Abstract
Introduction
The characteristics of dementia with Lewy bodies (DLB), Alzheimer’s disease (AD) and amnestic mild cognitive impairment (a-MCI) overlap but require different treatments; therefore, it is important to differentiate these pathologies. Assessment of dopamine uptake in the striatum using dopamine transporter (DaT) single-photon emission computed tomography (SPECT) is the gold standard for diagnosing DLB; however, this modality is expensive, time consuming and involves radiation exposure. Degeneration of the substantia nigra nigrosome-1, which occurs in DLB, but not in AD/a-MCI, can be identified by 3T susceptibility-weighted imaging (SWI). Therefore, the aim of this retrospective observational study was to compare SWI with DaT-SPECT for differentiation of DLB from AD/a-MCI.
Methods
SWI data were acquired for patients with clinically diagnosed DLB (n = 29), AD (n = 18), a-MCI (n = 13) and healthy controls (n = 26). Images were analysed for nigrosome-1 degeneration. Diagnostic accuracy was evaluated for DLB, AD and a-MCI compared with striatal dopamine uptake using DaT-SPECT.
Results
SWI achieved 90% diagnostic accuracy (93% sensitivity, 87% specificity) for the detection of nigrosome-1 degeneration in DLB and not in AD/a-MCI as compared with 88.3% accuracy (93% sensitivity, 84% specificity) using DaT-SPECT.
Conclusions
SWI nigrosome-1 evaluation was useful in differentiating DLB from AD/a-MCI, with high accuracy. This less invasive and less expensive method is a potential alternative to DaT-SPECT for the diagnosis of DLB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dementia with Lewy bodies (DLB) is recognised as the second most common form of dementia among older individuals after Alzheimer’s disease (AD) [1]. Differentiating DLB from AD is challenging because the clinical, neuropsychological and pathological features of these pathologies overlap. Therefore, effective patient management requires reliable imaging markers for each disease.
DLB is included in spectrum of Lewy body diseases such as Parkinson’s disease (PD) and PD with dementia (PDD) [1–3]. Dopamine transporter (DaT) single-photon emission computed tomography (SPECT) with [123I]-2β-carbomethoxy-3β-(4-iodophenyl)-N-(3-fluoropropyl) nortropane (123I-FP-CIT, DaTscan) is the imaging technique most widely used to assess dopamine degeneration in the nigrostriatum when diagnosing PD and DLB [1, 4]. Low DaT uptake in the basal ganglia revealed by SPECT is included as a suggestive feature in the revised criteria for the clinical diagnosis of DLB [1]. In contrast, uptake is preserved in the basal ganglia of patients with clinically diagnosed AD [1, 4]. However, because DaT-SPECT is expensive and exposes the subject to ionising radiation, less-invasive markers of dopaminergic degeneration are required.
Nigrosomes are calbindin-poor areas in the substantia nigra pars compacta (SNc). The loss of nigral dopaminergic cells in patients with PD is particularly severe in nigrosome-1, which resides in the caudal and medio-lateral SNc [5]. Studies that detected the nigrosome-1 using 7T-magnetic resonance imaging (MRI) found that nigrosome-1 serves as a useful biomarker of PD [6–9]. Susceptibility-weighted imaging (SWI) using 3T MRI, which is widely used in clinical practice, can detect nigrosome-1 as a hyperintense signal area, called the “swallow tail” sign, in healthy controls (Fig. 1) [10–13].
Substantia nigra (SN) anatomy using susceptibility-weighted imaging (SWI). a SWI axial slice at the level of nigrosome-1 in the midbrain structures. b Schematic outlining the relevant anatomical structures. c A barn swallow. The appearance of the healthy nigrosome-1 using SWI resembles the tail of the swallow. 1, Red nucleus; 2, midbrain tegmentum; 3, aqueduct; 4, medial lemniscus; 5, nigrosome-1; 6, SN; and 7, cerebral peduncle
In contrast, the nigrosome-1 signal is decreased in PD and no swallow tail sign is apparent [10–13]. The nigrosome-1 SWI signal using 3T MRI remains high in AD but is diminished in DLB [14]; however, these were preliminary findings for one patient with AD and two with DLB. Therefore, the aim of the present study was to investigate the utility of SWI for detection of the swallow-tail sign to differentiate DLB from AD in a larger number of patients with AD or DLB. Additionally, patients with amnestic mild cognitive impairment (a-MCI), which is widely considered a prodromal stage of AD, were evaluated [15]. The specific objective of the present study was to evaluate the hypothesis that nigrosome-1 assessment using 3T SWI effectively differentiates DLB from AD/a-MCI with diagnostic performance similar to that of DaT-SPECT.
