Abstract
Use of extracorporeal lithotripsy is declining in North America and many European countries despite international guidelines advocating it as a first-line therapy. Traditionally, lithotripsy is thought to have poor efficacy at treating lower pole renal stones. We evaluated the success rates of lithotripsy for lower pole renal stones in our unit. 50 patients with lower pole kidney stones ≤15 mm treated between 3/5/11 and 19/4/12 were included in the study. Patients received lithotripsy on a fixed-site Storz Modulith SLX F2 lithotripter according to a standard protocol. Clinical success was defined as stone-free status or asymptomatic clinically insignificant residual fragments (CIRFs) ≤3 mm at radiological follow-up. The mean stone size was 7.8 mm. The majority of stones (66 %) were between 5 and 10 mm. 28 % of stones were between 10 and 15 mm. For solitary lower pole stones complete stone clearance was achieved in 63 %. Total stone clearance including those with CIRFs was achieved in 81 % of patients. As expected, for those with multiple lower pole stones the success rates were lower: complete clearance was observed in 39 % and combined clearance including those with CIRFs was 56 %. Overall, complete stone clearance was observed in 54 % of patients and clearance with CIRFs was achieved in 72 % of patients. Success rate could not be attributed to age, stone size or gender. Our outcome data for the treatment of lower pole renal stones (≤15 mm) compare favourably with the literature. With this level of stone clearance, a non-invasive, outpatient-based treatment like lithotripsy should remain the first-line treatment option for lower pole stones. Ureteroscopy must prove that it is significantly better either in terms of clinical outcome or patient satisfaction to justify replacing lithotripsy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracorporeal shockwave lithotripsy (ESWL) is considered a safe and effective intervention for renal stones. However, the rate of stone clearance by ESWL is affected by a number of factors, namely body habitus, stone composition, size and location [1]. Stones in the lower pole can be challenging to treat as stone fragments created by ESWL are more likely to remain within the lower pole. Unfavourable anatomical factors such as reduced infundibular width and lower infundibulopelvic angle [2, 3] also reduce clearance rate of lower pole stones. Previous studies have shown efficacy of clearance of lower pole stones to be in the region of 35–54 %, with evidence that only 21 % of stones larger than 10 mm are cleared by ESWL [4–6]. Success rates may be improved with percussion, diuresis and inversion (PDI) techniques [7]. Current guidelines recommend ESWL as the first-line treatment modality for renal stones under 20 mm but there is ongoing debate as to whether ESWL for lower pole stones should carry the same degree of recommendation [8]. Studies have shown that ESWL is associated with fewer complications and a higher level of patient satisfaction compared to ureteroscopy and percutaneous nephrolithotomy (PCNL) [4, 5, 9]. Although PCNL is more effective at clearing stones of 10–20 mm (72–92 % clearance) compared with ESWL (21–44 % clearance), prospective and retrospective studies both show a significantly longer hospital stay, more morbidity and higher complication rate with PCNL [9, 10]. Ureteroscopy does not have the limitations of reduced efficacy with body habitus [11] but still carries the risks of a general anaesthetic. Given the on-going debate surrounding the best treatment modality for lower pole stones, further information is needed to inform patients on efficacy of clearance with ESWL in routine clinical practice. We have evaluated the effectiveness of ESWL with a retrospective study of 50 patients who underwent ESWL to lower pole stones ≤15 mm in size. The aims were to report the outcomes of a contemporary series of lower pole stones treated with ESWL to improve informed decision making for these patients.
Patients and methods
The study included 50 patients with radiologically proven, symptomatic, lower pole renal calculi measuring ≤15 mm. Patients with an abnormal renal collecting system anatomy (e.g. horseshoe kidney, duplex system, calyceal diverticulum stone) and those with stents were excluded.
