Abstract
The aim of this study was to detect, isolate and characterize the nanobacteria from human renal stones from a north Indian population, and to determine their role in biomineralization. Renal stones retrieved from the kidneys of 65 patients were processed and subjected to mammalian cell culture conditions. The isolated bacteria were examined using scanning (SEM) and transmission electron microscopy (TEM). They were characterized for the presence of DNA, proteins and antigenicity. The role of these bacteria in biomineralization was studied by using the 14C-oxalate based calcium oxalate monohydrate (COM) crystallization assay. We observed the presence of apatite forming, ultrafilterable gram negative, coccoid microorganisms in 62% of the renal stones. SEM studies revealed 60–200 nm sized organisms with a distinct cell wall and a capsule. TEM images showed needle like apatite structures both within and surrounding them. They were heat sensitive, showed antibiotic resistance and accelerated COM crystallization. A potent signal corresponding to the presence of DNA was observed in demineralized nanobacterial cells by flow cytometry. The protein profile showed the presence of several peptide bands of which those of 18 kDa and 39kDa were prominent. Apatite forming nanosized bacteria are present in human renal stones and may play a role in the pathophysiology of renal stone formation by facilitating crystallization and biomineralization. However, further studies are required to establish the exact mechanism by which nanobacteria are involved in the causation of renal stones.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urolithiasis is one of the oldest ailments affecting mankind. Epidemiological studies have shown that only 10–20% of patients with renal stones have predisposing factors such as anatomical defects, metabolic or genetic disorders, or bowel disease [1]. All others who develop stones due to any unknown cause are referred to as idiopathic stone formers.
The progression of events leading to stone formation begins with urine supersaturation, crystal nucleation and aggregation, bringing about retention of crystals (nidi) and continued growth on the retained crystals [2]. The stimuli for calcium salt deposition are not completely known, but it has become clear that nidi are needed for precipitation, even under supersaturated conditions. Urine is a complex solution, and in it crystal nuclei usually form on existing surfaces. Epithelial cells, cell debris, urinary casts, other crystals and red blood cells can all act as heterogenous nuclei [3]. Biological processes can create nucleation sites [4, 5] and stones are then formed on the preformed nuclei.
It has been suggested that tiny bacteria called nanobacteria may cause kidney stones [5]. Nanobacterial antigen has been reported in 97% of human kidney stones [5, 6]. Apparently, these bacteria surround themselves with a mineral coating and can serve as nidi for the genesis of renal calculi [5, 6, 24]. However, a significant controversy has erupted over the existence and significance of nanobacteria [7, 8, 9]. It has been suggested that the biomineralization attributed to nanobacteria may be initiated by non-living macromolecules such as phospholipids and by self-propagating microcrystalline apatite [10]. The present study was conducted to investigate the presence of nanaobacteria in renal stones and to study their role in stone formation.
Materials and methods
Patients who had undergone operative procedures such as pyelolithotomy, extended pyelolithotomy and/or nephrolithotomy for the removal of renal stones were included in the study. Surgically removed calculi from 65 patients with renal stones were collected. The stones were analysed for their chemical composition by standard chemical analytical methods. The stone samples were processed for the culture of nanobacteria according to the method of Ciftcioglu et al. [6]. The stones were pulverized, demineralised in 1 N HCl and neutralized with 0.5 M Tris, (pH 10.5, Sigma), and the solutions were centrifuged at 20,000 g for 30 min at 4°C in a Sorvall RC5B centrifuge. The pellet was suspended in serum free RPMI 1640 (HiMedia Laboratories, Mumbai, India), sterile filtered through 0.2 μm Millipore filters and the filtrate cultured in flasks containing RPMI 1640 with 10% fetal calf serum ( FCS, Biological Industries, Israel) and kept under tissue culture conditions (37°C, 5% CO2 and 95% air). As a control, RPMI was incubated with FCS but without stone filtrate. Subcultures were carried out in serum free RPMI after 4 weeks of initial inoculation and subsequently after every 15 days. The cultures were harvested by centrifugation at 20,000 g for 45 min at 4°C, washed with phosphate buffered saline (PBS, pH 7.2) and used for characterization.
