Abstract
The aim of this study was to assess the efficacy of desmopressin nasal spray compared with diclofenac given intramuscularly in patients with acute renal colic caused by urolithiasis. The study included 72 patients randomized into three different groups: group A received desmopressin (40 mg, nasal spray), group B diclofenac (75 mg) intramuscularly and group C, both desmopressin and diclofenac. Pain was assessed using a visual analogue scale at baseline, 10, 30 min and 1 h after administering the treatments. Rescue analgesia was given at 30 min if needed. On admission, the pain level was the same in all three groups (group A 85; and group B and C 90 each). At 10 min the pain decreased minimally in all the groups but more in group B and C (group A 80 and group B and C 70 each). At 30 min pain scores were 75, 37.5 and 40 for group A, B and C, respectively, indicating that there was no significant pain relief in desmopressin group. Rescue analgesic had to be given to all patients in group A and two patients in group B and three patients in group C. Pain relief in the desmopressin only group was significantly less at 1 h even after rescue analgesia (pain scores of 27.5, 15 and 20 for group A, B and C respectively). Intranasal desmopressin is not an effective analgesic in renal colic: exerts mild analgesic effect over a period of 30 min. It does not potentiate the effect of diclofenac.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal colic is caused by an increase in pelvi-ureteric pressure secondary to an obstruction of the urinary tract. This increase in pressure causes a prostaglandin (PG)-mediated increase in renal blood flow and a subsequent increase in diuresis which, in turn, further increases intrapelvic pressure, leading to more pain [1]. Modulation of antidiuretic hormone (ADH) is probably one of the most important mechanisms leading to an increased diuresis [2] and one of the roles of PGs seems to be blocking the action of ADH by interfering with cAMP-mediated signal transmission [3]. Non-steroidal anti-inflammatory drugs (NSAIDs), one of the drugs of choice in acute renal colic, acts by inhibiting PG synthesis. Along with the inhibition of stimulation of ureteric smooth muscles, they also reduce intrapelvic pressure by blocking PG-mediated afferent arteriolar vasodilatation and disrupting the antidiuretic hormone dependent concentrating mechanism [4]. A clinical study demonstrated that the effect of the prostaglandin synthesis inhibitor, indomethacin, on ureteral colic is better when the plasma level of antidiuretic hormone is high [5]. Hence, ADH-induced decrease in diuresis and reduced intrapelvic pressure is suggested to be a possible treatment option in acute renal colic [5].
Desmopressin (1-desamino-8-d-arginine vasopressin) is a synthetic structural analogue of antidiuretic hormone. Compared with ADH: it has a greater antidiuretic effect, a longer duration of action and reduced vasopressor activity. The marked antidiuretic effect of desmopressin is probably responsible for its efficacy in the treatment of renal colic [2].
To assess the efficacy of intranasal desmopressin in relieving the pain of renal colic caused by urolithiasis, we compared the analgesic efficacy of this drug with the most widely used NSAIDs in renal colic, intramuscular diclofenac. We also compared desmopressin alone with desmopressin plus diclofenac to see whether desmopressin has got any additive pain relief effect to diclofenac.
Patients and methods
A total of 72 patients presenting to the emergency department with the diagnosis of acute renal colic because of stone disease were included in this study. The diagnosis of renal colic was based on history, physical examination, urine analysis, ultrasound kidney ureter and bladder (KUB), X Ray KUB or NCCT KUB depending upon the requirement. Patients with evidence of high blood pressure, coronary disease, rhinitis, influenza, peptic ulcer, renal or liver failure or on anticoagulant therapy were excluded from the study, as were any pregnant women. No patient received analgesics before entering the study.
The patients were randomly assigned to three equal groups by Randomisation Block Design method: group A received desmopressin 40 μgm intranasally, group B diclofenac 75 mg intramuscularly and group C, both desmopressin and diclofenac simultaneously. Treatment was given as mentioned in the blocks in a chronological order.
The pain intensity at presentation was assessed and recorded on a 10-cm linear vertical visual analogue scale (VAS) ranging from ‘no pain’ to ‘unbearable pain’, with values recorded to the nearest millimetre. It was explained to the patient, in native language, how to use the visual analogue score to describe the pain intensity in numbers. The pain was assessed on admission, and at 10, 30 min and 1 h after therapy was administered. In patients who had no satisfactory pain relief at 30 min, a second treatment (rescue analgesia) was given, according to the following pre-established protocol: group A, diclofenac 75 mg intramuscular; group B, desmopressin 40 μg intranasal; and group C, tramadol (50 mg) im. If the pain persisted even after 30 min of rescue analgesia, intramuscular injection of 100 mg pethidine was prescribed and the patient was admitted to the urology ward. Intravenous fluids were not given during first 1 h of the study, and the patients were allowed just enough oral fluids to satisfy thirst, limiting the fluid intake. Results of the visual analogue score were recorded by the treating physician. Any adverse reactions were recorded. The final outcome was assessed qualitatively by the patients as ‘relieved’, ‘better’, ‘same’ or ‘worse.’
