Abstract
Implant malplacement is the second most common reason for revision and bottoming down is the most common presentation of implant malplacement. Submuscular biplane relocation was combined with capsulotomies and multilayer capsulorrhaphy when bottoming down was seen following subglandular breast augmentation. Between 2005 and 2009, bottoming down following subglandular mammoplasty was seen in 41 breasts (19 bilateral and three unilateral). Of the 19 patients, 12 had downward transgression of inframammary crease (IMC) alone; this also included a patient with vertical scar mastopexy. Two patients had multiplane malplacements where bottoming down was associated with lateral displacement (telemastia) in one and medial displacement (symmastia) in the other. Two had simultaneous downward transgression of the IMC and nipple areolar complex (NAC) and three had bottoming down with capsular contracture independent of NAC descent. Follow-up of up to 3 1/2 years showed stable IMC and NAC relationship with acceptable results. Dog ear revision was required in one patient when IMC relocation was accompanied with vertical scar mastopexy and one patient needed revision for further relocation and improvement of symmastia. No wound breakdown or periprosthetic infection was seen in their series. Multilayer capsulorrhaphy with submuscular biplane repositioning of implants is a suitable option to correct bottoming down following subglandular augmentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Capsular contracture and implant malplacement are the two most frequently seen complications of augmentation mammoplasty. In recent years, the incidence of revisions for capsular contracture has been reduced due to the subpectoral position of the implant [1], its improved quality, and better-sized implant pockets [2, 3]. Corrective surgery for implant malplacement is the second most common cause for revision surgery following augmentation mammoplasty [4]. Malplacements can be superior (high-riding breast), medial (symmastia), lateral (telemastia), and inferior (bottoming down). Bottoming down is the commonest presentation of malplaced implants. Bottoming down or implant ptosis is viewed as progressive lengthening of distance between nipple and breast fold. This deformity is almost always due to the result of implant malplacement or its descent. In the subglandular pocket, downward transgression of the implant often accompanies the inframammary crease (IMC). Presentation of bottoming down in the submuscular pocket may occur, independent of IMC descent, and the process is often due to an oversized pocket.
Bottoming down can be unilateral, bilateral, and asymmetrical and may present in combination with symmastia (medial malplacement) and telemastia (lateral malplacement). The downward implant malplacement or displacement may also be associated with augmentation mastopexies and capsular contractures. Factors leading to bottoming down are multiple and the process can be initiated by gravity [5, 6], stretching of the thin envelope [7], stretching of scar in vertical scar mastopexy with mammoplasty, early resumption of heavy pectoral exercises [8], or due to local steroids [2]. The process can be influenced by the weight and size of the implant and the pocket used for its placement [5, 6]. Descent of the implant can be due to an inadvertent oversized pocket dissection through the transaxillary approach [4] or due to disruption of the IMC in transumbilical breast augmentation [7] or secondary to over-recruitment of skin in the lower pole of a hypoplastic breast. Malplacement can only be minimized by appropriate selection of the size of implant, accurate pocket markings, and careful dissection of the pocket regardless of the incision used [6].
The surgical anatomy of the region has been studied in the past [9–12] and helps to explain the different patterns of bottoming down seen in the same pocket dissected through different approaches. Bottoming down in the subglandular pocket is almost always associated with the downward transgression of the IMC. The downward displacement of the IMC and the implant is usually independent of the nipple areolar complex (NAC) and results in unusually high nipples. Treatment can be conservative or invasive and depends on the timing of diagnosis after mammoplasty [4]. Combined downward transgression of the IMC and NAC require combined IMC relocation and mastopexy to maintain normal relationship between these two important anatomical landmarks. In the current series, bottoming down following subglandular augmentations was selected and IMC relocation was performed using multilayer capsulorrhaphy along with repositioning of the implant in the muscle-splitting biplane technique.
