Abstract
The aim was to compare the right ventricular (RV) Tei index obtained by the tissue Doppler imaging (TDI) method with that obtained by the pulsed Doppler method in 29 fetuses aged 24–39 weeks (29.9 ± 4.0 weeks). From pulsed Doppler recordings, the tricuspid closing-to-opening time (a) and RV ejection time (b) were measured. The Tei index determined by the pulsed Doppler method was calculated as (a – b)/b. From TDI recordings, the time interval during diastole (a′) and the duration of the systole S-wave (b′) were measured. The modified Tei index obtained by TDI was calculated as (a′ – b′)/b′. The time a′ correlated strongly with a (r = 0.90, p < 0.0001). The mean difference between a′ and a was 0.3 ± 5.0 ms. There was also a strong correlation between b′ and b (r = 0.94, p < 0.0001). The mean difference between b′ and b was 0.5 ± 3.3 ms. The TDI-Tei index correlated with the pulsed Doppler-Tei index (r = 0.83, p < 0.0001). The mean difference between the TDI-Tei index and the pulsed Doppler-Tei index was −0.003 ± 0.04. This study demonstrated that the TDI-Tei index correlates well with the Tei index determined by pulsed Doppler in fetuses, suggesting that the TDI-Tei index is a feasible approach to assess global RV function in fetuses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Tei index measured by the pulsed Doppler imaging method as a promising way to evaluate the cardiac function in healthy and diseased adults [19], children [11, 21], and even fetuses [6, 10, 18, 20]. More recently, the tissue Doppler imaging (TDI) technique enables us to measure simultaneously both the contraction and relaxation velocities of the myocardium [15], so the Tei index determined by TDI is a useful tool for evaluating cardiac function [4, 9, 14]. Compared to the traditional Tei index determined by the pulsed Doppler imaging method, Tekton et al. [16, 17] and Harada et al. [8] reported that the Tei index obtained the TDI method correlates well with the former in adults and children. To date, it remains unclear whether there is a correlation between Tei indexes obtained by these two methods in fetuses with special hemodynamic characters. The evaluation of right ventricular (RV) function is of major importance in the clinical management of fetuses with heart failure [1, 13]. This study demonstrates that the RV Tei index obtained by the TDI method is well correlated with that obtained by the pulsed Doppler method in fetuses, providing further evidence for evaluation of RV function by the TDI index in the fetus.
Methods
Subjects
The study group consisted of 29 fetuses aged 24–39 weeks (29.9 ± 4.0 weeks). Gestational age was calculated using biparietal diameter, head circumference, abdominal circumference, and/or femur length. All fetuses had normal morphological heart findings and were in normal sinus rhythm. The parents of the patients received an explanation of the study and gave informed consent.
Echocardiography
A complete two–dimensional and pulsed Doppler echocardiographic examination was performed using an Aloka SSD 6500 ultrasonoscope with a multifrequency 3.75–6.0-MHz transducer (Aloka Inc., Tokyo, Japan). The tricuspid inflow velocity pattern was recorded from the four-chamber view, with the pulsed wave Doppler sample volume positioned at the tips of the tricuspid leaflets. The width and length of the sample volume were 1 mm. Care was taken to direct the transducer beam as close as possible to the Doppler beam. There was no angle correction made.
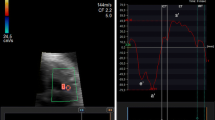
The TDI program was set to pulsed wave Doppler mode. Filters were set to exclude high-frequency signals. Gains were minimized to allow a clear tissue signal with minimal background noise. The TDI of the diastolic velocities was obtained from the four-chamber view of each subject as we reported previously [9]. A 1-mm sample volume was placed at the lateral corner of the tricuspid annulus. The resulting velocities were recorded at a sweep speed of 100 mm/s and stored on VHS videotapes for later playback and analysis.
Time interval measurements were performed using the internal analysis package of the ultrasound unit. The time intervals were determined by two carefully placed vertical cursors that were moved with a track ball. On pulsed Doppler recordings (Fig. 1A), the tricuspid closing-to-opening time (a) was measured as the interval from the end to the onset of the tricuspid inflow velocity pattern. The RV ejection time (b) was measured from the onset to the end of the RV outflow velocity pattern (Fig. 1B). The Tei index determined by the pulsed Doppler method was calculated as (a – b)/b for each patient. The time interval from the end to the onset of the tricuspid annular velocity pattern during diastole (a′) was measured on the TDI recordings (Fig. 2). The duration of the S-wave (b′) was measured from the onset to the end of the S-wave. The modified Tei index obtained by the TDI was calculated as (a′ – b′)/b′. To account for variations in heart rate, mean values were obtained by averaging at least 10 consecutive beats.