Descriptive estimates were calculated as mean, median and standard deviation. Frequencies and proportions were calculated for qualitative variables. Chi-square test of independence (with Fisher exact test if required) was used to see association of intervention groups with various categorical variables. Visual analogue scale for pain was compared among three groups using non-parametric Kruskal–Wallis test followed by post hoc analysis. Comparative analysis between any two groups was done using independent t-test or Mann–Whitney U test. All statistical tests were two-tailed and p values of <0.05 were taken as significant.
Results
A total of 72 patients with acute renal/ureteric colic received treatment in three equally divided treatment arms. All three groups are statistically comparable with respect to age, sex distribution, leukocyte count and renal function.
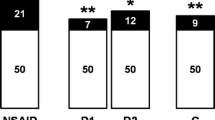
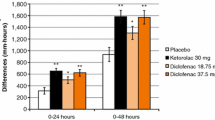
Median pain score at admission for group A patients was 85, and that of group B and C were 90 each and these were not statistically different (Table 1). Ten minutes after administration of therapy, pain scores reduced to 80 in group A, 70 in both group B and group C. Pain scores were again analysed after 30 min and the values were 75, 37.5 and 40 for group A, B and C respectively, indicating that satisfactory pain relief was not achieved in group A, i.e. desmopressin-only group. Hence, 2nd analgesic in the form of inj diclofenac 75 mg were given to all patients in group A, two patients in group B and three patients in group C. Pain score analysed at 1 h was found to be 27.5, 15 and 20 for group A, B and C, respectively.
After 10 min and 30 min
When pain relief at 10 min was compared between three groups, the pain relief was statistically significantly more in diclofenac only or combination group compared with vasopressin-only group; [p 0.001 (between A and B) and 0.008 (between A and C)]. There was a trend of difference between group B and group C (p = 0.059). This difference in pain relief with desmopressin and other two groups was there even at 30 min (p = 0.001 between A and B, and A and C), but there was no difference between group B and C (p = 0.098) (Fig. 1).
After 1 h
After 1 h, per cent change in pain scores in group A was 64.16 and there in group B and C was 84.46 and 78.59, respectively. All the patients in vasopressin-only group needed rescue analgesia and though pain decreased significantly in group A after administration of 2nd analgesic, it was not sufficient enough as a clinically effective analgesia in many patients. There was significant difference in pain relief between group A and both group B/C (p = 0.001 each).
Discussion
After intranasal application of desmopressin to patients with renal colic pain reduction was achieved to a mean of only 10 after 10 min of administration. If it was followed for another 30 min the mean pain was reduced to only 5 on the VAS. The percentage change in pain after intranasal desmopressin was 9.78 and 18.79 only after 10 and 30 min of application. The VAS in desmopressin-only group was significantly higher compared to diclofenac/combination group at 10 and 30 min. In none of the patients desmopressin achieved satisfactory pain relief after 30 min of application and all patients required 2nd rescue analgesic in the form of intramuscular diclofenac. This indicates that group A drug, i.e. desmopressin is not an effective analgesic in itself or when compared with diclofenac in renal colic. Pain reduction if any, attributed to desmopressin was mild in nature.
After application of rescue analgesia, there was considerable pain relief at 1 h, but VAS was still significantly higher in the desmopressin-only group compared with the other two groups. This indicates that addition of 2nd analgesic does not bring the pain scores to statistically significant level in desmopressin-only group. There was no significant difference in pain relief (VAS) at any time in groups treated with diclofenac only or combination of diclofenac and intranasal vasopressin; this means that combination of desmopressin adds no advantage to the degree and completeness of pain reduction to diclofenac-alone group. Moreover although statistically not significant, only 8.3% patients of group B (diclofenac only group) required 2nd analgesic, whereas 12.5% patients were given 2nd analgesic in group C (diclofenac and desmopressin). So desmopressin again dose not reduce the frequency of administration of 2nd analgesic.
Sherif et al. [2] in their study found that 54% patients had incomplete pain relief after desmopressin intranasal spray. In this study amongst the patients who received intranasal desmopressin and continued to complain of pain severe enough to require further analgesics (mean visual analogue scores 62 ± 27 mm) 90% had complete pain relief following the administration of second analgesic in the form of 50 mg intramuscular diclofenac sodium. They demonstrated that the administration of 40 μg of intranasal desmopressin spray resulted in a prompt and significant decrease in renal colic intensity, which was significant at 10, 20 and 30 min (p < 0.01, <0.001 and <0.001 respectively). Of the 18 patients, 8 (44.4%) had complete pain relief after administration of 40 μg desmopressin and did not require further analgesia.
