Abstract
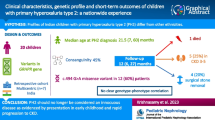
Primary hyperoxalurias (PH) are devastating, autosomal recessive diseases causing renal stones. Undifferentiated hyperoxaluria is seen in up to 43% of Pakistani paediatric stone patients. High rates of consanguinity in Pakistan suggest significant local prevalence. There is no detailed information regarding number of cases, clinical features, and genetics in Pakistan-origin (P-o) patients. We reviewed available information on P-o PH patients recorded in the literature as well as from two major PH registries (the Rare Kidney Stone Consortium PH Registry (RKSCPHR) and the OxalEurope PH Registry (OxER); and the Aga Khan University Hospital in Pakistan. After excluding overlaps, we noted 217 P-o PH subjects (42 in OxER and 4 in RKSCPHR). Presentations were protean. Details of mutations were available for 94 patients of 201 who had genetic analyses. Unique mutations were noted. Mutation [c.508G>A (p. Gly170Arg)] (present in up to 25% in the West) was reported in only one case. In one series, only 30% had mutations on exons 1,4,7 of AGXT. Of 42 P-o patients in OxER, 52.4% were PH1, 45.2% PH2, and 2.4% PH3. Of concern is that diagnosis was made after renal transplant rejection (four cases) and on bone-marrow aspiration (in five). Lack of consideration of PH as a diagnosis, late diagnosis, and loss of transplanted kidneys mandates that PH be searched for diligently. Mutation analysis will need to extend to all exons and include PH 1,2,3. There is a need to spread awareness and identify patients through a scoring or screening system that alerts physicians to consider a diagnosis of PH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The primary hyperoxalurias (PH) are associated with oxalate urinary tract stones, early onset renal impairment particularly in PH1, and tissue oxalate crystal deposition. Because presentation may be so diverse, ranging from asymptomatic patients to those with failure to thrive, haematuria, pyuria, recurrent urinary tract infection, nephrocalcinosis, or anaemia, this disease may escape detection.
A rare autosomal recessive disease, PH, is infrequently reported from Pakistan. This may be from failure to estimate urinary oxalate concentrations especially in paediatric patients and the lack of awareness of some of the characteristics of the disease, which include nephrocalcinosis, pure calcium oxalate monohydrate stones, variable but often early age at onset and early onset renal impairment with associated anaemia.
We believe that a large hidden burden of disease exists in Pakistan, as increasing prevalence of urinary stones is noted in children, [1], 72% of which are now in the upper urinary tract [2]. A significant number of stones may be attributed to PH, particularly in children under 6 months of age. Of 2618 paediatric urolithiasis patients, 24.3% have oxalate crystalluria; ~6% recur after clearance; and 18% have renal failure at presentation and 40–43% hyperoxaluria [2]. The presence of (undiagnosed) PH in adults is suspected, possible as 1.1% (of 449) stones from across Pakistan analysed by Fourier Transformation Infra-Red spectroscopy (FTIR) (June–October 2015) at the Aga Khan University clinical laboratory were pure calcium monohydrate stones (unpublished data from Dr Aysha Habib, clinical Laboratories, AKU). The incidence of PH in children born to P-o parents in West Midlands, UK, is higher than in those born to Western European parents [3]. Pakistan has a high consanguinity rate [4, 5] which makes it likely that this autosomal recessive disease has a high prevalence, as in countries such as Tunisia and in the Middle East [6]. Cochat has noted that 44% of the 78 PH patients in his series had Muslim parents [7].
We sought to review information on the incidence and prevalence of the disorder in those of Pakistani origin to highlight the need for early detection and therapy.
Objectives
To document the existing burden of PH in Pakistan-origin (P-o) populations.
Methods
We reviewed medical literature, data from two international PH registries and obtained information from the Aga Khan University hospital, listing all cases of PH in Pakistan-origin (P-o) populations, their clinical presentations, and genetic mutations.
The term Pakistan origin refers to those in whom a parent or both parents were of documented Pakistani origin, in either expatriate or native populations. Genetic documentation, strong clinical data to support a diagnosis of PH, proven hepatic alanine:glyoxalate transaminase (AGT), glyoxylate reductase/hydroxypyruvate reductase (GRHPR) or 4-hydroxy-2-oxoglutarate aldolase 1 (HOGA1) enzyme deficiency, or evidence of systemic oxalosis served as inclusion for a diagnosis of PH.
