Abstract
We aimed to ascertain the prevalence of cardiac malformation (CM) and its association with antenatal exposure to an antiepileptic drug (AED) in infants of mothers with epilepsy (IMEs). Women with epilepsy (WWE) are enrolled in Kerala Registry of Epilepsy and Pregnancy (KREP) in the prepregnancy or early pregnancy period and are followed up with a standard protocol until the IMEs are 6 years old. At 3 months postpartum, a cardiologist, blinded to the AED exposure, carried out a clinical examination and echocardiography on all live-born babies. Patent foramen ovale (PFO) and interatrial septal defects of < 5 mm in size were excluded from CM. Details of maternal epilepsy, folate usage, AED exposure in the first trimester, and newborn characteristics were abstracted from the records of the KREP. We examined 462 babies. Maternal epilepsy was generalized in 201 (43.50%) or localization related in 241 (52.2%). The AED exposure was monotherapy in 262 (56.7%)—carbamazepine (112), valproate (71), phenobarbitone (43), phenytoin (31), and clonazepam (2)—and polytherapy in 126 (27.3%). Seventy-four infants (16.01%) had no AED exposure. There were 36 infants with CM (7.8%; 95% confidence interval: 5.5–10.6). CMs included atrial septal defect (26; 72.2%), tetrology of Fallot (3; 8.3%), patent ductus arteriosus and pulmonic stenosis (2 each; 5.6%), and ventricular septal defect, tricuspid regurgitation, transposition of great arteries (1 each; 2.8%). CMs were significantly more for IMEs with premature birth (p < .003). There was no association between CM and maternal age, epilepsy syndrome, seizure frequency during pregnancy, and folate use. CMs were more frequent with polytherapy (13; 10.3%) compared to monotherapy (17; 6.5%). Those with valproate exposure had a trend (not statistically significant) toward higher frequency of CM compared to IMEs on other AEDs as monotherapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pregnancy in women with epilepsy (WWE) might carry higher risk to the mother and baby [15]. It is widely recognized that the use of antiepileptic drugs (AEDs) during pregnancy increases the risk of fetal malformations [16]. Antenatal exposure to AEDs is associated with a variety of congenital malformations, including neural tube defects (NTDs), cleft lip and palate, hypospadias, skeletal abnormalities, and cardiac defects [16]. Cardiac malformations (CMs) constitute a substantial proportion of them in most reports [1, 3, 6, 9, 14, 20, 23, 26, 28]. The data on the comparative teratogenicity of AEDs in humans are conflicting, mainly due to inadequate sample size and methodological shortcomings. The reported prevalence of CMs in the community varies widely depending on the time of ascertainment (newborn period vs. later), methods of ascertainment (clinical vs. echocardiography and Doppler studies), and the definitions used (size of the septal defects, direction of flow, etc.). Recent studies indicate that very small defects in the atrial septum or persistent flow across the ductus arteriosus, detected at birth, might not be significant because they might close in the subsequent weeks [24, 30]. The prevalence of CMs at birth has been estimated to be 7–9 per 1000 live births [5, 8, 17]. Prenatal exposure to medications accounts for only a small proportion of CMs, yet they are important modifiable or preventable factors. There have been few systematic prospective studies that evaluated the relationship between prenatal exposure to AEDs and the occurrence of CMs. Our objective was to prospectively ascertain the prevalence of CMs in infants with prenatal exposure to AEDs.
