Abstract
Purpose
Delayed cerebral ischemia (DCI) is a frequent cause of morbidity and mortality in patients with cerebral vasospasm (CV) following aneurysmal subarachnoid hemorrhage (aSAH). Refractory CV remains challenging to treat and often leads to permanent deficits and death despite aggressive therapy. We hereby report the feasibility and safety of stellate ganglion block (SGB) performed with a vascular roadmap-guided technique to minimize the risk of accidental vascular puncture and may be coupled to a diagnostic or therapeutic cerebral angiography.
Methods
In addition to a detailed description of the technique, we performed a retrospective analysis of a series of consecutive patients with refractory CV after aSAH that were treated with adjuvant roadmap-guided SGB. Clinical outcomes at discharge are reported.
Results
Nineteen SGB procedures were performed in 10 patients, after failure of traditional hemodynamic and endovascular treatments. Each patient received 1 to 3 SGB, usually interspaced by 24 h. In 4 patients, an indwelling microcatheter for continuous infusion was inserted. First SGB occurred on average 7.3 days after aSAH. SGB was coupled to intra-arterial nimodipine infusion or balloon angioplasty in 9 patients. SGB was technically successful in all patients. There were no technical or clinical complications.
Conclusion
Adjuvant SGB may be coupled to endovascular therapy to treat refractory cerebral vasopasm within the same session. To guide needle placement, using a roadmap of the supra-aortic arteries may decrease the risk of complications. More prospective data is needed to evaluate the therapeutic efficacy, durability, and safety of SGB compared with the established standard of care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Delayed cerebral ischemia (DCI) is a frequent cause of morbidity and mortality in patients with cerebral vasospasm (CV) following aneurysmal subarachnoid hemorrhage (aSAH) [1, 2]. Hemodynamic augmentation and intra-arterial infusion of calcium channel blockers represent the mainstay of CV treatment [3], but it was shown to be ineffective in 21% of the patients [4]. Balloon angioplasty is effective, although usually restricted to the proximal intracranial arteries; moreover, it carries a risk of vessel rupture [5]. Intra-arterial infusion of calcium channel blockers, on the other hand, is safer and better suited to treat peripheral spasms, although it tends to be short-acting and more often associated with CV recurrence. Additionally, its hypotensive side effect may complicate the hemodynamic management [2]. Intravenous milrinone is a more potent vasodilator than nimodipine, verapamil, and papaverine and has a positive inotrope effect but bears the risk of cardiotoxic side effects [6]. Clazosentan, finally, is an endothelin receptor agonist with a dose-dependent capacity to reduce angiographic vasospasms that initially appeared very promising but failed to reduce morbidity and mortality in prospective clinical trials mainly because of its pulmonary toxicity [7, 8].
As such, refractory CV, defined as recurrent vasospasm despite aggressive medical, hemodynamic and endovascular management [9], remains challenging to treat and still often leads to permanent neurologic deficits and death [10]. Search for other therapeutic options to treat refractory CV remains therefore important.
Stellate ganglion block (SGB) is currently performed to treat a variety of diseases, including complex regional pain syndrome, hyperhidrosis, post-herpetic neuralgia, refractory angina, and hot flushes [11]. It has previously been reported to improve brain perfusion as adjuvant therapy against CV [12] by reducing the sympathetic vascular tone of cerebral vessels, thereby inhibiting vasomotor constriction. As a reminder, the stellate ganglion, also known as the inferior cervical or cervico-thoracic ganglion, belongs to the sympathetic chain that sits along the vertebral column. It lies medially to the scalene muscles, laterally to the longus colli muscle, esophagus, and trachea (along with the recurrent laryngeal nerve) and anterior to the transverse processes of C7 and/or to the head of the first rib in front of the prevertebral fascia [13].