Relevant publications and cases were identified by literature review in Pubmed® and Google Scholar® and Google® search. The Aga Khan University Hospital [AKUH] admission database was analysed and both urology and paediatric surgical colleagues at AKUH were asked to identify if they had treated any cases of PH. Data on P-o patients were reviewed from two recognized data bases—that of Rare Kidney Stone Consortium PH Registry (RKSCPHR) and the OxalEurope PH Registry (OxER). Cases were examined for possible duplication and excluded as appropriate.
Findings
Pakistan-origin patients with PH
The initial overall count showed 260 patients. The PH registries yielded 46 patients (42 in OxER, four in RKSCPHR). There were no admissions with PH documented in the AKUH inpatient database. AKUH faculty yielded one ambulatory patient. Most (213) cases were identified using the web-based searches after cross checking with inclusion in the registries (see Table 1).
After exclusion of all potential overlaps, we noted a total of 217 patients in P-o population. Overlaps between cases documented in the Sindh Institute of Urology and Transplantation by Rizvi [2] and Khaliq’s [8] report is very likely; hence, 40 patients were eliminated from the final list. For 44 out of these 150, results from their genetic analysis were available, confirming PH1. For all 42 patients included in OxER, either genetic analysis (n = 41) or hepatic enzyme study (n = 1) was available.
Four P-o patients were noted in the RKSCPH Registry. Overlaps between RKSCPHR and two reported cases in the literature (cases #10 and #16 in Table 1) were confirmed by correspondence and excluded. One unreported case of PH (case #17 Table 1) was worked up in a Northern hospital and approached AKU for liver transplantation. The other case from AKUH (case #12 Table 1) was detected after a bone-marrow biopsy for anaemia showed oxalate crystals [9]. Although neither had genetic analysis nor had hepatic enzyme analysis to prove the diagnosis, all presented with the clinical features of PH.
Clinical spectrum and diagnostic pathway
The majority were children at time of diagnosis. The age of patients was not available in some publications. The youngest presented at 4 months (#7, Table 1). In the subset of 150 native Pakistanis [8], who underwent genetic analysis, the range of age of onset was 1–15 years, with rapid progression to renal failure at adolescence. In the three patients with PH2 in Johnson’s series, the age at diagnosis was 0.8–1.8 years, and the age at first stone was 0.8 years [10].
Adult diagnosis is documented. Four patients (one each in cohorts #2, #3, #6, and #18) were diagnosed after renal transplant failure. Five presented as adults with anaemia secondary to oxalate crystals noted in bone-marrow aspirate (#8, #12, #13, and two in #19). One additional patient underwent a bone biopsy (#10), which showed crystals of oxalate in bone. One patient died whilst awaiting transplant in Europe (#4) [11].
Most patients presented with renal calculi; some with pyuria (#4), UTI (#11); or failure to thrive (especially in younger patients—one each in # 7, #15, and #18). Median age at first stone in PH2 in a South Asian cohort was 39 months. With a median follow-up of 4 years, only 1 of 13 had a significant decline in renal function [10].
Confirmation of diagnosis
Hepatic enzyme studies had been done in patient #4, in two siblings of the index case in #18, and in one case from the OxER cohort. All other patients were diagnosed either by genetic analysis or clinical evidence of oxalosis.
Genetic analysis
Genetic analyses were available on 201 patients—150 by Khaliq, 41 from OxER and 10 from others. Results of detailed analysis beyond exon 1, 4 and 7 in Khaliq’s [8] series are still awaited.
Table 2 lists the genetic mutations and the related amino acid code, referenced according to the cohorts, as shown in Table 1.
With analysis limited to exons 1, 4, and 7, Khaliq noted 17 mutations in 44 of 150 patients (29% of their cohort). In the OxER data, 41/42 patients had confirmed genetic analysis. Combining results from genetic and enzyme analysis, 22 (52.4%) have PH1, 19 (45.2%) PH2, and 1 (2.4%) PH 3. Johnson [10], adding 13 cases to the list of known PH2, noted that all but one were from South Asia, three (from one family) of them P-o; the rest were Afghans. In the paper by Monico [12], at least one case of PH3 is included.
