Abstract
Purpose
Infarct growth and final infarct volume are established outcome modifiers following endovascular thrombectomy (EVT) for patients with large vessel occlusion stroke (LVO). Simple techniques for final infarct volume measurement are lacking, and therefore, we tested whether post-EVT ASPECTS can be used for prognostic evaluation after EVT.
Methods
Infarct size at baseline was measured in a prospective cohort of patients with LVO that underwent EVT with the ASPECTS score on admission non-contrast CT. Final infarct size was assessed with a post-EVT ASPECTS (ASPECTS-POST) obtained from a follow-up CT 24–72 h post-EVT. The best performing ASPECTS-POST was chosen based on comparisons of different thresholds. Outcome measures included survival rates and modified Rankin Score at 90 days.
Results
A total of 272 patients were included and 166 of them had an ASPECTS-POST ≥ 7. ASPECTS-POST ≥ 7 was associated with increased likelihood of favorable outcome at 90 days (67% vs. 21%, p < 0.001) with sensitivity, specificity, and positive and negative predictive values of 86%, 58%, 61%, and 85%, respectively. On multivariate analysis, ASPECTS-POST ≥ 7 was found to be a significant modifier of favorable outcome (Odds Ratio [OR] 6.2, 95% confidence intervals [CI] 3.1–12.4) and survival (OR 5.8 95% CI 2.4–14.3).
Conclusion
ASPECTS can be rapidly and easily obtained from the post-EVT NCCT and ASPECTS-POST ≥ 7 correlates with good outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Large vessel occlusion (LVO) in the anterior circulation causes large hemispheric infarctions that are amenable to treatment with endovascular thrombectomy (EVT) [1]. Early infarct growth [2,3,4] and final infarct volume [2, 5,6,7,8,9] have been associated with outcome in these patients. However, methods for evaluation of these parameters usually involved employing sophisticated software that is both time and resource consuming [2, 5,6,7,8,9,10,11,12]. A simpler, less expensive method of assessing infarct volumes may be advantageous under these circumstances. The Alberta Stroke Project Early CT Changes Score (ASPECTS) is a well-established simple-to-use tool for assessing infarct volumes on the pre-EVT non-contrast CT scans (NCCT) [13,14,15,16,17,18]. As such, it can be used for patient selection for EVT and is associated with outcome after EVT [13,14,15,16,17,18]. We therefore reasoned that assessment of ASPECTS on the post-EVT NCCT (ASPECTS-POST) can be used to prognosticate and may assist in making therapeutic decisions after EVT including rehabilitation status, nursing care placement, and withdrawal of care. Therefore, we aimed to identify cutoffs optimally correlated with outcome and examine the predictive value of these ASPECTS-POST cutoffs after EVT.
Patients and methods
All consecutive patients undergoing EVT for LVO were recruited into a prospective ongoing single-center database, and the data was retrospectively analyzed as previously described. The study was approved by the institutional review board that waived the need for obtaining informed consent due to the retrospective nature of the study.
The current study included patients who experienced an acute ischemic stroke with occlusion of the distal internal carotid artery (ICA) or M1 or M2 segments of the middle cerebral artery (MCA) proven on vascular imaging. Tandem occlusions were included. Distal occlusions to M3 segments of the MCA were not included. All patients underwent stentriever-assisted thrombectomy as the primary EVT modality but aspiration techniques were allowed as rescue. Patients that underwent systemic thrombolysis prior to EVT were included. Before 2018, only patients that presented within 7.5 h from symptom onset were included, but since 7/2018, patients treated up to 24 h from symptom onset were also included.
Overall, 282 consecutive patients with LVO that underwent EVT (mean age 70.2 ± 14.6, 53% females) were included in the database. The baseline characteristics of the study population are presented in Table 1. Of these, 272 patients (96%) had follow-up NCCT obtained 24–72 h after EVT that allowed scoring ASPECTS-POST and were included in the current study. Unenhanced brain CT images were obtained using standardized images on IQon-Spectral CT (Philips, Eindhoven, Holland) using the following parameters: kVp 120, mA 312, and ST 3 mm.
