Abstract
We present our experience with the use of the ureteral access sheath for the management of small impacted lower third ureteral stones, in comparison with more standard techniques. Ninety-eight consecutive patients, aged 18–73 years (mean 48.5), with small (diameter < or =10 mm) impacted lower third ureteral stones (<5 mm in 56, and 5–10 mm in 42 patients) were randomly managed with either a 12/14F coaxial ureteral dilator/sheath and a 7.5F flexible ureteroscope (group A; 48 patients), or with balloon dilatation and the 7.5F flexible ureteroscope (group B; 50 patients). In both groups, stones were grasped and extracted with a basket, and when necessary they were disintegrated with a 1.9F electrohydraulic lithotripsy (EHL) probe. Postoperatively, excretory urography was performed at 1 month and patients were followed-up for 1 year. The mean operative time was 45.5 min in group A, and 58.5 min in group B (P<0.05). EHL was performed in 16 (33.3%) patients of group A, and in 12 (24%) patients of group B. In group B, balloon dilatation was performed in 28 (56%) patients. Ureteral perforation was revealed in 4 (8%) patients of group B. The follow-up imaging tests showed stone-free status in 46 (95.8%) patients of group A and in all (100%) patients of group B. No long-term complications were recorded. Endoscopic management of small impacted lower third ureteral stones with the ureteral access sheath is a quicker and safer procedure, in comparison with the more standard approach, bearing comparable efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impacted ureteral stones, which are defined as calculi remaining at the same position for more than 2 months and not moving in response to ureteral catheterization, are extremely difficult to treat [1–3]. They respond poorly to extracorporeal shockwave lithotripsy (SWL) and they are usually managed with ureteroscopy and stone disintegration [1, 2]. However, fragments may remain in the ureter (usually at the lower third), even after successful stone breakage, resulting in renal impairment and infection, even if they are less than 4 mm in diameter [3]. Hence, complete removal of impacted calculi should be successful from the very beginning in one endoscopic procedure. Herein, we present our 3-year experience with the ureteral access sheath for the management of small impacted lower third ureteral stones.
Patients and methods
Between January 2001 and December 2004, 98 consecutive patients (58 men and 40 women, aged 18–73 years old; mean age 48.5), with small (diameter ≤10 mm) impacted unilateral lower third ureteral calculi, were randomly allocated to undergo retrograde endoscopic treatment with (48 patients; group A) or without (50 patients; group B) the aid of the ureteral access sheath. In 56 patients (30 and 26 of group A and B, respectively) the stones were <5 mm in diameter and in the remaining 42 patients the diameter of the stone was 5–10 mm. The mean duration of impaction was 2.7 months (range 2–3.5), according to clinical history and findings on plain X-ray and/or intravenous urography (IVU). Mild to moderate hydronephrosis was diagnosed in 42 (87.5%) patients of group A and in 46 (92%) patients of group B. The study was approved by the Ethical Committee of our Hospital, and all patients gave their written consent.
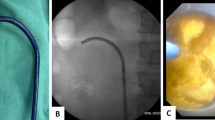
Under epidural anesthesia, patients were placed in the dorsal lithotomy position. A 0.035-in. floppy-tip guidewire was inserted into the ureteral orifice and was advanced, under fluoroscopic guidance, at least to the level of the impacted stone (if possible above the stone). In group A, a 20-cm kink-resistant, hydrophylically coated 12/14F coaxial ureteral dilator/sheath (Applied Medical, Athens, Greece) was forwarded over the guidewire and was positioned just below the lower edge of the stone. The 12F inner dilator was removed, leaving the open-ended sheath in the ureter with the guidewire running through the sheath lumen. A 7.5F flexible ureteroscope was then advanced through the sheath, under direct vision beside the guidewire. Thereafter, attempts were made for stones to be retracted into the sheath lumen with the basket. In particular, a flexible two-prong grasper was used in order to disrupt the mucosa overlying the stone and visualize the latter. Irrigant injection of sterile water was administered as an additional disimpaction maneuver. A 0-tip basket was used to entrap and extract the calculus. When intact extraction was not achieved, stones were disintegrated into smaller pieces with a 1.9F electrohydraulic lithotripsy (EHL) probe. In group B, balloon dilatation of the ureter was performed when necessary, according to the preference of the surgeon.
After successful stone management in both groups, the guidewire was advanced to the renal pelvis, and a double-J stent was left in situ at the end of the procedure to ensure postoperative drainage for approximately 1 week. Postoperative plain X-rays were taken immediately (for confirmation of the position) and after 1 month, in addition to an IVU. Treatment was considered successful when the stone was no longer detected and IVU showed improvement of hydronephrosis. All patients were followed-up for 1 year and IVU was performed if indicated, in cases of relevant symptoms. Statistical analysis was performed with the use of the Chi-square test, and results were considered statistical significant at P<0.05.
