Abstract
The aim of this study is to investigate the serum levels of parathyroid hormone (PTH), calcitonin, 1,25 (OH)2 vitamin D3, estradiol and testosterone in male patients with active renal calcium stone disease compared with controls and investigate their relationship with serum/urinary biochemistry. Male active renal calcium stone formers (ASF) were enrolled from December 2008 to April 2009. Controls were selected from age and sex matched individuals. Two 24-h urine samples and a blood sample were withdrawn from each participant while they were on free diet. Serum 1,25 (OH)2 vitamin D3 levels in the ASF and control groups were 127 ± 40 and 93 ± 35 pmol/l (p < 0.001). Serum levels of PTH, calcitonin, estradiol and testosterone were not statistically different between the ASF and control groups (all p > 0.05). Serum 1,25 (OH)2 vitamin D3 was associated with higher urinary excretion of calcium and phosphorus in ASF patients. Serum levels of calcitonin were related to less urinary excretion of calcium in the control group. Serum testosterone was related to higher urinary excretion of uric acid in ASF patients and to higher urinary excretion of oxalate in the control group. 1,25 (OH)2 Vitamin D3 is an important hormone in the pathogenesis of recurrent renal calcium stone disease and could increase renal stone risk by increasing the urinary excretion of calcium and phosphorus. There is a possibility of testosterone involvement in the pathogenesis of renal stones through higher urinary uric acid and oxalate excretion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal calcium stones represent more than 80% of kidney stones [1]. Different metabolic, anatomic, nutritional, genetic and environmental factors are involved in the pathogenesis of renal calcium stones [2–6]. Hypercalciuria is considered as an important factor contributing to the formation of calcium based kidney stones [7]. Therefore, hormones involved in calcium homeostasis were one of the early factors that were investigated in urinary stone pathogenesis. Hormones can modulate their effect through changes in their serum levels or in the sensitivity or activity of their receptors. Several studies have been published on the relationship of the serum levels of parathyroid hormone (PTH), calcitonin and vitamin D with kidney calcium stone disease.
Studies on PTH were mainly focused on kidney stones in hyperparathyroidism. In the few published studies about idiopathic renal stone formers, no relationship was reported between serum PTH and calcium stone disease [8–10]. Serum levels of calcitonin in active calcium stone disease have not been fully investigated [11–13]. Few published studies reported an association between serum calcitonin and calcium stone disease [13, 14]. Several studies investigated the relationship of vitamin D levels in serum with calcium stone disease. Some studies observed an association between serum vitamin D and urinary calcium and uric acid excretion [8, 15]. Other studies have failed to repeat such observations [15–17]. Since the serum levels of vitamin D is dependent on sunlight [18], we think that the significance of vitamin D contribution to calcium stone pathogenesis could be regionally dependent. Studies on the association of vitamin D with renal stones in the Middle East are scant.
As the prevalence of renal stones is different in males and females [19, 20], some studies have focused on the possible role of sexual hormones and their receptors in renal calcium stone disease. In animal studies serum estradiol was associated with increased urinary citrate and decreased urinary oxalate excretion [19, 21, 22] and castration in males was also associated with lower urinary oxalate excretion [2]. The clinical relevance of these observations in human subjects remains to be further elucidated.
In the Tehran Stone Study, we aimed at studying the hormonal profile of 1,25 (OH)2 vitamin D3, PTH, calcitonin, estradiol and testosterone and variations in their receptor genes in active stone formers versus normal controls. To the best of our knowledge, few studies have evaluated this complete set of hormones in a single study and such studies have not been completed in an endemic area for kidney stones such as Iran. We have presented the hormonal profile section of this study in this article.
Materials and methods
Subjects and settings
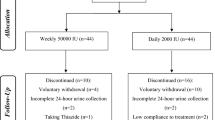
Male active stone formers (ASF) who were referred to the Labbafinejad Hospital urology clinic from December 2008 to April 2009 and agreed to participate and met the inclusion criteria were enrolled. The study protocol aimed at enrolling 109 ASF patients and 109 controls. ASF was defined as a patient with at least two episodes of stone relapse or increase in stone size during the previous 5 years. Inclusion criteria were: male gender, age of 30–55 years, absence of adrenal, hypophyseal or any systemic diseases such as sarcoidosis that alter calcium homeostasis, absence of cardiovascular, gastrointestinal, hepatic or renal disease. Patients with non-calcium stones, current use of medications namely calcium tablets, vitamin D, levothyroxine, lithium, hormonal medications, diuretics, antiacids, vitamin C, H2 blockers, probenecid, allopurinol, indinavir, obesity (body mass index > 30), positive urine culture and patients with anatomical anomalies of the urinary tract were excluded from the study. The exclusion of non-calcium stone formers was based on either the stone analysis report or, if not available, the radiological appearance of the stone in KUB films.