Gram staining was done with a commercially available kit (Hi Media Laboratories, Mumbai, India). Urease enzyme activity was assessed using the standard method [11]. Nanobacterial cultures were assayed for antibiotic sensitivity by subculturing them in serum free RPMI in the presence of different concentrations (1, 2, 5 and 10×) of penicillin (100 IU=1×), streptomycin, gentamicin and kanamycin (100 μg/ml=1× for each) for 6 weeks. To assess heat sensitivity, stone filtrate and subcultures were incubated at 60°C for 15 min and thereafter were subcultured in RPMI 1640 with 10% FCS and serum free RPMI, respectively. The cultures were examined for nanobacterial growth, every week over a period of 6 weeks.
Scanning electron microscopy
A 30-day old bacterial culture was centrifuged at 20,000 g for 30 min at 4 C and washed with PBS. Pellets were subcultured in serum free RPMI-1640 on glass cover slips for 72 h. The glass cover slips were washed with PBS and fixed with 2% gluteraldehyde for 16 h. Fixed bacterial samples were dehydrated with absolute alcohol; dried in a critical point dryer and layered with gold followed by examination in a JEOL-JSM 6100 electron microscope.
Transmission electron microscopy
The bacterial pellet was fixed with 3% glutaraldehyde overnight, followed by treatment with Os04 for 1 h. The bacteria were dehydrated in ethyl alcohol, embedded in epoxy and ultra thin sections were cut and placed on 200 mesh copper grids. The sections were stained with uranyl acetate and lead citrate and subjected to transmission electron microscopy (TEM) (Zeiss-900).
Nanobacterial cultures in serum free media were analysed for the presence of DNA by a fluorescence activating cell sorter (FACS) (Becton Dickinson, USA Calibur, Model 163-A1202) using a modified method of Ormerod [12]. The nanobacterial pellet was dematerialized with 1 N HCl, washed in PBS and treated with 70% ethanol. The pellet was then treated with RNase (1 mg/ml, ICN Biomedicals, Ohio) and incubated with propidium iodide (500 μg/ml, ICN Biomedicals). Nanobacterial samples without demineralization were also processed by the same method. Culture media alone, i.e. serum free RPMI 1640 without nanobacteria, served as a control.
Calcium uptake assay
Subcultured nanobacteria were pelleted and the calcium content was measured in both the pellet and media using a commercial kit (Calcium ASX-Chema Diagnostics) at weekly intervals.
In vitro calcium oxalate monohydrate crystallization assay
Calcium oxalate monohydrate (COM) seed crystals were prepared by the method of Pak et al. [13], and crystal growth was measured by the method of Nakagawa et al. [14]. The reaction mixture contained seed slurry, CaCl2(2 mM), sodium oxalate (0.4 mM) and 14C-sodium oxalate (0.5 μCi) (BARC, Mumbai, India). The bacterial pellet was inoculated into it. The radioactivity counts in the infiltrate were measured with a scintillation counter (LKB 1214 Rack beta) at different time intervals for a period of 72 h. The reaction mixture, without bacterial suspension, served as a control. The result was expressed as percent decrease in radioactivity compared to the control.
Nanobacterial protein profile and immunological characterization
Demineralized pellet was lysed by sonication (Misonix XL-2000) with 10% wave intensity in the presence of 2 μm EDTA (Sisco, India) and 1 mM PMSF (Sigma). Lysate was centrifuged at 10,000 g for 10 min and the supernatant subjected to SDS-PAGE under reducing conditions following the method of Laemmlli [15] and stained by Commasie blue 250 (Sisco).