Patients and Methods
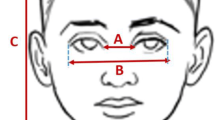
This study was carried out in the Kerala Registry of Epilepsy and Pregnancy (KREP) in one of the southern states of India. WWE are enrolled in this hospital-based registry in the preconception period or during pregnancy and are followed up according to a standard protocol during pregnancy, delivery, and afterward until the infants are 6 years old [29]. Informed consent is obtained from all participants and the study has the approval of the Institutional Ethics Committee. Women are closely monitored for AEDs, folic acid usage, exposure to teratogens (drugs or radiation), substance abuse, and seizure frequency during the entire course of pregnancy. All WWE are screened with serum α-feto protein and ultrasonography in the fourth month of pregnancy. Two doses of intramuscular injections of 10 mg vitamin K are given in the last month of pregnancy. A pediatrician carries out a standardized neonatal clinical examination focusing on congenital malformations on all newborns at birth. At 3 months of age, all infants are examined in the KREP for any congenital malformations. Then a cardiologist, blinded to AED exposure of the infants, carries out a clinical examination and echocardiogram on all infants. CM is defined as any major malformation of the heart or intrathoracic great vessels that is actually or potentially of functional significance [17]. The infants were sedated for echocardiography. Two-dimensional echocardiography or Doppler examination was done using 4–8-MHz probe using Sonos 1000 (Hewlett Packard, Hanover, NJ, USA) or CFM 800 machines. Standard parasternal, subcostal, apical, and suprasternal views were examined. A second cardiologist confirmed malformation using System 5 or Vivid 7 systems (GE Vingmed Ultrasound A/S; GE Healthcare, Horten, Norway) whenever required. Published literature and our experience had shown that some of the smaller defects in the interatrial septum, detected soon after birth, might close in the subsequent weeks. In order to avoid any overreporting, we carried out the echocardiograms when the babies were 3 months old. There are no widely accepted criteria to distinguish between patent foramen ovale (PFO) and atrial septal defect (ASD) [24, 30]. In this study we classified a defect in the interatrial septum that is less than 5 mm in size with the fossa ovalis location as the PFO and defects of other locations and size 5 mm or more as ASD [21, 24]. All of the complex cardiovascular malformations were classified according to the malformation that dominated in the pathological hemodynamics. Trivial patent ductus arteriosus (PDA) or mitral regurgitation detected only by Doppler echocardiography was not included as a CM [30]. We did not screen for any congenital arrhythmia in this study.
Maternal and infant characteristics were abstracted from the KREP protocol datasheets. Maternal epilepsy was classified according to the ILAE terminology into generalized epilepsy (GE) and localization-related epilepsy (LRE). The AEDs used, total daily dose, highest single dose, folic acid usage (milligram per day), exposure to other possible teratogens and drugs, and partial and generalized seizures are recorded in the protocol forms from the month prior to the last menstrual period through the entire pregnancy and postpartum period on a monthly basis. For the purpose of this study, we defined exposure as the use of AEDs anytime during the first trimester. The highest dose of the AED used anytime during the first trimester was taken as the dosage of exposure. In order to make interdrug comparisons and to quantify polytherapy, we used the scoring system from an earlier study to calculate the drug load for each patient irrespective of the AEDs used [13]. One drug score was equivalent to any of the following: 125 mg acetazolamide, 100 mg carbamazepine, 5 mg clobazam, 1 mg clonazepam, 30 mg lamotrigine, 5 mg nitrazepam, 150 mg oxcarbazepine, 50 mg phenobarbitone, 50 mg phenytoin, 100 mg primidone, 30 mg topiramate, or 100 mg valproate. Documented use of folic acid anytime during the first trimester was accepted as use of folic acid. Between April 1998 and December 2004, there were 593 live births from 740 pregnancies enrolled in the KREP. The outcome of other pregnancies were spontaneous abortion (33), medical termination for maternal or social reasons (12), medical termination because of fetal malformations detected antenatally—none of them cardiac defects (3), intrauterine death (13) continuing pregnancies (48), and lost for follow-up (38). There were 15 neonatal death and 47 infants were not eligible (aged less than 3 months) for echocardiography. No autopsy was carried out in the case of medical terminations or other fetal/infant deaths. Echocardiography was carried out in 462 of the 531 (87%) eligible infants.
Data were transferred to an Excel spreadsheet and was analyzed with the SPSS for Windows package. A chi-squared test was used to ascertain significant (p < .05) differences between proportions.
Results
The mean age of mothers of infants under study was 25.6 + 4.1 years. They had GE (201; 43.50%), LRE (241; 52.16%), or other types (20; 4.32%). Parental consanguinity was observed for 3.5% of infants. Family history was positive for a congenital malformation in 1% of the first-degree relatives of the mothers. There were 50 women with two pregnancies each (three of them had three pregnancies each) in this cohort. Within this group, 10 women had infants with CMs in the first or second pregnancy (3 of them were on monotherapy). None of them had infants with CMs in both pregnancies. AEDs were changed between pregnancies for only 3 of the 21 women who were on monotherapy and only 1 of them was associated with CM. These three women who were on carbamzepine were shifted to valproate (two) or phenobarbitone (one) because their diagnosis was revised to primary GE. We did not attempt any statistical analysis on these data because the numbers were very small.