All EVT procedures were performed by two experienced interventionists (JEC and JMG), and the imaging data were analyzed retrospectively by 4 experienced stroke neurologists and fellows (RRL, AH, AF, and NS) that were blinded to outcomes. We collected demographics and vascular risk factor profile. Neurological deficits were measured with the National Institutes of Health Stroke Scale (NIHSS) at admission and discharge [19]. Stroke etiology was classified with the TOAST classification [20]. We also assessed time metrics, imaging variables including ASPECTS before and after treatment, and collateral status on the admission CTA when available [13]. In patients with previous strokes, the ASPECTS was calculated for the new stroke only.
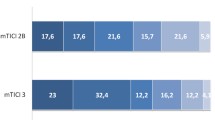
Data on procedural variables including the modified thrombolysis in cerebral infarction (mTICI) score at the end of the procedure and the number of passes needed to achieve the best possible recanalization were also studied [21]. mTICI2b-3 was considered as successful target vessel recanalization.
Functional outcome was assessed with the modified Rankin scale (mRS) [22] at 90 days from stroke, and an mRS ≤ 2 was considered as favorable outcome. Survival and symptomatic intracranial hemorrhage (sICH) rates determined according to the ECASS III criteria [23] were used as other outcome parameters.
Statistical analysis was performed using the SPSS 25 (IBM USA). p < 0.05 was considered significant. The χ2 test was used to explore the link between categorical variables. The Student’s t test was used to compare continuous variables. We determined sensitivity, specificity, and positive and negative predictive values for different ASPECTS-POST using crosstabs in order to determine the best values for clinical use. We next performed multivariate logistic regression modeling to test whether ASPECTS-POST had an impact on favorable outcome and survival. In the regression, we included variables that were shown to affect outcome in previous studies including age, successful reperfusion, collateral state, and stroke severity [5, 24] in addition to ASPECTS-POST.
Data availability
Individual de-identified participant data including vascular risk factor profiles, demographics, and procedural data as well as imaging findings will be shared in accordance with the Ministry of Health policies and regulations. Data sharing is limited for academic purposes only pending approval by the local IRB.
Results
Sensitivity, specificity, and positive and negative predictive values (PPV, NPV) for the correlation of different APSECTS-POST on favorite functional outcome (mRS ≤ 2) showed that the best predictive values are obtained with a cutoff of ASPECTS-POST ≥ 7 (Table 2). The sensitivity of ASPECTS-POST ≥ 7 was high (86%) but the specificity was relatively low (58%) with a high negative predictive value of 85% but a medium positive predictive value of 61%. For ASPECTS-POST ≥ 6, the sensitivity and NPV were slightly higher but the specificity and PPV were slightly lower which led us to use a cutoff of ASPECTS-POST ≥ 7 for the multivariate analyses.
In comparison with patients that had an ASPECTS-POST of < 7, those that had a score of ≥ 7 were significantly younger (68 ± 15 vs. 72 ± 18, p = 0.017), and less frequently had diabetes (23% vs. 40%; p = 0.003; Table 3). Patients in the ASPECTS-POST group ≥ 7 also had significantly lower admission and discharge NIHSS scores (15.3 ± 7 and 3.3 ± 4 vs. 18.1 ± 6 and 11.8 ± 7, respectively; p < 0.001 for both), and more often had favorable collateral profiles (62% vs. 25%; p < 0.001). These patients also had higher likelihood of favorable target recanalization (92% vs. 80%; p = 0.003) and lower likelihood of symptomatic ICH (1% vs. 9%; p = 0.002). Survival and favorable functional outcome rates were also significantly higher in patients that had an ASPECTS-POST ≥ 7 (95% vs. 76% and 67% vs. 21%; p < 0.001 for both, Table 3).
On the multivariate analysis for favorable outcome at 90 days post-stroke (Table 4), ASPECTS-POST ≥ 7 and successful recanalization remained significant positive modifiers for achieving functional independence while age and admission NIHSS remained negative modifiers of favorable outcome.
On multivariate analysis for survival at 90 days post-EVT (Table 5), ASPECTS-POST ≥ 7 remained the sole positive modifier of survival whereas age and admission NIHSS were found to negatively affect survival.
