Abstract
The objective of this study was evaluate the relationships between abnormal pulmonary circulation, lung function, and respiratory response during exercise in Fontan patients. Pulmonary function and cardiopulmonary exercise tests were performed in 101 Fontan patients and 122 controls. A small vital capacity (VC) with a high residual volume-to-total lung capacity ratio and a slight but significant low arterial saturation with hypocapnia were observed in Fontan patients. The number of surgical procedures determined VC. Total cavopulmonary connection, fenestration, higher pulmonary arterial wedge pressure, and smaller VC were independent determinants of low arterial saturation, which was the only determinant of hypocapnia. Arterial saturation decreased during exercise and resting arterial saturation correlated with that at peak exercise. Improvement in dead space ventilation was less in Fontan patients and was independently determined by resting arterial saturation. A steeper minute ventilation–carbon dioxide production slope was determined by resting arterial saturation, arterial carbon dioxide tension, and peak oxygen uptake. In Fontan patients, in addition to dead space ventilation, surgery-related reduced VC, the type of repair, and high pulmonary arterial wedge pressure cause arterial desaturation with subsequent hypocapnia, resulting in accelerated inefficient ventilation at rest and during exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Post-Fontan patients have an abnormal pulmonary circulation, cardiorespiratory response to exercise [6, 7, 12, 20], and impaired pulmonary function [10, 17]. However, their interrelationships, including pulmonary gas exchange or the influence of type of repair, have not been well demonstrated. Although the ventilatory response during exercise characterizes the severity of chronic congestive heart failure [3], it is unclear whether the abnormal ventilatory response characterizes the Fontan patients or stratifies their functional status. Therefore, we analyzed the ventilatory response and pulmonary gas exchange during exercise and compared the results with clinical profiles, including hemodynamics and pulmonary function.
Materials and Methods
Patients
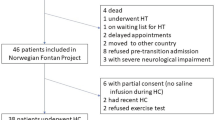
Of the 230 patients who underwent the Fontan operation between October 1979 and October 1999 at our institute, 101 of the 195 survivors who had performed exercise and pulmonary function tests were studied (Table 1). Surgical procedures included atriopulmonary connection (APC) in 29 patients and total cavopulmonary connection (TCPC) by intraatrial rerouting either with a polytetrafluorethylene tube in 38 patients or with a heterologous pericardial baffle in 24. TCPC was achieved without cardiopulmonary bypass in 10 patients (Table 1). Fenestration was created at the time of the Fontan operation in 4 patients, in 1 of whom it closed spontaneously, a trivial shunt persisted in 1, and a significant fenestration was demonstrated in the other 2. Patients with ventricular tachycardia who had received a beta blocking agent were excluded from the study. The control group consisted of a cohort of 64 male and 58 female patients aged 5–24 years with a history of Kawasaki disease without stenotic coronary arterial lesions. None of the controls had abnormal findings on physical examination, chest x-ray, electro cardiogram (ECG), two-dimensional echocardiogram, or treadmill exercise test.
Cardiac Catheterization and Ventricular Morphology
In 81 Fontan patients and 42 controls, cardiac catheterization with cineventriculography was performed within 6 months of exercise testing. We measured vascular and chamber pressures. Oxygen consumption was estimated from age, sex, and heart rate data and cardiac index was measured using the Fick principle with the assumption that right and left pulmonary arterial saturations were equal in patients with a bidirectional Glenn anastomosis because it was clinically difficult to measure a precise distribution of right and left pulmonary blood flow [17].
Ventricular morphology was determined angiographically and patients were subdivided into two groups [17]: (1) a non-left ventricular-type group with either a dominant right ventricle with or without a rudimentary left ventricle (n = 42) or the presence of both right and left ventricles (n = 14) (group non-LV, n = 56), and (2) a dominant left ventricle group with or without a rudimentary right ventricle (group LV, n = 45). The volumes of the right and left ventricles were calculated using Simpson’s rule and the area–length method, respectively. For standardization, end diastolic ventricular volume was divided by body surface area (volume index). Ejection fraction was calculated as the ratio of stroke volume to end-diastolic volume (%).