Mutations noted in different cohorts varied. c.1049G>A (p.G350D), accounted for 24% (n = 10) of all mutations (and 47.6% of the mutations specifically amongst PH1) in OxER data, cohort #5; and 8% of Khaliq’s cohort (#2) [8].
c.798–802 del insACAATCTCAG was seen in 4 of 21 (19%) PH1 patients (in OxER). Khaliq noted c.568G>C [p.G190R] in 7 of 44 (16%) PH1 cases and c.33dupC in 5 of 44 (11.3%) [8].
c. 245 G>A [p.G82E] was reported on exon 2 [7] and noted in 2% (cohort #2) [8] to 4.9% (cohort #5) of all mutations. ‘Three novel mutations, one splice-site, four index and twelve missense mutations’ have been noted without further description [8].
Noticeable was the absence of the most common mutation in Western Europe, and c.508G-A (p.G170R) noted only in one heterozygous patient [4], where it occurred with c.33_34InsC.
Other mutations unique to Pakistanis were noted in exon 2 (PH1), where Chanchlani [13] (case #15) noted a missense mutation PH1, with substitution of thymidine with cytosine at nucleotide 302 (c.302T>C). On exon 8 PH1, Schnakenberg [14, 15] describes “Nucleotides 920–924 (CATCA) deleted and replaced by ACAATCTCAG, leading to a shift in the reading frame and the introduction of a stop codon, with a loss of 119 amino acids at the C terminal”. This change was noted in only 2.5% of their total PH1 cohort; but occurred in two unrelated P-o families.
Other Pakistan specific mutations have been observed. As an example, Chu [16] noted a novel missense mutation 364 C>T R122X mutation, for the AGXT gene and Perera a c.653C>T (p.Ser 218Leu) mutation [17].
The commonest mutation on GRHPR (Table 2) was c.[403_404 + 2delAAGT] seen in 15 of 19 (80%) OxER patients, among which two patients had a combination of the c.[403_404 + 2delAAGT] and c.[540 del T] mutation, and two had c.[494G>A]G165N mutation.
Documentation of mutations in HOGA1 is available for one patient from OxER with c.134C > T.
Data on estimates of disease burden
Hyperoxaluria in 40–43% of paediatric stone patients [2] is indicative of a potentially high incidence of PH.
Discussion
This is the first attempt at description of PH in P-o patients. We have included 217 PH cases with documented clinical evidence, hepatic enzyme studies, or confirmed genetic analysis. Possible duplicates were excluded. We have not obtained information by questionnaire or established registry in Pakistan in this preliminary exploration. There are some additional shortcomings to our study: this survey was limited to recorded literature as we have yet to evaluate physician knowledge of the disease, its milder variants, delayed presentation, and existence without hyperoxaluria. We need to survey all hospitals, contact all nephrologists and urologists by questionnaire, and seek information from stone databases. We have not sought information on conservative treatment (e.g., supplementation with pyridoxine) in the reported patient groups.
Information on genetic mutations in this cohort of PH P-o patients was incomplete, but our consolidated series from multiple sources is valuable. Mutations noted in this cohort differ from those generally seen in Caucasian and perhaps the Japanese populations. Mutations were found on exons 1, 4, or 7 of AGXT in only 30% [8] as compared to 77% [17] noted in Caucasian populations. In PH2, the Exon4/Intron 4 missplicing c.[403_404 + 2delAAGT] were seen in ~80% of P-o patients in OxER and in 37.8% of PH2 patients in Takayama’s [18] series (where 78%–7/9 of those with this mutation were from the Indian subcontinent).
The terms ‘Asian origin’ and ‘Indian subcontinent’ are vague and misleading. Asia is composed of many genetically distinct populations. The word Indian subcontinent should be replaced by the term South Asia, which includes Afghanistan, India, Pakistan, Sri Lanka, Bangladesh, Nepal, and Bhutan. It includes populations in which the current mtDNA represents the original invasions of the ‘mother’ mtDNA (and who are mainly in the Deccan peninsula) as well as those in the northern areas of South Asia, which have been subject to many invasions of fresh mtDNA from the North-Western corridors.