Discussion
The current study identifies ASPECTS-POST ≥ 7 as a positive marker of survival and favorable functional outcome at 90 days post-EVT. We hypothesized that the effect of ASPECTS-POST should be similar to the effect of lesion growth and final infarct volume that were previously shown to affect long-term outcome after EVT [3, 5, 6, 8,9,10,11,12]. Our results corroborate this association although ASPECTS-POST estimation of lesion volume may possibly be less accurate compared with more precise measurement of lesion volume with dedicated volumetric software [10, 11]. Furthermore, magnetic resonance imaging parameters such as diffusion- and perfusion-weighted sequences may better correlate with outcome [25, 26], and an MRI-based ASPECTS-like imaging may be easily obtained. However, MRI may be problematic in that it is not as widely available as CT and that there are patients with absolute (e.g., shrapnel) or relative (e.g., claustrophobia, pacemakers) contraindications for imaging. Therefore, we suggest that using ASPECTS-POST ≥ 7 as a prognostic marker is advantageous given the simplicity and reproducibility of ASPECTS acquisition compared with the use of designated specialized software or naked eye estimations of the lesion volume. Furthermore, recent studies have shown that automated software determination of ASPECTS is feasible and more accurate than ascertainment of ASPECTS even by experienced radiologists [27]. Use of such strategies will simplify data acquisition even further making it very accurate and simple to use. Furthermore, while sophisticated multimodal neurovascular imaging is usually used before EVT for optimal patient selection, this type of imaging studies is usually not used after EVT. The sole use of clinical parameters such as the degree of neurological disability obtained on the NIHSS [28] or similar scales post-procedure may have its values but may be inaccurate in itself because other conditions such as infections, pulmonary embolism, and cardiac decompensation may influence the degree of neurological deficits. Thus, a prognostic imaging marker after completion of EVT is needed. As such, ASPECTS-POST can theoretically be used to prognosticate outcomes and guide therapeutic decisions after EVT such as suitability for rehabilitation on the one hand and withdrawal of care on the other. Other known markers for favorable outcome such as younger age, lower stroke severity, favorable collateral profile, lower number of stentriever passes needed to recanalize the occluded vessel, and higher likelihoods of favorable recanalization were all correlated with ASPECTS-POST ≥ 7.
Despite the high sensitivity and NPV observed, our data suggests that ASPECTS-POST ≥ 7 is still not a perfect surrogate predictor of outcome given the relatively low specificity and PPV observed in the current study. Interestingly, it was argued that since infarcts continue to grow over time in some patients, possibly due to progressive collateral failure, measurement of final infarct volume should be delayed for one week [11]. Thus, the relatively early determination of ASPECTS-POST in the current study which utilized the first post-EVT NCCT scan may have contributed to the relatively low specificity and PPV values observed in the current study. Therefore, and for reasons of simplicity, we suggest to further study the correlation of ASPECTS-POST obtained at 4–7 days post-EVT compared with outcome measures in future studies and examine whether PPV and specificity will improve. Another limitation for using the ASPECTS as a predictor of outcome is that the ASPECTS only accounts for lesions involving the MCA territory, and in cases with ICA occlusion affecting also the anterior cerebral, it may underestimate the actual damage, thus lowering its ability to predict outcome in such patients with a known poor prognostic marker such as ACA involvement [29]. Furthermore, ASPECTS is not calibrated to account for lesion eloquence. Thus, it is likely that patients with an ASPECTS of 7 with points taken off because of three separate eloquent cortical lesions (e.g., including the language area and motor cortex) will fare differently than those with an APSECTS of 7 in whom the points were deducted due to lesions involving less eloquent areas (e.g., right frontal area). Lesion side which is not accounted for in the ASPECTS may also influence outcomes such that a small infarct in the left temporal cortex could be more disabling than a large right frontal infarct. These drawbacks which are shared by all methods of infarct volume measurement may be responsible for the imperfect prediction of outcome by such methods. Ongoing research combining total lesion volume assessment with lesion side and relative eloquence of the affected brain lesions should help to determine if such a combinatory approaches may better predict outcome.