Significant fenestration was seen in two patients, and moderate to severe atrioventricular valve regurgitation was observed in four patients.
Pulmonary Function Tests
In all Fontan patients and 44 controls, we measured vital capacity (VC; L), the percentage forced expiratory volume in 1 second (Spirosift SP-600, Fukuda Denshi, Tokyo), the functional residual capacity (ml), residual volume (ml), total lung capacity (L) (Ellopse-1000 system, Fukuda Denshi), and the diffusion capacity of carbon monoxide of the lung (DLCO, ml/min/mmHg) by a single breath method. VC was also calculated as the percentage of the body height predicted normal value for 44 controls. We calculated the ratio of residual volume to total lung capacity (RV/TLC). Arterial oxygen saturation (SaO2) in 20 Fontan patients without cardiac catheterization was measured by pulse oxymeter (PULSOX-M2, Teijin, Tokyo) in the outpatient clinic after a supine rest.
Exercise Protocol
All patients exercised on a treadmill (Q-5000 system, Quinton, Seattle, WA, USA). After a 3-minute warm-up (1.5 km/min and 0% grade), treadmill speed and grade were increased at 30-second intervals [15]. All patients were exercised to the end of their tolerance.
Measurements
A 12-lead ECG was recorded throughout the exercise test. Ventilation was measured by a breath-by-breath method. Subjects breathed through a fitted mask and a hot wire anemometer (Riko AS500, Minato Medical Science, Osaka, Japan) measured inspired and expired flow continuously. The partial pressures of oxygen and carbon dioxide were measured continuously at the mouth with a mass spectrometer (MG-300, Perkin–Elmer, St Louis, MO, USA). The respiratory rate (breaths/min), tidal volume (L), minute ventilation (VE; L/min), oxygen uptake (VO2; ml/min), carbon dioxide production (ml/min), respiratory gas exchange ratio, and the oxygen and carbon dioxide ventilatory equivalents were computed in real time. Peak VO2 was also expressed as a percentage of predicted normal values. Ventilatory anaerobic threshold was defined by Wasserman’s criteria and/or determined by the V-slope method [1, 23] Normal data were also obtained from 122 controls as described previously [14].
Arterial Blood Gas Analysis
Blood samples were taken from an indwelling 22 G angiocath placed in a radial or brachial artery in 16 Fontan patients (APC = 6; TCPC =10) and 15 controls. Samples were taken at rest, 3 minutes after warm-up walking began, at AT, and at peak exercise and stored on ice (<20 min) until analyzed for pH, bicarbonate, and arterial partial pressures of oxygen and carbon dioxide (PaO2 and PaCO2; ABL3 blood gas analyzer, Radiometer, Copenhagen, Denmark). Arterial blood lactate concentration (mmol/L) was measured by an enzyme electrode.
Calculations
The physiologic dead space/tidal volume ratio (VD/VT) was calculated using Enghoff’s modification of the Bohr equation with PaCO2 [8], The ratio of change in VE to that in carbon dioxide production from warm-up to peak exercise (VE/VCO2 slope) was also calculated as an index of ventilatory acceleration and efficiency.
Informed Consent
Informed consent was obtained from each subject and his or her parents. This protocol was in agreement with the guidelines of the ethics committee of the National Cardiovascular Center, Osaka, Japan.
Statistical Analysis
The difference in cardiopulmonary function was evaluated using one-way analysis of variance with Scheffe’s post hoc test. Simple regression analysis was used to determine correlations between continuous parameters obtained. To detect independent predictors that determined ventilation, pulmonary gas exchange, and aerobic exercise capacity by stepwise multivariate linear regression analysis, we used 11 indices of patients’ background; [ages at exercise test and Fontan operation, follow-up period, number of surgical procedures, ventricular morphology (left ventricular type or not), type of Fontan operation (APC or TCPC, with or without a fenestration), with or without a history of pulmonary artery banding, with or without a previous Glenn anastomosis, with or without a significant atrioventricular valve regurgitation, and with or without a diuretic medication], hemodynamic parameters (mean pulmonary arterial, wedge and ventricular end-diastolic pressures, volume index, ejection fraction, and cardiac index), and pulmonary parameters (VC, RC/TLC, percentage forced expiratory volume in 1 second, DLCO, SaO2, and resting PaCO2 and VD/VT). Data are expressed as the mean ± SD. A p value <0.05 was considered statistically significant.
