Abstract
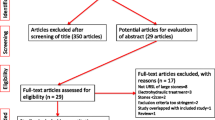
The treatment of urolithiasis has changed dramatically over the past several decades. Novel technologies have led to new management protocols. Percutaneous chemolysis as a primary or adjuvant treatment for urinary tract stones has widely been neglected. We present our own experience with it and discuss it in the light of an extensive literature review. From a MEDLINE search on percutaneous chemolysis we evaluated the most important studies, a total of 58 articles, 43 case series and 15 review articles. In our unit between 2001 and 2011, 29 patients (mean age 62 years) with infectious staghorn calculi were treated with adjuvant percutaneous chemolysis post-percutaneous nephrolithotripsy. There were 17 women, with 10 complete and 14 partial staghorn stones (mean size 32 mm). Patients were generally deemed at high risk to undergo another procedure in the future. Suby G solution was used following an established protocol. Sixteen patients (55.1 %) were stone free after chemolysis, eight stones showed partial dissolution, half of them with so-called “insignificant” residual fragments <4 mm. Patients with residual stones underwent SWL. Mean follow-up was 5.25 years (1–11). One stone-free patient (6 %) and three of eight patients (37.5 %) with residual fragments post local chemolysis, developed new stones during follow-up. The often neglected percutaneous chemolysis represents a significant and effective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemolysis has been used as an adjuvant and primary treatment modality in the management of urinary tract stones for decades. The first case of stone dissolution with chemolysis was reported in 1924 [1].
In case of large stones of suitable composition, a primary de-bulking and surface increasing procedure, i.e., percutaneous nephrolithotripsy (PCNL) may be complemented by topical chemolysis.
Techniques
To apply topical chemolysis directly onto a stone/fragment, various techniques have been described including use of ureteric catheters (UC), percutaneous nephrostomies (PCN), enhanced by special devices such as computer-controlled intrapelvic pressure monitoring, infusion pumps, and central pressure manometers (CVP) [2, 3]. Using a computer-controlled pressure monitoring, intermittent pump allows for a constant low intrarenal pressure (IP). This device stops irrigation when IP rises above a preset limit of 15 cm H2O. This increases not only the safety of irrigation chemolysis, but unfortunately also its cost [2].
The use of a single ureteric catheter is cheaper but hampered by severe outflow restriction. Therefore, it should be used in connection with a PCN. Retrograde irrigation allows for a good drainage of the kidney but immobilizes the patient. Anterograde irrigation restricts again the drainage through the much smaller UC. The latter can be used for a small stone burden over a shorter time period [4].
The insertion of a second PCN (co-axial technique) provides excellent flows and low IP. In patients with large stones, a JJ stent to facilitate fragment passage is recommended as well as an adequate position of the patient to allow maximum contact between stone and solution [5, 6].
Control of IP will avoid pyelovenous backflow, systemic absorption and extravasation of the solution which can lead to tissue reaction and de-balancing of the alkali-balance. A CVP connected to the inflow limb is commonly used but remains open to contamination or overflow spills and requires frequent monitoring. This can be overcome using a variable pressure volumetric pump which delivers a set rate of infusate within a specified pressure range in a closed system. During infusion, there is a constant display of IP. If the maximum set pressure limit is exceeded the pump audibly signals occlusion and the infusion is automatically discontinued [7]. Ureteral-access sheaths have been shown to allow high-flow low-pressure irrigation of the renal collecting system in combination with a catheter.
Complications
The emphasis on a good drainage at low pressure stems from an attempt to avoid complications. In the early 1960s, the safety of Renacidin (hemiacidrin) first came into question after the report of six deaths during percutaneous chemolysis. Postmortem finding included renal infarction, necrosis, pyelonephritis, ureteritis, papillary necrosis and chemical pyelitis, with high inflow pressures over 80 mm Hg [8, 9]. The Food and Drug Administration (FDA) initially banned the use of Renacidin for the upper urinary tract and bladder. Ultimately, all deaths were attributed to obstructed ureteral catheters resulting in increased IP and urosepsis [10]. Based on these findings, the FDA approved Renacidin to “prevent formation of and to dissolve calcifications in catheters in the urinary bladder”. Twenty-seven years later it was also approved for the treatment of infectious renal and bladder calculi [11].