Statistics
All data are expressed as mean value ± standard deviation (SD). Linear regression analysis was used to compare pulsed Doppler with the TDI methods for measurement of systolic and diastolic time intervals. Differences between of the measurements taken by conventional Doppler echocardiography and those by TDI methods were analyzed according to the statistical methods of Bland and Altman [2]. A p-value of <0.05 was considered significant. To evaluate the effects of observational variability on the measurement of the duration of the S-wave, the time interval between the end and onset of tricuspid annular diastolic velocities, and the modified Tei index, two independent observers analyzed 10 randomly selected TDI recordings. Interobserver variability was calculated as the standard deviation of the differences between the two observers, expressed as a percentage of the average value. Reproducibility was assessed in 10 fetuses that each underwent TDI measurements twice.
Results
The time interval between the end and onset of tricuspid annular velocities (a′) correlated strongly with the tricuspid closing-to-opening time (a) (r = 0.90, p < 0.0001) (Fig. 3, left). The mean difference between a′ and a was 0.3 ± 5.0 ms (Fig. 3, right). There was a significant correlation between the duration of the S-wave (b′) and the RV ejection time (b) (r = 0.94, p < 0.0001) (Fig. 4, left). The mean difference between b′ and b was 0.5 ± 3.3 ms (Fig. 4, right). The TDI-Tei index correlated with the pulsed Doppler-Tei index (r = 0.83, p < 0.0001) (Fig. 5, left). The mean difference between the TDI-Tei index and the pulsed Doppler-Tei index was −0.003 ± 0.04 (Fig. 5, right). There was good agreement between the two independent observers′ measurements for the duration of the S-wave, the time interval between the end and onset of tricuspid annular diastolic velocities, and the TDI-Tei index (r = 0.95, r = 0.96, and r = 0.93, respectively). Interobserver variability for the time interval between the end and onset of tricuspid annular diastolic velocities, the duration of the S-wave, and the TDI-Tei index was 6 ± 4%, 5 ± 3%, and 3 ± 3%, respectively. Reproducibility for the time interval between the end and onset of tricuspid annular diastolic velocities, the duration of the S-wave, and the TDI-Tei index were 7 ± 4%, 6 ± 3%, and 6 ± 4%, respectively.
Relationships (left) between the time interval from end to onset of tricuspid annular diastolic velocities (a′) and tricuspid closing-to-opening time (a). Bland and Altman plot of the difference (right) between time interval from end to onset of tricuspid annular diastolic velocities and tricuspid closing-to-opening interval. The solid and dashed lines represent the mean ±2 SD of the difference, respectively
Discussion
The Tei index has been reported to be independent of heart rate, RV geometry, and blood pressure [3, 7, 12] to evaluate cardiac function. In contrast to the pulsed Doppler method, the Tei index determined by the TDI method appears to be easier than the Doppler method for evaluation of RV function based on previous reports in adults, children [10, 16, 17], and fetuses [1, 13, 20], because the diastole time interval (a′) and the duration of the S-wave (b′) can be measured simultaneously during the same cardiac circle (Fig. 2), which can reduce inaccuracy due to fluctuation of heart rate that result from fetal movements, breathing, or during transient chord compression [13]. The correlation of the Tei index and cardiovascular score in the fetus [5] further demonstrated that the Tei index is useful for assessing cardiac function in the fetus; however, there is still a poor understanding of the TDI Tei index in the fetus because of an absence of comparison data to validate it. This study attempted to strengthen the evidence that the Tei index by TDI is an ideal parameter for evaluating RV function in the fetus.
Our study indicates the TDI Tei index in the fetus ranges from 0.4 to 0.7, compared to a TDI Tei index of 0.55 ± 0.05 in Aoki`s reports; our data must be carefully interpreted, as it is possible that mothers with diabetes, hypertension, Rhesus incompatility, and multiple gestations were included in our study. The TDI Tei index cutoff value for the fetal RV has not yet been established, but a consensus is expected with further data accumulation. A hypothesis was made that these younger gestational ages leads to a larger TDI Tei index, but these data have not been shown here.
In the present study, the time interval from the end to the onset of the tricuspid annular diastolic velocity correlated strongly with the tricuspid closing-to-opening time. Furthermore, there was an excellent correlation between the duration of S wave and RV ejection time. This indicates a close relation between the modified Tei index obtained by TDI and the Tei index determined by the pulsed Doppler method also exist in fetus. Our result is consistent with previous studies in adults and children.
This study demonstrated that the TDI-Tei index also correlates well with the Tei index determined by pulsed Doppler in the fetus, providing further evidence that the TDI-Tei index is a simple method of assessing RV myocardial performance even in the fetus.