There were no seizures for 216 pregnancies (46.32%), 1 seizure each for 79 pregnancies (17.09%), 2 or 3 seizures for 65 pregnancies (14.06%), 4–6 seizures for 32 pregnancies (6.92%), and 7 or more seizures for 72 pregnancies (15.58%). The infants’s mean birth weight (n = 442) was 2.91 + 0.45 kg (range: 0.95–4.12 kg).
Among the 462 infants examined, 36 infants (7.8%) had a CM (95% confidence interval: 5.5–10.6). Three of them also had other malformations, namely hydronephrosis, multiple cysts in the kidneys, and meningomyelocele in one infant each. The CMs included ASD secondum type (n = 26; 72.2%), tetrology of Fallot (TOF); n = 3; 8.3%), PDA (n = 2; 5.6%), pulmonic stenosis (PS) (n = 2; 5.6%), ventricular septal defect (VSD) (n = 1; 2.8%), tricuspid regurgitation (TR) (n = 1; 2.8%), and transposition of great arteries (TGA) (n = 1; 2.8%). There were 38 infants with PFO and 14 with interatrial septal defect of less than 5 mm in size who were not included in the malformation group. The frequency of CM according to different epileptic syndromes, AED usage, and other maternal characteristics is given in Table 1.
Infants of mothers with GE had a marginally higher frequency of CM (9.5%) than those with LRE (7.1%), but the difference was not statistically significant. Folate use or occurrence of seizures during pregnancy did not have any association with the presence of a CM.
Premature and postmature infants had a significantly higher prevalence of CM (31.3% and 50%, respectively) when compared to infants of normal maturity. Infants with a low birth weight ( < 2.5 kg) had significantly (p = 0.021) higher incidence of CM (15.3%) than others ( > 2.5 kg; 6.3%), the difference being statistically significant (p = 0.021). Nevertheless, when the analysis was restricted to infants with normal maturity, birth weight lost its significance.
Discussion
In this prospective study, we had screened IMEs born under the registry over a period of 6 years. This is probably the largest single-center prospective screening of IMEs for CMs. We chose to carry out clinical and echocardiographic examinations at 3 months of age in order to avoid overdiagnosis of CMs, as transient flow across the interatrial septum would have ceased by that age. There are no well-established criteria to distinguish PFO from ASDs in infants and it is often difficult to categorize between the two in young infants with small defects. By adhering to strict criteria on size (less than 5 mm) and location of the defect, we excluded 52 cases of PFO or very small defects in the atrial septum. It is possible that severe cardiac anomalies that lead to very early neonatal deaths might not have been recorded in this study because we chose to carry out the cardiac evaluation at 3 months. There were 15 deaths in this period, but no autopsy was carried out on them. All deliveries were conducted in the hospital, and a routine neonatal examination was carried out on all children. All deaths occurred in the hospital, and the available clinical records did not suggest any CM in any of them.
Our results indicate that IMEs had a higher prevalence of CMs (78 per 1000) when compared to the prevalence reported in most communities (7–9 per 1000) [5, 8, 10, 17, 22], Epidemiological data on the prevalence of CMs in the community vary widely, depending on the timing of the examination, the methods of ascertainment (echocardiography vs. angiography, clinical examination, autopsy, etc) and several other factors [10]. A case-control design for this study would have adjusted for possible underreporting of ASDs in the community. Nevertheless, we could not adopt this design due to technical constraints. An isolated ventricular septal defect is the most common CM reported in population-based studies as well as hospital-based samples and VSDs might account for 28% of all CMs [12, 22]. ASDs rank second or third only in the order of frequency in the community [11, 12]. In contrast to this, ASD was the most common CM in this series. This reversal in the order of frequency also points to a genuine increase in the prevalence of CMs for exposed infants rather than increased detection rate due to active surveillance. In contrast to our observations, an earlier study of children of parents with epilepsy did not show any excess risk of cardiac malformation [7]. The method of ascertainment of malformation and the design of this study is different from the present study.
