Abstract
The overall prevalence of kidney stones (KS) in the US rose from 3.2% in 1980 to 10.1% in 2016, but the trends in important subgroups have not been reported. We examined the prevalence trends of KS in subgroups of age, sex and race in the US and identified relevant laboratory factors associated with a history of KS using National Health and Nutrition Examination Survey (NHANES) data. We conducted a cross-sectional study among 28,209 US adults aged ≥ 20 years old in the NHANES from 2007 to 2016. We calculated the prevalence of a self-reported history of KS by using weights and standardized to the 2010 US Census population. We also compared relevant laboratory values according to the history of KS. The prevalence of KS decreased from 8.7% in 2007–2008 to 7.2% in 2011–2012 but then increased to 9.0% in 2013–2014 and 10.1% in 2015–2016. However, the overall prevalence of KS increased over 2007–2016 (p-trend = 0.02). Prevalence of KS among men was higher than women. Among men aged 20–79, there were significant quadratic trends in the prevalence of KS. Whereas, the prevalence of KS increased as a linear trend among women aged 20–59 years over 2007–2016. There were no consistent trends in the prevalence of KS by race. The prevalence trend of KS among non-Hispanic whites was 9.8% from 2007 to 2010 then dropped to 7.9% in 2011–2012 and increased to 10.6% in 2013–2014 and 12.1% in 2015–2016. A similar trend was also observed among non-Hispanic blacks. Among Hispanic, the prevalence of KS was 7.6% in 2007–2008 and 7.4% in 2009–2010 and then fluctuated over the next several time periods. For non-Hispanic Asians, the range was 4.4–4.6%. Regarding relevant laboratory factors, after adjusting for sex, race, age, BMI, smoking status, alcohol drinking, history of diabetes and gout, urine albumin-creatinine ratio and serum osmolality were independently associated with the history of KS in women and men. In conclusion, there was substantial variability in KS prevalence across individual 2-year time periods. This variation of period-specific prevalence values emphasizes the importance of looking at long-term trends and using more than a single 2-year cycle in analyses to increase the precision of the estimate. However, there was an overall increase in the prevalence of KS over 2007-2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney stones (KS) are common in the US and cost billions of dollars due to treatment and lost worker productivity [1]. Moreover, KS cause pain and hematuria and have been associated with chronic kidney disease (CKD) [2, 3], end-stage kidney disease (ESKD) [4, 5], osteoporosis [6, 7] and cardiovascular disease [8, 9]. A study based on National Health and Nutrition Examination Survey (NHANES) data reported that the overall prevalence of kidney stones has continued to rise from 3.2% in 1980 to 10.1% in 2014 [10]. Possible explanations for this growing trend include the obesity epidemic, higher prevalences of gout and diabetes, and poor diet [11, 12]. However, updated information is needed on the prevalence trends of KS across age, sex and race groups.
We examined the prevalence trends of KS in subgroups of age, sex, and race in the US. Additionally, we identified laboratory factors associated with a history of KS using National Health and Nutrition Examination Survey (NHANES) data from 2007 to 2016.
Methods
Data sources
NHANES is an ongoing evaluation of the health and nutritional status of children and adults in the United States. The survey includes interviews, physical examinations and laboratory measurements. All public-use de-identified data sets in NHANES were exempted from the requirement for institutional review board approval.
Study population
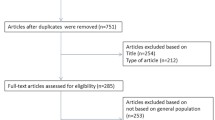
We conducted a serial cross-sectional study in the NHANES from 2007 to 2016. The population included 28,209 US males and females aged ≥ 20 years old who responded to the questions regarding a history of kidney stones contained in the household survey component.
Outcomes
The primary outcome was the prevalence of a self-reported history of KS from the response to the question, “Have you ever had kidney stones?”. However, given that some KS may be incidental findings on imaging performed for another indication, the secondary outcome was the prevalence of a history of symptomatic stone disease based on the response to the question, “How many times have you passed a kidney stone?”
Covariates
Covariates of interest included age, sex, race, ethnicity, cigarette smoking status, alcohol consumption, history of diabetes and history of gout. Participants were divided into four age groups: 20–39, 40–59, 60–79 and over 80 years old. Ethnicity/race categories included non-Hispanic white, non-Hispanic black, non-Hispanic Asian (data are available after 2011 NHANES cycle), Hispanic (Mexican–American and other Hispanic), and other race/multiracial. BMI was categorized as < 18.5, 18.5–24.9, 25–29.9 and ≥ 30 kg/m2. Cigarette smoking status was categorized as never, past and current smokers. Alcohol consumption was divided into 5 groups: life-long abstainer, former drinker, current drinker reporting ≤ 1 drink/week, 1–14 drinks/week and more than 14 drinks/week. We defined diabetic individuals as those answering “yes” to the question “Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” or having a hemoglobin A1C (HbA1C) more than 6.5%. Individuals with a history of gout were defined as those who answered “yes” to the question “Has a doctor or other health professional ever told you that you had gout?”