The controls were selected from similar age range and gender matched persons. The individuals were excluded from the control group if there was a positive history of urinary stone disease in them, their relatives, or if abdominal ultrasonography revealed the presence of urinary stones. The same exclusion criteria defined for the patients was also applied for the controls.
Blood and urinary sampling and analysis
Two 24-h urine collections and a blood sample were obtained from each subject. Participants were on a free diet with no restriction of their sodium or calcium intake when they were evaluated. Urine and blood samples were used to determine the blood, urinary biochemistry and serum hormonal levels. Serum biochemistry constituted total and ionized calcium, urea, creatinine, sodium, phosphorus, chloride, potassium, uric acid, bicarbonate and pH. The 24-h urinary biochemistry comprised phosphorus, creatinine, calcium, oxalate, sodium, uric acid, magnesium, urea, chloride, citrate and potassium. Hormonal profile investigation included PTH, calcitonin, 1,25 (OH)2 vitamin D3, estradiol and testosterone. The measurement of serum and urinary calcium, phosphorous and creatinine concentrations was carried out using selectra E autoanalyser (Vitalab, Merck, Germany). Urinary oxalate and citrate concentrations were measured by an enzymatic colorimetric method using standard kits (LTA s.r.l, Milan, Italy).
Serum PTH, testesterone and estradiol were measured by electrochemiluminescent method. (Elecsys 2010 automatic analyzer, Roche Hitachi) The concentration of calcitonin was evaluated by ELISA method (IBL international GMBH). Serum 1,25 (OH)2 vitamin D3 measurement was performed by EIA Kit (IDS Ltd, UK) in which the first step is immunoextraction, followed by quantification completed by enzyme immunoassay.
Statistical analysis
SPSS ver. 16.0 software was used to enter and analyze the data subsequently. Logarithmic transformations of serum PTH, testosterone, calcitonin, urinary creatinine, calcium, oxalate, sodium, uric acid, chloride and citrate were used to make a near normal distribution. Other variables were analyzed without transformation. Independent samples t test was used to compare quantitative variables between the ASF and control groups. To exclude the confounding effect of age, a logistic regression model was employed in which age was entered to the model and in the second step, predictor variables were introduced to the model. Bivariable scatter plots were used to judge the presence of evident nonlinear relationship between serum hormones and serum/urinary biochemistry. Pearson correlation coefficient was used to test the relationship of the serum levels of PTH, testosterone, calcitonin, estradiol and testosterone with serum or urinary biochemicals separately in ASF patients and controls. Two-sided p values less than 0.05 were considered statistically significant. In case of multiple comparisons, Bonferroni’s adjustment for α was employed.
Results
106 ASFs and 109 controls were enrolled as final eligible candidates during the study period (3 ASF subjects were excluded because of inadequate blood/urinary samples). The mean ± SD of age in ASF and the control subjects were 43.4 ± 6.9 and 38.4 ± 6.9 years, respectively (p < 0.001). The mean ± SD of BMI in ASF and the control subjects were 26.3 ± 2.7 and 25.8 ± 3.0, respectively (p > 0.05). A significant difference was observed between ASF and the control subjects regarding serum vitamin D3 and urinary 24-h calcium, oxalate, uric acid and citrate (Table 1). Mean (range) of serum PTH, calcitonin, testosterone, estradiol and 1,25 (OH)2 vitamin D3 in ASF individuals were 48.3 (24–117), 11.6 (0.2–121.9) pg/ml, 5.2 (2.3–13.2) ng/ml, 28.6 (12–45) pg/ml and 126.7 (48–193) pmol/l, respectively. The above figures for the controls were 48.6 (19.5–102), 14.3 (0.2–87.8) pg/ml, 5.7 (2.3–13.6) ng/ml, 30.3 (14–62) pg/ml and 93.1 (40–191) pmol/l, respectively. The comparison of serum hormonal levels with the subjects’ status of stone disease is shown in Fig. 1. The only statistically significant difference was for serum 1,25 (OH)2 vitamin D3 (p < 0.001) and this existed after adjusting for age. The odds ratio for the probability of active calcium stone disease with each pmol/l increase in serum vitamin D3 after adjusting for the effect of age was 1.024 (CI 95% 1.015–1.034).