A strict protocol in patients harboring infectious stones with appropriate antibiotic prophylaxis is mandatory [12]. Irrigation must be discontinued or reduced if flank pain occurs. Absolute contraindications include ongoing urinary tract infection, fever, persistent flank pain, and a creatinine clearance <10 mL/min [13]. Irrigation will begin on the fourth or fifth postoperative day with saline irrigation first, to test for possible leaking from the puncture site after PCNL. If no leakage, fever, or flank discomfort occurs, 10 % Renacidin can be started at 120 ml/h. IP should be kept <25 cm H2O. Once there was absence of visible particles on tomography, the irrigations would cease after an additional 24–48 h [14].
Indications
Topical chemolysis applied directly onto the stone(s) by the various techniques described above can be used as an adjuvant postoperative treatment or as primary therapy in selected cases, mainly those restricted from invasive surgery. Stone composition dictates the indication and results may vary:
Residual fragments infectious stones (struvite), often with embedded bacteria, may serve as a nidus for new stone formation and rapid recurrences. This needs not only rendering the patient stone-free but also sterilizing the urine. Persistence of infection occurs in ~40 %. Consequently, prophylactic adjuvant chemolysis may reduce struvite stone recurrences [15]. Success of adjuvant chemolysis can be improved by increasing the surface area of the stones through fragmentation [16]. One hundred and eighteen patients with infectious staghorn stones were treated with a combination of repeated SWL and chemolysis. The stone-free rate was 77 % and superior to SWL alone. They however had a long hospital stay of ~32 days [17]. In other studies, the stone-free rate after adjuvant chemolysis with hemiacidrin or Suby G was 80 %, with a treatment duration of 1–34 days, a recurrence rate of 11–20 % after a follow-up of 2–5 years [18, 19].
In infectious stones, topical chemolysis may be used as a primary therapy. In 46 patients, a stone-free rate of 52 % in the ureter and 50 % in the bladder was reported [20]. Chemolysis in 119 patients with spinal cord injury led to stone-freeness in 51 (43 %), and partial dissolution in 26 (22 %) patients after a mean treatment time of ~70 days. After 2 years, the recurrence rate was 23 %.
Results of topical chemolysis as primary therapy are limited, but it has been proposed for high-risk patients that are not suitable for surgery in an outpatient setting [21].
There are two types of cystine stones, the smooth type (cystine-S) and the rough type (cystine-R) [22]. The latter is easily fragmented with SWL which may facilitate chemolysis. Cystine-S stones are denser and harder. Dissolution agents include d-penicillamine, tromethamine-E or tiopronin, and N-acetylcysteine [23–25]. After PCNL or SWL of renal cystine stones >1.5 cm with adjuvant chemolysis stone-free rates were increased and recurrence rates decreased [23–26]. SWL enlarged the stone surface area and decreased the dissolution time by nearly 50 % [26].
Eleven patients underwent primary treatment with Tromethamine-E solution as an alternative to surgery. After 6–42 days, seven complete stone dissolutions were achieved, and three treatment failures [27].
Percutaneous adjuvant chemolysis of uric acid stones is effective. With the use of sodium bicarbonate irrigation, almost all stones can be dissolved in 4–18 days [28, 29]. Again, combination with SWL to increase the surface exposed to the solution may help even further [30]. Primary percutaneous chemolysis is similarly effective [31].
Calcium containing calculi are the least amenable to chemolysis. The strong acids required to dissolve this compound cannot be safely used in humans. Only chelating agents have successfully been used in vitro to dissolve calcium stones. Ethylene-diamine-tetraacetic acid (EDTA) is the most commonly used solvent, has moderate success in humans but also results in urothelial injury [32, 33]. Complete stone dissolution of over 50 % in 260 patients treated with EDTA was reported. Application in the early stages of stone formation is associated with a better response rate [32, 33]. Calcium oxalate stones do not dissolve with Suby G solution or hemiacidrin [18].
Our results
In our unit, we do use percutaneous adjuvant chemolysis after PCNL of infectious stones. Between 2001 and 2011, 29 such patients have been treated. There were 17 women and 12 men, presenting with 10 complete and 14 partial staghorn stones. Five patients presented with multiple renal stones >15 mm. The mean age was 62 years and the mean stone size was 32 mm. Patients had multiple co-morbidities, previous and/or failed kidney stone operations, and/or were unfit for second-look PCNL or other adjuvant procedures. The initial PCNL’s were uneventful in all patients. Irrigation was started with the use of a pressure feedback infusion pump through the PCN (F12 Malecot tube, Lingeman kit®, Boston Scientific, Natick, MA, USA) usually after 2–3 days when bleeding had stopped and the nephrostomy site had matured. Irrigation with saline only was gradually increased from 30 to 100 ml/h over 48 h. Suby G solution, a buffered mixture of 4 % citric acid, magnesium oxide and sodium bicarbonate (100 ml diluted in 500 ml 0.9 % NaCL) was started at a rate of 30 ml/h, gradually increasing to 100 ml/h over the following 72 h. All patients were on prophylactic antibiotics during chemolysis. Daily kidney function tests and serum bicarbonate levels were measured. Renal outflow was secured through an intraoperatively inserted JJ stent (F6) and an indwelling bladder catheter.