From the stellate ganglion, the post-ganglionic fibers travel through the cervical sympathetic chain to the head, along internal and external carotid arteries, and to the neck and to the upper extremities [14] (Fig. 1). In the setting of CV after aSAH, SGB has the potential to reduce blood flow velocity in the middle cerebral artery [15].
We hereby report the feasibility and safety of a vascular roadmap-guided SGB technique, with the goal of illustrating how to minimize the risk of dissection or thrombo-embolic complications when SGB is coupled with diagnostic or therapeutic cerebral angiography in the setting of refractory CV.
Methods
Patient selection
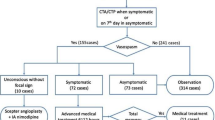
We retrospectively analyzed medical records of all consecutive patients with refractory CV after aSAH treated at our institution between January 2016 and April 2019 with adjuvant SGB. Refractory CV was defined as vasospasm poorly respondent to intra-arterial calcium-antagonist injection or with early recurrence (<24 h as measured clinically, and/or with Doppler-US and/or digital subtraction angiography). For each patient, the following data were collected and reviewed: WFNS grading and mFisher scale at admission, days elapsed from aSAH to treatment, associated endovascular treatments (intra-arterial vasodilators and/or balloon angioplasty), number of SGB treatments, use of indwelling microcatheter for continuous SGB injection, onset of clinically relevant DCI, and modified Rankin Scale (mRS) at discharge. Procedural and post-procedural complications were recorded. The local ethical committee (“Ethics Committee of Canton Ticino”) waived approval for this retrospective study. Informed consent was obtained from the patient or from the legal representative in all cases.
Technique
Following cerebral angiography on a biplane angio suite (Allura Xper FD20/20, Philips, The Netherlands), a fluoroscopic postero-anterior view of the C7 and T1 vertebral bodies is obtained, followed by a roadmap of the ipsilateral common carotid and vertebral artery. On the right side, a contrast-injection of the brachiocephalic trunk is sufficient to visualize both vessels. On the left side, a roadmap of the common carotid artery is obtained first, followed by contrast injection in the left subclavian artery during a fluoroscopic run which is saved and used as a “smart mask” roadmap, making the left common carotid artery appears bright and the left subclavian and vertebral arteries dark. This technique allows to visualize all the supra-aortic vessels in a single roadmap image when bilateral SGB is planned (Figs. 2 and 3). The vascular roadmap, showing the major supra-aortic vessels, is then coupled with the unsubtracted fluoroscopic projection to depict the osseous landmarks, lung apex, trachea, and esophagus (revealed by nasogastric tubing, when present). Using continuous or intermittent fluoroscopic control a 22 G × 9 cm spinal needle is inserted in a “bull’s eye” view through an antero-posterior approach targeting the head of the first rib or the transverse process of C7 until bony contact is made (Figs. 2 and 3). In case of large vessel superimposition on the targeted landmark, the c-arm is slightly rotated, and a new multivessel roadmap is obtained until the needle can safely be advanced to the target site while avoiding puncturing a major vessel (Fig. 3).
After bilateral supra-aortic arteries vascular roadmap in AP view a the needle is inserted with “bull’s eye” technique to the target, here on the left side, avoiding the major arteries. The unmasked image b is used for visualization of the bony landmark of T1, namely, the vertebral body of T1 (dashed lines) and the head of the first rib (arrow), with control of tracheal and pleural lines (white solid lines). Contrast injection c rules out vascular run-off and confirms correct needle tip location in the pre-vertebral fat plane and is followed by local anesthetic injection
Two cases of stellate ganglion block, one on the right (a–c) and one on the left side (d–f). In both cases, on a straight AP view, there was superimposition of large arteries on the T1 rib head, so that a slightly oblique AP view (spinous processes are not seen exactly midline) was used to resolve superimposition of arteries on the target and find a good window to reach the target with the needle
Once bony contact is established, the needle is gently retracted (5–10 mm) to position its tip superficially to the fascia of the longus colli muscle, where the stellate ganglion is situated. A 0.5–1-ml bolus of contrast agent (Iopamiro 300 mg/ml, Bracco, Italy) is injected to verify the homogenous spread in the pre-vertebral fat plane (Figs. 2 and 3) and to rule out undesired vascular runoff. Once the correct needle position is confirmed, 5 ml of 0.5% ropivacaine is injected to obtain the anesthetic block of the stellate ganglion [16] and to reduce the sympathetic tone of the cerebral arteries. SGB can be performed on both sides in case of bilateral CV.
