Abstract
QT interval on the surface electrocardiogram (ECG) reflects the time for repolarization of myocardium and prolongation of QTc is strongly associated with sudden cardiac death. Studies using novel techniques on beat-to-beat QT interval variability (QTV) have shown that it is influenced by the autonomic nervous system and is a predictor of sudden cardiac death. In this study, we examined the awake and sleep changes in QTV in 39 normal adults (mean age, 35 years) and 10 children (mean age, 11 years) using 24-hour ECG records. We obtained eight 5-minute segments of ECG sampled at 1000 Hz from the 24-hour records. Our results show that there is a diurnal variation of QTvm, detrended QT interval variance corrected for mean QT, and QTvi, an index of QTvm divided by heart rate variability corrected for mean heart rate. There was a significant increase in mean QT during sleep, whereas there was a significant decrease in QTvm and QTvi. QTvi significantly increased during the early morning hours. There were significant but modest correlations between the average 24-hour and awake QTvi and age (p < 0.01). There were also decreased low-frequency and high-frequency powers of QT during sleep. Coherence between heart rate and QT interval fluctuations in the range of 0–0.5 Hz, and especially in the high-frequency range (0.15–0.5 Hz), was significantly lower in adults than in children (p < 0.0002). These findings demonstrate diurnal fluctuations in ventricular repolarization lability. We speculate that these effects may relate to changes in cardiac autonomic function and may contribute to the well-known diurnal variation in the incidence of ventricular arrhythmias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Measures of cardiac autonomic function yield important information about various physiological and pathological conditions and include techniques such as the quantification of heart rate variability, the baroreceptor sensitivity index, and the rate of heart rate recovery after exercise [19, 20]. These studies suggest that children have a relatively higher cardiac vagal function compared to adults. Some of these indices are useful to stratify mild and severe heart failure in stable postoperative patients with congenital heart disease [20].
Spectral analysis can be used to decompose a given time series into its individual frequency components and this has been very fruitful in understanding various control mechanisms in physiological systems. Spectral analysis of heart rate (HR) series usually reveals three peaks in the following bands: very low frequency (VLF; 0–0.04 Hz), low frequency (LF; 0.04–0.15 Hz), and high frequency (HF; 0.015–0.5 Hz). VLF is related to peripheral vascular mechanisms, the renin–angiotensin system, and thermoregulatory mechanisms; LF power is related to baroreceptor mechanisms influenced by sympathetic as well as parasympathetic systems; and HF power is related to respiratory sinus arrhythmia (RSA), which mainly reflects cardiac vagal function [2, 16, 22]. With increasing age, there is a decrease in heart period (HP) or heart rate HR variability, especially in the HF range [25, 29, 34]. The HF power reflects RSA and thus cardiac vagal function. A decrease in HP variability is associated with increased cardiac mortality in patients with cardiac disease as well as normal controls [9, 17].
The QT interval on the surface electrocardiogram (ECG) reflects the time for repolarization of myocardium. The usual duration of the QT interval corrected for mean R-R interval is approximately 400 msec (QTc) and prolongation of QTc is strongly associated with sudden cardiac death. QTc values higher than 440 milliseconds should alert the clinician to the possible risk of serious cardiac events. Cardiac repolarization plays an important role in causing sudden death, and an increase in sympathetic activity and a decrease in cardiac vagal activity make the myocardium vulnerable to fatal arrhythmias [10, 24].
The QT interval closely follows HR, and the literature has shown the possible utility of QT variability as a noninvasive marker of cardiac repolarization. A higher QT variability is associated with sudden death in cardiac patients and also in coronary patients with angina pectoris [4, 7, 28]. Hence, we investigated the effect of age on short-term QT variability of 5-minute ECG records and reviewed several other studies on QT variability [30, 31, 32, 33, 34]. Our findings showed that coherence between QT and HR time series in the 0- to 0.5-Hz range and HF range was inversely related to age and that this may be modulated by vagal function [29,31].