During treatment, three patients developed fever and two chemical cystitis which led to an interruption of treatment. No serious complications (i.e. urosepsis or electrolyte misbalances) occurred.
In our series, 16 of 29 kidneys (55.1 %) were stone free after chemolysis, eight stones showed partial dissolution (27.5 %), with the half of them presenting so-called “insignificant” residual fragments <4 mm. In five cases (17.2 %), the residual fragments remained unchanged after the chemolytic treatment. The presence of residual calculi post local chemolysis, has been evaluated with a CT KUB performed in 2 months. Patients with residual stones have been treated with adjuvant SWL. After a mean follow-up of 5.2 years (1–11), 1 (6 %) stone-free patient developed small stone recurrences, and three of eight patients (37.5 %) with persistent residual fragments formed larger stones.
PCNL and SWL have made topical (i.e. percutaneous) chemolysis primarily an adjuvant treatment [11]. In both, SWL and PCNL, residual fragment may occur in up to 40 % depending on the stone composition and size, and the expertise of the operator [14]. Persistent residual fragments of certain stones may therefore represent an indication for percutaneous chemolysis. The choice of chemolytic agent and technique of administration is primarily dependent on stone composition [34, 35].
The advantages of percutaneous chemolysis are a low complication rate and the absence of the need for anaesthesia [36]. It can be an option in high-risk cases and in patients where standard treatment modalities can be problematic, i.e. paraplegics with insufficient bladder drainage, patients with bleeding disorders or an ileal conduit. On the other hand, intense treatment protocols, patient compliance, the need for additional ureteral and nephrostomy tubes, and prolonged hospitalization with associated costs need to be balanced.
In conclusion, percutaneous—mostly adjuvant—chemolysis is a helpful complement to stone fragmentation treatments in selected cases and for certain stones. Indications must be made on a case-by-case basis and strict protocols with continuous monitoring must be adhered to. Certainly, specialized stone centers must include percutaneous chemolysis in their armamentarium, albeit with the necessary caution. With the trend towards ambulatory care, ambulatory percutaneous chemolysis is currently investigated and may open new perspectives for the future.
References
Crowell A (1924) Cystine nephrolithiasis. Surg Gynecol Obstet 38:87–91
Kuwahara M, Kambe K, Takahashi K et al (1982) Intermittent irrigation system for dissolution of renal calculi monitored by computer. J Urol 128:1379–1381
Angermeier K, Streem SB, Yost A (1993) Simplified infusion method for 10% hemiacidrin irrigation of renal pelvis. Urology 41:243–246
Dretler SP, Pfister RC, Newhouse JH (1979) Renal-stone dissolution via percutaneous nephrostomy. N Engl J Med 300:341–343
Bernardo NO, Smith AD (2000) Chemolysis of urinary calculi. Urol Clin North Am 27:355–365
Rodman JS, Reckler JM, Israel AR (1981) Hemiacidrin irrigations to dissolve stone remnants after nephrolithotomy. Problems with solution flow. Urology 18:127–130
Angermeier K, Streem SB, Yost A (1993) Simplified infusion method for 10% hemiacidrin irrigation of renal pelvis. Urology 41:243–246
Fostvedt GA, Barnes RW (1963) Complications during lavage therapy for renal calculi. J Urol 89:329–331
Ebel A, Kuo J (1964) Post mortem findings in a patient treated with renacidin for unilateral renal calculosis. Proc Annu Clin Spinal Cord Inj Conf 13:93–97
Mulvaney WP, Henning DC (1962) Solvent treatment of urinary calculi: refinements in technique. J Urol 88:145–149
Gonzalez RD, Whiting BM, Canales BK (2012) The history of kidney stone dissolution therapy: 50 years of optimism and frustration with renacidin. J Endourol 26:110–118