Materials and methods
Subjects
Eighty-six subjects aged ≥60 years (29 with probable DLB, 18 with AD dementia, 13 with a-MCI and 26 healthy controls) were retrospectively selected from patients previously admitted to our institution. All patients with DLB, AD and a-MCI were evaluated for dementia between February 2014 and December 2015 and underwent DaT-SPECT and SWI. A neurologist (R.S.) with 30 years of experience and another (Y.T.) with 5 years of experience performed the diagnoses of DLB, AD or a-MCI according to the Consensus DLB criteria [1], the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association (NINCDS–ADRDA) criteria [16] or Petersen’s criteria, respectively [15]. Each of the DLB and AD patients satisfied the probable AD conditions according to the probable DLB NINCDS–ADRDA criteria in the Consensus DLB criteria. The criteria for a-MCI included memory complaint (preferably corroborated by an informant), impaired memory function for age and education, preserved general cognitive function, intact activities of daily living and insufficient impairment to meet the criteria for dementia [15]. All recruited patients (a-MCI, AD and DLB) underwent the mini-mental state examination (MMSE) to evaluate general cognitive function. Detailed descriptions of the patients with DLB, AD and a-MCI are shown in Table 1.
A total of 26 age- and gender-matched healthy controls were recruited and underwent neurological examinations for complaints mainly comprising headache and vertigo. These subjects were screened using MRI including SWI and were judged free of neurological abnormalities by the neurologists. None of the healthy subjects underwent DaT-SPECT or had a history of dementia, hypertension, diabetes mellitus, cardiovascular disease, stroke, brain tumour, epilepsy, depression, drug abuse, head trauma, neurological or psychiatric disorders. The structural MRI findings of all controls were normal.
The ethics committee of Toho University approved the research protocols. Written informed consent was not required for this study because of its retrospective observational design.
SWI 3T MRI
MRIs were performed using a 3T MRI scanner (Skyra; Siemens, Erlangen, Germany) with a standard eight-channel head coil. The SWI sequence was gradient echo acquisition with magnitude and phase images obtained in the axial plane. SWI scans were the first to be incorporated in the MRI protocol. Parameters for SWI were as follows: TR/TE, 28/20; flip angle, 15°; number of slices, 40; voxel size, 0.9 × 0.9 × 2 mm; and scan duration, 108 s; only the magnitude image was used. All axial slices were acquired from a plane parallel to the splenium and genu of the corpus callosum. Acquired axial slice images were perpendicular to the fourth ventricle floor with coverage from the splenium of the corpus callosum to the inferior border of the pons.
Visual evaluation and semi-quantitative analysis of nigrosome-1
A neuroradiologist (K.K.) with 6 years of experience and another (T.N.) with 5 years of experience independently interpreted brain MRI data through visual and semi-quantitative assessments of nigrosome-1. Prior to nigrosome-1 assessments in this study, the raters performed SWI assessments in at least 20 AD and DLB cases. The neuroradiologists were uninformed of the patient diagnosis, clinical information and DaT-SPECT findings. Nigrosome-1 of each subject was classified by comparing signals in the centre of nigrosome-1 with white matter lateral to the decussation of the superior cerebellar peduncles, in accordance with the methods described in a previous study [12]. The types of nigrosome-1 revealed by SWI were classified into the following groups: group 1, normal (iso- or hyperintensity in the central region of the presumed bilateral nigrosome-1; Fig. 2a, b); group 2, possibly abnormal (hypointensity observed in one nigrosome-1 but not >50% of the presumed nigrosome-1 (Fig. 2c, d); and group 3, abnormal (hypointensity in one nigrosome-1 accounting for ≥50% of the presumed nigrosome-1; Fig. 2e, f). Any patient in which the left and right nigrosome-1 group numbers indicated assignment to different group numbers were assigned to the higher (i.e. worse) group number. Evaluation of nigrosome-1 was performed using single slices acquired in the axial plane, which most clearly defined nigrosome-1. For statistical analysis, group 1 was defined as the normal group, and groups 2 and 3 were combined into the abnormal group. Discrepancy in neuroradiological diagnoses was resolved by consensus.