Results
Hemodynamics
Pulmonary arterial wedge pressure was higher and ejection fraction and cardiac index were lower in Fontan patients than in controls (Table 1).
Pulmonary Function
Although an obstructive ventilator impairment was not observed, total lung capacity, VC, and functional residual capacity were lower and the RV/TLC was higher in Fontan patients than in controls. Because there was no difference in residual volume between Fontan patients and controls, a high RV/TLC indicated “air trapping” in the lung after the Fontan operation (Table 2). Lower percentage predicted VC and higher RV/TLC were independently determined by the number of surgical procedures (p < 0.001). Older age at exercise test and large ventricular volume index independently determined a higher RV/TLC (p < 0.001). DLCO was lower in Fontan patients and a lower DLCO was determined by an older age at exercise test and a smaller VC (p < 0.001 for both).
Resting SaO2 was lower in Fontan patients and a lower SaO2 was determined independently by the procedures of TCPC and fenestration (p < 0.01 for both), higher pulmonary arterial wedge pressure (p < 0.001), and smaller VC (p < 0.05).
Exercise capacity
Gas exchange ratio at peak exercise exceeded 1.10 in all groups. Exercise duration, time of the AT, and peak VO2 and its percentage for controls were markedly lower in Fontan patients than in controls (Table 3).
Pulmonary gas exchange, Blood lactate, and Arterial Gas Analysis during Exercise
Blood Lactate
Blood lactate tended to be higher in Fontan patients (n = 7) from warm-up to the AT exercise level, but the peak value was lower compared to that of controls (n = 8) (p < 0.01). When the change in blood lactate was plotted against that in VO2, the change in lactate was greater in Fontan patients (Fig. 1a).
pH, Bicarbonate
PH was higher in Fontan patients (n = 16) than in controls (n = 15) throughout the test (p < 0.05–0.01), and bicarbonate from rest to the AT exercise level was lower in Fontan patients than in controls (p < 0.05). When the pH and bicarbonate changes were plotted against those in VO2, the changes were greater in Fontan patients (Figs 1a and 1c).
PaO2
PaO2 was lower in Fontan patients (n = 16) than in controls (n = 15) throughout the test (p < 0.0001). PaO2 was lower in TCPC patients than in APC patients (p < 0.01) and decreased during exercise (p < 0.05) (Fig. 2a).
SaO2
SaO2throughout the exercise test was lower in Fontan patients (p < 0.1, n = 16) and its decline tended be lower in Fontan patients than in controls (p < 0.001). Resting SaO2 correlated well with that at peak exercise (r = 0.80, p < 0.001) and tended to correlate with its decrease from rest to peak exercise (r = 0.43, p < 0.1).
Arterial to End-Tidal Oxygen and Carbon Dioxide Tension Differences
End-tidal to PaO2 difference was greater in Fontan patients than in controls throughout the study (p < 0.001) and it was greater in TCPC patients than in APC patients (p < 0.05). Although the arterial to end-tidal carbon dioxide tension difference was greater in Fontan patients (p < 0.05–0.001), no difference was observed between groups of APC and TCPC. Because a tight correlation between end-tidal and arterial carbon dioxide tensions in Fontan and control subjects (n = 31) was demonstrated at rest, warm-up, AT, and peak exercise (PaCO2 = 16.7 + 0.62 ·x, 16.6 + 0.57 ·x, 17.6 + 0.53 ·x, and 17.0 + 0.52 ·x, respectively, where x is end-tidal carbon dioxide tension; r = 0.84–0.91, p < 0.0001), it was possible to estimate PaCO2 from end-tidal carbon dioxide tension and apply these equations to the other patients and controls without an arterial gas analysis to calculate VD/VT.