The current study has several advantages including the facts that the patients represent a typical non-selected population of LVO patients which depicts real-life status and that it did not use strict inclusion criteria.
Our study also has several limitations including the fact that it was based on single-center data and that the data was retrospectively analyzed. Furthermore, ASPECTS-POST was not determined by investigators that were blinded to the EVT result; although given the retrospective nature of the study, it is unlikely that the evaluators were biased in their scoring. Third, by assessing properties at multiple thresholds and then choosing the best performing cutoff for further analyses within the same dataset, a bias that favors the prognostic tool may have been created, and external validation will be needed to test whether these cutoffs are the best. Fourth, the multivariable model for assessment of the impact of ASPECTS-POST on survival model could be under-powered. Therefore, the results should be interpreted cautiously and need corroboration in a larger data set.
In conclusion, ASPECTS-POST ≥ 7 is an easily obtained marker that is correlated to survival and favorable functional outcome. ASPECTS-POST ≥ 7 may add significant prognostic information following EVT in patients with LVO, and future studies could use this marker as part of a prognostic scale after EVT.
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millan M, Davis SM, Roy D, Thornton J, Roman LS, Ribo M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, collaborators H (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Albers GW, Goyal M, Jahan R, Bonafe A, Diener HC, Levy EI, Pereira VM, Cognard C, Yavagal DR, Saver JL (2015) Relationships between imaging assessments and outcomes in solitaire with the intention for thrombectomy as primary endovascular treatment for acute ischemic stroke. Stroke 46(10):2786–2794. https://doi.org/10.1161/STROKEAHA.115.010710
Man S, Aoki J, Hussain MS, Wisco D, Tateishi Y, Toth G, Hui FK, Uchino K (2015) Predictors of infarct growth after endovascular therapy for acute ischemic stroke. J Stroke Cerebrovasc Dis 24(2):401–407. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.09.004
Marks MP, Lansberg MG, Mlynash M, Kemp S, McTaggart R, Zaharchuk G, Bammer R, Albers GW, Investigators D (2014) Correlation of AOL recanalization, TIMI reperfusion and TICI reperfusion with infarct growth and clinical outcome. J Neurointerv Surg 6(10):724–728. https://doi.org/10.1136/neurintsurg-2013-010973
Al-Ajlan FS, Al Sultan AS, Minhas P, Assis Z, de Miquel MA, Millan M, San Roman L, Tomassello A, Demchuk AM, Jovin TG, Cuadras P, Davalos A, Goyal M, Menon BK, Investigators R (2018) Posttreatment infarct volumes when compared with 24-hour and 90-day clinical outcomes: insights from the REVASCAT randomized controlled trial. AJNR Am J Neuroradiol 39(1):107–110. https://doi.org/10.3174/ajnr.A5463
Al-Ajlan FS, Goyal M, Demchuk AM, Minhas P, Sabiq F, Assis Z, Willinsky R, Montanera WJ, Rempel JL, Shuaib A, Thornton J, Williams D, Roy D, Poppe AY, Jovin TG, Sapkota BL, Baxter BW, Krings T, Silver FL, Frei DF, Fanale C, Tampieri D, Teitelbaum J, Lum C, Dowlatshahi D, Shankar JJ, Barber PA, Hill MD, Menon BK, Investigators ET (2016) Intra-arterial therapy and post-treatment infarct volumes: insights from the ESCAPE randomized controlled trial. Stroke 47(3):777–781. https://doi.org/10.1161/STROKEAHA.115.012424
Albers GW, Goyal M, Jahan R, Bonafe A, Diener HC, Levy EI, Pereira VM, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, de Rochemont RM, Singer OC, Bammer R, Saver JL (2016) Ischemic core and hypoperfusion volumes predict infarct size in SWIFT PRIME. Ann Neurol 79(1):76–89. https://doi.org/10.1002/ana.24543