When repetitive SGB seemed likely in the setting of “malignant” vasospasms, a small infusion catheter (20-G catheter from an epidural injection kit, B. Braun, Germany) was inserted through a 18-G Tuohy needle and left in place for continuous or repeated injections. The dosage of continuous injections was 0.2% ropivacaine at 5 ml/h (Fig. 4).
CT-angiography MIP reconstruction on axial (a) and sagittal (b) planes demonstrating the course of the percutaneous microcatheter at the level of the prevertebral fat plane at T1 (arrows) for continuous or repeated anesthetic injections. The axial image (a) shows the complex and delicate loco-regional anatomy, with the catheter passing between trachea and esophagus medially and the common carotid and vertebral arteries just laterally
Since miosis and ptosis are not reliable signs of efficacious SGB in intubated patients, a subjective operator’s assessment evaluated anhidrosis and temperature change on the skin of the ipsilateral side of face compared with the skin of contralateral side (for monolateral block) or to the skin of the chest (for bilateral blocks).
Results
Ten consecutive patients with refractory CV after aSAH were identified (7 females; mean age 50.2 years, range 37–66; coiling in 6, clipping in 4). All patients were treated with SGB after failure of traditional hemodynamic and endovascular treatments. Nineteen SGB were performed (bilaterally in 7) by three interventional neuroradiologists with 2 to 18 years of experience trained in both endovascular and spinal procedures. Patient characteristics are summarized in Table 1. Each patient received 1 to 3 SGB, usually interspaced by 24 h. In 4 patients, a catheter was implanted for continuous infusion of ropivacaine. The first SGB was performed on average 7.3 days (range 2–15) after aSAH. SGB was coupled to intra-arterial nimodipine infusion or balloon angioplasty in all but one case, in which a stand-alone SGB treatment was preferred due to hemodynamic instability. The same patient died 14 days after SAH due to a Tako-Tsubo syndrome and extensive DCI. A second patient died 11 days after SAH because of extensive DCI.
No procedural complications related to SGB were encountered. Clinical outcome for each patient measured by modified Rankin Scale (mRS) at discharge is reported in Table 1.
Discussion
Fluoroscopic and vascular roadmap guidance, combined to perform image-guided SGB, as described for the first time in the present work, allowed precise and simultaneous visualization of the osseous landmarks, lung apices, trachea, esophagus, and supra-aortic vessels, thereby mitigating the risk of injury to the loco-regional critical structures and of peri-procedural complications. All patients presented with refractory CV, which justified adjunctive SGB as a last-resort measure or so-called compassionate off-label use.
Sympathetic ganglia activity has long been considered a co-factor potentially affecting the onset and duration of CV. Indeed, a rich plexus of adrenergic fibers is well documented within the adventitial layer of the pial vasculature [17], and it has been demonstrated that SGB decreases cerebral vascular tone without affecting autoregulation [18]. Hu et al. [14] showed in a rat model of SAH that SGB increased the diameter and cross-sectional area of the basilar and middle cerebral arteries and could enhance neuroprotection. The clinical literature on SGB to treat CV is however scarce. In two series of patients with refractory vasospasm after aSAH, SGB reduced both the mean velocity in the middle cerebral arteries and the occurrence of radiological CV, with a trend toward lower rates of neurological deficits post-operatively [12, 15].