PaCO2
Resting PaCO2 was lower in Fontan patients than in controls and was determined by only SaO2 (p < 0.001) when resting ventilatory equivalent for carbon dioxide production was excluded from the multivariate analysis. There was no difference in change in PaCO2 from rest to peak exercise between Fontan patients and controls; a lower PaCO2 persisted throughout exercise in the Fontan patients (p < 0.001; Fig. 2b).
Respiratory Pattern
Resting respiratory rate was faster in Fontan patients (Table 3), and a smaller VC (p < 0.001) and lower PaCO2 (p < 0.01) independently determined the faster respiratory rate. Tidal volume tended to be smaller in Fontan patients, and the smaller tidal volume was independently determined by a smaller VC (p < 0.001). VE per body weight tended to be greater in Fontan patients and a lower PaCO2, smaller VC, younger age (p < 0.001 for all) and higher RV/TLC (p < 0.05) independently determined resting VE.
Respiratory rate, tidal volume, and VE at peak exercise and their changes from rest to exercise were smaller in Fontan patients than in controls (p < 0.001). However, ratios of change in respiratory rate to that in VE from both rest to the AT and AT to peak exercise were higher and a ratio of change in tidal volume from rest to the AT level was smaller in Fontan patients than in controls (p < 0.01–0.001) (Table 3). The higher former ratio and lower latter ratios were independently determined by a smaller VC (p < 0.001). Relationships between respiratory rate, tidal volume, and VE are illustrated in Fig. 3. Diffusion capacity and the VD/VT also independently determined respiratory rate increase from rest to the AT exercise (p < 0.05); however, because these two indices were independently determined by VC, VC was the most important and powerful determinant of respiratory pattern at rest and during exercise.
Ventilatory Efficiency
Although there was no difference in resting VD/VT between Fontan patients and controls, the decline (improvement) in VD/VT from warm-up to peak exercise was smaller (p < 0.001) in Fontan patients, and a lower PaCO2 as well as a lower VD/VT independently determined this improvement (p < 0.001). Resting ventilatory equivalent for CO2 and VE/VCO2 slope were markedly higher in Fontan patients than in controls (Table 3). Higher resting ventilatory equivalent for carbon dioxide was independently determined by a lower PaCO2 and a higher RV/TLC (p < 0.001), and a higher VE/VCO2 slope was independently determined by a lower SaO2 (p < 0.05) and a lower PaCO2 (p < 0.001). Relationships between SaO2, PaCO2, and the VE/VCO2 slope are illustrated in Fig. 4. Thus, PaCO2 was the most important and powerful determinant of ventilatory efficiency at rest and during exercise.
Determinants of Aerobic Exercise Capacity
According to a multivariate analysis using patients’ background, hemodynamics, and pulmonary variables, lower percentage predicted peak VO2 was independently associated with older age at exercise test (p < 0.001), non-left ventricular type ventricle patients (p < 0.01), higher RV/TLC (p < 0.01), and lower PaCO2 (p < 0.001).
Discussion
Our major findings are that after Fontan operation, (1) in addition to TCPC and a fenestration, high pulmonary arterial wedge pressure and surgery-related small VC result in a slight but significant hypoxia that causes significant resting hypocapnia; (2) this secondary resting hypocapnia is an important and powerful determinant of subsequent continuing hypocapnia and accelerated low-efficient ventilation during exercise; and (3) the respiratory pattern is determined only by surgery-related vital capacity and not by the impaired hemodynamics.
Accelerated Low-Efficient Ventilation
The current study demonstrates for the first time that in Fontan patients a slight but significant desaturation is the primary cause of abnormal ventilation at rest and during exercise.
In addition to the high sensitivity of the chemoreceptor to PaO2 in the carotid body [4], because hypocapnia in cyanotic congenital heart disease has been demonstrated by several investigators [9], the secondary hypocapnia demonstrated in our study is not surprising.