Boers AMM, Jansen IGH, Brown S, Lingsma HF, Beenen LFM, Devlin TG, Roman LS, Heo JH, Ribo M, Almekhlafi MA, Liebeskind DS, Teitelbaum J, Cuadras P, du Mesnil de Rochemont R, Beaumont M, Brown MM, Yoo AJ, Donnan GA, Mas JL, Oppenheim C, Dowling RJ, Moulin T, Agrinier N, Lopes DK, Aja Rodriguez L, Compagne KCJ, Al-Ajlan FS, Madigan J, Albers GW, Soize S, Blasco J, Davis SM, Nogueira RG, Davalos A, Menon BK, van der Lugt A, Muir KW, Roos Y, White P, Mitchell PJ, Demchuk AM, van Zwam WH, Jovin TG, van Oostenbrugge RJ, Dippel DWJ, Campbell BCV, Guillemin F, Bracard S, Hill MD, Goyal M, Marquering HA, Majoie C (2019) Mediation of the relationship between endovascular therapy and functional outcome by follow-up infarct volume in patients with acute ischemic stroke. JAMA Neurol 76(2):194–202. https://doi.org/10.1001/jamaneurol.2018.3661
Zaidi SF, Aghaebrahim A, Urra X, Jumaa MA, Jankowitz B, Hammer M, Nogueira R, Horowitz M, Reddy V, Jovin TG (2012) Final infarct volume is a stronger predictor of outcome than recanalization in patients with proximal middle cerebral artery occlusion treated with endovascular therapy. Stroke 43(12):3238–3244. https://doi.org/10.1161/STROKEAHA.112.671594
Boers AM, Marquering HA, Jochem JJ, Besselink NJ, Berkhemer OA, van der Lugt A, Beenen LF, Majoie CB, Investigators MC (2013) Automated cerebral infarct volume measurement in follow-up noncontrast CT scans of patients with acute ischemic stroke. AJNR Am J Neuroradiol 34(8):1522–1527. https://doi.org/10.3174/ajnr.A3463
Krongold M, Almekhlafi MA, Demchuk AM, Coutts SB, Frayne R, Eilaghi A (2015) Final infarct volume estimation on 1-week follow-up MR imaging is feasible and is dependent on recanalization status. Neuroimage Clin 7:1–6. https://doi.org/10.1016/j.nicl.2014.10.010
Yoo AJ, Chaudhry ZA, Nogueira RG, Lev MH, Schaefer PW, Schwamm LH, Hirsch JA, Gonzalez RG (2012) Infarct volume is a pivotal biomarker after intra-arterial stroke therapy. Stroke 43(5):1323–1330. https://doi.org/10.1161/STROKEAHA.111.639401
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 355(9216):1670–1674
Bhuva P, Yoo AJ, Jadhav AP, Jovin TG, Haussen DC, Bonafe A, Budzik RJ, Yavagal DR, Hanel RA, Hassan AE, Ribo M, Cognard C, Sila CA, Morgan PM, Zhang Y, Shields R, Smith W, Saver JL, Liebeskind DS, Nogueira RG, Investigators DT (2019) Noncontrast computed tomography Alberta Stroke Program Early CT Score may modify intra-arterial treatment effect in DAWN. Stroke:STROKEAHA118024583. https://doi.org/10.1161/STROKEAHA.118.024583
Broocks G, Rajput F, Hanning U, Faizy TD, Leischner H, Schon G, Gellissen S, Sporns P, Deb-Chatterji M, Thomalla G, Kemmling A, Fiehler J, Flottmann F (2018) Highest lesion growth rates in patients with hyperacute stroke. Stroke:STROKEAHA118023457. https://doi.org/10.1161/STROKEAHA.118.023457
Hill MD, Demchuk AM, Goyal M, Jovin TG, Foster LD, Tomsick TA, von Kummer R, Yeatts SD, Palesch YY, Broderick JP, Investigators IMS (2014) Alberta Stroke Program early computed tomography score to select patients for endovascular treatment: Interventional Management of Stroke (IMS)-III Trial. Stroke 45(2):444–449. https://doi.org/10.1161/STROKEAHA.113.003580
Park JS, Lee JM, Kwak HS, Chung GH (2019) Predictive value of CT angiography source image ASPECTS in patients with anterior circulation acute ischemic stroke after endovascular treatment: ultimate infarct size and clinical outcome. J Neurointerv Surg 11(4):342–346. https://doi.org/10.1136/neurintsurg-2018-014359