To date, SGB is generally performed by placing the needle under fluoroscopic guidance in the pre-vertebral space at the C7 or T1 level via an anterior para-tracheal approach without direct visualization of the supra-aortic vessels [13, 19, 20]. Due to the complex and delicate regional anatomy, several complications may occur, including pneumothorax, epidural injection, recurrent laryngeal nerve block with laryngeal paralysis and airway obstruction, seizures, blindness, stroke, and even locked-in syndrome [16, 21,22,23,24]. Alternatively, ultrasound-assisted needle placement is potentially cheaper and more readily accessible than fluoroscopy-assisted SGB although this requires advanced operator skills, may be difficult to perform in overweight patients or in case of neck deformities, and may result in inadvertent vascular injury, despite color-Doppler assistance [20].
In our cohort, there were no technical or clinical complications. Based on our series, multivessel roadmap guidance used during diagnostic or therapeutic cerebral angiography of refractory CV may not only serve to catheterize the supra-aortic arteries but also to optimize fluoroscopy-guided SGB and minimize the risk of complications.
Since SGB was performed in addition to triple H and endovascular therapy, including intra-arterial calcium channel blocker infusion and balloon angioplasty, its precise contribution in correcting CV remains speculative. Besides several confounding factors on the potential benefit of SGB, a major limitation of our report is the lack of a control group. Furthermore, SGB was used as a stand-alone therapy in only one hemodynamically unstable patient in cardiac failure status who could not tolerate any drop in blood pressure. In this patient, we observed evidence of vasospasm relief when comparing pre- and post-SGB DSA and CT-angiography (Fig. 5), arguing in favor of a proof of concept. Similar to the results shown after selective percutaneous blockage of the superior cervical ganglion [25], the angiographic vasodilation effect of SGB seemed more obvious on the distal circulation than on the more proximal arterial segments of the circle of Willis. This might illustrate the complementary role that SGB may play in treating refractory CV compared with alternative treatment strategies for the proximal segments, such as balloon angioplasty or stent-like-assisted techniques [26]. For more distal spasms, indwelling microcatheter placement with IA Nimodipine infusion has shown promising results [27]. Nonetheless, this increases the risk of thromboembolic complications since continuous catheter perfusion is not easy to implement in the intensive care unit, especially during non-working hours. Since SGB seems to have a similar effect on the distal vasculature, placement of an indwelling catheter at the site of the stellate ganglion may prove to be a safer alternative. More data is needed regarding the subgroup of CV patients that might benefit the most from SGB and how often or how long it should be performed before envisioning a paradigm shift. Nonetheless, the underlying mechanism of DCI and the role of CV and therapeutic vasodilatation to improve clinical outcome remain debate [28]. Indeed, clazosentan, the most potent spasmolytic drug known to date, failed to show any benefit in terms of death and DCI [7] even though the systemic side-effects may have largely contributed to the disappointing outcome. On the other hand, current evidence shows that CV still appears to be associated with DCI and hence a legitimate therapeutic target [29]. Recently, there has been a regain of interest in neuroprotective agents like nerinetide in stroke patients undergoing mechanical thrombectomy that seems to improve neurological outcome in patients not receiving r-tPA [30]. Consequently, a combined approach of new neuroprotective drugs, proximal mechanical dilatation, and adjuvant SGB could be worth exploring in severe CV. While it is unlikely that SGB may represent a stand-alone treatment for these patients, its value for milder CV or as a prophylactic treatment to avoid the occurrence of more severe CV remains an open question.
This patient with vasospasm was treated exclusively with left stellate ganglion block (SGB), due to poor hemodynamic tolerance to intra-arterial vasodilators. The left internal carotid artery arteriography before (a) and 20 min after (b) unilateral left SGB shows vasodilation effect in the M2–M4 segments (white arrows). A greater more delayed effect might be supposed. In the same patient, 1 day later, bilateral SGB was repeated, and CT-angiography MIP reconstruction before (c–e) and after (f–h) demonstrates a mild vasodilation effect both in anterior and posterior circulations
The technique we describe in this case series allowed to safely associate SGB with intra-arterial treatments in the angio suite, with the twofold objective of strengthening the effect of traditional endovascular treatments and avoiding vascular complications, that are feared when SGB is performed in a standard way, either under fluoroscopy or ultrasound. Future improvements of interventional angio suite will hopefully lead to better tools in the assessment of needle/catheter positioning, by means of detailed multiplanar tomographic images, and SGB efficacy, through advanced perfusional imaging.