As several serum and urinary parameters were different between ASF and the control subjects, we tested the hypothesis of association between serum levels of investigated hormones and urinary biochemicals separately in the ASF and the control groups (Table 2).
The associations between serum vitamin D3 and urinary phosphorus, magnesium, calcium, oxalate, uric acid, potassium, sodium and chloride, between calcitonin and urinary calcium and citrate, and between testosterone and urinary uric acid were observed in the whole sample of ASFs and the controls. Other associations were only observed in either the ASF or the control groups. As explained in Table 2, after adjusting α for multiple comparisons only the associations of (1) serum 1,25 (OH)2 vitamin D3 with urinary phosphorus, magnesium and calcium in ASF patients, (2) serum calcitonin with urinary calcium in controls, (3) serum testosterone with urinary uric acid in ASF patients and (4) serum testosterone with urinary oxalate in controls were statistically significant.
The associations of age with urinary calcium, citrate and oxalate were also tested (Data not provided). Positive correlation was observed between age and urinary citrate excretion. However, this difference is not statistically significant if we adjust α level for multiple comparisons according to Bonferroni (partial Pearson correlation coefficient after controlling for disease status: r = 0.17, p = 0.02). Furthermore, the associations of age with serum PTH, calcitonin, 1,25 (OH)2 vitamin D3, estradiol and testosterone were evaluated after controlling for disease status. No statistically significant association was observed (all r < 0.1, all p > 0.05).
As supersaturation of urinary CaO x , CaHPO4 and uric acid are confirmed risk factors for calcium stones; we tested the relationship between serum PTH, calcitonin, 1,25 (OH)2 vitamin D3, estradiol and testosterone with urinary supersaturation of the aforementioned crystals. There were statistically significant relationships between the serum levels of 1,25 (OH)2 vitamin D3 and the urinary supersaturation of CaO x (p = 0.001) and CaHPO4 (p < 0.001) after controlling for disease status.
Discussion
The results of the current study confirm that serum vitamin D plays an important role in active idiopathic renal calcium stone disease and suggest a role for calcitonin and testosterone in the pathogenesis of the disease which are covered separately below under respective topics. Patients and controls were similar regarding demographic characteristics except for age. We used age range matching for controls in 10-year intervals. For example, each ASF subject from the 30–39-year age group was matched with a control from the same age range. This can explain the statistically significant difference in age between ASFs and controls. Nevertheless, we cannot exclude the possibility of selection bias.
Vitamin D3
In this study, serum 1,25 (OH)2 vitamin D3 levels were 30% higher in ASF patients compared to the controls (Fig. 1). 1,25 (OH)2 Vitamin D3 was the only investigated hormone that was related to the participants’ status of stone disease. The relationship of vitamin D3 with calcium stone disease has been previously reported in some studies while this relationship was not observed in certain other studies. We think that part of this inconsistency is environmental dependent as different levels of sunlight exposure result in different serum levels of vitamin D3 [18]. In fact, serum levels of 25 OH vitamin D3 were reported to be related to the latitude and seasons of the year [23]. If we consider 39–193 pmol/l as the reference range for serum 1,25-dihydroxyvitamin D [24], no participant in the current study had subnormal serum levels. All subjects’ serum 1,25 (OH)2 vitamin D3 fell within the reference range. The frequency of subnormal serum levels of 25-hydroxyvitamin D in Spanish and Finnish reports were within the range of 26–29% in the healthy adult population [25, 26]. The variation in the serum vitamin D3 in different regions and/or climates may result in varied contributions of vitamin D3 to stone pathogenesis. Other explanations could be the effect of calcium restriction on serum vitamin D3 [16, 27] which was exerted in some studies and polymorphisms in the gene for vitamin D receptor which can result in augmented response to the lower serum levels of vitamin D3 [3–5].
1,25 (OH)2 vitamin D3 was the only hormone in the current study that was associated with several urinary biochemicals (phosphorus, magnesium and calcium after correction by Bonferroni and also with uric acid, potassium and sodium if not considering the correction by Bonferroni). These associations could increase the possibility of calcium stone disease as urinary calcium and phosphorus are risk factors for renal calcium stone formation. The associations of serum vitamin D3 with urinary calcium and uric acid have been previously demonstrated [15]. Moreover, higher excretion of urinary oxalate has been reported after vitamin D3 consumption [28] and a positive association has been observed between the two [8]. In the current study, however, no relationship was observed between serum vitamin D3 and urinary oxalate excretion in either the ASF or the control groups. It should be noted that high intake of calcium in free diet with no restriction on calcium intake, practiced in the current study, could result in lower intestinal absorption of oxalate and less excretion of urinary oxalate [8, 29]. Therefore, it is possible that such a relationship which could be observed in calcium restricted diets has been overlooked in the current study.