Assessment of nigrosome-1 in the substantia nigra using 3T susceptibility-weighted imaging (six different patients). The green arrows indicate normal nigrosome-1, the yellow arrows indicate possibly abnormal nigrosome-1 and the red arrows indicate an abnormal nigrosome-1. a An Alzheimer’s disease (AD) patient (66-year-old woman, group 1; nigrosome-1 appears bilaterally normal). b An amnestic mild cognitive impairment (a-MCI) patient (62-year-old woman, group 1; nigrosome-1 appears bilaterally normal). c A dementia with Lewy bodies (DLB) patient (77-year-old woman, group 2; right nigrosome-1 appears normal, left nigrosome-1 appears possibly abnormal). d A DLB patient (77-year-old, woman, group 2; right nigrosome-1 appears normal, left nigrosome-1 appears possibly abnormal). e A DLB patient (71-year-old man, group 3; right nigrosome-1 appears possibly abnormal, left nigrosome-1 appears abnormal). f A DLB patient (77-year-old woman, group 3; right nigrosome-1 appears possibly abnormal, left nigrosome-1 appears abnormal)
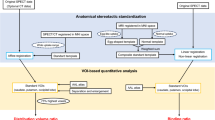
Semi-quantitative assessment was performed according to nigrosome-1 contrast by drawing small circular left and right regions of interest (ROIs) on the same slice used for visual assessment and inferred as nigrosome-1 regions from that assessment to be the nigrosome-1 regions. The signal intensity of each ROI was measured (Fig. 3). The sizes of the ROIs varied slightly between individuals to accommodate the entirety of each nigrosome-1 (Table S1). An ROI (9 pixels, 7.29 mm2) was drawn at the centre of the midbrain tegmentum, and signal intensity was defined as the background signal (Fig. 3). The mean signal intensity of nigrosome-1 was normalised to the mean value of the background signal of the midbrain tegmentum. The normalised mean signal intensity of nigrosome-1 was defined as the contrast ratio of nigrosome-1.
Procedure used to draw regions of interest (ROIs) in nigrosome-1 and the midbrain tegmentum. Representative susceptibility-weighted imaging (SWI) axial slice at the level of nigrosome-1 in the midbrain structures of a patient with Alzheimer’s disease. Locations of ROIs are depicted on the SWI axial slice at the level of nigrosome-1. The right nigrosome-1 (red), left nigrosome-1 (blue), right midbrain tegmentum (light green) and left midbrain tegmentum (purple) are outlined. Each ROI was demarcated to encompass the entire nigrosome-1; therefore, size varied slightly between individuals. An ROI of 9 pixels (7.29 mm2) was drawn at the centre of the midbrain tegmentum, where the signal intensity was measured and was defined as the background signal
DaT-SPECT
A dual-head gamma camera equipped with a low-medium-energy general purpose collimator (E. Cam; Toshiba Medical Systems, Tochigi, Japan) for DaT-SPECT scanning 4 h after injecting 123I-FP-CIT (DaTscan, 150–185 MBq). The gamma camera was calibrated using a photopeak of 159 keV, and an energy window of ±15%. SPECT acquisition was performed within a 128 × 128 matrix with steps of 4° over a range of 180°. Projection data were acquired for 28 min. Data were reconstructed using the ordered subset expectation maximisation method (iteration 8, subset 6).
Visual rating and semi-quantitative analysis of DaT-SPECT
Two neuroradiologists (K.K. and T.N.) with 3 years of experience in the interpretation of DaT-SPECT examined the DaT-SPECT results. The neuroradiologists were uninformed of the patient diagnosis, clinical information and nigrosome-1 findings. Scans were classified as follows: group 1, normal striatal uptake of 123I-FP-CIT in the right and left striata (Fig. 4a, b); group 2, a slight reduction in uptake in any of the striatum (Fig. 4c, d); and group 3, marked reduction in uptake in any of the striatum (Fig. 4e, f). For statistical analyses, group 1 was defined as the normal group, and groups 2 and 3 were combined into the abnormal group. Discrepancies between the neuroradiological diagnoses were resolved by consensus rating.
Assessment of striatal uptake using dopamine transporter (DaT)–single-photon emission computed tomography (SPECT) in six different DLB, AD and a-MCI patients (same patient group as in the Fig. 2). The green arrows indicate normal striatal uptake, the yellow arrows indicate slight reduction in striatal uptake and the red arrows indicate marked reduction in striatal uptake. a An AD patient (66-year-old woman, group 1; normal striatal uptake bilaterally). b An a-MCI patient (62-year-old woman, group 1; normal striatal uptake bilaterally). c A DLB patient (80-year-old man, group 2; slight reduction in left striatal uptake, normal right striatal uptake). d A DLB patient (81-year-old man, group 2; slight reduction in left striatal uptake, normal right striatal uptake). e A DLB patient (71-year-old man, group 3; marked reduction in striatal uptake bilaterally). f A DLB patient (77-year-old woman, group 3; slight reduction in right striatal uptake, marked reduction in left striatal uptake)
The specific binding ratio (SBR) was semi-quantitatively calculated using DaTView software (Nihon Medi-Physics, Tokyo, Japan) [17]. Semi-quantitative analysis of 123I-FP-CIT SPECT images can improve sensitivity and diagnostic accuracy [18]. Assessment of inter-rater reliability was unnecessary, because the SBR was calculated automatically using DaTView software and, therefore, free from rater bias. SBR was determined as the mean of the right and left SBRs.
