Abstract
Defects around the elbow region are often irregular with exposed nerves, tendons, bones/joint, and implants. Skin grafts, though possible in some cases, must be avoided, as it requires prolonged splintage and physiotherapy to prevent recurrence and elbow stiffness. Distant flaps require multiple stages, and free flaps are rarely indicated for elbow defects. Muscle flaps are bulky. To overcome these problems, distally based fasciocutaneous flaps from medial and lateral sides of the arm based on posterior ulnar recurrent artery and radial recurrent artery, respectively, were used. Ten patients were studied. Age of the patients ranged from 10 to 40 years. Five were male, and five were female. Radial and ulnar recurrent flaps were used in five patients each. The largest flap size was 18 × 8 cm, and the smallest was 10 × 6 cm. The flaps were islanded in four cases, and in six cases, they were used as pedicled flaps. Skin grafts were used in 90% of the patients because large flaps were required for resurfacing; also, our patients had thinner arms with less girth. All flaps survived well. One island flap had venous congestion and marginal necrosis, which eventually healed. A significant improvement of mobility and elbow movement was noted in all patients. These flaps can be raised even from the previously burnt skin, as the pedicle is located deep. These flaps have the following advantages: The flap is reliable (deeply located consistent vascular pedicle), can cover both the flexor and extensor surface of the elbow joint, avoids prolonged splintage, elbow stiffness, and recurrence, good aesthetic, and has functional results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Defects around the elbow resulting from various causes, such as trauma and release of contracture, are often irregular with exposed nerves, vessels, tendons, bones, and joint. Various methods have been described for reconstructing these defects, but any treatment that allows early mobilization and rehabilitation should be considered for defect closure to avoid risk of functional impairment of the most important joint of the upper extremity. The possibility of using the medial and lateral arm skin as flaps was investigated as distally based flaps. In this search, different recurrent flaps of the arm are a better option. They have the advantages of excellent color match, fine texture, ideal thickness, concealed donor areas, and one-stage reconstruction without any functional impairment of the donor area. In this study, we report our experience with radial and ulnar recurrent flaps of the arm for covering large size defects of elbow due to various causes with their advantages and disadvantages.
Patients and methods
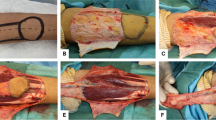
Ten cases were selected for flap coverage around elbow due to various causes between October 2006 and February 2009. All procedures were carried out by the same surgeon. Preoperatively, a bacterial wound culture was taken in open wounds and radiological evaluation done in all patients to rule out any joint or bone pathology. In all patients, preoperative evaluation of the recurrent vessels and perforators was done with handheld Doppler using an 8- and 12-MHz linear transducer. This offered additional preoperative confirmation of the vessel position, which would serve as the pivot point rotation flaps. The contractures dealt with in this series were of major type involving more than 50% of antecubital area. The defects were created after release of contractures or by freshening the margins in case of posttraumatic wounds with exposed bones, implants, or joint. The defect size was assessed, and the flap was planned accordingly (Figs. 1 and 2).
a Preoperative photograph of a 29-year-old man with post-thermal burn contracture at left elbow showing major contracture. b Intraoperative photograph of radial recurrent flap of arm transposed to the defect after release of contracture. c Two-week postoperative photograph showing good flap inset and full elbow extension
a Preoperative photograph of a 23-year-old man showing post-traumatic ulcer at left elbow with exposed elbow joint and implant over the posterior aspect. Ulnar artery perforators marked by handheld Doppler. b. Intraoperative photograph showing the defect and ulnar recurrent artery flap marking. c Raising the flap and completely islanding it based on the pedicle. d Postoperative photograph showing good soft tissue coverage at posterior elbow
Flap description
Radial and ulnar recurrent arteries arise from the radial and ulnar arteries in forearm, crossing the elbow, and entering into the arm along the lateral and medial intermuscular septum, respectively, to anastomose with their corresponding collateral arteries arising from the profunda brachii artery. These anastomoses send perforators along the intermuscular septum to supply the skin over the lateral and medial aspects of the arm, and flaps are planned distally based on these vessels to resurface the elbow defects [1, 2].