The change from supine to standing posture and intravenous administration of isoproterenol result in a highly significant increase in QTvi suggesting a link between higher QTvi and increased sympathetic activity [30]. Fei et al. [13] showed that the QT/RR relationship is significantly altered in patients with idiopathic ventricular tachycardia compared to normal controls. Atiga et al. [5] showed that patients with hypertrophic cardiomyopathy caused by β-myosin heavy chain gene mutations exhibit labile repolarization quantified by QTvi and may be more at risk for sudden death, and that it is particularly abnormal in patients with poor prognosis. Another important study by Bonnemeier et al. [11] showed that the reduction of the QT interval and QT interval variability after reperfusion at an appropriate time of the infarct-related artery appears to be one of the beneficial mechanisms of primary percutaneous transluminal coronary angioplasty in acute myocardial infarction. This report suggests that a decrease in QTV is related to successful reperfusion. This study clearly showed the effect of early perfusion on changes in QT interval and QTV and its positive prognostic implications on arrhythmic events during a 1-year follow-up. Thus, irrespective of the mechanism of this decrease in QTV after successful reperfusion, the outcome of a decreased QTV is a very important prognostic indicator. The decrease in QTV was 27.5 ± 3 to 24.9 ± 6 msec (p < 0.001).
Thus, the relationship between QTvi, QTc, and the risk of serious cardiac events needs systematic investigation, and QTV appears to be a very promising noninvasive tool to study ventricular repolarization. There have been a few reports of children who died suddenly during tricyclic antidepressant treatment [23], causing one to speculate if these subjects were more vulnerable to such events due to a prolonged QTc or higher QT variability. It is also important to note that sudden cardiac death is very rare in children compared to adults. In our study, we investigated QT interval variability over 24 hours to determine if there are sleep–awake differences and also if the variability differs between children and adults.
Materials and Methods
Thirty-nine adults (26 males and 13 females; 34.5 ± 9.2 years) and 10 children (5 males and 5 females; 11 ± 2.3 years) participated in this study. This study was approved by the institutional review boards at the Wayne State University School of Medicine and the Wright State University School of Medicine. All subjects were healthy and informed consent was obtained prior to participation. The subjects had no history of hypertension, and their routine blood chemistry and ECG were within normal limits. These subjects had not taken any medication for at least 2 weeks prior to the study except for occasional nonopioid analgesics.
Data Collection
Twenty-four-hour ECG was recorded using Delmar Cardiocorders on microcassettes using standard procedures. The 5-minute segments of ECG were digitized from the 24-hour ECG at 1000 Hz at the beginning of each hour. These 5-minute segments provide more accuracy for the QT variability analyses because the resolution for the QT intervals is 1 msec. From these 20 24-hour segments, we chose 8 noise-free, 256-second ECG segments every 3 hours for QT analyses. The patients recorded when they went to sleep and when they woke up. Almost all records were begun between 8 and 11 am and continued for 24 hours.
Analysis of the Data
All analyses were conducted on 256-second segments of data sampled at 1000 Hz. This QT variability algorithm has been described by Berger et al. [7] in detail and has been used by his and our groups in previous studies [4, 30, 31, 32, 33]. This was performed on a PC using Solaris Desktop Unix software (SunSoft, Mountain View, CA, USA), which uses a graphical interface of digitized ECG where the time of the R wave is obtained using a peak detection algorithm. Then the operator provides the program with the beginning and the end of the QT wave template. This algorithm finds the QT interval for each beat using the time–stretch model. If the operator chooses a longer QT template, all the QT intervals will be biased accordingly.
The HR [beats per minute (bpm)] time series were sampled at 4 Hz using the technique of Berger et al. [6]. This technique preserves all the frequencies up to one-fourth of the sampling rate. This does not affect the data up to 1 Hz because we sample the signal at 4 Hz. Even when the breathing rate is 30 bpm, the RSA-related changes in HR would occur at 0.5 Hz. We used HR time series free of ventricular premature beats and noise. The data were then detrended by using the best-fit line prior to the computation of spectral analyses. All 39 adults and nine children had complete data, and one child had some missing data. This subject was excluded from some of the analyses.