All lithotripsy treatments were carried out on the same Storz Modulith F2 lithotripter by one of two experienced radiographers. All patients were treated in a supine position using fluoroscopic guidance (n = 45) or ultrasound guidance (n = 5). Lithotripsy was delivered at low energy for ~200 shocks to acclimatise the patient and kidney [12] to lithotripsy and then gradually increased to the highest tolerable/maximum recommended intensity at a frequency of 1.5–2 Hz for a maximum of 4,000 shocks. We aimed to deliver 4,000 shocks in each treatment in total but reduced this if the patient could not tolerate the treatment or if the stone was adequately fragmented. This resulted in most treatment times lasting around 35–40 min. Audiovisual distraction was provided via a wall-mounted 32 inch (82 cm) television (Technika) with wireless headphones (Sony) to mitigate any discomfort [13].
Patients with successful fragmentation proven on ultrasonography/CT scanning and/or X-ray of the kidney, ureter and bladder were reviewed at a mean of 57 days after their last treatment. Treatment success was determined by the criteria: asymptomatic; stone-free on X-ray of the kidney, ureter and bladder; or clinically insignificant residual fragment (CIRF ≤3 mm).
Results
Demographics and treatment
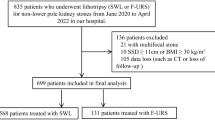
50 patients with lower pole calculi ≤15 mm were treated with ESWL. The demographics of group are typical for stone formers and are summarised in Table 1. The mean stone size was 7.8 mm. The majority of stones were between 5 and 10 mm (66 %), but 28 % of stones were between 10 and 15 mm. Where there were multiple stones the largest stone was taken as the reference size. There was a non-significant trend towards increased treatment numbers and size of stone or multiple stones. Most stones required two or three lithotripsy sessions (Fig. 1).
Outcomes
Overall, complete stone clearance was observed in 54 % of patients and clearance with only CIRFs was achieved in 72 % of patients. Success rate could not be attributed to age or gender (Table 2). Success rate did not decrease significantly with increasing stone size. Those with stone size 10–15 mm had a comparable success rate of 71 % compared with the 73 % success rate of the 5 to <10 mm stone group. For solitary lower pole stones the success rates were higher with complete stone clearance achieved in 63 %. When clearance is defined as including those with CIRFs, as was the case by Albala et al. [4], the clearance rate for solitary stones rises to 81 %. As expected, for those with multiple lower pole stones the success rates were lower. Complete clearance was observed in 39 %. Total clearance rate including those with CIRFs was achieved in 56 % (Table 3).
Discussion
Lithotripsy is a well-established method of stone fragmentation. Since its introduction to clinical practice in the 1980s it has proven to be a valuable non-invasive method of stone treatment [14]. Extracorporeal lithotripsy is recommended as first-line treatment in joint EAU/AUA guidelines in 2007 [15]. In the recent EAU guidelines (2012), ESWL remains a first-line recommendation for small (<10 mm) stones and for larger stones (10–15 mm) where there are “favourable factors for ESWL” [8]. In the UK, the number of lithotripsy cases has been increasing each year over the last decade and exceeds the number of ureteroscopies for stones [16]. However, in North America and other European countries there has been a decline in lithotripsy use and a compensatory rise in the number of ureteroscopies performed. The reason for this change is not clear. Factors may include patient choice, surgeon choice, local success rates, access to lithotripsy and flexible ureteroscopy, and local costs and remuneration systems.
Treatment choice for lower pole stones less than 2 cm remains contentious. Previous landmark studies have suggested that lower pole stones are relatively resistant to lithotripsy. The widely cited lower pole stone papers of Albala et al. [4] and Pearle et al. [17] demonstrated a low success rate (35–37 %) with lithotripsy. Various factors have been correlated with lithotripsy clearance rates including body habitus, infundibulopelvic angle, infundibular width, and stone composition. These factors were not measured in this study and thus are the limitations. However, the data presented represents 50 consecutive unselected lower pole stones, and, because we have access to a fixed-site lithotripter on site, it is our practice to offer these patients lithotripsy as a first-line treatment.