The donor site is closed primarily or grafted depending on the situation of the particular patient. In islands, the skin and subcutaneous tissue flap can be rotated 180°.
Results
The age of the patients varied from less than 10 to 40 years. The majority of cases were between 21 and 30 years (40%). Out of the ten cases, five cases each were reconstructed by radial and ulnar recurrent artery flaps. The male/female ratio was 1:1. Out of ten patients, seven patients had a post-burn contracture (five post-thermal burn and one each of electrical and chemical burn sequelae). One case of congenital contracture of long-standing duration presented for treatment at 19 years; this requires flap cover after release. Major contractures with acute flexion at the elbow involving more than 50% of the antecubital area was present in all eight cases of contractures, the release of which required flaps of bigger dimensions. Two patients had post-traumatic ulcers, one of which had exposed bone and one had an exposed joint with implant. Most of the cases (50%) presented with contractures after 1–2 years of the primary injury. Posttraumatic defects usually present 2–3 months after injury referred from orthopedics for flap cover of the wound. The maximum flap size was 18 × 8 cm, and minimum was 10 × 6 cm; pedicled flap was used in six cases and islanded in four cases. Donor site was split skin grafted in nine cases, and primary closure was obtained in one case. All flaps survived well. Minor complications such as venous congestion and flap edema were corrected by conservative treatment. One case developed partial flap necrosis, which healed by secondary intention. One case developed wound infection which was treated with dressing changes and antibiotics. Early mobilization was generally commenced on the seventh postoperative day depending on wound condition. A significant improvement of mobility and elbow movements was noticed in all the patients. There was no sensory loss in any of the patients. The follow-up examination after 6 months demonstrated a stable condition with good soft tissue coverage and skin elasticity. Most of the patients failed to present for follow-up beyond 6 months.
Discussion
Surgical release of contractures involving the flexor aspect of joints, such as the elbow, may result in a skin defect greater than expected, and such defects are not suitable for coverage with grafting alone. Baux et al. [3] stated that, after release of elbow contractures, the irregular bed is not suitable for skin grafting and flaps are preferred. Frequent bulky dressings and prolonged splintage are cumbersome and results in recontracture. In addition to the well-known Z-plasty, many creative local flaps, such as the seven-flap plasty [4], running Y–V-plasty [5], X-plasty [6], and square flap methods [7], have been proposed; each has its pros and cons. Sometimes, they fail to release the entire contracture and should be reserved for relatively narrow linear bands. Linear band contractures are also relatively uncommon.
Hallock [8] used local random fasciocutaneous flaps for the burned elbow. Van Landuyt et al. [9] and Lamberty and Cormark [10] used an island antecubital flap for soft tissue cover of the elbow. El-Khatib et al. [11] proposed an adipofascial flap for elbow coverage. All these flaps are criticized, as they are limited in reach and not suitable for large defects. Various muscle and musculocutaneous flaps such as brachialis [12], extensor carpi radialis longus [13], rectus abdominis [14, 24], external oblique [15], and latissimus dorsi [16] flaps were described for such defects by various authors. These flaps induce functional loss of the harvested muscle. Besides their donor site morbidity, multiple stages, keeping the arm immobilized in one position for a prolonged period, and texture and color mismatch, in addition to being considered thick, may even impede elbow flexion.
De Lorenzi et al. [17] described their experience with free flaps for reconstruction in burn patients. However, these flaps can only be used if microsurgical expertise is available.
One-stage local flaps are preferred to multi-stage regional or distant flaps because of less cost, shorter hospitalization, and avoidance of immobilization of the involved elbow.
The vascular territories of the arm have been studied by various authors [1, 2], and in many years, plastic surgeons are attracted to the upper arm as a potential donor site for flaps because of color, texture, and thickness and the fact that it can be well-concealed.
The radial and ulnar recurrent artery flaps are best suited for covering elbow defects and serving the purpose. They were first described by Maruyama and Takeuchi [18] and Hayashi et al. [19] while searching for a suitable alternative to the available local options for covering elbow defects. The versatile nature of these flaps is due to the constant anatomy of the recurrent arteries together with their anastomosis to the corresponding collateral arteries around the elbow joint. Easy dissection of the pedicle without any functional disability and without the help of Doppler is the prominent feature of these flaps.