Right-to-left shunting, ventilation–perfusion mismatch in the lung, and diffusion capacity are the major factors that cause arterial hypoxia. In the usual TCPC, and also fenestration, coronary and systemic venous return(s) through small channels from great veins drains to the systemic atrium and there is often slight leakage through the intraatrial rerouting baffle—both causes of mild hypoxia. The greater difference in the end-tidal to arterial oxygen tension difference in TCPC patients compared to APC patients indicates that the significant difference in SaO2 between the two groups is due to intra cardiac right-to-left shunting. Because a small VC results from repeated palliative surgeries, the ventilation–perfusion mismatch resulting in hypoxia can be caused by uneven lung inflation (probably together with uneven pulmonary arterial resistance) due to adhesions after surgeries. Because high pulmonary arterial wedge pressure may be a result of both ventricular and atrioventricular valve functions and abnormal intrapulmonary capillary circumstances, the pulmonary circulation may be easily disturbed, leading to ventilation–perfusion mismatch in the lung. In contrast, diffusion capacity is independently determined by VC; therefore, the lower diffusion capacity is not a primary factor in their hypoxia.
Although a high resting ventilatory equivalent for CO2 inversely correlated well with resting SaO2 (r = −0.43, p < 0.0001), because the lower PaCO2 was a secondary phenomenon caused by hypoxia and based on the equation, VE = 863 · VCO2/PaCO2 (1 − VD/VT), where VCO2 is a carbon dioxide production, a high ventilatory equivalent for CO2 is not a cause but a result of hypoxia.
SaO2 decline during exercise may represent worsening of the ventilation–perfusion mismatch in the lung [10]. However, the tight correlation between resting and peak SaO2 values implies that factors that determine right-to-left shunting at rest also have a significant influence on progressive hypoxia during exercise [7].
Greater VD/VT during exercise has been identified as an important cause of accelerated ventilation in Fontan patients [19]. Although the decline in VD/VT is small, it is independently determined by the resting PaCO2 as well as resting VD/VT. Moreover, VE/VCO2 slope is independently determined by resting PaCO2 and SaO2. Oren et al. [18] demonstrated that PaCO2 during exercise remains at the preexercise level. Based on the alveolar equation described, previously, together with a small VD/VT reduction, this mechanism may be very important in explaining how the resting desaturation with subsequent lower PaCO2 has a great impact on accelerated inefficient ventilation during exercise in Fontan patients.
Buffering an accumulating blood lactate by the bicarbonate begins above the AT exercise and produces additional CO2 production [23]. Influx of carbon dioxide into the lung is an important stimulus to ventilation [22]; therefore, the early appearance of the AT is certainly responsible for accelerated ventilation at a given workload in Fontan patients [24].
Central sensitivity to CO2 is associated with excess ventilation in heart failure patients [11]. This mechanism may be operative because Fontan patients have similar characteristics as those of heart failure patients (i.e., low cardiac output and exercise capacity and sympathetic activation) [16], although the contribution of this mechanism is unclear in our study. The carotid body sensitivity to PaO2 is also augmented in heart failure patients [2]. Because an inverse correlation between arterial baroreceptor sensitivity and the chemosensitivity exists in humans [21], chemosensitivity may be augmented in Fontan patients with severely depressed arterial baroreflex sensitivity [13]. Therefore, a high chemosensitivity in addition to mild hypoxia may be another explanation for the accelerated ventilation at rest and during exercise.
Rapid and Shallow Respiration
In Fontan patients, rapid and shallow respiration, as observed in patients with congestive heart failure [5], is determined by a small VC caused by repeated surgical procedures. Therefore, the respiratory pattern (respiratory rate and tidal volume) during exercise does not stratify the hemodynamics of the Fontan circulation.
Impact of Ventilatory Impairment on Aerobic Exercise Capacity
In addition to age at exercise test and ventricular morphology [7, 17], because a lower PaCO2 and higher RV/TLC are associated with lower aerobic capacity, a lower PaCO2 caused by the abnormalities linked to hypoxia may be a sensitive marker of overall cardiopulmonary status. Surgical-related significant chest wall deformity as well as adhesions of the lung may restrict the mobility of the chest wall and the lung. Moreover, a large ventricular volume may also reduce lung mobility. Thus, a high RV/TLC may indicate a reduced mechanical mobility of the lung system, resulting in air trapping, and may also limit aerobic exercise capacity.