For raising polyclonal antibodies, demineralized nanobacteria were emulsified with Freund’s complete adjuvant (1:1, v/v) (Pharmacia, Sweden) and injected intramuscularly into New Zealand white rabbits. Two booster doses were given with Freund’s incomplete adjuvant (Pharmacia) at 14 day intervals. Serum was separated and stored at −20°C. The reactivity of the serum with isolated nanobacterial content was examined by the Ouchterlony immunodiffusion method [16]. Western blot of the nanobacterial lysate was done by the standard method of Towbin et al. [25]
Results and discussion
Forty out of 65 (62%) kidney stones showed a growth of nanobacteria. A pale white biofilm attached to the bottom of the culture flask was observed in 4 weeks old culture, whereas the control did not show any growth. These organisms were subculturable in serum free RPMI. Subculture showed a biofilm within 1 week. The bacteria were slow growing, with a doubling time of 3–5 days and could be filtered through a 0.2 μm filter. Standard microbiological techniques did not reveal the presence of any other micro-organism in the culture medium. Gram staining of the biofilm and microscopic examination at 100× showed tiny, clustered gram negative particles. These nanobacteria did not have any urease activity and the pH of the culture medium remained unchanged.
The bacteria were acid resistant and acid treated bacteria could be subcultured. Bacterial growth was found to be resistant to penicillin, streptomycin, and gentamicin at up to a 2×concentration and to kanamycin at up to a 10× concentration. Higher concentrations of penicillin, streptomycin and gentamicin were found to be inhibitory. Serum free bacterial cultures were observed to be sensitive to heat treatment as no bacterial growth was seen after heating at 60°C for 15 min.
SEM of the biofilm revealed coccoid particles with a diameter ranging between 60 and 200 nm. The organisms were pleomorphic, prokaryotic in shape and had a rough surface (Fig. 1a, b). TEM also showed coccoid thick cell walled structures. Cell wall and capsule were distinct. Both within and surrounding the organisms were needle like apatite structures (Fig. 2).
An estimation of maximum fluorescence intensity (MFI) by FACS revealed the presence of DNA in the bacterial cells (samples containing nanobacteria treated with 1 N HCl showed 97% cells giving MFI between 103–104) (Fig. 3a). Conversely FACS analysis of non-demineralized samples showed 100% unlabelled cells and no fluorescence signal was observed in the control samples (Fig. 3b, c).
. 3 Photomicrographs showing propidium iodide uptake by nanobacteria. a 97.2% labeled nanobacterial cells after demineralization, b minimum fluorescence signal by nanobcaterial cells without demineralization, c 100% unlabelled cells in controls. The x axis (FL2-H)=propidium iodide uptake, the y axis=relative cell counts
An increase in the calcium content of the bacterial pellet was observed in nanobacterial cells for up to 45 days. On day 10 (5.7%) there was an increased calcium incorporation of 16.5% with 40% on days 28 and 45 (Fig. 4).
In the COM crystallization assay, there was a significant decrease in the residual radioactivity of the filtrate in the presence of the nanobacterial pellet compared to the control (Fig. 5)
SDS-PAGE of the bacterial lysate showed several polypeptide bands with molecular weights varying between 18 and 96 kDa, and prominent bands corresponding to molecular weights of 18 and 39 kDa (Fig. 6). An immune response to nanobacterial lysate antigen was observed, as evidenced by the formation of antibodies in rabbit models. This polyclonal antiserum showed a single precipitin identification band on double immunodiffusion with nanobacterial lysate (Fig. 7). Western blot of the nanobacterial lysate showed a single band at 39 kDa (Fig. 8).
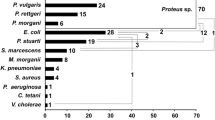
These bacteria have long been implicated in the causation of stone disease. Moynihan’s statement “that gall stones are the tombs erected in the memory of the bacteria” probably holds true for renal stones as well [17]. Bacterial infection of the urinary tract may induce urinary stone formation by urease production, increasing crystal adherence to urothelium and/or by the production of an organic matrix [18]. The most common organism associated with struvite calculi is Proteus mirabilis. Ureaplasma urealyticum has also been reported to be associated with urinary stones [19]. Escherichia coli does not produce urease but is the most common organism identified in urinary culture, even in patients with urinary stone. Nanobacteria are extremely small bacteria which have been implicated as a novel human pathogen [5]. They are urease negative, however, they can produce carbonate apatite in their cell walls at physiological pH [5, 6]. When injected intravenously, these bacteria were found to accumulate in the kidney and produce apatite [20]. The formation of calculi in experimental rat models after the administration of nanobacteria, has also been reported [21]. Nanobacterial antigens have also been found in polycystic kidney [22].