For the AGXT gene, a comprehensive genetic analysis of all 11 exons is required, because (i) the >150 known mutations in PH occur across all 11 exons [19] and (ii) mutations have been noted in P-o patients on other exons: on Exon 2 by Cochat [3] Chanchlani [13] and on Exon8 (von Schnakenburg) [15]. Limiting the analysis to exons 1, 4, 7 (PH1) will miss other unique mutations reported in P-o persons. Some will question the use of gene wide screening of all exons, but it is well known that some genetic variations are ethnically determined, and would be missed by limited screening [20].
In addition, GRHPR and HOGA1 should also be considered, after initial screening the urine for glyceric acid for PH2 and HOG, DHG, and 4-OH-Glu metabolites for PH3. We know from Monico’s report [12] that at least one of the patients with HOGA1 mutation was from Pakistan, and the OxER documents a significant number of patients with PH2. Johnson [10] reports on additional cases with PH2, all but one originated from South Asian region, from Pakistan (three patients), and Afghanistan.
In Mandrile’s [21] analysis of 410 patients (from the OxER) with documented AGXT genotype, nearly, 10% of patients were from ‘other countries’, which included a very wide swathe of countries inclusive of Afghanistan and Pakistan. Our data from the OxER pertains to those registered as Asians in whom ethnicity was attributed to Pakistan and who had genetic or liver enzyme study confirmation of the disease.
We suggest that genetic analysis algorithms will need to be modified. Alternatives of whole genome sequencing and testing for a panel of genes will need to be considered for P-o patients. This would provide important knowledge that will help to better understand the PH spectrum in Pakistan.
The ‘missing’ genetic mutations
Coulter-Mackie [22] draws attention to the fact that some genetic mutations such as c.508G>A (p.G170Arg) and 33_34insC show no obvious ethnic associations and have been found in a variety of populations. Danpure [23] has shown that c.508G>A (p.Gly170Arg) allows significant residual catalytic activity, and is found in 20–40% of patients in the West. Only one patient in this series had this mutation.
This has ominous portents: If p.Gly170Arg (c.508G>A) mutation or the Phe152Ile (c.454T>C; p.F1521) mutations are indeed absent, and not unreported, then the P-o population will be unresponsive to pyridoxine therapy, and will develop end-stage renal disease earlier. Harambat reports that patients with p.Gly170Arg (allelic frequency 21.5%) show a delayed onset of renal failure (at a median age of 47 years for homozygotes, 35 years for heterozygotes compared with 21 years for PH without this mutation) [20]. On the other hand, c.33dupC (12% allele frequency in Caucasians) that leads to protein truncation was found in only 3.3% P-o patients.
Variance in phenotypic expression of genotype
Whilst the ultimate diagnosis of PH rests on genetic analysis, there is considerable variation in phenotypic expression [17]. Population analysis by Hopp [24] suggests that PH is more common than determined from clinical cohorts. This might be because milder forms of PH, in which suspicion of the disease is not raised, result in missed diagnosis. The genetic mutations influencing all three PH enzymes AGT, GRHPR, and HOGA1 will need to be studied, as Beck [25] notes that multi-allelic inheritance might be responsible for the phenotypic variation.
Ignorance regarding PH and possible missed diagnosis in Pakistanis
As many patients in the OxalEurope registry OxER are of P-o, we suggest that Pakistan could harbour a larger load of PH than we record, and it is worth determining the actual disease burden as this is a devastating disease. Our inability to find more cases might arise from reporting failure, insufficient awareness, milder forms of disease, and late onset (masquerading as idiopathic stone disease).
Prediction of future total PH burden in Pakistan
Estimates of disease burden are difficult. Hutchesson, noted an incidence of 1 in 14,552 P-o births in Birmingham [26], an immense number as compared to the estimated incidence rate (1 in 201,777) in NW European new-born’s in the same region. This was the finding in a small community isolated from home, in which the gene frequency could have been enhanced beyond that in the parent country (Pakistan). This is likely, because the rate of first cousin marriages (55%) in the Pakistani origin parents is higher than that in the new-born’s maternal grandmothers (33%) [27]. PH incidence in Pakistan might be predicted to be as high as found in the P-o population in Birmingham, because similar rates of consanguinity, ‘biraderi’, and endogamy exist in Pakistan (ranging between 50% [27] and 76%) [3]). This could well increase allele frequency to significantly impact on the incidence of PH [28]. In addition, though an autosomal recessive disorder, there is evidence that in some of the families, more than 25% of the siblings are affected.