Lopes et al. [6] also showed that treatment with intranasal desmopressin 40 μg induced prompt pain relief with significant decreases in pain scores after only 10 min. This effect was maintained at 20 min and then decreased slightly.
This apparently insignificant analgesic effect of desmopressin in our study population can be attributed to several causes. First, possibility of delayed absorption of intranasal desmopresin. Seif et al. [7] found that peak plasma level of desmopressin occurred in 0.5–4 h after intranasal administration, indicating that the drug is slowly absorbed from nasal mucosa. We did not wait more than 30 min for pain relief in any patient and rescue analgesia was given, so effect of any possible delayed absorption cannot be commented upon. Second, it may be due to the individual variations in absorption of intranasal of desmopressin because of genetic polymorphisms. Desmopressin is a synthetic analogue of vasopressin that acts through G protein coupled receptor that increases intracellular cyclic AMP (cAMP), thereby inducing translocation of aquaporin water channel in the apical membrane. A growing number of variations in the G protein coupled receptors, i.e. genetic polymorphisms have been documented. Studies by Rana et al. [8] have uncovered functional importance of these polymorphisms. According to their studies, genetic polymorphisms have significant impacts on variations of drug action in different individuals. The analgesic action of desmopressin is dependent upon its antidiuretic action which is again a function of intrinsic renal reserve of an individual. This could be another explanation to its differential actions. Last, it may be because of improper administration of intranasal desmopressin. Because manual spray is not standardised, inadequate doses may be delivered intranasally to a patient; which may not produce the desired effects. Although it was administered under guidance of trained health care personnel only, this possibility in some cases cannot be ruled out fully. This could have been ruled out only it was administered by a single researcher. We believe that this is a limitation of our study.
Earlier studies indicated intranasal desmopressin as an effective and safe therapy in acute renal colic. Our study, the largest study of desmopressin in renal colic in Indian population showed only mild analgesic effect when used alone and no potentiating effect with NSAIDs. Moreover, desmopressin is ten times costlier than NSAID and has different absorption because of reasons cited above. However it was safe and can be used as a mild analgesic in patients in whom NSAIDs are contraindicated because of impaired renal function.
Conclusions
The result of this study suggests that desmopressin is not an effective analgesic in renal colic as it exerts mild analgesic effect over a period of 30 min. In view of agonising nature of renal colic, more effective and rapidly acting analgesics in the form of NSAIDs or opioids are more appropriate than desmopressin alone. Chance of varied and delayed absorption, higher cost and lack of safety profiles amongst elderly and those with deranged electrolytes is another deterrent for its use. It may be used as a supplemental analgesic in patients when NSAIDs are contraindicated or have potentially serious side effects. Because of increasing concern about the nephrotoxicity of prostaglandin synthetase inhibitors, further studies are required to investigate the effect of desmopressin combined with other analgesics such as tramadol or spasmolytics.
References
Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (2007) Campbell-Walsh urology, 9th edn. Elsevier, Philadelphia, p 1213
El-Sherif AE, Salem M, Yahia H, al-Sharkawy WA, al-Sayra M (1995) Treatment of renal colic by desmopressin intranasal spray and diclofenac sodium. J Urol 153:1395–1398
Marumo F, Edelman IS (1971) Effect of Ca ++ and prostaglandin E1 on vasopressin activation of renal adenyl cyclase. J Clin Invest 50:1613–1620
Grantham JJ, Orloff J (1968) Effect of prostaglandin E1 on the permeability response of the isolated collecting tubule to vasopressin, adenosine 3,5-monophosphate and theophylline. J Clin Invest 47:1154
Grenabo L, Aurell M, Delin K, Holmlund D, Sjadin LG (1983) Antidiuretic hormone levels and the effect of indomethacin on ureteral colic. J Urol 129:941–943
Lopes T, Dias JS, Marchlero J (2001) An assessment of clinical efficacy of intranasal desmopressin spray in the treatment of renal colic. BJU Intern 87:322–325
Seif SM, Zenser TV, Clarochi FF, Davis BB, Robinson AG (1978) DDAVP (1-desamino-8-arginine-vasopressin) treatment of central diabetes incipidus- mechanism of prolonged antidiauresis. J Clin Endocr Metab 46:381–388
Rana BK, Shiina T, Insel PA (2001) Genetic variations and polymorphisms of G protein coupled receptors functional and therapeutic implications. Annu Rev Pharmacol Toxicol 41(2):593
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, S., Behera, N.C., Sarkar, D. et al. A comparative assessment of the clinical efficacy of intranasal desmopressin spray and diclofenac in the treatment of renal colic. Urol Res 39, 397–400 (2011). https://doi.org/10.1007/s00240-010-0354-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-010-0354-6