, Verhaaren H, Matthys D, Moerman A, Poelaert J, Vanhaesebroeck P, Van Nooten G (2004) Outcome analysis of major cardiac operations in low weight neonates. Ann Thorac Surg 78:181–187
Chen MR, Hwang HK, Yu CH, Lin YC (2005) Cardiac catheterization in low-birth-weight infants. J Formos Med Assoc 104:408–411
Fenton KN, Siewers RD, Rebovich B, Pigula FA (2003) Interim mortality in infants with systemic-to-pulmonary artery shunts. Ann Thorac Surg 76:152–156
Godart F, Rey C, Muilwijk C, Francart C, Breviere GM, Vaksmann G (1996) Percutaneous pulmonary valvuloplasty in neonates and infants with tetralogy of Fallot. Arch Mal Coeur Vaiss 89:533–539
Godart F, Rey C, Prat A, Muilwijk C, Francart C, Vaksmann G, Breviere GM (1998) Early and late results and the effects on pulmonary arteries of balloon dilatation of the right ventricular outflow tract in tetralogy of Fallot. Eur Heart J 19:595–600
Guerin P, Jimenez M, Dos Santos P, Srour S, Choussat A (1996) Percutaneous dilatation of the pulmonary tract in tetralogy of Fallot. Arch Mal Coeur Vaiss 89:541–545
Kohli V (2005) Balloon dilatation of pulmonary valve in tetralogy of Fallot’s. Indian J Pediatr 72:181
Kretschmar O, Dahnert I, Berger F, Ewert P, Lange PE (2000) Interventional treatment of congenital heart defects in infants with a body weight up to 2,500 grams. Z Kardiol 89:1126–1132
Massoud I, Imam A, Mabrouk A, Boutros N, Kassem A, Daouod A, El Hakem MA (1999) Palliative balloon valvoplasty of the pulmonary valve in tetralogy of Fallot. Cardiol Young 9:24–36
Matsuoka S, Ushiroguchi Y, Kubo M, Tatara K, Kitagawa T, Katoh I, Kuroda Y (1993) Balloon pulmonary valvuloplasty for infants with severe tetralogy of Fallot. Jpn Heart J 34:643–651
Michel-Behnke I, Thul J, Schranz D (1999) Balloon dilatation of the pulmonary valve in a 690-gm neonate with tetralogy of Fallot. J Perinatol 19:305–306
Oppido G, Napoleone CP, Formigari R, Gabbieri D, Pacini D, Frascaroli G, Gargiulo G (2004) Outcome of cardiac surgery in low-birth-weight and premature infants. Eur J Cardiothorac Surg 26:44–53
Rao PS, Brais M (1988) Balloon pulmonary valvuloplasty for congenital cyanotic heart defects. Am Heart J 115:1105–1110
Reddy VM, McElhinney DB, Sagrado T, Parry AJ, Teitel DF, Hanley FL (1999) Results of 102 cases of complete repair of congenital heart defects in patients weighing 700 to 2,500 grams. J Thorac Cardiovasc Surg 117:324–331
Rossi AF, Seiden HS, Sadeghi AM, Nguyen KH, Quintana CS, Gross RP, Griepp RB (1998) The outcome of cardiac operations in infants weighing two kilograms or less. J Thorac Cardiovasc Surg 116:28–35
Sreeram N, Saleem M, Jackson M, Peart I, McKay R, Arnold R, Walsh K (1991) Results of balloon pulmonary valvuloplasty as a palliative procedure in tetralogy of Fallot. J Am Coll Cardiol 18:159–165
Acknowledgment
We acknowledge the editorial services of Ms. Nimrat D. Khandpur.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00246-009-9550-y
Rights and permissions
About this article
Cite this article
Kohli, V., Azad, S., Sachdev, M.S. et al. Balloon Dilation of the Pulmonary Valve in Premature Infants with Tetralogy of Fallot. Pediatr Cardiol 29, 946–949 (2008). https://doi.org/10.1007/s00246-008-9247-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9247-7