The main limitations of this study are the relatively small number of patients in the series and the lack of a control group, but this is the first report of a novel technique that might serve as a proof of concept for larger prospective future investigations. The efficacy of SGB in reducing DCI remains unproven, due to the overlap with other concurrent treatments.
Conclusions
In patients with severe cerebral vasospasm, stellate ganglion block using multivessel roadmap of the supra-aortic arteries for needle guidance may potentially decrease the risk of complications compared with traditional fluoroscopy-guided SGB techniques. Adjuvant SGB coupled to mechanical or chemical intra-arterial therapy within a single session is feasible. A prospective controlled trial remains necessary to establish the role of SGB on a broader scale.
References
Findlay JM, Nisar J, Darsaut T (2015) Cerebral vasospasm: a review. Can J Neurol Sci 43:15–32
Francoeur CL, Mayer SA (2016) Management of delayed cerebral ischemia after subarachnoid hemorrhage. Crit Care:20
Diringer MN, Bleck TP, Hemphill JC et al (2011) Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care 15:211–240
Suwatcharangkoon S, De Marchis GM, Witsch J et al (2019) Medical treatment failure for symptomatic vasospasm after subarachnoid hemorrhage threatens long-term outcome. Stroke 50:1696–1702. https://doi.org/10.1161/STROKEAHA.118.022536
Linskey ME, Horton JA, Rao GR, Yonas H (1991) Fatal rupture of the intracranial carotid artery during transluminal angioplasty for vasospasm induced by subarachnoid hemorrhage. Case report J Neurosurg 74:985–990. https://doi.org/10.3171/jns.1991.74.6.0985
Wu EM, El Ahmadieh TY, Kafka B et al (2018) Milrinone-associated cardiomyopathy and arrhythmia in cerebral vasospasm. World Neurosurg 114:252–256. https://doi.org/10.1016/j.wneu.2018.03.151
MacDonald RL, Kassell NF, Mayer S et al (2008) Clazosentan to overcome neurological ischemia and infarction occurring after subarachnoid hemorrhage (CONSCIOUS-1): Randomized, double-blind, placebo-controlled phase 2 dose-finding trial. Stroke 39:3015–3021. https://doi.org/10.1161/STROKEAHA.108.519942
Macdonald RL, Higashida RT, Keller E et al (2011) Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol 10:618–625. https://doi.org/10.1016/S1474-4422(11)70108-9
Andereggen L, Beck J, Z’Graggen WJ et al (2017) Feasibility and safety of repeat instant endovascular interventions in patients with refractory cerebral vasospasms. American Journal of Neuroradiology, In, pp 561–567
Frontera JA, Fernandez A, Schmidt JM et al (2009) Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke 40:1963–1968. https://doi.org/10.1161/STROKEAHA.108.544700
Gunduz OH, Kenis-Coskun O (2017) Ganglion blocks as a treatment of pain: current perspectives. J Pain Res 10:2815–2826
Jain V, Rath GP, Dash HH et al (2011) Stellate ganglion block for treatment of cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage - a preliminary study. J Anaesthesiol Clin Pharmacol 27:516–521. https://doi.org/10.4103/0970-9185.86598
Elias M (2000) Cervical sympathetic and stellate ganglion blocks. Pain Physician 3:294–304
Hu N, Wu Y, Chen BZ et al (2014) Protective effect of stellate ganglion block on delayed cerebral vasospasm in an experimental rat model of subarachnoid hemorrhage. Brain Res 1585:63–71. https://doi.org/10.1016/j.brainres.2014.08.012