Surgical anatomy and surface markings
The IMC, or fold, is a defining structure of a developed breast and its robust anatomical presence has led to the basis of the classification of ptosis [13]. The breast in a female is highly variable, but the size of the base of the breast is fairly constant and extends from the second to sixth rib in the midclavicular line. From this circular base, the breast protrudes and this depends to a degree that varies in almost every individual female [10]. The IMC, on the other hand, extends from fifth and sixth rib, curves medially down, and extends to the seventh or eighth rib laterally to the anterior axillary line. The midpoint usually lies just behind the areola at a level of the sixth rib in midclavicular line. Muntan et al. [9], in their histological study, defined it as a microscopic structure due to condensation of the superficial Camper's fascia and the deeper Scarpa's fascia. Collagen bundles from these two layers were attached to the dermis at or just below the fold level. Scarpa's fascia or the deeper layer was continuous with the deep investing fascia. This deep investing fascial layer or extended pectoral fascia is continuous with the anterior leaf of the rectus sheath medially and the deep fascia over serratus anterior laterally.
Methods
Patient selection, plan, and marking
Surgical planning includes a good medical history and physical examination. The patient presenting with bottoming down in the partial submuscular plane and exhibiting marked dynamic or animation deformity are offered conversion into a muscle-splitting biplane. Similarly, patients presenting with bottoming down following subglandular augmentation and with an adequate skin envelope or positive pinch test are informed about the ever-changing nature of the skin envelope and a change of plane into muscle-splitting biplane is routinely discussed. Otherwise, all patients with bottoming down following subglandular augmentation and showing wrinkling of the implant in the upper pole, loss of upper pole tone, texture and shape due to maternity, weight, body fat changes, or changes related to aging are offered a change of plan.
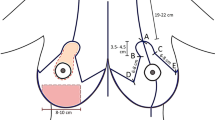
Markings
All patients are marked preoperatively in the standing position; normal surface markings of the IMC are used to reconstitute and reposition the displaced surface anatomy of the IMC. An ideal IMC should lie at the level of the sixth rib in the midclavicular line. The inframammary scar, when present, shows cephalic migration due to the relative downward transgression of the implant and may serve as the lower boundary of the proposed IMC relocation, provided the nipple to scar length is adequate for an acceptable esthetic result. In the absence of the scar or to accommodate changes in the proposed size of the implant, new pocket dimensions are marked appropriately [6]. With the patient standing and using a marker, a new IMC is marked after establishing its level and position. The next and important step is to examine the lateral and medial extent of the breast pocket with the patient lying in the supine position. The implant is manually pushed medially and laterally and the maneuver demonstrates the absence or presence of symmastia or telemastia. These two dimensions can be easily missed in the standing position and can limit the scope and the outcome of surgery [2].
The medial and lateral extension of the IMC is marked to tailor the final extent of the capsulorrhaphy and the size of an appropriate implant dimension is chosen. Once the extent of the capsulorrhaphy is established, simulation of new IMC is performed by manually pushing the implant superiorly up to the level of the new IMC and the relative position of the nipple and the new IMC is checked. If the position of the NAC is lower than the new IMC, the procedure should include simultaneous mastopexy. The selection of mastopexy depends on the degree of simulated ptosis and the experience and choice of the surgeon. If the plan includes a simultaneous vertical scar mastopexy with IMC relocation, then the lower limit of the vertical scar must be at least 2.0 cm above the marked new IMC.
Surgical planning is discussed with the patient, and the complexity and nature of the procedure is explained.
Between 2005 and 2009, bottoming down following subglandular mammoplasty was seen in 41 breasts (19 bilateral and three unilateral) and treated with IMC relocation along with repositioning of the implant in the muscle-splitting biplane. Three patients presented with unilateral bottoming down (Fig. 1a–d) and 19 presented with bilateral bottoming down. Of the 19 patients, 12 had downward transgression of the IMC alone (Fig. 2a–d) and included a patient with vertical scar mastopexy (Fig. 3a–d). Two had multiplane displacements where bottoming down was associated with lateral malplacement (telemastia) in one (Fig. 4a, b) and medial displacement (symmastia) in the other. Two had simultaneous IMC and NAC downward transgression (Fig. 5a–d) and three had bottoming down with capsular contracture independent of NAC descent (Fig. 6a–d).