The Finnish scientists who first discovered these bacteria have suggested that nanobacteria are the Helicobacter pylori of kidney stone disease and that urolithiasis is a nanobacterial disease [4, 5]. They isolated nanobacteria from 97% of kidney stones, although other investigators have not been able to duplicate the results [10]. We observed the growth of nanobacteria in 62% of kidney stones from a north Indian population. The nanobacteria could not be cultured under standard microbiological techniques and biofilm was detected within a week only when stones were subjected to tissue culture conditions. The nanobacteria isolated in our study had similar morphological characteristics to those described earlier [5, 6]. However, we found that they were heat sensitive whereas the nanobacteria isolated by Kajander et al. [22] were heat resistant. Controversy exists regarding the living or non-living nature of these bacteria. Cisar et al. [10] contested that these biofilms were bacterial and suggested that apparent replication could be due to crystallization from culture medium and that the so called nanobacteria are non-living, self-propagating mineral compounds. The critics of nanobacteria consider that there was not enough evidence to prove that these particles were living organisms. Breitschwett et al. [23] have reported the detection of nanobacterial antigen in North Carolina cattle which had a 16srRNA sequence identical to Bartonella weissii.
We have enough evidence to suggest that these microparticles are living microorganisms. In the present study, we examined nanobacteria for the presence of nucleic acids using a DNA specific dye, propidium iodide, at a concentration used to detect DNA in bacterial or mammalian cells. We observed that a high percentage of demineralized nanobacterial cells were labelled with fluorescent dye. These results confirm the presence of DNA in nanobacteria. The lack of fluorescence in controls (non-demineralised nanobacterial and medium only) show the specificity of this method. The presence of several distinct protein bands suggests that these bacteria have protein synthesizing machinery. The molecular examination of demineralised nanobacterial culture for proteins, revealed the presence of several polypeptide bands. Polyclonal antibodies raised against demineralised bacteria showed a single precipitin band with bacterial lysate; Western blot of this lysate showed a band at 39 kKDa. The presence of nanobacteria in kidney stones suggests that these bacteria may be involved in the etiology of such stones. It has been proposed that nanobacteria may act as seeds for mineral deposits and thus for kidney stone formation [5, 6, 9]. Our results show a significant incorporation of calcium by these bacteria. They were also found to accelerate in vitro crystal growth under supersaturated conditions of calcium by COM assay, as a significant increase in 14C-oxalate incorporation into seed crystals was seen in their presence.
The present study was initiated to confirm the presence of nanobacteria in kidney stones from a north Indian population, and to study their potential role in kidney stone formation. Our results indicate the presence of atypical mineral forming ultrafilterable nanobacteria like micro-organisms in the kidney stones. Our findings indicate that these are living organisms rather than non-living macromolecules capable of self-propagation. However, there is a need for further studies to characterize and to delineate sets of unambiguous criteria to validate the existence of these bacteria and their role in urinary stone disease.