Statistical analysis
We calculated the prevalence of a self-reported history of KS and the prevalence of self-reported passing at least one stone (symptomatic stone disease) by incorporating survey weights and design factors in all estimations to account for the unequal probabilities of selection, oversampling, and nonresponse. All estimates were standardized to the 2010 US Census population, using age adjustment [13]. Linear and quadratic trends overall and stratified by sex, age, diabetes, history of gout, alcohol consumption and cigarette smoking status were examined in regression models with 2-year survey cycles modeled as an orthogonal polynomial. We summarized characteristics and compared some relevant laboratory factors between individuals with the history of KS and without the history of KS after adjusting for age. Due to a skewed distribution, urine albumin-creatinine ratio, urine flow rate and serum copper were log-transformed. The mean values of these log-transformed variables were calculated for each group and these means were back-transformed exponentially to represent geometric means. Moreover, we categorized serum 25-OH vitamin D (25(OH)D) into three categories including vitamin D deficiency defined as 25(OH)D < 50 nmol/l, vitamin D insufficiency defined as 50 ≤ 25(OH)D < 75 nmol/l and replete vitamin D defined as 25(OH)D ≥ 75 nmol/l [14].
Additionally, we used multivariable logistic regression accounting for the survey weights to evaluate the association between relevant laboratory values and self-reported history of KS. We adjusted in the multivariable model for potential confounders specified a priori, including age, sex, race, BMI, cigarette smoking status, alcohol consumption, history of diabetes and history of gout. Given that some laboratory values are not available in all NHANES cycles, we created four models additionally adjusted for other laboratory values to evaluate whether that particular laboratory value was independently associated with the history of KS based on the availability of the data in each NHANES cycle. Model 1 was using data from NHANES cycle 2007–2014 since the data for 25(OH)D are available from only 2007–2014. In model 2, we added serum trace elements as predictors using data from NHANES cycle 2011–2014 since the data for 25(OH)D along with serum trace elements are available only from 2011 to 2014. For model 3 adding serum estrogen, we used data from NHANES cycle 2013–2014 among women since serum estrogen along with other laboratory parameters are available only in 2013–2014. For model 4 adding serum testosterone, we used data from NHANES cycle 2011–2014 among men given that serum testosterone and other laboratory parameters are available only from 2011 to 2014.
All statistical analyses were conducted using STATA 15.1 (StataCorp LLC, Texas, USA). Results were considered statistically significant with two-sided α < 0.05 unless otherwise specified.
Results
Among 28,209 individuals in NHANES who responded to the kidney stone question, the weighted and age-standardized overall prevalence of KS from 2007 to 2016 was 9.3% (95% CI 8.8–9.8). Men were more likely to report a history of KS (10.6% [95% CI 9.9–11.3]) than women (8.1% [95% CI 7.3–8.8]). The prevalence of KS fluctuated during these years initially decreasing from 8.7% (95% CI 7.7–9.8) in 2007–2008 to 8.6% (95% CI 7.9–9.2) in 2009–2010 and 7.2% (95% CI 6.0–8.5) in 2011–2012 and then increased to 9.0% (95% CI 7.9–10.0) in 2013–2014 and 10.1% (95% CI 8.9–11.4) in 2015–2016. However, there was a significant overall increase in a quadratic trend (p-trend = 0.02) in the prevalence of kidney stones from 2007 to 2016. There was no significant trend for the secondary outcome of symptomatic KS (Table 1).
The prevalence of KS among men fluctuated during 2007–2016 initially decreasing from 11.8% (95% CI 9.8–13.8) in 2007–2008 to 10.2% (95% CI 8.8–11.6) in 2009–2010 and 7.8% (95% CI 6.0–9.3) in 2011–2012 and then increased to 10.5% (95% CI 9.3–11.8) in 2013–2014 and 13.0% (95% CI 11.5–14.6) in 2015–2016 (p for quadratic trend < 0.001). Overall, the prevalence of KS in men increased with age. The highest prevalence was found among male individuals with age ≥ 80 years which was 19.7% (95% CI 16.9–22.5) followed by age of 60-79 which was 18.8% (95% CI 16.8–20.7), age of 40–59 which was 11.5% (95% CI 10.1–12.9) and age of 20–39 which was 5.1% (95% CI 4.3–6.0). Among women, the prevalence of KS increased from 6.0% (95% CI 4.9–7.0) in 2007–2008 to 7.3% (95% CI 6.3–8.4) in 2009–2010 and 8.0% (95% CI 5.8–10.3) in 2011–2012 and then increased to 9.4% (95% CI 7.6–11.3) in 2013–2014 and 9.8% (95% CI 7.7–11.8) in 2015–2016 with an overall increasing linear trend (p-trend < 0.001). Supplementary Table 1. The prevalence of KS in women was similar among those aged ≥ 80 which was 10.6% (95% CI 8.1–13.0), aged 60–79 which was 9.2% (95% CI 7.9–10.5) and aged 40–59 which was 9.8% (95% CI 8.5–11.1). However, the prevalence of KS among women aged 20–39 years was only 5.8% (95% CI 4.9–6.6). Moreover, the prevalence of KS among women was lower than men except at age 20–39 years.