Parathyroid hormone
In this study, serum PTH was not related to the status of calcium stone disease. Serum levels of PTH were not related to any serum or urinary biochemistry evaluated in this study. This finding is in accordance with the results of previous studies. It has been suggested that PTH is not directly involved in urinary stone pathogenesis in idiopathic stone formers [30]. Other studies have also reported that serum levels of PTH were not different in renal stone formers versus the controls and between hypercalciuric and normocalciuric stone formers [9, 10].
It does not seem that PTH plays an important role in idiopathic active kidney calcium stone disease.
Calcitonin
In this study serum calcitonin levels were not related to the status of calcium stone disease. A previous study by Fuss et al. [14] reported higher baseline levels of calcitonin in recurrent kidney calcium stone formers who were on a low calcium diet. He reported higher response of calcitonin to calcium infusion in recurrent stone formers. Later D’Angelo et al. [30] demonstrated that the relationship of calcitonin with urinary stones is dependent on calcium intake.
We observed an association between the serum levels of calcitonin and higher urinary excretion of oxalate in the ASF group and less urinary magnesium, calcium and citrate in the controls. After considering Bonferroni’s correction for multiple comparisons, only the association of calcitonin with less urinary excretion of calcium in controls was statistically significant (Table 2). All these associations except for less urinary calcium in the controls can theoretically increase stone formation risk. Since in this study, no restriction was applied on calcium intake it is possible that effects dependent on calcium restriction have been overlooked.
Estradiol
Estrogen has been demonstrated to inhibit bone resorption and increase renal absorption of calcium [31, 32] and urinary citrate levels [19, 21]. In some studies, the possibility of stone prevention after menopause through estrogen supplementation was suggested through decreased urinary saturation of calcium crystals [21, 22], but clinical studies failed to observe decreased incidence of urinary stones in women treated with supplemental exogenous estrogen [33, 34].
In this study, no association was found between serum estradiol levels and the studied urinary risk/protective factors of stone formation. It should be noted that our study population was restricted to men with a narrow window of range for estradiol levels. Nevertheless, it seems that serum estradiol does not play an important role in recurrent idiopathic calcium stone pathogenesis in the male patients.
Testosterone
In the current study, serum levels of testosterone were not associated with the status of renal stone disease. The two to three times higher prevalence of renal stones in males [22] in comparison with females formed the rationale for hypothesizing a possible role for sexual hormones in urinary stone pathogenesis. Animal studies have found that stone incidence severely decreases from 71 down to 14% after castration in ethylene glycol-treated male rats [35, 36]. A human study reported higher levels of testosterone and FSH in stone forming males relative to the controls [37].
In bivariable analyses of the current study, we observed that serum levels of testosterone were related to urinary excretion of uric acid in both the ASF and the control groups and to urinary oxalate excretion in the control group. After implementing Bonferroni’s correction, only the association of testosterone with urinary uric acid in ASF patients and oxalate in controls were statistically significant. Animal studies have confirmed that androgens increase and estrogens decrease urinary and serum oxalate levels and oxalate crystal deposition in rat kidneys [38]. It was observed that estrogen supplementation in castrated rats treated with ethylene glycol did not result in stone formation whereas testosterone supplementation did [38]. Yagisawa et al. studied both castrated and normal male rats also treated with ethylene glycol. They observed less urinary oxalate excretion in castrated male rats [39]. Furthermore, human studies have revealed that in men urinary excretion of uric acid and oxalate is higher than females [40, 41]. Increased urinary excretion of uric acid is another risk factor for calcium stone disease [3] as uric acid can form the nidus for calcium stone formation.
At last the following points should be kept in mind when studying the results of this study. We assert that in this study only male active calcium stone formers were studied and that the results are only pertinent to male patients. We implemented Bonforroni’s correction for multiple comparisons. Such a correction in this study with relatively small sample size makes this study inadequately powered to detect small to moderate differences in serum/urinary biochemicals between study groups.