a and b Anterior and oblique views of bottoming down in a patient 8 months after simultaneous vertical scar mammoplasty with 230 cc implants. c and d Six months postoperative anterior and oblique views after correction of bottoming down through the lower end of the vertical scar with same size implants positioning in submuscular biplane pocket
a and b Preoperative anterior and oblique views of a patient who presented with capsular contracture along with descent of IMC and NAC 9 years after her surgery with 440 cc implants in subglandular plane. c and d Nine months postoperative anterior and oblique views showing combined vertical scar mastopexy with IMC relocation after capsulectomy and using 300 cc implants in muscle-splitting biplane. Patient needed a dog ear excision of the lower end of the vertical scar
a and b Anterior and oblique views of bilateral grade IV capsular contracture with bottoming down in a patient 9 years after initial augmentation mammoplasty with 260 cc implants in subglandular plane. c and d Six months postoperative anterior and oblique views after capsulectomy and IMC relocation with 300 cc implants in muscle-splitting biplane
Technique
All procedures are performed under general anesthetic, predominantly as a day case. After explantation, prosthesis integrity is checked and the preoperatively marked boundaries of the new IMC and pocket are tattooed percutaneously using methylene blue. The level of the lower or inferior capsulotomy should ideally be at a level close to the sixth rib in the midclavicular line. Lateral, medial, and inferior capsulotomies are performed along the tattooed part in both anterior and posterior parts of the capsule. The medial capsulotomy is limited up to the junction of the middle and lower third of the sternum. Multilayer closure, using 3-0 Vicryl, is performed and includes freshened capsule with a bite of underlying subcutaneous tissue on the anterior area and muscle or periosteum on the posterior aspect (Fig. 7a). Capsulotomies are also performed in other quadrants or dimensions to release pocket constriction, when present. Selective or total capsulectomies are performed in the presence of grade IV contractures. Lateral multilayer capsulorrhaphy is performed in lateral malplacements (telemastia) in addition to routine lower pole multilayer capsulorrhaphy with repositioning in the muscle-splitting biplane [14]. Mirror image medial capsulotomies may be required if there is concomitant medial quadrant pocket constriction (Fig. 4a, b) Medial malplacements (symmastia) require mirror image lateral capsulotomies. In these cases, placing an implant in the muscle-splitting biplane, the medial pectoralis attachment to the upper and middle sternum acts as a new medial boundary and obviates the need for the capsulorrhaphy at this level.
a Illustration showing medial to lateral extent of the capsulorrhaphy. bArrow showing extent, level, and direction of the pectoralis split. c Side view showing stitching of the lower border of upper split pectoralis to the corresponding level of the posterior aspect of the breast gland. d Insertion of the implant in muscle-splitting biplane with repositioning of IMC using multilayer capsulorrhaphy. The pectoralis lies in front and behind the implant at the same time in the muscle-splitting biplane
Once IMC relocation and repair is completed, the submuscular pocket is reached medially at the level of the junction of the middle and lower thirds of the sternum. Submuscular access at this level is achieved after splitting or separating muscle to allow an index finger for submuscular dissection along marked dimensions. Once the submuscular dissection is completed, a muscle is split or separated along its fibers' direction, up and laterally, to the anterior axillary fold [14] (Fig. 7b). The anterior layer of the capsule is marked corresponding to the lower border of the upper split muscle and after capsulotomy, it is stitched to the lower free border of upper split muscle using continuous 3-0 locking Vicryl (Fig. 7c). This closure is essential to prevent future relocation of prosthesis in its previous upper subglandular pocket. In cases where relocation of IMC is expected to be more than 4 cm, quilting of the anterior and posterior layers of the capsule, inferior to the proposed neo-IMC, is performed. The quilting obliterates the dead space and helps to prevent air entrapment or fluid collection. The adequacy of the pocket is checked using a ballooning maneuver [15]. Irrigation and hemostasis are carried out before insertion of the new implant (Fig. 7d). Skin closure is performed in three layers using 3-0 and 4-0 Vicryl suture and drains are used when necessary.