The mean HR (HRm), detrended HR variance (HRv), mean QT interval (QTm), detrended QT variance (QTv), and QTvm corrected for QTm QTv/QT 2m ) were calculated from the instantaneous HR and QT time series of 1024 points (256 seconds).
A normalized QT variability index was calculated as follows, as suggested by Berger et al. [7]:
This index represents the log-ratio between the QT interval and the HR variabilities, each normalized for the corresponding mean.
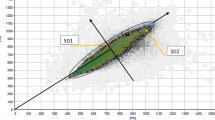
HR and QT interval time series (256 seconds at 4 Hz = 1024 points) were subjected to spectral analyses and the power spectrum was computed with the Blackman–Tukey method [8]. The powers were integrated in the bands of VLF, LF, and HF regions. HR and QT interval time series were subjected to spectral analysis and the cross-spectrum between the two time series was computed from 256 seconds with the Blackman–Tukey method [8].
Statistical Analysis
Analysis of variance for repeated measures was used for all eight epochs of HR and QT variables. Significant effects were followed up by individual comparisons (two-tailed t-tests) for variables of interest. Twenty-four-hour means were also compared using two-tailed t-tests. The significance level was set at p ≤ 0.05. Subjects with missing data points were excluded from the analyses.
Results
There were significant increases in QTm (F = 6.5, df = 7,315, p < 0.00001) and significant decreases in QTvm (F = 5.2, df = 7,315, p < 0.00001) and QTvi (F = 6.7, df = 7,315, p < 0.00001) during sleep in adults as well as children (p < 0.00001) (Figs. 1, 2, 3). LF and HF powers were also lower during sleep in both groups (F = 6.71, df = 7,315; and F = 7,315; p < 0.00001). The HF power was also significantly higher in adults (F = 3.8, df = 1,38, p < 0.05) (Figs. 4 and 5). Although there was an increase in coherence in the bands of 0–0.5 Hz and HF range (0.15–0.5 Hz) during sleep in both group (F = 5.9, df = 7,315; and F = 4.5, df = 7,315; p < 0.00001), coherence was significantly higher in the children’s group compared to the adult group (F = 10.5, df = 1,45, p < 0.002; and F = 16.3, df = 1,45, p < 0.0002 respectively) (Figs. 6 and 7).
Table 1 shows the mean values for 24-hour records for all variables. HF power was significantly higher in adults compared to children, and total coherence between HR and QT interval fluctuations (0–0.5 Hz) was higher in children (Table 1).
There were significant but modest correlations between QTvi and age for 24-hour and awake periods (r = 0.29 and 0.35; n = 48; p < 0.05, respectively).
Discussion
To our knowledge, this is the first report on the relationship between age and 24-hour QT variability. However, we used only eight segments of 256 seconds of ECG every 3 hours rather than the whole 24-hour record due to the labor-intensive nature of using a 1000-Hz sampling rate and to have relatively stationary segments. These findings are in agreement with our previous findings of increased coherence in children, especially in the range of 0–0.5 Hz. This appears to be related to the significantly increased coherence in children in during sleep compared to adults. Coherence indicates how closely the QT interval changes in relation to each R-R interval.
These findings have important implications for the use of QTV as a noninvasive tool to investigate the effects of certain drugs on cardiac repolarization in children. Drugs such as tricyclic antidepressants are associated with several sudden deaths in children [23]. It is also important to note that in the study by Berger et al. [7], there was a significantly decreased coherence in the 0- to 0.2-Hz range in patients with dilated cardiomyopathy (0.39 vs 0.28, p < 0.0001). Our previous values of coherence from laboratory records of subjects in supine posture for the 0- to 0.5-Hz range were 0.36 and 0.50, respectively, for adults and children, which are much higher than the hourly values of coherence for the 24-hour records (0.25 and 0.36, respectively for adults and children during sleep). This may be due to the difference between the laboratory records and the 24-hour ambulatory records. One should also note that the mean coherence used in this study is simply the arithmetic mean of all the values in a particular frequency band and was not weighted. Hence, the coherence values may have been low for each band.