Statistical analysis
IBM SPSS for Windows, version 20.0 (IBM, Armonk, NY, USA) was used to perform statistical analyses. The demographic and clinical data of the AD and a-MCI groups were combined (AD/a-MCI group) and compared with the DLB and control groups using analysis of variance (ANOVA) with the Tukey’s honest significant difference (HSD) test for continuous variables and the χ 2 test for categorical variables. A probability (p) value of <0.05 was considered statistically significant.
To assess inter-rater variability and reproducibility of visual assessment of SWI and DaT-SPECT, absolute inter-rater agreement and the kappa statistic (κ) were calculated. Inter-rater reliability for the contrast ratio of nigrosome-1 was assessed using the intraclass correlation coefficient.
The capacity to differentiate DLB from AD/a-MCI was calculated using the clinical diagnosis as the gold standard.
One-way ANOVA with the Tukey’s HSD test was used to compare the contrast ratio and ROI size of nigrosome-1 among patients with DLB or AD/a-MCI and healthy controls and to compare values of normalised mean signal intensity and ROI size of nigrosome-1. The unpaired t test was used to assess inter-group differences in SBR for DaT-SPECT.
Receiver operating characteristic (ROC) analysis was performed to compare the diagnostic utility of the normalised signal intensity of nigrosome-1 and SBR from DaT-SPECT between DLB and AD/a-MCI. The Pearson correlation test was used to determine correlations between the contrast ratio and the ROI size of nigrosome-1 or SBR of DaT-SPECT and disease duration or MMSE score in the DLB, AD/a-MCI and combined DLB/AD/a-MCI groups. The Pearson correlation test was also used to investigate correlations between the contrast ratio or ROI size of nigrosome-1 and the SBR of DaT-SPECT in the DLB, AD/a-MCI and combined DLB/AD/a-MCI groups. The mean values of the contrast ratio and the ROI size of nigrosome-1 between rater 1 and rater 2 were used for the Pearson correlation test.
Results
Clinical data
There were no significant differences in age (p = 0.77, ANOVA) and gender (p = 0.92, χ 2 test) among the AD/MCI, DLB and control groups (Table 1). Also, there was no significant difference in disease duration between patients with AD/a-MCI or DLB (p = 0.79, Student’s t test). As expected, because a-MCI patients have mild cognitive dysfunction and were included in the AD/a-MCI group, the MMSE scores of DLB patients were significantly lower than those of patients with AD/a-MCI (p = 0.02, Student’s t test).
Visual evaluation and semi-quantitative analysis of nigrosome-1
The image quality of the evaluable scans was sufficient and lacked motion artefacts. After assessing the presence or absence of nigrosome-1 on SWI, 79 of 86 cases were classified into the same groups by both raters (absolute inter-rater agreement, 92% [κ = 0.84, p < 0.001]). There were four inter-rater discrepancies between groups 2 and 3 (DLB, n = 3; AD, n = 1) and three between groups 1 and 2 (AD, n = 1; a-MCI, n = 1; controls, n = 1).
Patients were assigned to groups as follows: 25/29 DLB to group 3, two to group 2 and two to group 1; 27/31 AD/a-MCI to group 1, three to group 2 and one to group 3; and 24/26 controls to group 1, one to group 2 and one to group 3. For SWI evaluation of nigrosome-1, 78 patients were correctly classified (DLB, n = 27; AD, n = 15; a-MCI, n = 12; controls, n = 24). There were abnormal or normal findings for 33/86 and 53/86 patients, respectively (Table 2). There were left/right differences in group number in 13 cases (DLB, n = 7; AD, n = 2; a-MCI, n = 2; controls, n = 2). Sensitivity and specificity for the DLB and AD/a-MCI groups (n = 60) were 93 and 87%, respectively (Table 2). Positive and negative predictive values were 87.1% (27/31) and 93% (27/29), respectively (Table 2). Diagnostic accuracy was 90.0%.
The contrast ratio and ROI size of the nigrosome-1 (intraclass correlation coefficient) were reproducible to the extent of 0.98 and 0.84, respectively. There were no significant differences between raters for either right or left contrast ratio and ROI size (p > 0.05). Therefore, averages were used for additional analyses.