In the present study there were two infant characteristics that had significant association with the occurrence of CMs (viz. low birth weight and abnormal maturity), but low birth weight lost its significance when premature infants were excluded. In our comparison of pregnancies in WWE with that of women without epilepsy, WWE did not exhibit any increased risk of prematurity or low-birth-weight babies [25]. These infancy-specific characteristics are probably independent of maternal epilepsy. Although IMEs had a higher frequency of CMs, maternal age or epilepsy-specific characteristics (type of seizures, classification of epilepsy, or seizure frequency) did not correlate with the increased risk of CMs in the IMEs. Apparently, the increased risk is independent of maternal epilepsy characteristics, yet associated with other external or environmental factors, including exposure to AEDs. In this series, there was a trend toward a higher frequency of CMs with polytherapy compared to monotherapy but the difference was not statistically significant. The risk of CM was not significantly higher for any specific AED (as monotherapy) although sodium valproate had a higher frequency than others. Because an individual AED as monotherapy had only a small number of subjects, the study was limited in identifying the risk of CM for any particular AED. It is widely recognized that antenatal exposure to AEDs increases the risk of congenital malformations by two to three times, the risk being higher with polytherapy and increasing dosages [22]. CMs, NTDs, orofacial malformations, and other malformations related to the gastrointestinal, genitourinary, and other systems tend to occur in these patients [2, 16, 19, 20]. The mechanisms by which AED exposure could cause CMs are largely unknown and complex. Except for an association between NTDs and valproate and, to a lesser extent, carbamazepine, no other defect had been specifically associated with any given AEDs. Several CMs, including VSD, PDA, coarctation, hypoplasia of the left heart, hypoplasia of the right heart, PS, and anomalous origin of the pulmonary artery have been reported with antenatal exposure to sodium valproate [18, 26, 27] Recent studies suggest that cardiac defects might be the result of disordered neural crest migration [18]. There were eight cases of NTDs in this cohort, but only one of them had a CM. Our experience suggests that the CM and NTDs do not share a common pathogenesis.
Great care should be exercised while attempting to ascertain the etiology of a given congenital malformation. Genetic factors, nutritional deficiencies, exposure to teratogens, and other environmental factors might operate independently or conjointly [4]. Although this is a prospective study, there is a possibility of underascertainment. No autopsy was carried out on the abortus or intrauterine death. Thirteen percent of the eligible live-born infants did not undergo echocardiography; some for technical reasons like the baby failed to sleep. The distinction between PFO and ASD was somewhat arbitrary. Our data had demonstrated that IMEs have a higher prevalence of CMs than the community. Prematurity was an important risk factor for CMs in IMEs. Maternal characteristics (epilepsy classification, seizure frequency during pregnancy) and therapy characteristics (number of AEDs used, cumulative dosage, and concomitant use of folic acid) did not have any significant association with risk of CMs. There was no significant association between CMs and any specific AED, although those exposed to valproate had the highest frequency of CMs. Data from such large prospective cohorts are helpful in counseling WWE and their families on the specific issues related to risk of CMs in their infants.
References
American Academy of Pediatrics Committee on Drugs, Anticonvulsants and Pregnancy (1979) Pediatrics 63:331–333
Artama M, Auvinen A, Raudaskoski T, Isojarvi I, Isojarvi J (2005) Antiepileptic drug use of women with epilepsy and congenital malformations in offspring. Neurology 64:1874–1878
Bertollini R, Mastroiacovo P, Segni G (1985) Maternal epilepsy and birth defects: a case-control study in the Italian Multicentric Registry of Birth Defects (IPIMC). Eur J Epidemiol 1:67–72
Brent RL (2004) Environmental causes of human congenital malformations: the pediatrician's role in dealing with these complex clinical problems caused by a multiplicity of environmental and genetic factors. Pediatrics 113(4 Suppl):957–968