Our previous reports showed that enhanced sympathetic activity is associated with an increased QTvi [30]. However, the present study did not find any differences in QTvi between children and adults, most likely because the increased HR variability is also associated with an increased QT variability in children. Sympathetic as well as parasympathetic systems influence the QT interval and the enhanced sympathetic drive may be responsible for the circadian variation of the QT interval [1, 3, 18]. Beta-blockers are associated with a decrease in QT variability [26]. Kostis and Belina [14] showed that although there was an increase in the mean QT interval at nighttime, beat-to-beat QT variability was significantly lower (p = 0.0005). They attributed these changes to an increased vagal activity at nighttime. Our findings are similar, and QTvm as well as QTvi were significantly lower during sleep and increased again during the morning. It is also important to note that autonomic modulation of the sinus node and ventricular myocardium is independent to a certain extent, and this may be exaggerated in cardiac conditions [7, 15]. This again highlights the importance of QT variability as a novel measure of ventricular repolarization, which may yield additional information to that provided by HR variability alone. We also showed that QTvi increases significantly during pemoline administration in normal controls [21]. Pemoline is a sympathomimetic drug with similar effects to amphetamines and sudden deaths have been associated with eve and ecstasy (3,4-methylenedioxyethamphetamine and 3,4-methylenedioxymethamphetamine, respectively), which are street drugs with a similar chemical structure to that of amphetamines [12]. We have also found that nortriptyline increases QTvi in patients with panic disorder, most likely due to its sympathomimetic effects, and tricyclic antidepressants similar to nortriptyline are associated with sudden death in children [23].
The increased HF power of the QT interval in adults differs from what is seen in HR time series; thus, the HF power may be modulated by some other mechanisms in addition to cardiac vagal function and should be investigated further. An additional finding is that the coherence between HR and QT time series was significantly higher in children. This may be due to the fact that children have a higher vagal activity. These findings demonstrate diurnal fluctuations in ventricular repolarization lability. These effects may relate to changes in cardiac autonomic function and may contribute to the well-known diurnal variation in the incidence of ventricular arrhythmias. These findings may have implications for evaluating the risk for significant cardiac events in vulnerable populations.
It is also important to note that children are not vulnerable to sudden cardiac death except in conditions such as long QT syndrome and in cases in which children are taking certain medications such as tricyclic antidepressants. One could speculate that the reason for this is the higher vagal and lower sympathetic function in children compared to adults. There are other established techniques to study cardiac autonomic function, including baroreceptor sensitivity and heart rate recovery after exercise in children [19, 20]. These measures also reflect cardiac autonomic function.
Study Limitations
The small number of subjects in the study in the children’s group makes it difficult to draw definite conclusions. Possible hormonal changes during and after puberty, and the effect of contraceptives on QT measures, may also have influenced the findings to some extent.