References
WL Beaver K Wasserman BJ Whipp (1986) ArticleTitleA new method for detecting anaerobic threshold by gas exchange J Appl Physiol 60 2020–2027 Occurrence Handle1:STN:280:BimB2M%2FkvVw%3D Occurrence Handle3087938
TP Chua AL Clark AA Aham AJ Coats (1996) ArticleTitleRelation between chemosensitivity and the ventilatory response to exercise in chronic heart failure J Am Coll Cardiol 27 650–657 Occurrence Handle10.1016/0735-1097(95)00523-4 Occurrence Handle1:STN:280:BymB3cvotFM%3D Occurrence Handle8606277
AL Clark AJ Coats (1992) ArticleTitleThe mechanisms underlying the increased ventilatory response to exercise in chronic stable heart failure Eur Heart J 13 1698–1708 Occurrence Handle1:STN:280:ByyC2s%2FjsVM%3D Occurrence Handle1289102
DJC Cunningham PA Robbins CB Wolff (1986) Integration of respiratory responses to changes in alveolar partial pressures of CO2 and O2 and in arterial pH Handbook of Physiology Bethesda MD . 475–528
I Dimopoulou OK Tsintzas PA Alivizatos GE Tzelepis (2001) ArticleTitlePattern of breathing during progressive exercise in chronic heart failure Int J Cardiol 81 117–121 Occurrence Handle10.1016/S0167-5273(01)00562-9 Occurrence Handle1:STN:280:DC%2BD3MnpvVSlug%3D%3D Occurrence Handle11744124
DJ Driscoll GK Danielson FJ Puga et al. (1986) ArticleTitleExercise tolerance and cardiorespiratory response to exercise after the Fontan operation for tricuspid atresia or functional single ventricle J Am Coll Cardiol 7 1087–1094 Occurrence Handle1:STN:280:BimC28bjtl0%3D Occurrence Handle3958365
K Durongpisitkul DJ Driscoll DW Mahoney et al. (1997) ArticleTitleCardiorespiratory response to exercise after modified Fontan operation: determinants of performance J Am Coll Cardiol 29 785–790 Occurrence Handle10.1016/S0735-1097(96)00568-2 Occurrence Handle1:STN:280:ByiB38njvFc%3D Occurrence Handle9091525
H Enghoff (1938) ArticleTitleVolumen inefficax: Bemerkungzur Frage des shadlichen Raumes, Upsala Lak Foren Forh . 44
BO Eriksson B Bjarge (1975) ArticleTitleOxygen uptake, arterial blood gases and blood lactate concentration during submaximal and maximal exercise in adult subjects with shunt-opened tetralogy of Fallot Acta Ned Scad . 97 187–193 Occurrence Handle1099377
PM Fredriksen J Therrien G Veldtman et al. (2001) ArticleTitleLung function and aerobic capacity in adult patients following modified Fontan procedure Heart 85 295–299 Occurrence Handle10.1136/heart.85.3.295 Occurrence Handle1:STN:280:DC%2BD3M3msFaktQ%3D%3D Occurrence Handle11179270
K Narkiewicz CA Pesek PJH Borne Particlevan de M Kato VK Somers (1999) ArticleTitleEnhanced sympathetic and ventilatory responses to central chemoreflex activation in heart failure Circulation 100 262–267 Occurrence Handle1:STN:280:DyaK1MzktF2htQ%3D%3D Occurrence Handle10411850
H Ohuchi Y Arakaki Y Hiraumi H Tasato T Kamiya (1998) ArticleTitleCardiorespiratory response during exercise in patients with cyanotic congenital heart disease with and without a Fontan operation and in patients with congestive heart failure Int J Cardiol 66 241–251 Occurrence Handle10.1016/S0167-5273(98)00249-6 Occurrence Handle1:STN:280:DyaK1M%2FovFCksA%3D%3D Occurrence Handle9874076