Among men across the ages of 20–79, there were significant quadratic trends from 2007 to 2016 as prevalence trends of KS initially decreased from 2007 to 2008 to the nadir in 2011–2012 then increased again in 2015–2016. However, for men aged ≥ 80 years, the prevalence varied substantially during the study period with no statistically significant trend. The prevalence initially decreased from 21.5% (95% CI 13.33–29.7) in 2007-2008 to 14.5% (95% CI 8.9–20.2) in 2009–2010 then increased to 23.8% (95% CI 15.3–32.3) in 2011–2012 but decreased to 16.6% (95% CI 11.8–21.5) in 2013–2014 then increased again to 22.1% (95% CI 16.1–28.1). Among women aged 20–79 years, the prevalence of KS gradually increased from 2007–2008 to 2015–2016. However, linear trends were significant only among women aged 20–59 years. In women aged ≥ 80 years, the prevalence of KS also varied substantially as evidenced by no statistically significant trend (Table 2, Fig. 1a, b). A quadratic trend for a secondary outcome of symptomatic KS was seen among men aged 40–59 years while an increasing linear trend for symptomatic KS was seen among women aged 20–39 years (Table 3, Fig. 1c, d).
a Weighted prevalence of kidney stone by age among male from 2007 to 2016. b Weighted prevalence of kidney stone by age among female from 2007 to 2016. c Weighted prevalence of symptomatic kidney stone by age among male from 2007 to 2016. d Weighted prevalence of symptomatic kidney stone by age among female from 2007 to 2016
Among different races, non-Hispanic whites had the highest prevalence of KS at 9.9% (95% CI 8.9–10.9) followed by Hispanic which was 8.3% (95% CI 7.4–9.3), non-Hispanic blacks which was 4.9% (95% CI 4.3–5.5) and non-Hispanic Asians which had the lowest prevalence of KS at 4.4% (95% CI 3.4–5.3). However, the prevalence of KS among non-Hispanic Asians and non-Hispanic blacks was not significantly different. For non-Hispanic whites, the prevalence of KS was stable at 9.8% (95% CI 8.4–11.3 in 2007–2008 and 8.8–10.9 in 2009–2010) from 2007 to 2010 then declined to 7.9% (95% CI 5.7–10.0) in 2011–2012 but then increased to 10.6% (95% CI 9.2–12.0) in 2013–2014 and 12.1% (95% CI 10.0–14.2) in 2015–2016. Regarding Hispanic, the prevalence of KS was stable at 7.6% (95% CI 6.1–9.1) in 2007–2008 and 7.4% (95% CI 6.1–8.8) in 2009–2010 and then fluctuated over the next several time periods. The prevalence of KS among non-Hispanic blacks also slightly fluctuated. For non-Hispanic Asians, the prevalence of KS was stable at 4.4–4.6% from 2011 to 2016 (Table 4 and Fig. 2a). There were no significant trends for the prevalence of KS across any race. Similar findings were seen in the secondary outcome of symptomatic KS (Table 5 and Fig. 2b).
The prevalence of KS among diabetic participants was higher than those without diabetes (13.1% vs 8.0%; p < 0.001) and the prevalence of KS among participants with the history of gout was higher than those without a history of gout (16.6% vs 8.5%; p < 0.001). In terms of cigarette smoking status, the prevalence of KS among past smokers and current smokers were higher than never smokers. For alcohol consumption, the prevalence of KS among former drinkers was higher than life-long abstainers while the prevalence of KS among participants who drank more than 1 drink/week was lower than life-long abstainers. Overall from 2007 to 2016, there were no significant trends for the prevalence of KS across either history of diabetes, history of gout, smoking or alcohol drinking status (Supplementary Table 3). The age-standardized laboratory values among stone formers and non-stone formers are shown in Table 6. Although statistically significant, individuals with a history of KS had no clinically significant differences in mean serum creatinine (0.88 vs 0.86 mg/dl; p = 0.01) or estimated glomerular filtration rate (eGFR) (95.4 vs 96.5 ml/min/1.73 m2; p = 0.01), serum phosphate (3.7 vs 3.8 mg/dl; p = 0.0001), serum chloride (104.1 vs 103.8 mmol/l; p = 0.001), serum bicarbonate (24.6 vs 25.0 mmol/l; p < 0.0001) and serum osmolality (278.2 vs 277.9 mmol/kg; p = 0.004). Individuals with a history of KS had slightly higher albumin-creatinine ratio (8.7 vs 7.8 mg/g; p = 0.0001) and a slightly lower urine flow rate (0.8 vs 0.9 ml/min; p = 0.02). While many laboratory values were statistically different, the only ones that were clinically different were serum estrogen which was lower among female stone formers (74.5 vs 108.5 pg/ml; p = 0.003) and serum testosterone which was lower among male stone formers (393.5 vs 416.4 ng/dl; p = 0.02).