Extrapolation of Western incidence such as the prevalence rates from North American data in the RKSCPHR (which suggests a prevalence of 1 in 58,000 and carrier rate 1 in 70), to Pakistani population would be erroneous, as the population demographics are different. In Pakistan, 33% are under 15 years of age, whilst in the UK, this group only represents 17.3%. Age standardized rates are not available. Nevertheless, based on Western data, we would have 24–62 patients a year and a total existing PH burden ranging between 40 and 2897.
In Pakistan, high consanguinity rates increase the chances for manifestation of this autosomal recessive disorder. One could argue that continuous intermarriage would eventually eliminate deleterious recessive genes, especially in a fatal condition such as PH. However, reproductive compensation occurs in these groups to maintain a level of persistence of the disease [29], and thus, we need to draw attention to the importance of considering a diagnosis of PH in this population.
More insight into the disease burden in Pakistan is pivotal to improve therapeutic strategies for this devastating disease, especially with new promising therapeutic modalities under development [30, 31]. There are options for genetic counselling and chorionic villus biopsy in subsequent pregnancies. Loss of kidney transplants in undiagnosed cases can be avoided and screening must be considered appropriately in transplant recipients [32]. Focused effort is needed to detect all patients. Cases will continue to be missed because of lack of awareness and failure to estimate urinary metabolites; glycolate, glycerate, 4-hydroxy-2-oxoglutarate (HOG), and 2,4-dihydroxyglutarate (DHG) (which are raised in PH1, 2 and 3, respectively) [33]. Better understanding of the PH spectrum in Pakistan (including its common mutations) will help to set up a cost-effective, first-line investigation pathway to diagnose PH in an earlier stage of the disease course.
Conclusion
-
1.
This preliminary survey suggests high numbers of P-o patients in Pakistan.
-
2.
Information on PH needs to be disseminated to all urological units in Pakistan, and a PH risk score card developed to alert the need for detailed diagnostic evaluation.
-
3.
Methods for chemical analysis and normal ranges of 24-h urines and spot samples for oxalate: creatinine ratio should be standardized across Pakistan. Physicians need to be urged to investigate urinary excretion of oxalate and other metabolites.
-
4.
Genetic analysis for diagnosis of PH will need to include investigation of AGXT (all exons), GRHPR, and HOGA1 as appropriate.
-
5.
All children presenting with renal stones, and adults presenting with recurrent stones should be evaluated with at least one urinary oxalate and possibly a glyceric acid excretion screen.
-
6.
A registry of urinary tract stone disorders needs to be initiated in Pakistan to contribute data and provide valuable information for physicians nationally and internationally.
References
The News correspondent (2015) Sukkur has become a ‘red zone’ with regards to Kidney diseases: Dr Adib. Dawn. http://www.dawn.com/news/1218564. Accessed 26 Sept 2016
Rizvi SA, Sultan S, Zafar MN, Ahmed B, Faiq SM, Hossain KZ, Naqvi SA (2007) Evaluation of children with urolithiasis. Indian J Urol 23(4):420
Cochat P, Nogueira PCK, Mahmoud MA, Jamieson NV, Scheinman JI, Rolland M-O (1999) Primary hyperoxaluria in infants: medical, ethical, and economic issues. J Pediatr 135(6):746–750
Spasovski G, Beck BB, Blau N, Hoppe B, Tasic V (2010) Late diagnosis of primary hyperoxaluria after failed kidney transplantation. Int Urol Nephrol 42(3):825–829
Hashmi M (1997) Frequency of consanguinity and its effect on congenital malformation-a hospital based study. J Pakistan Med Assoc 47:75–77