References
Aoki M, Harada K, Ogawa M, Tanaka T (2004) Quantitative assessment of right ventricular function using Doppler tissue imaging in fetuses with and without heart failure. J Am Soc Echocardiogr 17:28–35
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurements. Lancet 1:307–310
Curtiss EI, Reddy PS, O’ Toole JD, Shawer JA (1976) Alterations of right ventricular systolic time intervals by choronic pressure and volume overloading. Circulation 53:997–1003
Eiden BW, O’ Leary PW, Tei C, Seward JB (2000) Usefulness of the myocardial performance index for assessing right ventricular function in congenital heart disease. Am J Cardiol 86:654–658
Falkensammer CB, Paul J, Huhta JC (2001) Fetal congestive heart failure: correlation of Tei-index and cardiovascular-score. J Pernat Med 29:390–398
Friedman D, Buyon J, Kim M, Glickstein JS (2003) Fetal cardiac function assessed by Doppler myocardial performance index (Tei Index). Ultrasound Obstet Gynecol 21:33–36
Harada K, Takahashi Y, Shiota T, Suzuki T, Tamura M, Ito T, Takada G (1995) Effect of heart rate on left ventricular diastolic filling patterns assessed by Doppler echocardiography in normal infants. Am J Cardiol 76:634–636
Harada K, Tamura M, Tyono M, Yasuoka K (2002) Comparision of the right ventricular Tei index by tissue Doppler imaging to that obtained by pulsed Doppler in children without heart disease. Am J Cardiol 90:566–569
Harada K, Tsuda A, Orino T, Tanaka T, Takada G (1999) Tissue Doppler imaging in normal fetus. Int J Cardiol 71:227–234
Imamura N, Taketazu M, Smallhorn JF, Hornberger LK (2005) Left ventricular myocardial performance in the fetus with severe tricuspid valve disease and tricuspid insufficiency. Am J Perinatol 22:91–97
Ishii M, Eto G, Tsutsumi T et al (2000) Quantitation of the global right ventricular function in children with normal heart and congenital heart disease: a right ventricular myocardial performance index. Pediatr Cardiol 21:416–421
Leighton RF, Weisser AM, Weinstein PB,Wooley VF (1970) Right and left ventricular systolic time intervals: effects of heart rate, respiration and atrial pacing. Am J Cardiol 27:66–72
Mori Y, Rice MJ, McDonald RW, Wantikun S, Harada K, Shan DJ (2001) Evaluation of systolic and diastolic ventricular performance of the right ventricule in fetuses with ductul constriction using the Doppler Tei index. Am J Cardiol 88:1173–1178
Paladini D, Lamberti A, Teodoro A, Arienzo M, Tartaglione A, Martinelli P (2000) Tissue Doppler imaging in the fetal heart. Ultrasound Obstet Gynecol 6:530–536
Tei C, Nishimura RA, Seward JB, Tajik AJ (1997) Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurements. J Am Soc Echocardiogr 10:169–178
Tekten T, Onbasili AO, Ceyhan C, Unal S, Discigil B (2003) Novel approach to measure myocardial performance index: pulsed-wave tissue Doppler echocardiography. Echocardiography 20(6):503–510
Tekten T, Onbasili AO, Ceyhan C, Unal S, Discigil B (2003) Value of measuring myocardial performance index by tissue Doppler echocardiography in normal and diseased heart. Jpn Heart J 44(3):403–416
Tsutsumi T, Ishii M, Eto G, Hota M, Kato M (1999) Serial evaluation for myocardial performance in fetuses and neonates using a new Doppler index. Pediatr Int 41:722–727
Thomas JD, Weyman AE (1991) Echocardiographic Doppler evaluation of left ventricular diastolic function: physics and physiology. Circulation 84:977–990
Tutschek B, Zimmermann T, Buck T, Bender HG (2003) Fetal Doppler echocardiography: detection rates of cardiac structures and quantitative assessment of the fetal heart. Ultrasound Obstet Gynecol 21:26–32
Williams RV, Ritter S, Tani LY, Pagotto LT, Minich LL (2000) Quantitative assessment of ventricular function in children with single ventricles using the Doppler myocardial performance index. Am J Cardiol 86:1106–1110
Acknowledgment
We thank Dr. Harada for helpful comments and for suggesting the idea for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duan, Y., Harada, K., Wu, W. et al. Correlation Between Right Ventricular Tei Index by Tissue Doppler Imaging and Pulsed Doppler Imaging in Fetuses. Pediatr Cardiol 29, 739–743 (2008). https://doi.org/10.1007/s00246-008-9215-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9215-2