In multivariate analyses, we adjusted for age, sex, race, BMI category, history of DM, gout, smoking status and alcohol drinking in every model. In model 1 including available laboratory data of eGFR, log urine flow rate, log albumin-creatinine ratio, serum osmolality, serum calcium, phosphate, 25(OH)D categories from NHANES cycle 2007–2014, we found that higher log urine albumin-creatinine ratio and serum osmolality were independently associated with higher odds of history of KS. In model 2 after adding serum trace elements, we found independently association between higher serum copper and lower odds of history of KS among men (OR = 0.85 [95% CI 0.77–0.95] per 10 μg/L) but not women (OR = 1.01 [95% CI 0.91–1.11] per 10 μg/L) (p interaction = 0.02). After adding serum estrogen and trace elements, none of the laboratory values were associated with a history of KS among women (model 3). However, in model 4, after adding serum testosterone and serum trace elements, higher serum copper was independently associated with lower odds of history of KS among men (Table 7).
Discussion
The prevalence of KS, defined as a history of KS, has continued to rise over the past three decades in the US from 3.2% in 1980 [15] to 5.2% in 1994 [15, 16], 8.8% in 2010 [17] and 10.1% in 2016. However, the NHANES data for the decade 2007–2016, demonstrates substantial variability over many 2-year cycles. For example, the prevalence of KS in the US decreased from 2007 to 2010 but then increased after 2011. This is most likely due to random variability as it is very unlikely that there were abrupt changes in the true population prevalence over such a short period of time. It is also unlikely that increasing use and sensitivity of imaging studies led to an increase in incidental findings since we observed similar trends of prevalence for symptomatic KS. However, we found an overall increase in the quadratic trend of the prevalence of KS from 2007 to 2016.
Previous literature using NHANES for chronic diseases such as the study by Yoon et al. [18] of trends in blood pressure among adults with hypertension, the study by Hales et al. [19] of trends in obesity and severe obesity prevalence in US youth and adults, the study by Palmer et al. [20] of trends in diabetes as well as the study by Chen-Xu et al. [21] of the trends in gout and hyperuricemia also demonstrated variability in prevalence between 2-year cycles as we observed for kidney stones. This emphasizes the importance of examining long-term trends. From 2007 to 2016, our study observed an overall increase in the trend of the prevalence of KS. However, after stratified by diabetes and a history of gout, we did not find any significant trends in the prevalence of KS. These findings suggested that the increase in trend of the prevalence of KS might be explained in part by the increasing prevalence of diabetes [19] and diabetes is associated with a higher risk of KS. The prevalence of KS varied by age and sex. On average, among women aged 20–79 years, the prevalence of KS was increasing since 2007. We observed a quadratic trend for the prevalence trend of KS among men aged 20–79 with the nadir in 2011–2012. Nonetheless, for both men and women aged ≥ 80 years, the variability from cycle to cycle was larger than other age ranges as we observed the substantial fluctuating prevalence from 2007 to 2016. Moreover, we noticed larger confidence intervals among men and women aged ≥ 80 years, likely explained by smaller sample size in this age group. Furthermore, we also found that the prevalence of KS among women was higher than men at age 20–39 years. We postulated that this reproductive age group was the time when most of the pregnancies occurred. As pregnancy is the risk of KS [22], it might be the reason for the higher prevalence of KS among women compared to men in this age group.
Regarding race/ethnicity, the overall prevalence was lowest among non-Hispanic Asians, followed by non-Hispanic blacks, Hispanic and non-Hispanic whites, respectively. For the prevalence of symptomatic KS, the lowest prevalence was found among non-Hispanic blacks. However, there was no significant difference between non-Hispanic blacks and non-Hispanic Asians. These findings across all races including Asians were consistent with the previous nationwide study using data from the Cancer Prevention Survey (CPS II). The lower prevalence of kidney stones among non-Hispanic blacks than non-Hispanic whites might be explained by the lower urinary calcium excretion leading to a lower relative urinary supersaturation of calcium salts [23]. Although there appeared to be an increase in the prevalence of kidney stone among non-Hispanic blacks, it was not statistically significant. The increasing prevalence trend might be explained by the lower vegetable intake among non-Hispanic blacks [24]. Future studies should focus on 24-h urinary chemistries and dietary intake among Asians to better understand the lower prevalence in this group.