Results
In group A, the ureteral access sheath insertion was successful in all cases, and all procedures were completed without any special type of dilatation, except for the use of the ureteral access sheath as a mechanic dilator. Endoscopic observation revealed intraureteral inflammatory polyps (histologically confirmed by endoscopic biopsies) in six (12.5%) patients and ureteral stricture adjacent to the stone in four (8.3%) patients, which was successfully managed with the access sheath dilator. These ureteral lesions did not require any further endoscopic treatment and did not impede the use of the ureteral access sheath. EHL was performed in 16 (33.3%) patients, while in the remaining 32 (66.6%) patients intact basket extraction (without EHL) was achieved. Bleeding did not disturb endoscopic stone manipulation through the sheath. The stone fragments were extracted rapidly, as the ureteral access sheath allowed rapid entry, exit and re-entry of the flexible ureteroscope and the basket. No false passages or ureteral perforations were recorded during the procedure. The mean operative time was 45.5 min (range 22–70).
In group B, the mean operative time was 58.5 min (range 31–94), which was statistically significantly (P<0.05) longer in comparison with group A. In group B, the passage of the flexible ureteroscope was more laborious in comparison with group A. Intraureteral inflammatory polyps was revealed in four (8%) patients and ureteral stricture in eight (16%) patients, which was managed with balloon dilatation in four (8%) patients, and with cold-knife in the other four (8%) patients. Balloon dilatation of the ureter was performed in 28 (56%) patients (P<0.05). EHL was performed in 12 (24%) patients (P>0.05), while in the remaining 38 (76%) patients intact basket extraction was achieved. Ureteral perforation was revealed in four (8%) patients (P<0.05), and was managed conservatively. In all these cases of perforation, EHL was performed and patient characteristics were similar to those of the remaining ones (e.g., ureteral anatomy, stone).
The follow-up imaging tests revealed stone-free status in 46 (95.8%) patients of group A, and in all 50 (100%) patients of group B. In group A, residual lithiasis was diagnosed at the level of the iliac vessels and was successfully managed with SWL. During the follow-up, IVU showed improvement of hydronephrosis in 38 out of 42 patients (90.4%) of group A with initial hydronephrosis, and in 44 out of 46 patients (95.6%) of group B. Furthermore, no long-term complications such as ureteral obstruction or stricture were revealed in either group after 1 year of follow-up. Collectively, the results are presented in Table 1.
Discussion
The lower third is the location of the great majority of ureteral stones and SWL is often used as first-line treatment [1, 2, 4]. Impacted lower ureteral stones are known to poorly respond to SWL, as they have no natural expansion space, and concomitant ureteral pathology (e.g., adjacent stricture and inflammatory polyps) may further restrain spontaneous passage of lithotripsy fragments [1, 3]. It has been demonstrated that ureteroscopic management of impacted lower ureteral calculi bears a far better cost-effect ratio in comparison with SWL [5, 6]. However, ureteroscopic treatment may be laborious, especially with rigid instruments, time consuming and bears a risk of ureteral trauma and perforation, estimated to be up to 15% and 6%, respectively [7, 8]. Initial ureteroscope insertion is a common problem, as well as ureteral kinking, while multiple ureteroscope withdrawals and reinsertions result in ureteral injury and shortening of the lifespan of ureteroscopic instruments [8].
Recently, the routine use of the novel kink-resistant, coaxial ureteral dilator/sheath, for access to the collecting system has been demonstrated to be safe, reliable and economical [9–12]. Compared with previous ureteral access systems this device has the advantage of the two-piece construction and of the availability of a range of sizes and lengths suitable for a variety of endourologic applications [9, 10]. The lubricious coating allows for easy, non-traumatic insertion and the body is more resistant to kinking, allowing multiple non-traumatic straightforward passages of ureteroscopic instruments, without causing ureteral ischemia [9]. Irrigant flow through the access sheath optimizes visibility, while maintaining low intrapelvic pressure, and helps to flush smaller stone particles out of the collecting system [10]. The ureteral access sheath reduces operative time by obviating balloon ureteral dilation, and by allowing rapid and repeat insertion and withdrawal of the ureteroscope, with minimal associated morbidity [11, 12]. Furthermore, simplified ureteral stent placement can be achieved through the lumen of the ureteral access sheath [13].
In the present study, it was demonstrated that ureteroscopic treatment of small impacted lower ureteral stones was facilitated with the use of the ureteral access sheath, which allowed continuous visualization of the impacted stone and easy basket manipulations alone or in combination with the EHL device. As a result, the mean operative time was statistically significantly decreased (45.5 vs. 58.5 min), representing a saving in operating room costs. Furthermore, in comparison with the standard unaided approach, the cost of the access sheath was also counterbalanced by the lack of usage of balloon dilatation.