The purpose of our study was not to compare clearance efficacy of lithotripsy to ureteroscopy but to ascertain whether outpatient lithotripsy can achieve high clearance rates in an unselected patient group. Several other studies have compared lithotripsy and ureteroscopy. One randomised trial did not find any difference in clearance rates [17]. Another retrospective series suggested higher clearance rates with ureteroscopy [18]. If the clearance rates and complication rates are comparable, clinicians and patients may need to balance possible small differences in stone clearance and complication rates against the impact of the treatment on their quality of life and also treatment cost. Ureteroscopy, with its associated anaesthetic, urinary tract instrumentation and possible stent insertion may have a greater negative impact on quality of life than lithotripsy. Currently there is insufficient data to answer this. Furthermore, to date, the limited number of studies have not been able to determine which treatment is more cost effective [19, 20]. Clearly, in cases of failed lithotripsy and in those in whom lithotripsy is contraindicated, ureteroscopy and PCNL are necessary treatments. However, given the non-invasive nature of ESWL, it should be considered as initial treatment.
Our average review period was 57 days compared to previous studies that have a review period of 3 months [4, 17, 18]. It may be that longer follow-up may allow time for more of the CIRFs to be eliminated from the kidney. We recognise the importance of continued follow-up of these patients as a significant number of patients with CIRFs after ESWL do need retreatment as time goes on [21]. However, there is no clear evidence as to the significance and natural history of CIRFs left after ESWL compared to those patients who are completely stone free. CIRFs can take 30 months to pass spontaneously, and with increased use of CT scanning for post-treatment evaluation, very small fragments are being picked up that would not have been noticed before on plain radiograph [21, 22].
Our outcome data for the treatment of lower pole renal stones (≤15 mm) compares favourably with the literature [17, 23]. Reasons for this success should be attributed to the dedication of the lithotripsy team in optimising treatment and ensuring accurate targeting, good coupling and appropriate analgesia. With these levels of success, a non-invasive, outpatient-based treatment like lithotripsy should remain a first-line treatment option for lower pole stones. The onus is on ureteroscopy to prove that it is significantly better either in terms of clinical outcome or patient satisfaction to justify replacing lithotripsy.
References
Cortes JA, Motamedinia P, Gupta M (2011) Update on technological and selection factors influencing shockwave lithotripsy of renal stones in adults and children. Curr Opin Urol 21(2):134–140. doi:10.1097/MOU.0b013e3283435c1f
Lin CC, Hsu YS, Chen KK (2008) Predictive factors of lower calyceal stone clearance after extracorporeal shockwave lithotripsy (ESWL): the impact of radiological anatomy. J Chin Med Assoc 71(10):496–501. doi:10.1016/S1726-4901(08)70157-6
Talas H, Kilic O, Tangal S, Safak M (2007) Does lower-pole caliceal anatomy predict stone clearance after shock wave lithotripsy for primary lower-pole nephrolithiasis? Urol Int 79(2):129–132. doi:10.1159/000106325
Albala D, Assimos D, Clayman R, Denstedt J, Grasso M, Gutierrez-Aceves J et al (2001) Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol 166(6):2072–2080. doi:10.1097/00005392-200112000-00014
Pearle MS, Lingeman JE, Leveillee R, Kuo R, Preminger GM, Nadler RB et al (2005) Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol 173(6):2005–2009. doi:10.1097/01.ju.0000158458.51706.56