Risk factors for stone formation include family history of KS, renal tubular acidosis (RTA) [25], inflammatory bowel disease (IBD) [26], sarcoidosis [27], obesity, diabetes [28], metabolic syndrome [29] and urine risk factors including urine oxalate, urine calcium and urine citrate [30,31,32]. The increasing trends in the prevalence of IBD [33], obesity [19], diabetes [34], and metabolic syndrome [35] over time might increase in affecting the rate of kidney stones. However, regarding laboratory risk factors, there are limited data from the previous literature. Our study investigated the association between sex hormones and the risk of KS. Interestingly, we found that serum testosterone among male stone formers was lower than non-stone formers in contrast with the previous purported belief that testosterone may promote calcium oxalate stone formation. Testosterone enhances the activity of hepatic glycolic acid oxidase, suppresses osteopontin in the kidney and increases urinary oxalate excretion [36,37,38]. Nonetheless, more recent studies reported low serum testosterone levels in men were associated with a higher risk of KS [39, 40]. Potential explanations for these findings are obesity and metabolic syndrome including diabetes and hypertension, which confound the association between low serum testosterone and risk of KS. Metabolic syndrome and obesity are strongly associated with a higher risk of kidney stones [29] and are associated with lower testosterone levels [41, 42]. Obesity and metabolic syndrome including insulin resistance increase inflammatory cytokine leading to a suppression of testosterone production [43] as well as precipitating kidney stone formation through the expression of monocyte chemoattractant protein 1, osteopontin and macrophage infiltration [44]. Similarly, for estrogen, we observed lower mean serum estrogen among female stone formers compared to non-stone formers. Estrogen has anti-lithogenic effects: it inhibits bone resorption and increases calcium absorption in the distal tubule, and increases urine citrate excretion [45,46,47]. Nevertheless, we did not find a significant association between serum estrogen and KS. Thus, the multivariable-adjusted model demonstrated that the differences in testosterone and estrogen levels by KS status could be explained by other factors. Future studies should explore these complex interactions between estrogen and testosterone and risk of KS along with assessing 24-h urine chemistry.
After multivariable adjustment, higher albumin-creatinine ratio and serum osmolality in model 1 were independently associated with higher odds of history of KS. Having a history of KS might increase the risk of CKD and proteinuria [48]. Additionally, higher serum osmolality was associated with higher odds of history of KS. The most likely explanation is lower fluid consumption, one of the strongest risk factors for stone formation [49, 50]. However, these findings were not significant in either model 2, 3 or 4 possibly due to confounding by serum trace elements and sex hormones on urine albumin-creatinine ratio and serum osmolality. Furthermore, using data from NHANES cycle 2011–2014, we unexpectedly found that higher serum copper was independently associated with lower odds of history of KS among men but not women, and the interaction of serum copper and sex was statistically significant. Some studies postulated that copper might have a modest inhibitory effect on calcium phosphate crystallization [51, 52]. However, lithogenic effects of copper still remain unclear since a study by Ferraro et al. [53] revealed that higher total intake of copper was associated with a higher risk of KS; however, this association was significant only among women. Furthermore, serum copper was no longer associated with lower odds of history of KS after Bonferroni adjustment (Bonferroni p-value = 0.06).
Regarding vitamin D, there was no significant difference in serum 25(OH)D level between stone formers and non-stone formers in our study. A previous study from the UK reported that ~ 30% of stone formers had vitamin D deficiency while only 18% of stone formers had vitamin D deficiency in our study. However, it is difficult to compare across studies since the distributions of ethnicity, dietary patterns, geographic location, seasonal variation and the technique of vitamin D measurement might be different. Moreover, in our study, it appears that replete vitamin D, defined as serum 25(OH)D level ≥ 75 nmol/l, was not significantly associated with odds of KS. It is uncertain whether vitamin D supplementation, especially among individuals with vitamin D deficiency, would increase the risk of KS. Previous studies did not show a significant risk of KS even though there was a non-significant rise in 24-h urine calcium excretion [54]. Furthermore, a study by Ferraro et al. did not find a significant association between vitamin D intake in typical amounts and risk of KS. The relationship between vitamin D intake, circulating level of 25(OH)D and risk of kidney stones is complex as the active metabolite 1,25(OH)2D, a pivotal factor of calcium stone formation is tightly regulated by the activity of 1-alpha-hydroxylase enzyme and PTH axis [55,56,57].
Prior studies by Scales et al. [17] focused on responses to the 2007–2010 NHANES and Chen et al. [10] performed analysis using data from 2007 to 2014. While these studies examined overall trends over periods of time, neither one reported statistical tests for the time trends across age, sex and races. Our study updated the prevalence of KS with the newest available data in NHANES and age-standardized to 2010 US Census to compare populations at more than two-time points and to remove the impact of different age distributions. Additionally, we also examined risk factors of kidney stones based upon various laboratory chemistries including sex hormones and trace elements. Compared to previous studies using different cohorts by Tasian et al. [58] based on South Carolina Medical Encounter data and Kittanamongkolchai et al. [59] based on Rochester Epidemiology Project data results from all studies including our study demonstrated the overall increasing rates of KS. There was a significant increasing rate of KS among female. This increase in the rate of KS parallels with the increase in female obesity in the US [19, 60]. However, the change in rates of KS among male was not consistent across studies. Our results did not show a significant change in the linear trend of the rate of KS consistent with the study by Tasian et al. that reported a relatively stable rate of KS among men but in contrast to the study by Kittanamongkolchai et al. that showed a significant increase in KS rate in men. In terms of race, although there were increasing rates of KS among non-Hispanic whites and blacks, these trends were not statistically significant in our study. Similarly, the study by Tasian et al. pointed out that the rates of kidney stones were increasing in whites and blacks. However, they found that the change in the rate of KS was greater among blacks.