References
Parks JH, Coe FL (1996) Pathogenesis and treatment of calcium stones. Semin Nephrol 16: 398
Menon M, Resnick MI (2002) Urinary lithiasis: etiology, diagnosis and medical management. In: Walsh PC, Retick AB, Vaughan ED, Wein AJ (eds) Campbell’s urology, 8th edn, vol 4. Saunders, Philadelphia p 3229
Brown CM, Purich DL (1992) Physical chemical process in kidney stone formation. In: Coe FL, Flames ML (eds) Disorders of bone and mineral metabolism. Ravan Press, New York p 613
Drach GW, Boyce WH (1972) Nephrocalculosis as a source for renal calculi: observation on humans and squirrel monkeys and on hyperparathyroidism in squirrel monkey. J Urol 107: 897
Kajander EO, Ciftcioglu N (1998) Nanobacteria: an alternative mechanism for pathogenic intra and extracellular calcification and stone formation. Proc Natl Acad Sci U S A 95: 8274
Ciftcioglu N, Bjorklund M, Kuorikoski K, Bergstrom K, Kajander EO (1999) Nanobacteria: nn infections cause for kidney stone formation. Kidney Int 56: 1893
Abbott A (1999) Battle lines drawn between Nanobacteria researchers. Nature 401: 105
Abbott A (2000) Researchers fail to find signs of life in living particles. Nature 408: 394
Drancourt M, Jacomo V, Hubert L, Lechevallier, Grisoni V, Coulange C, Ragni E, Claude A, Dussol B, Berland Y, Raoult D (2003) Attempted isolation of Nanobacterium sp. Microorganisms from upper urinary tract stones. J Clin Microbiol 41: 368
Cisar JO,Xu D-Q, Thompson J, Swaim W, Hu L, Kopecko DJ (2000) An alternative interpretation of nanobacteria—induced biomineralization. Proc Natl Acad Sci U S A 97: 11511
Collee JG, Meles RS,Watt B (1996) Tests for identification of bacteria. In: Collee JG, Fraser AG, Marurion BP, Simmons A (eds) Practical medical microbiology,14th edn. Churchill Livingstone, New York p 141
Ormerod MG (1990) Analysis of DNA. In: Ormerod MG (ed) Flowcytometry : a practical approach, 1st edn. Oxford University Press, Oxford p 69
Pak CYC, Ohata M, Holt K (1975) Effect of diphosphate on crystallization of calcium oxalate in vitro. Kidney Int 7: 154
Nakagawa Y, Ahmed MA, Hall SL (1987) Isolation from human calcium oxalate renal stones nephrocalcin, a glycoprotein inhibitor of calcium oxalate crystal growth. J Clin Invest 79: 1782
Laemmli UK (1970) Cleavage of the structural proteins during the assembly of the head of bacteriophage T4 Nature 227: 680
Ouchterlony O, Nilson LA (1986) Immunodiffusion and Immunoelectrophoresis. In: Weri DM (ed) Handbook of experimental immunology, 4th edn, vol 1. Blackwell Scientific, Oxford, pp 32.1–32.50
Hruska KA (2001) Nephrolithiasis. In: Schrier RW (ed) Diseases of the kidney, 7th edn, vol1, Lippincott William and Wilikins, Philadelphia p 789
Dewan B, Sharma M, Nayak N, Sharma SK (1997) Upper urinary tract stones and Ureaplasma urealyticum. Indian J Med Res 105: 15
Kajander EO, Kuronen I, Kari A, Alpo P, Ciftcioglu N (1997) Nanobacteria from blood, the smallest culturable autonomously replicating agent or earth. SPIE 3111: 420
Cuerpo EG, Kajander EO, Ciftcioglu N, Lovaco CF, Correa C, Gonzalez J, Mampaso F, Liano F, Garcia E, Escudero BA (2000) Nanobacteria: an experimental neo-lithogenesis model. Arch Esp Urol 53: 291
Hejelle JT, Miller HMA, Poxton IR, Kajander EO, Ciftcioglu N, Jones ML, Caughey RC, Brown R, Millikin PD, Darras FS (2000) Endotoxin and nanobacteria in polycystic kidney disease. Kidney Int 57: 2360
Kajander EO, Bjorklund M, Ciftioglu N (1998) Mineralization by nanobacteria. SPIE 3441: 86
Breitschwerdt EB, Sontakke S, Cannedy A, Hancock SI, Bradley JM (2001) Infection with Bartonella weisii and detection of nanobacterium antigens in north Carolina beef herd. J Clin Microbiol 39: 879
Bradbury J (1998) Nanobacteria may lie at heart of kidney stones. Lancet 352: 121
Towbin H, Stachelin T, Gordon J (1979) Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci U S A, 76: 4350
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00240-012-0505-z
Rights and permissions
About this article
Cite this article
Khullar, M., Sharma, S.K., Singh, S.K. et al. Morphological and immunological characteristics of nanobacteria from human renal stones of a north Indian population. Urol Res 32, 190–195 (2004). https://doi.org/10.1007/s00240-004-0400-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-004-0400-3