The most common age group in our study was 21–30 years (40%), and male/female sex ratio was1:1, which is consistent with the study group of Aslan et al. [20] in which the most common age group was 20–30 years and male/female sex incidence was 1:1.13. The young age group shows the working group who are susceptible to trauma and injury due to burns resulting in contracture formation.
Deep burns such as electrical burns, lightening injuries, contact burns, and deep thermal burns cause extensive tissue loss. The problem usually involves exposed bone, tendon, joint, and nerve. Flap coverage of the elbow should be done expeditiously. Our study shows similar etiology for producing contracture or defects requiring flap cover (Table 1). Because of the location of defects or availability of donor areas over the arm region due to various causes, both radial and ulnar recurrent flaps were used in equal frequency (1:1). Prantl et al. [21] used more lateral flaps than medial ones in a study group of ten patients in the ratio of 4:1. Maruyama and Takeuchi [18] utilized the radial recurrent flap with success in three cases of elbow defects in his original paper. Hayashi et al. [19] successfully used the ulnar recurrent flap in nine defects in eight patients.
Pedicled fasciocutaneous flaps were used in six cases in our study to utilize the anastomotic arcade around the elbow joint. In addition to improving the arterial input to the flaps, it also improves venous drainage of the flaps. The flaps were islanded in four cases (where the pedicle was confirmed before surgery by a handheld Doppler), as the defect sizes were larger, and it enabled reaching the defect comfortably. The largest flap size was 18 × 8 cm, and the smallest was 10 × 6 cm in our study. The bigger flap sizes were due to the major contracture with acute flexion and extensive scarring around the elbow region, the release and excision of which resulted in big defects. This agrees with the study of Hayashi et al. [19], where the maximum flap size was 20 × 8 cm without any loss of overlying skin. They have also suggested in their study that the distally based flap can be extended almost as far as the axilla with lateral margins between the mid-anterior and posterior margins.
The donor site was split skin grafted in 90% of cases because our patients had thinner arms with less girth. Furthermore, all the patients required bigger flaps to resurface the large defect after release of major elbow contractures. The donor defect can be closed primarily if it is not wider than 6–7 cm [22, 23]. Although grafting the donor area is a major disadvantage, Indian patients usually cover the arm with clothes. However, for smaller defects, small flaps can be planned to obtain primary closure of the donor site.
The time between injury and flap cover was 1–2 years in 50% of cases and less than 1 year in 40% of cases. This was also the observation of Maruyama and Takeuchi [18] in their study.
Minor complications such as venous congestion and flap edema were observed in one case due to islanding of the flap, which later subsided after limb elevation and conservative measures. Prantl et al. [21] successfully used leeches early for such complications. One case developed partial flap necrosis on the distal part, as the anatomic landmark of the axis of the flap with the vessel was distorted during the preoperative marking because of post-burn scarring in the arm with the pull of the tissues to one side. One case developed wound infection, which was cured with daily dressing and antibiotics. Early mobilization was generally commenced on the seventh postoperative day depending on wound conditions. A significant improvement of mobility and elbow movement was noticed in all the patients. There was no sensory loss in any of the patients. The follow-up examination after 6 months demonstrated a stable condition with good soft tissue cover and skin elasticity in all patients. Most of the patients failed to present for follow-up beyond 6 months.
Conclusion
When compared with the other techniques, the favorable features of the recurrent flaps of the arm include the following:
-
1.
The vascular pedicle of the recurrent flaps of the arm is fairly consistent because of its deep location (flaps can even be raised from previously burnt skin).
-
2.
Dissection of the flap is straightforward and simple.
-
3.
The donor site is in a relatively inconspicuous area.
-
4.
It does not require sacrifice of a major artery or functional muscle.
-
5.
It allows for early mobilization of the involved elbow joint for rehabilitation.
-
6.
It does not require prolonged splinting as in skin grafting.
-
7.
It offers a single-stage reconstruction with an acceptable skin color and texture match.
-
8.
It avoids the chance of recurrence of contracture.
-
9.
It can cover both the flexor and extensor aspects of the elbow joint.
Therefore, we conclude that recurrent flaps of the arm are versatile and reliable for reconstructing all forms of elbow defects and, hence, are strongly recommended for all the defects in this region for permanent and stable soft tissue coverage.