Limitations include the cross-sectional study design of NHANES. Hence, the temporal relationship between KS and laboratory values cannot be determined. We could only estimate the associations but not causal effects. In addition, since NHANES data are self -reported, response to kidney stone questions in the survey might not be as accurate as coded data. Validation of a history of kidney stone might be needed. However, a recent population-based study in Olmsted County, Minnesota identified participants based upon ICD-9 codes and manual chart review. This study also found the rate of kidney stones had been increasing from 1984 to 2012, especially among men and women aged 18-60 years old [59]. Finally, NHANES did not have information on some bone-mineral markers and no 24-hour urine data.
In conclusion, there was substantial variability in the prevalence of KS during individual 2-year time periods. However, there was an overall increase in prevalence of KS over 2007-2016. Future analyses of NHANES data on kidney stones as well as other chronic conditions should keep this variability in mind before drawing conclusions about abrupt changes in prevalence. The variability of period-specific prevalence values emphasizes the importance of examining long-term trends using more than a single 2-year cycle in analyses to increase the precision of the estimate.
References
Hyams ES, Matlaga BR (2014) Economic impact of urinary stones. Transl Androl Urol 3(3):278–283. https://doi.org/10.3978/j.issn.2223-4683.2014.07.02
Rule AD, Krambeck AE, Lieske JC (2011) Chronic kidney disease in kidney stone formers. Clin J Am Soc Nephrol 6(8):2069–2075. https://doi.org/10.2215/CJN.10651110
Li C-C, Chien T-M, Wu W-J, Huang C-N, Chou Y-H (2018) Uric acid stones increase the risk of chronic kidney disease. Urolithiasis 46(6):543–547. https://doi.org/10.1007/s00240-018-1050-1
Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Morgan C, Samuel S, Klarenbach SW, Curhan GC, Tonelli M (2012) Kidney stones and kidney function loss: a cohort study. BMJ (Clin Res Ed) 345:e5287. https://doi.org/10.1136/bmj.e5287
El-Zoghby ZM, Lieske JC, Foley RN, Bergstralh EJ, Li X, Melton LJ 3rd, Krambeck AE, Rule AD (2012) Urolithiasis and the risk of ESRD. Clin J Am Soc Nephrol 7(9):1409–1415. https://doi.org/10.2215/CJN.03210312
Taylor EN, Feskanich D, Paik JM, Curhan GC (2016) Nephrolithiasis and risk of incident bone fracture. J Urol 195(5):1482–1486. https://doi.org/10.1016/j.juro.2015.12.069
Lu YM, Chien TM, Li CC, Chou YH, Wu WJ, Huang CN (2018) Urolithiasis is associated with the increased risk for osteoporosis: a nationwide 9-year follow-up study. Urol Sci 29(3):145–150. https://doi.org/10.4103/UROS.UROS_20_17
Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Samuel S, Klarenbach SW, Curhan GC, Tonelli M (2014) Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol 9(3):506–512. https://doi.org/10.2215/cjn.04960513
Cheungpasitporn W, Thongprayoon C, Mao MA, O’Corragain OA, Edmonds PJ, Erickson SB (2014) The risk of coronary heart disease in patients with kidney stones: a systematic review and meta-analysis. N Am J Med Sci 6(11):580–585. https://doi.org/10.4103/1947-2714.145477
Chen Z, Prosperi M, Bird VY (2018) Prevalence of kidney stones in the USA: the national health and nutrition evaluation survey. J Clin Urol. https://doi.org/10.1177/2051415818813820
Alelign T, Petros B (2018) Kidney stone disease: an update on current concepts. Adv Urol 2018:3068365. https://doi.org/10.1155/2018/3068365
Romero V, Akpinar H, Assimos DG (2010) Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol 12(2–3):e86–e96
Howden L, Meyer J (2011) Age and Sex Composition:2010 2010 Census Briefs. U.S. Department of Commerce, United States Census Bureau
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930. https://doi.org/10.1210/jc.2011-0385
Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC (2003) Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int 63(5):1817–1823. https://doi.org/10.1046/j.1523-1755.2003.00917.x
Antonelli JA, Maalouf NM, Pearle MS, Lotan Y (2014) Use of the National Health and Nutrition Examination Survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur Urol 66(4):724–729. https://doi.org/10.1016/j.eururo.2014.06.036
Scales CD Jr, Smith AC, Hanley JM, Saigal CS, Urologic Diseases in America P (2012) Prevalence of kidney stones in the United States. Eur Urol 62(1):160–165. https://doi.org/10.1016/j.eururo.2012.03.052