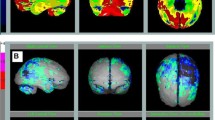
The contrast ratio of nigrosome-1 for both raters was significantly lower in patients with DLB, as compared with those with AD/a-MCI or healthy controls (p < 0.001) (Fig. 5a, b). There were no significant differences in the contrast ratios of nigrosome-1 between healthy controls and patients with AD/a-MCI (rater 1, p = 0.137; rater 2, p = 0.318) or in the ROI size of nigrosome-1 among groups (Table S1). In the DLB, AD/a-MCI and combined DLB/AD/a-MCI groups, the contrast ratio or ROI size of nigrosome-1 was not correlated with disease duration or MMSE score (p > 0.05).
a, b Box plot of nigrosome-1 intensity of healthy volunteers and patients with amnestic mild cognitive impairment (a-MCI), Alzheimer’s disease (AD), or dementia with Lewy bodies (DLB). c Box plot of specific binding ratio (SBR) in patients with a-MCI, AD or DLB. The plots indicate median values, and the boxes include upper and lower quartiles. Whiskers represent the lowest (highest) values within the 1.5 inter-quartile range from the box. Outliers are shown as small circles. d Receiver operating curve characteristics of the contrast ratio of nigrosome-1 and DaT-SPECT SBR. The nigrosome-1 contrast ratio of both raters showed better diagnostic performance, as compared with DaT-SPECT SBR. HC healthy controls
Accuracy of DLB diagnosis using DaT-SPECT
After assessing the DaT-SPECT, 55 of 60 patients were classified into the same groups by both raters (absolute inter-rater agreement, 97% [κ = 0.88, p < 0.001]). There were five inter-rater discrepancies between groups 2 and 3 (DLB, n = 1; AD, n = 1; a-MCI, n = 1).
The consensus rating assigned patients as follows: 25/29 DLB, group 3, two to group 2 and two to group 1 and 26/31 AD/a-MCI to group 1, two to group 2 and three to group 3. Consensus DaT-SPECT evaluation correctly classified 53 patients (DLB, n = 27; AD, n = 15; a-MCI, n = 11). There were 32/60 and 38/60 abnormal and normal results, respectively, with 93% sensitivity and 84% specificity (Table 2). Positive and negative predictive values were 84.4% (27/32) and 92.9% (26/28), respectively. Diagnostic accuracy was 88.3%.
The SBR of DaT-SPECT was significantly lower in patients with DLB, as compared with those of AD/a-MCI patients (p < 0.001) (Fig. 5c). The SBR of DaT-SPECT of the DLB was positively correlated with disease duration (r = 0.40, p = 0.03). The DaT-SPECT SBR was not correlated with disease duration or MMSE score for the AD/a-MCI and combined DLB/AD/a-MCI groups, respectively.
Comparison of SWI and DaT-SPECT findings
False negative SWIs were noted in two patients and for DaT in two patients, and one was the same as the SWI false negative. False positive results from SWI were noted for two of each of the patients with AD and a-MCI, respectively. False positive DaTs were observed for three and two patients with AD and a-MCI, respectively, and one each with AD and a-MCI was the same as the false positive SWI.
In the combined DLB/AD/a-MCI group, the mean contrast ratios for nigrosome-1 and SBR were positively correlated (r = 0.54, p < 0.001). The mean contrast ratios and MMSE scores for nigrosome-1 and SBR were not correlated in the separate DLB and AD/a-MCI groups (DLB group, r = 0.006, p = 0.98; AD/a-MCI group, r = 0.11, p = 0.57). ROC curves of the nigrosome-1 contrast ratio for both raters and the DaT-SPECT SBRs were plotted to determine their accuracies for distinguishing patients with DLB from those with AD/a-MCI (Fig. 5d), and the sensitivity and specificity of the nigrosome-1 contrast ratio for both raters and the DaT-SPECT SBR at each optimal cutoff point are summarised in Table 3. The nigrosome-1 contrast ratio for both raters performed better compared with the DaT-SPECT SBR (rater 1, mean cutoff, 0.87; sensitivity, 0.90; specificity, 0.86; rater 2, mean cutoff, 0.88; sensitivity, 0.94; specificity, 0.90). Areas under the ROC curve (Table 3) were 0.953, 0.968 and 0.892 for the nigrosome-1 contrast ratios of raters 1 and 2 and SBR of DaT-SPECT, respectively.