H Ohuchi S Hasegawa K Yasuda et al. (2001) ArticleTitleSeverely impaired cardiac autonomic nervous activity after the Fontan operation Circulation 104 1513–1518 Occurrence Handle1:STN:280:DC%2BD3MrisVWhuw%3D%3D Occurrence Handle11571245
H Ohuchi Y Katou H Hayakawa Y Arakaki T Kamiya (1995) ArticleTitleVentilatory response in children during progressive exercise testing: evaluation using ramp protocol on a treadmill J Jpn Pediatr Soc 99 1246–1255
H Ohuchi T Nakajima M Kawade M Matsuda T Kamiya (1996) ArticleTitleMeasurement and validity of the ventilatory threshold in patients with congenital heart disease Pediatr Cardiol 117 7–14 Occurrence Handle10.1007/s002469900002
H Ohuchi H Tasato Y Sugiyama Y Arakaki T Kamiya (1998) ArticleTitleResponses of plasma norepinephrine and heart rate during exercise in patients after Fontan operation and patients with residual right ventricular outflow tract obstruction after definitive reconstruction Pediatr Cardiol 19 408–413 Occurrence Handle10.1007/s002469900337 Occurrence Handle1:STN:280:DyaK1czmvFWgtA%3D%3D Occurrence Handle9703566
H Ohuchi K Yasuda S Hasegawa et al. (2001) ArticleTitleInfluence of ventricular morphology on aerobic exercise capacity in patients after the Fontan operation J Am Coll Cardiol 37 1967–1974 Occurrence Handle10.1016/S0735-1097(01)01266-9 Occurrence Handle1:STN:280:DC%2BD3MzjtlKhsw%3D%3D Occurrence Handle11401140
A Oren K Wasserman JA Davis BJ Whipp (1981) ArticleTitleEffect of CO2 set point on ventilatory response to exercise J Appl Physiol 51 185–189 Occurrence Handle1:STN:280:Bi6B28znslU%3D Occurrence Handle6790499
J Rhodes (1998) ArticleTitleConcerning the Fontan patients’ excessive minute ventilation during exercise J Am Coll Cardiol 32 1132 Occurrence Handle1:STN:280:DyaK1cvjvFKrsg%3D%3D
J Rhodes RP Garofano FO Bowman SuffixJr et al. (1990) ArticleTitleEffect of the right ventricular anatomy on the cardiopulmonary response to exercise: implications for the Fontan procedure Circulation 81 1881–1887 Occurrence Handle2344681
VK Somers AL Mark FM Abboud (1991) ArticleTitleInteraction of baroreceptor and chemoreceptor reflex control of sympathetic nerve activity in normal humans J Clin Invest 87 1953–1957 Occurrence Handle1:CAS:528:DyaK3MXksVKkuro%3D Occurrence Handle2040688
SA Ward BJ Whipp S Koyal K Wasserman (1983) ArticleTitleInfluence of body CO2 stores on ventilatory dynamics during exercise J Appl Physiol 55 742–749 Occurrence Handle1:STN:280:BiuD3s7osVU%3D Occurrence Handle6415010
K Wasserman BJ Whipp SN Koyal WL Beaver (1973) ArticleTitleAnaerobic threshold and respiratory gas exchange during exercise J Appl Physiol 35 236–243 Occurrence Handle1:CAS:528:DyaE3sXkslKmt7o%3D Occurrence Handle4723033
K Wasserman YY Zhang A Gitt et al. (1997) ArticleTitleLung function and exercise gas exchange in chronic heart failure Circulation 96 2221–2227 Occurrence Handle1:STN:280:ByiH2sjhtlQ%3D Occurrence Handle9337193
Acknowledgements
We are grateful to Drs. P. M. Olley and S. Olley for assistance in preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohuchi, H., Ohashi, H., Takasugi, H. et al. Restrictive Ventilatory Impairment and Arterial Oxygenation Characterize Rest and Exercise Ventilation in Patients After Fontan Operation. Pediatr Cardiol 25, 513–521 (2004). https://doi.org/10.1007/s00246-003-0652-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-003-0652-7