Nemoy NJ, Stamey TA (1971) Surgical, bacteriological, and biochemical management of “infection stones”. JAMA 215:1470–1476
Cato A, Tulloch A (1974) Hypermagnesemia in a uremic patient during renal pelvis irrigation with renacidin. J Urol 111:313–314
Skolarikos A, Papatsoris AG (2009) Diagnosis and management of postpercutaneous nephrolithotomy residual stone fragments. J Endourol 23:1751–1755
Griffith DP (1978) Struvite stones. Kid Int 13:372–382
Joshi HB, Kumar PVS, Timoney AG (2001) Citric Acid (solution R) irrigation in the treatment of refractory infection (struvite) stone disease: is it useful? Eur Urol 39:586–590
Tiselius HG, Hellgren E, Andersson A, Borrud-Ohlsson A, Eriksson I (1999) Minimally invasive treatment of infection staghorn stones with shock wave lithotripsy and chemolysis. Scand J Urol Nephrol 33:286–290
Wall I, Tiselius HG, Larsson L (1988) Hemiacidrin: A useful component in the treatment of infectious renal stones. Eur Urol 15:26–30
Sant GR, Blaivas JG, Meares EM Jr (1983) Hemiacidrin irrigation in the management of struvite calculi: Long-term results. J Urol 130:1048–1050
Mulvaney WP (1960) The clinical use of Renacidin in urinary calcifications. J Urol 84:206–212
Palmer J, Bishai MB, Mallon DS (1987) Outpatient irrigation of the renal collecting system with 10 percent hemiacidrin: cumulative experience of 365 days in 13 patients. J Urol 138:262–265
Bhatta KM, Prien EL Jr, Dretler SP (1989) Cystine calculi–rough and smooth: a new clinical distinction. J Urol 142:937–940
Hayase Y, Fukatsu H, Segawa A (1980) The dissolution of cystine stones by irrigated tio- pronin solution. J Urol 124:775–778
Stark I, Savir A (1980) Dissolution of cystine calculi by pelviocaliceal irrigation with d-penicillamine. I Urol 124:895–898
Tseng CH, Talwalkar YB, Tank ES, Hatch T, Alexander SR (1982) Dissolution of cystine calculi by pelviocalyceal irrigation with trometamine-E. J Urol 128:1281–1284
Schmeller NT, Kersting H, Schüller J, Chaussy C, Schmiedt E (1984) Combination of chemolysis and shock wave lithotripsy in the treatment of cystine renal calculi. J Urol 131:434–438
Dretler SP, Pfister RC, Newhouse JH, Prien EL Jr (1984) Percutaneous catheter dissolution of cystine calculi. J Urol 131:216–219
Vandeursen H, Pittomvils G, Baert I (1991) Combined extracorporeal shock wave lithotripsy and percutaneous alkalinisation in uric acid calculi. Urol lnt 46:27–28
Breuel F, Altwein JE, Schneider W (1988) Local chemolysis of occluding uric acid calculi. Z Urol Nephrol 81:613–622
Lee YH, Chang LS, Chen MT, Huang JK, Chen KK, Lin AD (1991) Experience with percutaneous nephrostomy, extracorporeal shock wave lithotripsy and chemolysis in the treatment of obstructive uric acid stones. Eur Urol 19:209–212
Nummi P (1973) Dissolution of uric acid stones by local lavage. Scand J Urol Nephrol 7:172–174
Ziolkowski F, Perrin D (1977) Dissolution of urinary stones by calcium-chelating agents: a study using a model system. Invest Urol 15:208–211
Verplaetse H, Verbeeck RMH, Minnaert H, Oosterlinck W (1986) Screening of chelating agents for chemolysis. Eur Urol 12:190–192
Dormia E, Dormia G, Malagola G, Minervini S (2003) Experience with instrumental chemolysis for urolithiasis. J Urol 170(4 Pt 1):1105–1110
Collins S, Ortiz J, Maruffo F et al (2007) Expedited struvite-stone dissolution using a high-flow low-pressure irrigation system. J Endourol 21:1153–1158
Heimbach D, Winter P, Hesse A (1995) When is the indication of percutaneous chemolysis justified? Urol Int 54:157–161
Conflict of interest
All authors declared that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kachrilas, S., Papatsoris, A., Bach, C. et al. The current role of percutaneous chemolysis in the management of urolithiasis: review and results. Urolithiasis 41, 323–326 (2013). https://doi.org/10.1007/s00240-013-0575-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-013-0575-6