References
Hayashi A, Maruyama Y (1990) Anatomical study of the recurrent flaps of the upper arm. Br J Plast Surg 43:300–306
Cormack GC, Lamberty BGH (1984) Fasciocutaneous vessels in the upper arm: application to the design of fasciocutaneous flaps. Plast Reconstr Surg 74:244–249
Baux S, Mimoun M, Kirsch JM, Zumer L, Berard V (1987) Treatment of elbow contractures in burns. Burns 13:241–244
Karacaoglan N, Uysal A (1996) Use of seven-flap plasty for the treatment of axillary and groin postburn contractures. Burns 22:69–72
Lai CS, Lin SD, Tsai CC, Tsai CW (1995) Running Y-V plasty for burn scar contracture. Burns 21:458–462
Vartak A, Keswani MH (1992) X-plasty for repair of burn contractures. Burns 18:326–328
Hyakusoku H, Fumiiri M (1997) The square flap method. Br J Plast Surg 40:40–46
Hallock GG (1991) Local random fasciocutaneous flaps for repair of the burned elbow. J Burn Care Rehabil 12:26
Van Landuyt K, DeCordier BC, Monstrey SJ et al (1998) The antecubital fasciocutaneous island flap for elbow coverage. Ann Plast Surg 41:252
Lamberty BGH, Cormack GC (1983) The antecubital fasciocutaneous flap. Br J Plast Surg 36:428
El-Khatib HA, Mehboub TA, Ali TA (2002) Use of an adipofascial flap based on the proximal perforators of the ulnar artery to correct contracture of elbow burn scars: An anatomic and clinical approach. Plast Reconstr Surg 109(1):130–136
Mathes SJ, Nahai F (1979) Clinical atlas of muscle and musculocutaneous flaps, 1st edn. Mosby, St. Louis
Ohtsuka H, Imagawa S (1985) Reconstruction of a posterior defect of the elbow joint using an extensor carpi radialis longus myocutaneous flap: case report. Br J Plast Surg 38:238
Burstein FD, Salomon JC, Stahl RS (1989) Elbow joint salvage with the transverse rectus island flap: a new application. Plast Reconstr Surg 84:492
Fisher J (1985) External oblique fasciocutaneous flap for elbow coverage. Plast Reconstr Surg 75:51
Mordick TG, Britton EN, Brantigan C (1996) Pedicled latissimus dorsi transfer for immediate soft tissue coverage and elbow flexion. Plast Reconstr Surg 99:1742–1744
De Lorenzi F, van der Hulst R, Boeckx W (2001) Free flaps in burn reconstruction. Burns 27:603–612
Maruyama Y, Takeuchi S (1986) The radial recurrent fasciocutaneous flap: reverse upper arm flap. Br J Plast Surg 39:458–6
Hayashi A, Maruyama Y, Saze M, Okada E (2004) Ulnar recurrent adipofascial flap for reconstruction of massive defects around the elbow and forearm. Br J Plast Surg 37:632–637
Aslan G, Tuncali D, Cigsar B et al (2006) The propeller flap for postburn elbow contractures. Burns 32:112–115
Prantl L, Schreml S, Schwarze H et al (2008) A safe and simple technique using the distal pedicled reverse upper arm flap to cover large elbow defects. J Plast Reconstr Aesthet Surg 61:546–551
Turegun M, Nisanci M, Duman H et al (2005) Versatility of the reverse lateral arm flap in the treatment of post-burn antecubital contractures. Burns 31:212–216
Lai CS, Lin SD, Chou CK, Tsai CC (1994) The reverse lateral arm flap, based on the interosseous recurrent artery, for cubital fosse burns. Br J Plast Surg 47:341–345
Sbitany U, Wray RC Jr (1986) Use of the rectus abdominis muscle flap to reconstruct an elbow defect. Plast Reconstr Surg 77:988
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tripathy, S., Khan, A.H. & Sharma, S. Clinical study of the recurrent flaps of the arm for resurfacing of elbow defects. Eur J Plast Surg 33, 23–28 (2010). https://doi.org/10.1007/s00238-009-0371-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-009-0371-2