Carlgren L-E, Ericson A, Kallen B (1987) Monitoring of congenital cardiac defects. Paediatr Cardiol 8:247–256
Craig J, Morrison P, Morrow J, Patterson V (1999) Failure of periconceptual folic acid to prevent a neural tube defect in the offspring of a mother taking sodium valproate. Seizure 8:253–254
Friis ML, Hauge M (1985) Congenital heart defects in live-born children of epileptic parents. Arch Neurol 42:374–376
Hanna EJ, Nevin NC, Nelson J (1994) Genetic study of congenital heart defects in Northern Ireland (1974–1978). J Med Genet 31:858–863
Hernandez-Diaz S, Werler MM, Walker AM, Mitchell AA (2000) Folic acid antagonists during pregnancy and the risk of birth defects. N Engl J Med 343:1608–1614
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardol 39:1890–1900
Hoffman JIE (2002) Incidence, mortality and natural history. In Anderson RH, Baker EJ, Macartney FJ, Rigby ML, Shinebourne EA, Tynan MJ (eds), Paediatric cardiology, 2nd ed. Churchill Livingstone, Edinburgh, Vol, I, pp 111–139
Izukawa T (1992) Lightfoot NE trends in neonatal congenital heart disease: the Toronto experience. In Freedom RM, Benson LN, Smallhorn JF (eds), Neonatal heart disease. Springer-Verlag, London, pp 31–33
Kaneko S, Battino D, Andermann E, Wada K et al. (1999) Congenital malformations due to antiepileptic drugs. Epilepsy Res 33:145–158
Kaneko S, Otani K, Kondo T et al. (1992) Malformations in infants of mothers with epilepsy receiving antiepileptic drugs. Neurology 42(4 Suppl 5):68–74
Kaplan PW (2004) Reproductive health effects and teratogenicity of antiepileptic drugs. Neurology 63(10 Suppl 4):S13–S23
Lindhout D, Omtzigt JG (1994) Teratogenic effects of antiepileptic drugs: implications for the management of epilepsy in women of childbearing age. Epilepsia 35(Suppl 4):S19–S28
Mitchell SC, Korones SB, Berendes HW (1971) Congenital heart disease in 56,109births; incidence and natural history. Circulation 43:323–332
Mo CN Ladusans EJ (1999) Anomalous right pulmonary artery origins in association with fetal valproate syndrome. J Med Genet 36:83–84
Morrow J, Russell A, Guthrie E, Parsons L et al. (2006) Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 77:193–198
O’Brien MD, Gilmour-White S (1993) Epilepsy and pregnancy Br Med J 307:492–495
Ooshima A, Fukushige J, Ueda K (1995) Incidence of structural cardiac disorders in neonates: an evaluation by color Doppler echocardiography and the results of a 1-year follow-up. Cardiology 86:402–406
Pradat P, Francannet C, Harris JA, Robert E (2003) The epidemiology of cardiovascular Defects, Part I: A study based on data from three large registries of congenital malformations. Pediatr Cardiol 24:195–221
Perucca E (2005) Birth defects after prenatal exposure to antiepileptic drugs. Lancet Neurol 4:781–786
Samanek M, Goetzova J, Benesova D (1986) Causes of death in neonates born with a heart malformation. Int J Cardiol 11:63–74
Sindhu K, Thomas SV, Ajaykumar B, Sylaja PN, Sulekhadevi PB, Jacob S (2005) Complications of pregnancy and delivery in women with epilepsy. Epilepsia 46(Suppl 6):84
Sodhi P, Poddar B, Parmar V (2001) Fatal cardiac malformation in fetal valproate syndrome. Indian J Pediatr 68:989–990
Ten Berg K, van Oppen AC, Nikkels PG et al. (2005) Complex cardiac defect with hypoplastic right ventricle in a fetus with valproate exposure. Prenat Diagn 25:156–158
Thisted E, Ebbesen F (1993) Malformations, withdrawal manifestations and hypoglycemia after exposure to valproate in utero. Arch Dis Child 69:288–291
Thomas SV, Indrani L, Devi GC, Jacob S et al. (2001) Pregnancy in women with epilepsy: preliminary results of Kerala Registry of Epilepsy and Pregnancy. Neurol India 49:60–66
Venugopalan P, Agarwal AK, Johston WJ, Riveia E (2002) Spread of heart diseases seeen in an open access pediatric echocardiography clinic. Int J Cardiol 84:211–216
Acknowledgment
The Kerala Registry of Epilepsy and Pregnancy is supported by a grant-in-aid from the Kerala Council of Science Technology and Environment, the Indian Epilepsy Society, and the Indian Council of Medical Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, S.V., Ajaykumar, B., Sindhu, K. et al. Cardiac Malformations Are Increased in Infants of Mothers with Epilepsy. Pediatr Cardiol 29, 604–608 (2008). https://doi.org/10.1007/s00246-007-9161-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-007-9161-4