Wendel C, Scheibe R, Wagner S et al (2019) Decrease of blood flow velocity in the middle cerebral artery after stellate ganglion block following aneurysmal subarachnoid hemorrhage: a potential vasospasm treatment? J Neurosurg:1–7. https://doi.org/10.3171/2019.5.jns182890
Narouze S (2014) Ultrasound-guided stellate ganglion block: safety and efficacy. Curr Pain Headache Rep:18
Heros RC, Zervas NT, Varsos V (1983) Cerebral vasospasm after subarachnoid hemorrhage: an update. Ann Neurol 14:599–608. https://doi.org/10.1002/ana.410140602
Gupta MM, Bithal PK, Dash HH et al (2005) Effects of stellate ganglion block on cerebral haemodynamics as assessed by transcranial Doppler ultrasonography. Br J Anaesth 95:669–673. https://doi.org/10.1093/bja/aei230
Jadon A (2011) Revalidation of a modified and safe approach of stellate ganglion block. Indian J Anaesth 55:52–56. https://doi.org/10.4103/0019-5049.76601
Wang D (2018) Image guidance technologies for interventional pain procedures: ultrasound, fluoroscopy, and CT. Curr Pain Headache Rep 22
Narouze S, Vydyanathan A, Patel N (2007) Ultrasound-guided stellate ganglion block successfully prevented esophageal puncture. Pain Physician 10:747–752
Chaturvedi A, Dash HH (2010) Locked-in syndrome during stellate ganglion block. Indian J Anaesth 54:324–326. https://doi.org/10.4103/0019-5049.68376
Lu F, Tian J, Dong J, Zhang K (2019) Tonic-clonic seizure during the ultrasound-guided stellate ganglion block because of an injection into an unrecognized variant vertebral artery: a case report. Med (United States):98. https://doi.org/10.1097/MD.0000000000018168
Goel V, Patwardhan AM, Ibrahim M et al (2019) Complications associated with stellate ganglion nerve block: a systematic review. Reg Anesth Pain Med 44:669–678
Treggiari MM, Romand JA, Martin JB et al (2003) Cervical sympathetic block to reverse delayed ischemic neurological deficits after aneurysmal subarachnoid hemorrhage. Stroke 34:961–966. https://doi.org/10.1161/01.STR.0000060893.72098.80
Kwon HJ, Lim JW, Koh HS et al (2019) Stent-retriever angioplasty for recurrent post-subarachnoid hemorrhagic vasospasm – a single center experience with long-term follow-up. Clin Neuroradiol 29:751–761. https://doi.org/10.1007/s00062-018-0711-3
Hockel K, Diedler J, Steiner J et al (2016) Long-term, continuous intra-arterial nimodipine treatment of severe vasospasm after aneurysmal subarachnoid hemorrhage. World Neurosurg 88:104–112. https://doi.org/10.1016/j.wneu.2015.11.081
Rowland MJ, Hadjipavlou G, Kelly M et al (2012) Delayed cerebral ischaemia after subarachnoid haemorrhage: looking beyond vasospasm. Br J Anaesth 109:315–329
Brami J, Chousterman B, Boulouis G et al (2020) Delayed cerebral infarction is systematically associated with a cerebral vasospasm of large intracranial arteries. Clin Neurosurg 86:E175–E183. https://doi.org/10.1093/neuros/nyz340
Hill MD, Goyal M, Menon BK et al (2020) Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet 395:878–887. https://doi.org/10.1016/S0140-6736(20)30258-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pileggi, M., Mosimann, P.J., Isalberti, M. et al. Stellate ganglion block combined with intra-arterial treatment: a “one-stop shop” for cerebral vasospasm after aneurysmal subarachnoid hemorrhage—a pilot study. Neuroradiology 63, 1701–1708 (2021). https://doi.org/10.1007/s00234-021-02689-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02689-9