Yoo AJ, Berkhemer OA, Fransen PS, van den Berg LA, Beumer D, Lingsma HF, Schonewille WJ, Sprengers ME, van den Berg R, van Walderveen MA, Beenen LF, Wermer MJ, Nijeholt GJ, Boiten J, Jenniskens SF, Bot JC, Boers AM, Marquering HA, Roos YB, van Oostenbrugge RJ, Dippel DW, van der Lugt A, van Zwam WH, Majoie CB, Investigators MC (2016) Effect of baseline Alberta Stroke Program Early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised phase 3 trial (MR CLEAN). Lancet Neurol 15(7):685–694. https://doi.org/10.1016/S1474-4422(16)00124-1
Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, Spilker J, Holleran R, Eberle R, Hertzberg V et al (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20(7):864–870
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24(1):35–41
Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, Dillon W, Warach S, Broderick J, Tilley B, Sacks D (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34(8):e109–e137
Rankin J (1957) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2(5):200–215. https://doi.org/10.1177/003693305700200504
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, Investigators E (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359(13):1317–1329. https://doi.org/10.1056/NEJMoa0804656
Broocks G, Kniep H, Schramm P, Hanning U, Flottmann F, Faizy T, Schonfeld M, Meyer L, Schon G, Aulmann L, Machner B, Royl G, Fiehler J, Kemmling A (2019) Patients with low Alberta Stroke Program Early CT Score (ASPECTS) but good collaterals benefit from endovascular recanalization. J Neurointerv Surg 12:747–752. https://doi.org/10.1136/neurintsurg-2019-015308
Baird AE, Lovblad KO, Dashe JF, Connor A, Burzynski C, Schlaug G, Straroselskaya I, Edelman RR, Warach S (2000) Clinical correlations of diffusion and perfusion lesion volumes in acute ischemic stroke. Cerebrovasc Dis 10(6):441–448. https://doi.org/10.1159/000016105
Lovblad KO, Baird AE, Schlaug G, Benfield A, Siewert B, Voetsch B, Connor A, Burzynski C, Edelman RR, Warach S (1997) Ischemic lesion volumes in acute stroke by diffusion-weighted magnetic resonance imaging correlate with clinical outcome. Ann Neurol 42(2):164–170. https://doi.org/10.1002/ana.410420206
Albers GW, Wald MJ, Mlynash M, Endres J, Bammer R, Straka M, Maier A, Hinson HE, Sheth KN, Taylor Kimberly W, Molyneaux BJ (2019) Automated calculation of Alberta Stroke Program Early CT Score: validation in patients with large hemispheric infarct. Stroke 50(11):3277–3279. https://doi.org/10.1161/STROKEAHA.119.026430
Reznik ME, Yaghi S, Jayaraman MV, McTaggart RA, Hemendinger M, Mac Grory BC, Burton TM, Cutting SM, Siket MS, Madsen TE, Thompson BB, Wendell LC, Mahta A, Potter NS, Furie KL (2018) Baseline NIH Stroke Scale is an inferior predictor of functional outcome in the era of acute stroke intervention. Int J Stroke 13(8):806–810. https://doi.org/10.1177/1747493018783759
King S, Khatri P, Carrozella J, Spilker J, Broderick J, Hill M, Tomsick T (2007) Anterior cerebral artery emboli in combined intravenous and intra-arterial rtPA treatment of acute ischemic stroke in the IMS I and II trials. AJNR Am J Neuroradiol 28(10):1890–1894. https://doi.org/10.3174/ajnr.A0702
Funding
This study was supported in part by the Peritz and Chantal Scheinberg Cerebrovascular Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not obtained from all individual participants included in the study because the IRB approved a retrospective analysis of anonymized data without the need to obtain informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leker, R.R., Honig, A., Filioglo, A. et al. Post-stroke ASPECTS predicts outcome after thrombectomy. Neuroradiology 63, 769–775 (2021). https://doi.org/10.1007/s00234-020-02576-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02576-9