Kamoun A, Lakhoua R (1996) End-stage renal disease of the Tunisian child: epidemiology, etiologies, and outcome. Pediatr Nephrol 10(4):479–482
Cochat P (1999) Primary hyperoxaluria type 1. Kidney Int 55(6):2533–2547
Khaliq S, Abid A, Shahid S, Hashmi S, Sultan S, Aziz T, Rizvi SAH, Mehdi SQ (2013) Comprehensive mutation screening of the AGXT gene in patients with primary hyperoxaluria type-1. Paper presented at the 63rd annual meeting of the American Society of Human Genetics, Boston
Sajid R, Moiz B, Adil S, Khurshid M (2009) Calcium oxalate crystals in the bone marrow. Br J Haematol 146(1):1
Johnson SA, Rumsby G, Cregeen D, Hulton S-A (2002) Primary hyperoxaluria type 2 in children. Pediatr Nephrol 17(8):597–601
Illum N, Lavard L, Danpure C, Horn T, AErenlund JH, Skovby F (1991) Primary hyperoxaluria type 1: clinical manifestations in infancy and prenatal diagnosis. Child Nephrol Urol 12(4):225–227
Monico CG, Rossetti S, Belostotsky R, Cogal AG, Herges RM, Seide BM, Olson JB, Bergstrahl EJ, Williams HJ, Haley WE (2011) Primary hyperoxaluria type III gene HOGA1 (formerly DHDPSL) as a possible risk factor for idiopathic calcium oxalate urolithiasis. Clin J Am Soc Nephrol 6(9):2289–2295
Chanchlani R, Sinha A, Gulati A, Agarwal V, Bagga A (2012) Common mutation underlying primary hyperoxaluria type1 in three Indian children. Indian J Nephrol 22(6):459
von Schnakenburg C, Rumsby G (1997) Identification of new mutations in primary hyperoxaluria type 1 (PH1). J Nephrol 11:15–17
von Schnakenburg C, Hulton SA, Milford DV, Roper HP, Rumsby G (1998) Variable presentation of primary hyperoxaluria type 1 in 2 patients homozygous for a novel combined deletion and insertion mutation in exon 8 of the AGXT gene. Nephron 78(4):485–488
Chu W (2011) Case report renal and musculoskeletal manifestations of primary hyperoxaluria in a girl 女孩原發性高尿酸血症的腎臟及肌肉骨胳的臨床表現. HK J Paediatr 16(1):41–46
Perera MTP, Sharif K, Lloyd C, Foster K, Hulton SA, Mirza DF, McKiernan PJ (2011) Pre-emptive liver transplantation for primary hyperoxaluria (PH-I) arrests long-term renal function deterioration. Nephrol Dial Transpl 26(1):354–359
Takayama T, Takaoka N, Nagata M, Johnin K, Okada Y, Tanaka S, Kawamura M, Inokuchi T, Ohse M, Kuhara T (2014) Ethnic differences in GRHPR mutations in patients with primary hyperoxaluria type 2. Clin Genet 86(4):342–348
Williams EL, Acquaviva C, Amoroso A, Chevalier F, Coulter-Mackie M, Monico CG, Giachino D, Owen T, Robbiano A, Salido E (2009) Mutation update. Hum Mutat 30:910–917
Harambat J, Fargue S, Acquaviva C, Gagnadoux M-F, Janssen F, Liutkus A, Mourani C, Macher M-A, Abramowicz D, Legendre C (2010) Genotype–phenotype correlation in primary hyperoxaluria type 1: the p. Gly170Arg AGXT mutation is associated with a better outcome. Kidney Int 77(5):443–449
Mandrile G, van Woerden CS, Berchialla P, Beck BB, Bourdain CA, Hulton S-A, Rumsby G (2014) Data from a large European study indicate that the outcome of primary hyperoxaluria type 1 correlates with the AGXT mutation type. Kidney Int 86(6):1197–1204
Coulter-Mackie MB, Rumsby G (2004) Genetic heterogeneity in primary hyperoxaluria type 1: impact on diagnosis. Mol Genet Metab 83(1):38–46
Danpure CJ (2005) Primary hyperoxaluria: from gene defects to designer drugs? Nephrol Dial Transpl 20(8):1525–1529
Hopp K, Cogal AG, Bergstralh EJ, Seide BM, Olson JB, Meek AM, Lieske JC, Milliner DS, Harris PC, Consortium RKS (2015) Phenotype-genotype correlations and estimated carrier frequencies of primary hyperoxaluria. J Am Soc Nephrol 26(10):2559–70. doi:10.1681/ASN.2014070698
Beck BB, Baasner A, Buescher A, Habbig S, Reintjes N, Kemper MJ, Sikora P, Mache C, Pohl M, Stahl M, Toenshoff B, Pape L, Fehrenbach H, Jacob DE, Grohe B, Wolf MT, Nürnberg G, Yigit G, Salido EC, Hoppe B (2013) Novel findings in patients with primary hyperoxaluria type III and implications for advanced molecular testing strategies. Eur J Hum Genet 21(2):162–172. doi:10.1038/ejhg.2012.139