Postoperative care
The procedure is usually done as a day case with single intravenous antibiotics. Support undergarments are worn for 4 to 6 weeks and patients are encouraged to go back to routine activities after 4 weeks. Exercises, aerobics, or activities involving upper body and shoulder girdle can be resumed after 4 to 6 weeks with caution.
Results
Follow-up of up to 3 1/2 years showed a stable IMC and NAC relationship with acceptable results. One patient with a combination of bottoming down and symmastia needed revision for further relocation of the IMC. Another patient requiring IMC relocation along with vertical scar mastopexy needed excision of a dog ear over the lower end of the vertical scar. Severe scar puckering was seen in one patient who presented with an asymmetrical IMC along with a very thin skin envelope. Multilayer capsulorrhaphy left her with noticeable puckering of the IMC for almost 8 months before it settled to an acceptable degree (Fig. 8a–f).
a and b Anterior and oblique views of a patient with a 10-year history of 250 cc breast implants placed through an axillary approach in the subglandular plane. Patient presented with asymmetrical IMC with very thin breast envelope and requested for bigger implants with restoration of IMC symmetry. c and d Three months postoperative anterior and oblique views after capsulotomy and left IMC relocation with 300 cc implant in muscle-splitting biplane. Left IMC puckering was noticeable after multilayer capsulorrhaphy in a thin breast envelope. e and f Nine months postoperative anterior and oblique views showing improvement in the puckering and appearance of the crease on left side
Discussion
Continued improvement in implant quality and texture, bigger pocket dissection, and subpectoral placement of implants has reduced the incidence of capsular contracture. However, it is still considered the commonest cause of corrective surgery after augmentation mammoplasty and may constitute up to 8% of cases [16]. On the other hand, the relative incidence of implant malplacement is on the rise due to fewer capsular contractures and absolute rise in breast augmentation performed today. In one series, up to 12% patients were seen to have malplacements when the transaxillary subpectoral approach was used for the augmentation mammoplasty [4].
Bottoming down or implant ptosis is seen as an increase in the distance between the nipple and the lowest border or fold of the breast. The treatment has evolved over a period of time and is centered at procedures involving minimal scarring as opposed to early extensive resection of inframammary folds using external inframammary incisions [8, 17]. The current treatment modalities include external supportive bandages, with or without minimally invasive keyhole incisions [4] or internal repairs using inframammary or periareolar incisions [7, 18]. These internal repairs and treatments include multilayer capsulorrhaphy [2], internal autologous capsular flaps [7, 18], and allogeneic dermal grafts [19].
The breast envelope is dynamically active and the envelope thickness varies in each individual and varies in an individual from time to time. The breast envelope is commonly affected with aging, parity, breastfeeding, and total body or fat changes [5, 14, 20]. The plane of implantation plays an important role in the dynamics of the breast envelope, these secondary envelope changes are more prevalent when an implant is placed in the subglandular plane and can also be influenced by the size and weight of an implant [20]. An intact muscle parenchymal interface in a submuscular pocket provides stability to the breast envelope and this is possibly due to an active support provided by the muscle to an elastic inactive skin [20]. When a submuscular biplane pocket is added, a multilayer capsulorrhaphy provides primary and immediate support to the IMC and the implant and submuscular positioning plays a supportive and secondary role. The submuscular biplane relocation has the added advantage of improving soft tissue cover in the upper esthetic unit of the breast and restores normal configuration of skin and muscle interface. Intervening muscle between skin and implant provides a smoother transition and prevents rippling and a step-off deformity, especially when a soft cohesive gel prosthesis is used [14] (Fig. 9a–d). Submuscular positioning of the implant also helps to improve breast cancer screening [5].