Conclusion
In this study on a Middle Eastern male population as an endemic area for renal stones, we observed that in adult men aged 30–55-year-old 1,25 (OH)2 vitamin D3 is an important hormone in the pathogenesis of recurrent renal calcium stone disease and could increase renal stone risk by increasing urinary excretion of calcium and phosphorus. There is a possibility of testosterone involvement in the pathogenesis of renal stones through higher urinary uric acid and oxalate excretion.
References
Bihl G, Meyers A (2001) Recurrent renal stone disease-advances in pathogenesis and clinical management. Lancet 358:651–656
Griffin DG (2004) A review of the heritability of idiopathic nephrolithiasis. J Clin Pathol 57:793–796
Mossetti G, Rendina D, Viceconti R, Manno G, Guadagno V, Strazzullo P, Nunziata V (2004) The relationship of 3′ vitamin D receptor haplotypes to urinary supersaturation of calcium oxalate salts and to age at onset and familial prevalence of nephrolithiasis. Nephrol Dial Transplant 19:2259–2265
Relan V, Khullar M, Singh SK, Sharma SK (2004) Association of vitamin D receptor genotypes with calcium excretion in nephrolithiatic subjects in northern India. Urol Res 32:236–240
Scott P, Ouimet D, Valiquette L, Guay G, Proulx Y, Trouve ML, Gagnon B, Bonnardeaux A (1999) Suggestive evidence for a susceptibility gene near the vitamin D receptor locus in idiopathic calcium stone formation. J Am Soc Nephrol 10:1007–1013
Smith LH (1987) Pathogenesis of renal stones. Miner Electrolyte Metab 13:214–219
Robertson WG (1986) Pathophysiology of stone formation. Urol Int 41:329–333
Giannini S, Nobile M, Castrignano R, Pati T, Tasca A, Villi G, Pellegrini F, D’Angelo A (1993) Possible link between vitamin D and hyperoxaluria in patients with renal stone disease. Clin Sci (Lond) 84:51–54
Khanam A, Rahman MA (1993) Parathyroid hormone in urinary stone patients. Mol Cell Biochem 121:1–4
von Lilienfeld-Toal H, Bach D, Hesse A, Franck H, Issa S (1982) Parathyroid hormone is normal in renal stone patients with idiopathic hypercalciuria and high fasting urinary calcium. Urol Res 10:205–207
Chen WC, Wu HC, Lu HF, Chen HY, Tsai FJ (2001) Calcitonin receptor gene polymorphism: a possible genetic marker for patients with calcium oxalate stones. Eur Urol 39:716–719
Goodman HO, Holmes RP, Assimos DG (1995) Genetic factors in calcium oxalate stone disease. J Urol 153:301–307
Shainkin-Kestenbaum R, Winikoff Y, Paran E, Lismer L (1984) The role of calcitonin in calcium stone formation. Nephron 38:154–155
Fuss M, Pepersack T, Corvilain J, Bergmann P, Simon J, Body JJ (1991) Calcitonin secretion in idiopathic renal stone formers. J Bone Miner Res 6:35–38
Jarrar K, Amasheh RA, Graef V, Weidner W (1996) Relationship between 1,25-dihydroxyvitamin-D, calcium and uric acid in urinary stone formers. Urol Int 56:16–20
Gascon-Barre M, D’Amour P, Dufresne L, Perreault JP (1985) Interrelationships between circulating vitamin D metabolites in normocalciuric and hypercalciuric renal stone formers. Ann Nutr Metab 29:289–296
Netelenbos JC, Jongen MJ, van der Vijgh WJ, Lips P, van Ginkel FC (1985) Vitamin D status in urinary calcium stone formation. Arch Intern Med 145:681–684
Ding C, Cicuttini F, Parameswaran V, Burgess J, Quinn S, Jones G (2009) Serum levels of vitamin D, sunlight exposure, and knee cartilage loss in older adults: the Tasmanian older adult cohort study. Arthritis Rheum 60:1381–1389
Hammar ML, Berg GE, Larsson L, Tiselius HG, Varenhorst E (1987) Endocrine changes and urinary citrate excretion. Scand J Urol Nephrol 21:51–53
Johnson CM, Wilson DM, O’Fallon WM, Malek RS, Kurland LT (1979) Renal stone epidemiology: a 25-year study in Rochester, Minnesota. Kidney Int 16:624–631
Dey J, Creighton A, Lindberg JS, Fuselier HA, Kok DJ, Cole FE, Hamm LL (2002) Estrogen replacement increased the citrate and calcium excretion rates in postmenopausal women with recurrent urolithiasis. J Urol 167:169–171