Hutchesson A, Bundey S, Preece M, Hall S, Green A (1998) A comparison of disease and gene frequencies of inborn errors of metabolism among different ethnic groups in the West Midlands, UK. J Med Genet 35(5):366–370
Darr A, Modell B (1988) The frequency of consanguineous marriage among British Pakistanis. J Med Genet 25(3):186–190
Bittles AH (2001) Consanguinity and its relevance to clinical genetics. Clin Genet 60(2):89–98
Overall A, Ahmad M, Nichols R (2002) The effect of reproductive compensation on recessive disorders within consanguineous human populations. Heredity 88(6):474–479
Liebow A, Li X, Racie T, Hettinger J, Bettencourt BR, Najafian N, Haslett P, Fitzgerald K, Holmes RP, Erbe D, Querbes W, Knight J (2017) An Investigational RNAi Therapeutic Targeting Glycolate Oxidase Reduces Oxalate Production in Models of Primary Hyperoxaluria. J Am Soc Nephrol 28(2):494–503. doi:10.1681/ASN.2016030338
Gambaro G, Ferraro MP, D’Addessi A (2011) Ayurvedic medicine and NADPH oxidase: a possible approach to the prevention of ESRD in hyperoxaluria. Nephrol Dial Transpl 26(6):1759–1761
Naderi G, Tabassomi F, Latif A, Ganji M (2015) Primary hyperoxaluria type 1 diagnosed after kidney transplantation: the importance of pre-transplantation metabolic screening in recurrent urolithiasis. Saudi J Kidney Dis Transpl 26(4):783
Clifford-Mobley O, Hewitt L, Rumsby G (2016) Simultaneous analysis of urinary metabolites for preliminary identification of primary hyperoxaluria. Ann Clin Biochem 53(4):485–494
Rizvi AH speaks on management of pediatric urolithiasis (2013). Pulse international. http://www.pulsepakistan.com/index.php/main-news-jan-15-14/613-prof-adeebul-hassan-rizvi-speaks-on-management-ofpediatric-urolithiasis
Alsuwaida A, Hayat A, Alwakeel JS (2007) Oxalosis presenting as early renal allograft failure. Saudi J Kidney Dis Transpl 18(2):253
Hassan K, Qaisrani JH, Qazi H, Naseem L, Zaheer HA, Zafar T (2006) Oxalosis in the bone and bone marrow. Int J Pathol 4(2):129–131
Tang X, Bergstralh EJ, Mehta RA, Vrtiska TJ, Milliner DS, Lieske JC (2015) Nephrocalcinosis is a risk factor for kidney failure in primary hyperoxaluria. Kidney Int 87(3):623–631
Ehsan A, Lone A, Sabir O, Riaz S, Tareef N, Tanvir I (2015) Refractory anemia with Hyperoxaluria. J Adv Plant Biol 1(1):1–5. http://oap-journals.org/jna/article/153. Accessed 26 June 2017
Raza F, Hussain CA, Khan SA, Saeed H, Ayyub M (2016) Crystalline bone marrow in young lady Pakistan Society of Hematology Newsletter 10(1):7–12. http://psh.org.pk/forumfiles/Newsletter_2016.pdf. Accessed 26 June 2017
Acknowledgements
We acknowledge the support and valued critique of earlier drafts of this paper by Professor Dawn S Milliner, Director, Rare Kidney Stone Consortium, and principal investigator, Primary Hyperoxaluria group, Mayo Clinic Hyperoxaluria Center, Rochester. We acknowledge with gratitude the contribution of data from the OxalEurope registry (see http://www.oxaleurope.com) and the sharing of laboratory data by Farooq Ghani, M.B.B.S., M.S., Ph.D., FACB, Diplomate American Board, Service Chief & Director Clinical Laboratories, Associate Professor, Department of Pathology, Aga Khan University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have declared that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
This study has not received any grant funding.
Rights and permissions
About this article
Cite this article
Talati, J.J., Hulton, SA., Garrelfs, S.F. et al. Primary hyperoxaluria in populations of Pakistan origin: results from a literature review and two major registries. Urolithiasis 46, 187–195 (2018). https://doi.org/10.1007/s00240-017-0996-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-017-0996-8