a and b Preoperative anterior and oblique views of a patient presenting with asymmetrical bottoming down who had a severe pectus excavatum deformity. Patient had 260 cc cohesive gel silicone implants in subglandular plane 6 years ago. c and d Six months postoperative anterior and oblique views after relocation of 350 cc cohesive gel microtextured implants in muscle-splitting biplane with multilayer capsulorrhaphy
Malplacement or bottoming down can present asymmetrically and may be associated with lateral malplacement (telemastia) or medial malplacement (symmastia). Similarly, displacements associated with capsular contractures can be multidirectional and a thorough examination and assessment is mandatory to address and include these associated malplacements in the surgical plan of bottoming down correction. Bottoming down is usually associated with lowering of the IMC independent of the NAC and relocation of IMC alone is sufficient for adequate results. However, when the IMC lowering is associated with lowering of the NAC, it is important to perform a mastopexy at the same time in order to maintain the normal IMC and NAC inter-relationship in a repositioned IMC (Fig. 5a–d). Relocation of the IMC alone in these patients will induce a ptotic appearance to the breast and mastopexy without relocation of the IMC will worsen bottoming down.
Correction of bottoming down following subglandular breast augmentation using the inframammary crescentic de-epithelialized dermal advancement flap and repositioning of the implant in the partial submuscular implant has been described as a case report [21] and pocket replacement from subglandular to partial submuscular plane was selectively performed when displacement was associated with wrinkling [22]. Dual-plane repositioning is an option [23]; however, the muscle release in the partial submuscular or dual plane quite often results in muscle contraction-associated deformities and dynamic breasts [24–26]. Even though an 88% subjective satisfaction rate after dual-plane augmentation mammoplasty is reported, these muscle contraction-associated deformities may be present in up to 77.5% of patients to a varying degree [26]. In the muscle-splitting biplane procedure, the pectoralis remains attached all along the sternocostal margin, preventing muscle contraction deformities [14, 25]. These animation or muscle contraction deformities may possibly be seen in the muscle-splitting biplane technique but the incidence was seldom seen in over 1,000 mammoplasties in the muscle-splitting biplane by the author and was limited to some of the very muscular athletic patients. In these patients, the strong upper medial pectoralis can displace the implant without breast envelope distortion [14]. Bottoming down or malplacement following partial submuscular augmentation are treated using multilayer capsulorrhaphy without change of plane. However, in selected cases of bottoming down following partial submuscular augmentation, marked dynamic or animation deformity may require a change of plane into the muscle-splitting biplane as described by the author [25]. Similarly, a patient presenting with bottoming down following subglandular augmentation and with an adequate upper pole envelope cover does not require a change of pocket. In these cases, the reliability of the pinch test needs to be considered in the long term, especially in young patients [20]. In patients presenting with bottoming down with symmastia following subglandular augmentation, muscle-splitting biplane repositioning avoids the need for capsulorrhaphy in the medial quadrant. Medial pectoralis major attachment to the lateral sternal border provides a new medial boundary to the implant that helps to restore adequate intermammary cleavage [27].
Conclusion
Treatment of bottoming down with capsulotomies and multilayer capsulorrhaphy is combined with relocation of the prosthesis in the submuscular muscle-splitting biplane pocket. It restores normal skin muscle interface in its upper part, improves soft tissue cover and esthetic results, and is without the risk of dynamic breast deformities.