References
S Ahnve H Vallin (1982) ArticleTitleInfluence of heart rate and inhibition of autonomic tone of the QT interval Circulation 65 435–439
S Akselrod D Gordon FA Ubel et al. (1981) ArticleTitlePower spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control Science 213 220–222 Occurrence Handle1:STN:280:Bi6B38rot1Q%3D Occurrence Handle6166045
JP Amlie H Refsum (1981) ArticleTitleVagus-induced changes in ventricular electrophysiology of the dog heart with and without beta-blockade J Cardiovasc Pharmacol 3 1203–1210 Occurrence Handle1:CAS:528:DyaL38XmtVU%3D Occurrence Handle6173519
WL Atiga H Calkins JH Lawrence et al. (1998) ArticleTitleBeat-to-beat repolarization lability identifies patients at risk for sudden cardiac death J Cardiovasc Electrophysiol 9 899–908 Occurrence Handle1:STN:280:DyaK1M%2FgtVSjuw%3D%3D Occurrence Handle9786070
WL Atiga L Fananpazir D McAreavey H Calkins RD Berger (2000) ArticleTitleTemporal repolarization lability in hypertensive cardiomyopathy caused by beta-chain heavy gene mutations Circulation 101 1237–1242
RD Berger S Akselrod D Gordon RJ Cohen (1986) ArticleTitleAn efficient algorithm for spectral analysis of heart rate variability IEEE Trans Biomed Eng 33 900–904 Occurrence Handle1:STN:280:BiiD3cnnvV0%3D Occurrence Handle3759126
RD Berger EK Casper KL Baughman et al. (1997) ArticleTitleBeat-to-beat QT interval variability. Novel evidence for repolarization lability in ischemic and nonischemic dilated cardiomyopathy Circulation 96 1557–1565
RD Berger JP Saul RJ Cohen (1989) ArticleTitleTransfer function analysis of autonomic regulation. I. The canine atrial response Am J Physiol 25 H142–H152
JT Bigger JL Fleiss R Steinman et al. (1992) ArticleTitleFrequency domain measures of heart period variability and mortality after myocardial infarction Circulation 85 164–171
O Binah M Rosen (1992) ArticleTitleMechanisms of ventricular arrhythmias Circulation 85 I25–I31
H Bonnemeier F Hartmann KH Uwe et al. (2001) ArticleTitleCourse and prognostic implications of QT interval and QT interval variability after primary coronary angioplasty in acute myocardial infarction J Am Coll Cardiol 37 44–50 Occurrence Handle10.1016/S0735-1097(00)01061-5 Occurrence Handle1:STN:280:DC%2BD3M%2Fptl2hsw%3D%3D Occurrence Handle11153771
GP Dowling ET McDonough RO Bost (1987) ArticleTitleEve and ecstasy: a report of five deaths associated with the use of MDEA and MDMA J Am Med Assoc 257 1615–1617 Occurrence Handle10.1001/jama.257.12.1615 Occurrence Handle1:STN:280:BiiC2c7lsVA%3D
L Fei DJ Statters JS Gill D Katritsis AJ Camm (1994) ArticleTitleAlteration of the QT/RR relationship in patients with idiopathic ventricular tachycardia Pacing Clin Electrophysiol 17 199–206 Occurrence Handle1:STN:280:ByuB38vmtFE%3D Occurrence Handle7513405
WJ Kostis JC Belina (2000) ArticleTitleDifferences in beat-to-beat variability of the QT interval between day and night Angiology 5 905–911
P Kowallik C Braun M Meesman (2000) ArticleTitleIndependent autonomic modulation of sinus node and ventricular myocardium in healthy young men during sleep J Cardiovasc Electrophysiol 11 1063–1070 Occurrence Handle1:STN:280:DC%2BD3crgvVWlsQ%3D%3D Occurrence Handle11059967
A Lindqvist J Jalonen P Parviainen K Antilla LA Laitinen (1990) ArticleTitleEffect of posture on thermally stimulated cardiovascular oscillations Cardiovasc Res 24 373–380 Occurrence Handle1:STN:280:By%2BA383js1I%3D Occurrence Handle2372793
H Molgaard KE Sorensen P Bjerregard (1991) ArticleTitleAttenuated 24-hour heart rate variability in apparently healthy subjects, subsequently suffering sudden cardiac death Clin Auton Res 1 233–237 Occurrence Handle1:STN:280:By2A2crnsF0%3D Occurrence Handle1822256