Discussion
This study revealed that using SWI, nigrosome-1 intensity is diminished in most patients with DLB and is maintained in those with AD/a-MCI as well as controls, consistent with the published data [14]. Furthermore, SWI nigrosome-1 evaluation was used to differentiate DLB from AD/a-MCI with high sensitivity and specificity. Visual assessment of nigrosome-1 using SWI was approximately as sensitive and specific as visual assessment of DaT-SPECT images. Moreover, semi-quantitative analyses according to nigrosome-1 contrast ratios were more sensitive and specific with SWI than DaT-SPECT.
A small number of researchers recently used 7T MRI to assess nigrosome-1 and confirmed that nigrosome-1 assessment is effective for the diagnosis of PD [6–10]. However, 7T MRI has limited availability in hospitals, making its clinical use difficult. Therefore, a number of studies have investigated whether 3T MRI, which is clinically available, is appropriate to assess nigrosome-1. In comparison to 7T MRI, 3T MRI has a lower magnetic field strength, which results in a reduced signal-to-noise ratio and weak T2* contrast and magnetic susceptibility effects of paramagnetic substances [19, 20], which are disadvantages when assessing nigrosome-1. However, several studies have indicated that 3T MRI can be used to assess nigrosome-1 [10–13]. The results of the present study, therefore, provide additional evidence that 3T MRI SWI images can be used to assess nigrosome-1. Furthermore, these findings indicate that nigrosome-1 is effective for assessment of DLB and AD/a-MCI. 123I-FP-CIT is a standard DaT-SPECT imaging ligand that generates in vivo images of DaT loss. Reduced binding in the basal ganglia reflects loss or dysfunction of nigrostriatal dopamine nerve terminals. Ligand uptake by DaT in the corpus striatum is reduced in patients with DLB, as compared with healthy individuals and patients with AD. DaT-SPECT is, therefore, useful to differentiate DLB from AD [1, 21]. In a phase III multicentre imaging study, DaT-SPECT differentiated DLB from AD with 78% sensitivity and 90% specificity [22]. Additionally, an autopsy study found that DaT-SPECT differentiated DLB from AD with 88% sensitivity and 100% specificity [21], which are similar to the findings reported here.
DaT-SPECT findings of decreased basal ganglia uptake represent the gold standard for diagnostic imaging of DLB and are included in the diagnostic criteria of DLB [1]. The present study found a significant positive correlation between SBR and disease duration. Striatal uptake using DaT-SPECT was correlated with disease duration, reflecting a loss of dopaminergic neurons [23–26], which is consistent with the findings of the present study. Moreover, there was no significant correlation between MMSE findings and DaT-SPECT striatal uptake, again supporting previous descriptions of the lack of correlation between MMSE findings, which reflect global cognitive functions and striatal dopaminergic function [25, 27].
However, DaT-SPECT still has some drawbacks, including the need for radiation exposure, the high cost and prolonged imaging time. SWI is non-invasive and cheaper and involves a short imaging time, so nigrosome-1 evaluation using SWI offers many advantages for the diagnosis of DLB. Ideally, this method could supplant DaT-SPECT for the diagnosis of DLB.
Marked degeneration of nigrosome-1 of patients with PD occurs in the SNc [5]. In DLB, as established by a previous autopsy study, significant nigrostriatal degeneration and DAT loss occur [28]. Nerve cell loss in the SNc is also more conspicuous in DLB than in patients with AD and healthy individuals [29]. Decreased nigrosome-1 signals are thought to reflect SNc degeneration. A diminished nigrosome-1 signal may reflect increased iron deposition associated with SNc degeneration and decreased neuromelanin accompanied by decreased iron stores [13, 30]. This may cause an increase in free iron accompanied by paramagnetic properties [13, 30]. If such findings reflect nigrosome-1 degradation, it is reasonable to expect a positive correlation between DaT-SPECT SBR, which represents nigrostriatal dopaminergic activity and the contrast ratio of nigrosome-1. In this study, there was a significant correlation between the contrast ratio and the SBR in the AD/a-MCI/DLB combined group, whereas there was no significant correlation when correlation analysis was performed individually with the AD/a-MCI and DLB groups. Therefore, the results of the present study merely indicated that the SBRs and contrast ratios were high in the AD/a-MCI group and low in the DLB group. Alternatively, the number of cases in each group was likely insufficient to allow detection of a significant correlation.
False positive nigrosome-1 data were associated with 4/33 patients with abnormal results, which may be explained by our use of clinical diagnoses, some of which may be incorrect. No patient with false positive results had preclinical symptoms of Lewy body disease, such as rapid eye movement, sleep behavioral disorders, anosmia or autonomic dysfunction. However, incidental Lewy pathology or presymptomatic Lewy body disease may coexist in patients with AD and a-MCI as well as healthy controls, leading to false positive results using SWI. Moreover, incidental Lewy pathology and mild SN neuron degeneration occurs in 7.8% of healthy individuals aged ≥60 [22]. For example, 22.5% of such patients with AD exhibit incidental Lewy pathology, and 14% show mild loss of SN neurons [22]. This comorbidity with incidental Lewy pathology, loss of SN neurons or both may lead to false positive results for nigrosome-1.