References
Biggs TM, Yarish RS (1990) Augmentation mammoplasty: a comparative analysis. Plast Reconstr Surg 85:368
Spears SL, Little JW III (1988) Breast capsulorraphy. Plast Reconstr Surg 81:274–279
Millan Mateo J, Vaquero P (2001) Innovative new concepts in augmentative breast surgery. Part II: systematic and drawing. Aesth Plast Surg 25:436–442
Troilius C (1996) Correction of implant ptosis after a transaxillary subpectoral breast augmentation. Plast Reconstr Surg 98:889–895
Tebbetts JB (2001) Dual-plane breast augmentation: optimizing implant–soft tissue relationship in a wide range of breast types. Plast Reconstr Surg 107:1255
Khan UD (2006) Lower pole enhancement in breast augmentation. Proceedings of the 6th Croatian Congress of Plastic, Reconstructive and Aesthetic Surgery, Opatja-Rijeka, Croatia
Rowe NM, Freund R (2005) The autologous internal breast splint: a novel technique for the treatment of postaugmentation ptosis. Aesthet Surg J 25:545–664
Clarendon CCD (1988) Implant descent: a complication of augmentation mammoplasty and its correction. Ann Plast Surg 21:452–457
Muntan CD, Sundine MJ, Rink RD, Acland RD (2000) Inframammary fold: a histologic reappraisal. Plast Reconstr Surg 105:549–556
Last RJ (1978) Anatomy regional and applied, 6th edn. Churchill Livingstone, Edinburgh, pp 65–66
Barnett A (1990) Transaxillary subpectoral augmentation in the ptotic breast: augmentation by disruption of the extended pectoral fascia and parenchymal sweep. Plast Reconstr Surg 86:76–83
Tebbetts JB (1984) Transaxillary subpectoral augmentation mammoplasty: long-term follow-up and refinements. Plast Reconstr Surg 74:636–647
Regnault P (1976) Breast ptosis: definition and treatment. Clin Plast Surg 91:657–662
Khan UD (2007) Muscle splitting biplane breast augmentation. Aesth Plast Surg 31:353–358
Keramidas E, Khan UD (2005) The ballooning manoeuvre in breast augmentation. Plast Reconstr Surg 115:1795–1796
Kjoller K, Holmich LR, Jacobsen PH, Friis S, Fryzek J, McLaughlin JK, Lipworth L, Henrikson TF, Jorgensen S, Bittmann S, Olsen JH (2002) Epidemiological investigation of local complications after cosmetic breast implant surgery in Denmark. Ann Plast Surg 48:229–237
Wechselberger G, Del Frari B, Pulzl P, Schoeller T (2003) Inframammary fold reconstruction with a deepithelializd skin flap. Ann Plast Surg 50:433–436
Parsa FD (1990) Breast capsulopexy for capsular ptosis after augmentation mammoplasty. Plast Reconstr Surg 85:809–812
Baxter RA (2003) Intracapsular allogenic dermal grafts for breast implant-related problems. Plast Reconstr Surg 112:1692–1696
Khan UD (2009) Selection of breast pocket using pinch test in augmentation mammoplasty: can it be relied in long term? Aesth Plast Surg 33:780–781
Sallbian MS, DiGregorio VR (2000) A simple technique to correct “bottoming-out” of the breast after augmentation mammoplasty. Aesthet Surg J 20:301–303
Chasen PE, Francis CS (2008) Capsuloraphy for revisionary breast surgery. Aesthet Surg J 28:63–69
Spear SL, Carter ME, Ganz JC (2006) The correction of capsular contracture by conversion to “dual-plane” positioning: technique and outcomes. Plast Reconstr Surg 118(Suppl 7):103S–113S
Baxter RA (2005) Subfascial breast augmentation: theme and variation. Aesthet Surg J 25:447–453
Khan UD (2009) Dynamic breasts: a common complication following partial submuscular augmentation and its correction using muscle splitting biplane technique. Aesth Plast Surg 33:353–360
Spear SL, Schwartz J, Dayan JH, Clemens MW (2009) Outcome assessment of breast distortion following submuscular breast augmentation. Aesth Plast Surg 33:44–48
Khan UD (2009) Correction of acquired synmastia with muscle-splitting biplane implant replacement. Aesth Plast Surg 33:605–610
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, U.D. Combining muscle-splitting biplane with multilayer capsulorrhaphy for the correction of bottoming down following subglandular augmentation. Eur J Plast Surg 33, 259–269 (2010). https://doi.org/10.1007/s00238-010-0414-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-010-0414-8