Heller HJ, Sakhaee K, Moe OW, Pak CY (2002) Etiological role of estrogen status in renal stone formation. J Urol 168:1923–1927
Holick MF (1995) Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr 61:638S–645S
Group LLS (2006) Laboratory test information guide. London Health Sciences Centre, London
Calatayud M, Jodar E, Sanchez R, Guadalix S, Hawkins F (2009) Prevalence of deficient and insufficient vitamin D levels in a young healthy population. Endocrinol Nutr 56:164–169
Lamberg-Allardt CJ, Outila TA, Karkkainen MU, Rita HJ, Valsta LM (2001) Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe? J Bone Miner Res 16:2066–2073
Adams ND, Gray RW, Lemann J Jr (1979) The effects of oral CaCO3 loading and dietary calcium deprivation on plasma 1,25-dihydroxyvitamin D concentrations in healthy adults. J Clin Endocrinol Metab 48:1008–1016
Erickson SB, Cooper K, Broadus AE, Smith LH, Werness PG, Binder HJ, Dobbins JW (1984) Oxalate absorption and postprandial urine supersaturation in an experimental human model of absorptive hypercalciuria. Clin Sci (Lond) 67:131–138
Lindsjo M, Danielson BG, Fellstrom B, Norheim I, Wide L, Ljunghall S (1992) Parathyroid function in relation to intestinal function and renal calcium reabsorption in patients with nephrolithiasis. Scand J Urol Nephrol 26:55–64
D’Angelo A, Calo L, Cantaro S, Giannini S (1997) Calciotropic hormones and nephrolithiasis. Miner Electrolyte Metab 23:269–272
McKane WR, Khosla S, Burritt MF, Kao PC, Wilson DM, Ory SJ, Riggs BL (1995) Mechanism of renal calcium conservation with estrogen replacement therapy in women in early postmenopause—a clinical research center study. J Clin Endocrinol Metab 80:3458–3464
Nordin BE, Need AG, Morris HA, Horowitz M (1999) Biochemical variables in pre- and postmenopausal women: reconciling the calcium and estrogen hypotheses. Osteoporos Int 9:351–357
Domrongkitchaiporn S, Ongphiphadhanakul B, Stitchantrakul W, Chansirikarn S, Puavilai G, Rajatanavin R (2002) Risk of calcium oxalate nephrolithiasis in postmenopausal women supplemented with calcium or combined calcium and estrogen. Maturitas 41:149–156
Mattix Kramer HJ, Grodstein F, Stampfer MJ, Curhan GC (2003) Menopause and postmenopausal hormone use and risk of incident kidney stones. J Am Soc Nephrol 14:1272–1277
Lee YH, Huang WC, Chiang H, Chen MT, Huang JK, Chang LS (1992) Determinant role of testosterone in the pathogenesis of urolithiasis in rats. J Urol 147:1134–1138
Lee YH, Huang WC, Huang JK, Chang LS (1996) Testosterone enhances whereas estrogen inhibits calcium oxalate stone formation in ethylene glycol treated rats. J Urol 156:502–505
Kuczera M, Kiersztejn M, Kokot F, Klin M (1993) Behavior of sex hormone and gonadotropin secretion in men with active nephrolithiasis. Endokrynol Pol 44:539–547
Fan J, Chandhoke PS, Grampsas SA (1999) Role of sex hormones in experimental calcium oxalate nephrolithiasis. J Am Soc Nephrol 10(Suppl 14):S376–380
Yagisawa T, Ito F, Osaka Y, Amano H, Kobayashi C, Toma H (2001) The influence of sex hormones on renal osteopontin expression and urinary constituents in experimental urolithiasis. J Urol 166:1078–1082
Curhan GC, Willett WC, Speizer FE, Stampfer MJ (2001) Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int 59:2290–2298
Parks JH, Coe FL (1986) A urinary calcium-citrate index for the evaluation of nephrolithiasis. Kidney Int 30:85–90
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shakhssalim, N., Roohi Gilani, K., Parvin, M. et al. An assessment of parathyroid hormone, calcitonin, 1,25 (OH)2 vitamin D3, estradiol and testosterone in men with active calcium stone disease and evaluation of its biochemical risk factors. Urol Res 39, 1–7 (2011). https://doi.org/10.1007/s00240-010-0276-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-010-0276-3