Similarly, reliance on similar clinical diagnoses may help explain the false negative results for nigrosome-1 in DLB, and therefore, the possibility of errors in the clinical diagnosis of DLB cannot be excluded. Furthermore, the patients with DLB may include those with extensive cortical Lewy body pathology without nigrostriatal involvement. DLB is pathologically classified as brainstem, limbic and neocortical types according to the distribution and frequency of Lewy pathology [1]. The majority of pathological studies emphasise SN Lewy pathology as a constant in each pathological subtype [31–33]. However, isolated cases of DLB patients with cortical, but not brainstem, Lewy body pathology have been reported on rare occasions [34]. DLB cases in the present study may have included cases in which Lewy pathology had not yet reached the nigrostriatal area.
Limitations of this study include the possibility of misdiagnosis of DLB, AD and a-MCI due to the lack of histopathological confirmation. In addition, evaluations of nigrosome-1 using SWI and striatum DaT-SPECT were performed visually and did not include analysis using an automated diagnostic system. However, SWI nigrosome-1 and DaT-SPECT striatum evaluations were performed by two raters uniformed of patient clinical data, and high inter-rater agreement was achieved (approximately 90%) for both. However, because visual assessment of nigrosome-1 using SWI can be difficult, it may be necessary for raters to practice nigrosome-1 assessment. In cases in which nigrosome-1 signals are very faint, it is often difficult to categorise such cases as belonging to group 1 (normal) or group 2 (possibly abnormal) because it is not possible to determine whether very faint signals are artefacts/noise or actual abnormalities. In this study, the raters had differing opinions on the classification of three cases to group 1 or 2. To overcome difficulties that are inherent in visual assessment, a semi-quantitative method may be effective to measure the signal ratio between nigrosome-1 and midbrain tegmentum signals using ROI, as was done in this study. Semi-quantitative analysis of nigrosome-1 is relatively simple and offers high reproducibility (intraclass correlation coefficient, 0.98). Therefore, this method may be useful in clinical settings. It should be noted that image quality of SWI images is extremely important for nigrosome-1 analysis. Fortunately, in this study, no case had poor image quality or strong motion artefacts. However, because nigrosome-1 has an extremely small structure, even small amounts of noise or motion artifacts render assessment difficult. In this study, SWI imaging took only 108 s to complete, and the SWI scans were the first to be incorporated in the MRI protocol, which could explain the absence of motion artifacts. In addition, the resolution of the SWI sequence used in this study was 0.9 × 0.9 × 2 mm, which was slightly inferior to that used by Schwarz et al. (0.55 × 0.55 × 0.7 mm or 0.43 × 0.43 × 0.75) and Noh et al. (0.9 × 0.9 × 2 mm, particularly at a slice thickness of 2 mm). Thus, the use of higher resolution images could improve both the nigrosome-1 assessment and the ability to diagnose DLB.
In conclusion, the results of the present study showed that assessment of nigrosome-1 using 3T SWI was able to differentiate DLB from AD/a-MCI with sensitivity and specificity comparable to DaT-SPECT. Although this was a retrospective case–control study of a small number of subjects, these preliminary results indicate that SWI and DaT-SPECT are useful to differentiate DLB from AD/a-MCI.