Sumino Y, Mimata H, Tasaki Y, Ohno H, Hoshino T, Nomura T et al (2002) Predictors of lower pole renal stone clearance after extracorporeal shock wave lithotripsy. J Urol 168(4):1344–1347. doi:10.1097/00005392-200210010-00009
Chiong E, Hwee ST, Kay LM, Liang S, Kamaraj R, Esuvaranathan K (2005) Randomized controlled study of mechanical percussion, diuresis, and inversion therapy to assist passage of lower pole renal calculi after shock wave lithotripsy. Urology 65(6):1070–1074. doi:10.1016/j.urology.2004.12.045
Turk C, Knoll T, Petrik A, Sarica K, Straub M, Seitz C, eds (2012) Guidelines on urolithiasis. 27th Annual EAU Congress, Paris
Preminger G (2006) Management of lower pole renal calculi: shock wave lithotripsy versus percutaneous nephrolithotomy versus flexible ureteroscopy. Urol Res 34(2):108–111. doi:10.1007/s00240-005-0020-6
Havel D, Saussine C, Fath C, Lang H, Faure F, Jacqmin D (1998) Single stones of the lower pole of the kidney. Eur Urol 33(4):396–400. doi:10.1159/000019623
Drăguţescu M, Mulţescu R, Geavlete B, Mihai B, Ceban E, Geavlete P (2012) Impact of obesity on retrograde ureteroscopic approach. J Med Life 5(2):222–225
Handa RK, McAteer JA, Connors BA, Liu Z, Lingeman JE, Evan AP (2012) Optimising an escalating shockwave amplitude treatment strategy to protect the kidney from injury during shockwave lithotripsy. BJU Int 110:E1041–E1047. doi:10.1111/j.1464-410X.2012.11207.x
Marsdin E, Noble JG, Reynard JM, Turney BW (2012) Audiovisual distraction reduces pain perception during shockwave lithotripsy. J Endourol 26(5):531–534. doi:10.1089/end.2011.0430
Chaussy C, Schmiedt E, Jocham D, Schüller J, Liedl B (1984) Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology 23(5, Suppl):59–66. doi:10.1016/0090-4295(84)90243-7
Preminger G, Tiselius H, Assimos D, Alken P, Buck C, Gallucci M et al (2007) 2007 Guideline for the management of ureteral calculi. J Urol 178(6):2418–2434. doi:10.1016/j.juro.2007.09.107
Turney BW, Reynard JM, Noble JG, Keoghane SR (2011) Trends in urological stone disease. BJU Int 109(7):1082–1087. doi:10.1111/j.1464-410X.2011.10495.x
Pearle M, Lingeman J, Leveillee R, Kuo R, Preminger G, Nadler R et al (2005) Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol 173(6):2005–2009. doi:10.1097/01.ju.0000158458.51706.56
El-Nahas AR, Ibrahim HM, Youssef RF, Sheir KZ (2012) Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10–20 mm. BJU Int 110(6):898–902. doi:10.1111/j.1464-410X.2012.10961.x
Matlaga BR, Jansen JP, Meckley LM, Byrne TW, Lingeman JE (2012) Economic outcomes of treatment for ureteral and renal stones: a systematic literature review. J Urol 188(2):449–454. doi:10.1016/j.juro.2012.04.008
Koo V, Young M, Thompson T, Duggan B (2011) Cost-effectiveness and efficiency of shockwave lithotripsy vs flexible ureteroscopic holmium:yttrium-aluminium-garnet laser lithotripsy in the treatment of lower pole renal calculi. BJU Int 108(11):1913–1916. doi:10.1111/j.1464-410X.2011.10172.x
Khaitan A, Gupta NP, Hemal AK, Dogra PN, Seth A, Aron M (2002) Post-ESWL, clinically insignificant residual stones: reality or myth? Urology 59(1):20–24. doi:10.1016/S0090-4295(01)01494-7
Delvecchio FC, Preminger GM (2000) Management of residual stones. Urol Clin North Am 27(2):347–354. doi:10.1016/S0094-0143(05)70263-9
Alanee S, Ugarte R, Monga M (2010) The effectiveness of shock wave lithotripters: a case matched comparison. J Urol 184(6):2364–2367. doi:10.1016/j.juro.2010.08.023
Acknowledgments
We would like to thank Jackie Redgwell, Fiona Barber, Mandy Spencer and Paul Martin for help with collection of data for this study and delivering the lithotripsy service.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cui, H., Thomee, E., Noble, J.G. et al. Efficacy of the lithotripsy in treating lower pole renal stones. Urolithiasis 41, 231–234 (2013). https://doi.org/10.1007/s00240-013-0549-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-013-0549-8