Y Murakawa H Inoue A Nozaki T Sugimoto (1992) ArticleTitleRole of sympathovagal interaction in diurnal variation of QT interval Am J Cardiol 69 339–343
H Ohuchi H Suzuki K Yasuda et al. (2000) ArticleTitleHeart rate recovery after exercise and cardiac autonomic nervous system activity in children Pediatr Res 47 329–335
H Ohuchi H Takasugi H Ohashi et al. (2003) ArticleTitleStratification of pediatric heart failure on the basis of neurohormonal and cardiac autonomic nervous system activities in patients with congenital heart disease Circulation 108 2368–2376
R Pohl R Balon A Jayaraman RG Doll VK Yeragani (2003) ArticleTitleEffect of fluoxetine, moline and placebo on heart period and QT variability in normal humans J Psychosom Res 55 247–251 Occurrence Handle10.1016/S0022-3999(02)00478-6 Occurrence Handle12932798
B Pomeranz RJB Macaulay MA Caudill et al. (1985) ArticleTitleAssessment of autonomic function in humans by heart rate spectral analysis Am J Physiol 248 H151–H153
MA Ridlle JC Nelson CS Kleinman et al. (1991) ArticleTitleSudden death in a child receiving norpramin: a review of three reported cases and commentary J Am Acad Child Adolesc Psychiatr 30 104–108 Occurrence Handle1:STN:280:By6C2s%2FhtFU%3D Occurrence Handle2005044
PJ Schwartz S Wolf (1978) ArticleTitleQT interval prolongation as predictor of sudden death in patients with myocardial infarction Circulation 57 1074–1077 Occurrence Handle1:STN:280:CSeC2cnoslQ%3D Occurrence Handle639227
DC Shannon DW Carley H Benson (1987) ArticleTitleAging of modulation of heart rate Am J Physiol 22 H874–H877
JP Singh P Musialek P Sleight P Davey M Marinho (1998) ArticleTitleEffect of atenolol or metoprolol on waking hour dynamics of the QT interval in myocardial infarction Am J Cardiol 81 924–926
GF Tomaselli DJ Buckelmann HG Calkins (1994) ArticleTitleSudden cardiac death in heart failure: the role of abnormal repolarization Circulation 90 2534–2539 Occurrence Handle1:STN:280:ByqD2czitFQ%3D Occurrence Handle7955213
B Vrtovec V Starc R Starc (2000) ArticleTitleBeat-to-beat QT interval variability in coronary patients J Electrocardiol 33 119–125 Occurrence Handle1:STN:280:DC%2BD3c3nslGmtA%3D%3D Occurrence Handle10819405
VK Yeragani R Pohl R Berger R Balon K Srinivasan (1994) ArticleTitleRelationship between age and heart rate variability in supine and standing postures: a study of spectral analysis of heart rate Pediatr Cardiol 15 14–20
VK Yeragani R Pohl VC Jampala et al. (2000) ArticleTitleEffect of posture and isoproterenol on beat-to-beat heart rate and QT variability Neuropsychobiology 41 113–123
VK Yeragani R Pohl VC Jampala R Balon C Ramesh (2000) ArticleTitleEffect of age on QT variability Pediatr Cardiol 21 411–415
VK Yeragani R Pohl VC Jampala et al. (2000) ArticleTitleIncreased QT variability in patients with panic disorder and depression Psychiatr Res 93 225–235 Occurrence Handle10.1016/S0165-1781(00)00119-0 Occurrence Handle1:STN:280:DC%2BD3c3is1WhsA%3D%3D
VK Yeragani RKA Radhakrishna R Pohl VC Jampala R Balon (2001) ArticleTitleHeart rate and QT variability in children with anxiety disorders: a preliminary report Anxiety Depression 13 72–77 Occurrence Handle10.1002/da.1019 Occurrence Handle1:STN:280:DC%2BD3Mris1eksA%3D%3D
VK Yeragani E Sobolewski J Kay VC Jampala G Igel (1997) ArticleTitleEffect of age on long-term heart rate variability Cardiovasc Res 35 35–42 Occurrence Handle10.1016/S0008-6363(97)00107-7 Occurrence Handle1:STN:280:ByiH2cjptVA%3D Occurrence Handle9302345
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yeragani, V., Berger, R., Pohl, R. et al. Effect of Age on Diurnal Changes of 24-Hour QT Interval Variability . Pediatr Cardiol 26, 39–44 (2005). https://doi.org/10.1007/s00246-004-0676-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-004-0676-7