Yoon Sung S, Gu Q, Nwankwo T, Wright Jacqueline D, Hong Y, Burt V (2015) Trends in blood pressure among adults with hypertension. Hypertension 65(1):54–61. https://doi.org/10.1161/HYPERTENSIONAHA.114.04012
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL (2018) Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA 319(16):1723–1725. https://doi.org/10.1001/jama.2018.3060
Palmer MK, Toth PP (2019) Trends in lipids, obesity, metabolic syndrome, and diabetes mellitus in the United States: an NHANES analysis (2003-2004 to 2013-2014). Obesity 27(2):309–314. https://doi.org/10.1002/oby.22370
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK (2019) Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the National Health and Nutrition Examination Survey, 2007–2016. Arthr Rheumatol 71(6):991–999. https://doi.org/10.1002/art.40807
Reinstatler L, Khaleel S, Pais VM Jr (2017) Association of pregnancy with stone formation among women in the United States: a NHANES Analysis 2007 to 2012. J Urol 198(2):389–393. https://doi.org/10.1016/j.juro.2017.02.3233
Taylor EN, Curhan GC (2007) Differences in 24-Hour urine composition between black and white women. J Am Soc Nephrol 18(2):654–659. https://doi.org/10.1681/asn.2006080854
Talati JJ, Haroon N, Trinchieri A (2012) Renal stone disease in different racial groups. In: Talati JJ, Tiselius H-G, Albala DM, Ye Z (eds) Urolithiasis: basic science and clinical practice. Springer, London, pp 107–110. https://doi.org/10.1007/978-1-4471-4387-1_14
Buckalew VM Jr (1989) Nephrolithiasis in renal tubular acidosis. J Urol 141(3 Pt 2):731–737
Parks JH, Worcester EM, O’Connor RC, Coe FL (2003) Urine stone risk factors in nephrolithiasis patients with and without bowel disease. Kidney Int 63(1):255–265. https://doi.org/10.1046/j.1523-1755.2003.00725.x
Rodman JS, Mahler RJ (2000) Kidney stones as a manifestation of hypercalcemic disorders. Hyperparathyroidism and sarcoidosis. Urol Clin North Am 27(2):275–285
Taylor EN, Stampfer MJ, Curhan GC (2005) Diabetes mellitus and the risk of nephrolithiasis. Kidney Int 68(3):1230–1235. https://doi.org/10.1111/j.1523-1755.2005.00516.x
Taylor EN, Stampfer MJ, Curhan GC (2005) Obesity, weight gain, and the risk of kidney stones. JAMA 293(4):455–462. https://doi.org/10.1001/jama.293.4.455
Curhan GC, Willett WC, Speizer FE, Stampfer MJ (2001) Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int 59(6):2290–2298. https://doi.org/10.1046/j.1523-1755.2001.00746.x
Taylor EN, Curhan GC (2007) Oxalate Intake and the risk for nephrolithiasis. J Am Soc Nephrol 18(7):2198. https://doi.org/10.1681/ASN.2007020219
Mandel EI, Taylor EN, Curhan GC (2013) Dietary and lifestyle factors and medical conditions associated with urinary citrate excretion. Clin J Am Soc Nephrol 8(6):901. https://doi.org/10.2215/CJN.07190712
Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB (2016) Prevalence of inflammatory bowel disease among adults aged ≥ 18 years — United States. MMWR Morb Mortal Wkly Rep 65:1166–1169
Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S (2017) Diabetes 2030: insights from yesterday, today, and future trends. Popul Health Manag 20(1):6–12. https://doi.org/10.1089/pop.2015.0181
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ (2015) Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA 313(19):1973–1974. https://doi.org/10.1001/jama.2015.4260
Yagisawa T, Ito F, Osaka Y, Amano H, Kobayashi C, Toma H (2001) The influence of sex hormones on renal osteopontin expression and urinary constituents in experimental urolithiasis. J Urol 166(3):1078–1082
Soundararajan P, Mahesh R, Ramesh T, Begum VH (2006) Effect of Aerva lanata on calcium oxalate urolithiasis in rats. Indian J Exp Biol 44(12):981–986
Fan J, Chandhoke PS, Grampsas SA (1999) Role of sex hormones in experimental calcium oxalate nephrolithiasis. J Am Soc Nephrol 10(Suppl 14):S376–S380
Otunctemur A, Ozbek E, Cakir SS, Dursun M, Polat EC, Ozcan L, Besiroglu H (2015) Urolithiasis is associated with low serum testosterone levels in men. Arch Ital Urol Androl 87(1):83–86. https://doi.org/10.4081/aiua.2015.1.83
Polat EC, Ozcan L, Otunctemur A, Ozbek E (2016) Relation of urinary stone disease with androgenetic alopecia and serum testosterone levels. Urolithiasis 44(5):409–413. https://doi.org/10.1007/s00240-016-0888-3