It is noteworthy that ultrasound lithotripsy is now rarely performed in the ureter and electrohydraulic lithotriptors with 1.9F or smaller probes are preferred [14]. Recently, the use of ureteroscopic pneumatic lithotripsy and of holmium:YAG laser has shown very promising results in the treatment of impacted ureteral stones [10, 15]. However, the cost of EHL instrumentation is substantially less than laser lithotripsy, thus making it preferable at many institutions [14]. Although the use of EHL may cause ureteral perforation, this was prevented in our study with the offered protection of the ureteral access sheath, which keeps the scope within the sheath. In all our cases of ureteral perforation, EHL took place without the aid of the ureteral access sheath, while no other predisposing factor was revealed (e.g., ureteral pathology, iatrogenic fault). Moreover, ureteral strictures were successfully managed with the ureteral access sheath mechanic dilatation, and did not require additional endoscopic treatment as in the 8% of patients in group B. However, our initial experience concerned small impacted calculi and the potency of this procedure cannot be prejudged for larger stones, which are usually associated with more severe ureteral lesions [16]. Finally, the ureteral access sheath has been demonstrated to be useful for other endourologic procedures, such as removal of large renal stone burden during SWL, percutaneous nephrolithotripsy, incision of ureteropelvic junction and management of upper-tract transitional cell carcinoma [17–20].
In conclusion, our results reveal that the ureteroscopic treatment of small impacted lower third ureteral stones by flexible ureteroscopy with the use of the ureteral access sheath can be highly successful, in only one session. Currently, we are performing a relevant study regarding ureteral stones in the upper- and mid-ureter and the preliminary results are encouraging. We feel that urologists who routinely perform ureteroscopic procedures can easily master this technique in favor of patients’ outcome.
Conclusions
Endoscopic management of small impacted lower third ureteral stones with the aid of the ureteral access sheath, in comparison with the more standard unaided approach, is a more feasible, quick and safe procedure, which bears comparable efficacy. The use of the ureteral access sheath allows easy and intact extraction of small stones and lithotripsy fragments of larger calculi. We feel that the ureteral access sheath is a useful addition to the endoscopic armamentarium which could be further evaluated for the management of larger impacted stones located in any portion of the ureter.
References
Morgentaler A, Bridge SS, Dretler SP (1990) Management of the impacted ureteral calculus. J Urol 143:263
Ather MH, Paryani J, Memon A et al (2001) A 10-year experience of managing ureteric calculi: changing trends towards endourological intervention—is there a role for open surgery? BJU Int 88:173
Mugiya S, Nagata M, Un-No T et al (2000) Endoscopic management of impacted ureteral stones using a small caliber ureteroscope and a laser lithotriptor. J Urol 164:329
Pearle MS, Nadler R, Bercowsky E et al (2001) Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol 166:1255
Chang CP, Huang SH, Tai HL et al (2001) Optimal treatment for distal ureteral calculi: extracorporeal shockwave lithotripsy versus ureteroscopy. J Endourol 15:563
Lotan Y, Gettman MT, Roehrborn CG et al (2002) Management of ureteral calculi: a cost comparison and decision making analysis. J Urol 167:1621
Pardalidis NP, Smith AD (1995) Mechanical techniques and meatotomy for ureteral dilation. In: Smith AD (ed) Controversies in endourology. Saunders, Philadelphia, p 320
Harmon WJ, Sershon PD, Blute ML et al (1997) Ureteroscopy: current practice and long-term complications. J Urol 157:28
Monga M, Bhayani S, Landman J et al (2001) Ureteral access for upper unirary tract disease: the access sheath. J Endourol 15:831
Kourambas J, Byrne RR, Preminger GM (2001) Does a ureteral access sheath facilitate ureteroscopy? J Urol 165:789
Monga M, Bodie J, Ercole B (2004) Is there a role for small-diameter ureteral access sheaths? Impact on irrigant flow and intrapelvic pressures. Urology 64:439
Monga M, Gawlik A, Durfee W (2004) Systemic evaluation of ureteral access sheaths. Urology 63:834
Wu NZ, Auge BK, Preminger GM (2001) Simplified ureteral stent placement with the assistance of a ureteral access sheath. J Urol 166:206
Elashry OM, DiMeglio RB, Nakada SY et al (1996) Intracorporeal electrohydraulic lithotripsy of ureteral and renal calculi using small caliber (1.9F) electrohydraulic lithotripsy probes. J Urol 156:1581
Yagisawa T, Kobayashi C, Ishikawa N et al (2001) Benefits of ureteroscopic pneumatic lithotripsy for the treatment of impacted ureteral stones. J Endourol 15:697
De Sio M, Autorino R, Damiano R et al (2004) Expanding applications of the access sheath to ureterolithotripsy of distal ureteral stones. A frustrating experience. Urol Int 72(Suppl 1):55
Vanlangendonck R, Landman J (2004) Ureteral access strategies: pro-access sheaths. Urol Clin North Am 31:71
Okeke Z, Lam JS, Gupta M (2004) Use of a ureteral access sheath to facilitate removal of large stone burden during extracorporeal shock wave lithotripsy. Urology 63:574
Auge BK, Wu NZ, Pietrow PK et al (2003) Ureteral access sheath facilitates inspection of incision of ureteroplevic junction. J Urol 169:1070
Auge BK, Pietrow PK, Lallas CD et al (2004) Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol 18:33
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pardalidis, N.P., Papatsoris, A.G., Kapotis, C.G. et al. Treatment of impacted lower third ureteral stones with the use of the ureteral access sheath. Urol Res 34, 211–214 (2006). https://doi.org/10.1007/s00240-006-0044-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-006-0044-6