Wang C, Jackson G, Jones TH, Matsumoto AM, Nehra A, Perelman MA, Swerdloff RS, Traish A, Zitzmann M, Cunningham G (2011) Low testosterone associated with obesity and the metabolic syndrome contributes to sexual dysfunction and cardiovascular disease risk in men with type 2 diabetes. Diabetes Care 34(7):1669–1675. https://doi.org/10.2337/dc10-2339
Tajar A, Forti G, O’Neill TW, Lee DM, Silman AJ, Finn JD, Bartfai G, Boonen S, Casanueva FF, Giwercman A, Han TS, Kula K, Labrie F, Lean ME, Pendleton N, Punab M, Vanderschueren D, Huhtaniemi IT, Wu FC (2010) Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European Male Ageing Study. J Clin Endocrinol Metab 95(4):1810–1818. https://doi.org/10.1210/jc.2009-1796
Salam R, Kshetrimayum AS, Keisam R (2012) Testosterone and metabolic syndrome: The link. Indian J Endocrinol Metab 16:S12–S19. https://doi.org/10.4103/2230-8210.94248
Kohjimoto Y, Sasaki Y, Iguchi M, Matsumura N, Inagaki T, Hara I (2013) Association of metabolic syndrome traits and severity of kidney stones: results from a Nationwide Survey on urolithiasis in Japan. Am J Kidney Dis 61(6):923–929. https://doi.org/10.1053/j.ajkd.2012.12.028
Heller HJ, Sakhaee K, Moe OW, Pak CY (2002) Etiological role of estrogen status in renal stone formation. J Urol 168(5):1923–1927. https://doi.org/10.1097/01.ju.0000033907.21910.be
Zhao Z, Mai Z, Ou L, Duan X, Zeng G (2013) Serum estradiol and testosterone levels in kidney stones disease with and without calcium oxalate components in naturally postmenopausal women. PLoS ONE 8(9):e75513. https://doi.org/10.1371/journal.pone.0075513
Wilson C (2011) Estrogen and kidney stones. Nat Rev Endocrinol 7(1):3. https://doi.org/10.1038/nrendo.2010.206
Haley WE, Enders FT, Vaughan LE, Mehta RA, Thoman ME, Vrtiska TJ, Krambeck AE, Lieske JC, Rule AD (2016) Kidney function after the first kidney stone event. Mayo Clin Proc 91(12):1744–1752. https://doi.org/10.1016/j.mayocp.2016.08.014
Curhan GC, Taylor EN (2008) 24-h uric acid excretion and the risk of kidney stones. Kidney Int 73(4):489–496. https://doi.org/10.1038/sj.ki.5002708
Taylor EN, Curhan GC (2006) Diet and fluid prescription in stone disease. Kidney Int 70(5):835–839. https://doi.org/10.1038/sj.ki.5001656
Komleh K, Hada P, Pendse AK, Singh PP (1990) Zine, copper and manganese in serum, urine and stones. Int Urol Nephrol 22(2):113–118. https://doi.org/10.1007/BF02549826
Meyer JL, Angino EE (1977) The role of trace metals in calcium urolithiasis. Invest Urol 14(5):347–350
Ferraro PM, Gambaro G, Curhan GC, Taylor EN (2018) Intake of trace metals and the risk of incident kidney stones. J Urol 199(6):1534–1539. https://doi.org/10.1016/j.juro.2018.01.077
Johri N, Jaeger P, Ferraro PM, Shavit L, Nair D, Robertson WG, Gambaro G, Unwin RJ (2017) Vitamin D deficiency is prevalent among idiopathic stone formers, but does correction pose any risk? Urolithiasis 45(6):535–543. https://doi.org/10.1007/s00240-016-0954-x
Ferraro PM, Taylor EN, Gambaro G, Curhan GC (2017) Vitamin D intake and the risk of incident kidney stones. J Urol 197(2):405–410. https://doi.org/10.1016/j.juro.2016.08.084
Taylor EN, Hoofnagle AN, Curhan GC (2015) Calcium and phosphorus regulatory hormones and risk of incident symptomatic kidney stones. Clin J Am Soc Nephrol 10(4):667–675. https://doi.org/10.2215/cjn.07060714
Letavernier E, Daudon M (2018) Vitamin D, hypercalciuria and kidney stones. Nutrients 10(3):366. https://doi.org/10.3390/nu10030366
Tasian GE, Ross ME, Song L, Sas DJ, Keren R, Denburg MR, Chu DI, Copelovitch L, Saigal CS, Furth SL (2016) Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol 11(3):488. https://doi.org/10.2215/CJN.07610715
Kittanamongkolchai W, Vaughan LE, Enders FT, Dhondup T, Mehta RA, Krambeck AE, McCollough CH, Vrtiska TJ, Lieske JC, Rule AD (2018) The changing incidence and presentation of urinary stones over 3 decades. Mayo Clin Proc 93(3):291–299. https://doi.org/10.1016/j.mayocp.2017.11.018
Talati VM, Soares RMO, Khambati A, Nadler RB, Perry KT (2020) Trends in urinary calculi composition from 2005 to 2015: a single tertiary center study. Urolithiasis 48(4):305–311. https://doi.org/10.1007/s00240-019-01151-z
Acknowledgments
We would like to thank Dr. Stefania Papatheodorou at Harvard T.H. Chan School of Public Health for suggesting statistical analysis methods in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chewcharat, A., Curhan, G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis 49, 27–39 (2021). https://doi.org/10.1007/s00240-020-01210-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-020-01210-w