Abbreviations
- AD:
-
Alzheimer’s disease
- a-MCI:
-
Amnestic mild cognitive impairment
- DLB:
-
Dementia with Lewy bodies
- DaT:
-
Dopamine transporter
- MMSE:
-
Mini-mental state examination
- MRI:
-
Magnetic resonance imaging
- NINCDS–ADRDA:
-
National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association
- PD:
-
Parkinson’s disease
- PDD:
-
Parkinson’s disease with dementia
- SBR:
-
Specific binding ratio
- SPECT:
-
Single-photon emission computed tomography
- SWI:
-
Susceptibility-weighted imaging
- 123I-FP-CIT:
-
[123I]-2β-carbomethoxy-3β-(4-iodophenyl)-N-(3-fluoropropyl) nortropane
References
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A, Kosaka K, Lee VM, Lees A, Litvan I, Londos E, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ, Yamada M (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65(12):1863–1872. doi:10.1212/01.wnl.0000187889.17253.b1
McKeith I, Mintzer J, Aarsland D, Burn D, Chiu H, Cohen-Mansfield J, Dickson D, Dubois B, Duda JE, Feldman H, Gauthier S, Halliday G, Lawlor B, Lippa C, Lopez OL, Carlos Machado J, O'Brien J, Playfer J, Reid W, International Psychogeriatric Association Expert Meeting on DLB (2004) Dementia with Lewy bodies. The Lancet Neurology 3(1):19–28
McKeith I (2007) Dementia with Lewy bodies and Parkinson’s disease with dementia: where two worlds collide. Pract Neurol 7(6):374–382. doi:10.1136/jnnp.2007.134163
Bajaj N, Hauser RA, Grachev ID (2013) Clinical utility of dopamine transporter single photon emission CT (DaT-SPECT) with (123I) ioflupane in diagnosis of parkinsonian syndromes. J Neurol Neurosurg Psychiatry 84(11):1288–1295. doi:10.1136/jnnp-2012-304436
Damier P, Hirsch EC, Agid Y, Graybiel AM (1999) The substantia nigra of the human brain. II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain 122(Pt 8):1437–1448
Blazejewska AI, Schwarz ST, Pitiot A, Stephenson MC, Lowe J, Bajaj N, Bowtell RW, Auer DP, Gowland PA (2013) Visualization of nigrosome 1 and its loss in PD: pathoanatomical correlation and in vivo 7 T MRI. Neurology 81(6):534–540. doi:10.1212/WNL.0b013e31829e6fd2
Cosottini M, Frosini D, Pesaresi I, Costagli M, Biagi L, Ceravolo R, Bonuccelli U, Tosetti M (2014) MR imaging of the substantia nigra at 7 T enables diagnosis of Parkinson disease. Radiology 271(3):831–838. doi:10.1148/radiol.14131448
Kwon DH, Kim JM, SH O, Jeong HJ, Park SY, ES O, Chi JG, Kim YB, Jeon BS, Cho ZH (2012) Seven-Tesla magnetic resonance images of the substantia nigra in Parkinson disease. Ann Neurol 71(2):267–277. doi:10.1002/ana.22592
Lotfipour AK, Wharton S, Schwarz ST, Gontu V, Schafer A, Peters AM, Bowtell RW, Auer DP, Gowland PA, Bajaj NP (2012) High resolution magnetic susceptibility mapping of the substantia nigra in Parkinson’s disease. Journal of Magnetic Resonance Imaging: JMRI 35(1):48–55. doi:10.1002/jmri.22752
Cosottini M, Frosini D, Pesaresi I, Donatelli G, Cecchi P, Costagli M, Biagi L, Ceravolo R, Bonuccelli U, Tosetti M (2015) Comparison of 3T and 7T susceptibility-weighted angiography of the substantia nigra in diagnosing Parkinson disease. AJNR Am J Neuroradiol 36(3):461–466. doi:10.3174/ajnr.A4158
Mueller C, Pinter B, Reiter E, Schocke M, Scherfler C, Poewe W, Seppi K, Blazejewska AI, Schwarz ST, Bajaj N, Auer DP, Gowland PA (2014) Visualization of nigrosome 1 and its loss in PD: pathoanatomical correlation and in vivo 7T MRI. Neurology 82(19):1752. doi:10.1212/WNL.0000000000000398
Noh Y, Sung YH, Lee J, Kim EY (2015) Nigrosome 1 detection at 3T MRI for the diagnosis of early-stage idiopathic Parkinson disease: assessment of diagnostic accuracy and agreement on imaging asymmetry and clinical laterality. AJNR Am J Neuroradiol 36(11):2010–2016. doi:10.3174/ajnr.A4412
Schwarz ST, Afzal M, Morgan PS, Bajaj N, Gowland PA, Auer DP (2014) The ‘swallow tail’ appearance of the healthy nigrosome—a new accurate test of Parkinson’s disease: a case-control and retrospective cross-sectional MRI study at 3T. PLoS One 9(4):e93814. doi:10.1371/journal.pone.0093814
Haller S, Fallmar D, Larsson EM (2015) Susceptibility weighted imaging in dementia with Lewy bodies: will it resolve the blind spot of MRI? Neuroradiology. doi:10.1007/s00234-015-1605-6
Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, Ritchie K, Rossor M, Thal L, Winblad B (2001) Current concepts in mild cognitive impairment. Arch Neurol 58(12):1985–1992
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology 34(7):939–944
Tossici-Bolt L, Hoffmann SM, Kemp PM, Mehta RL, Fleming JS (2006) Quantification of [123I]FP-CIT SPECT brain images: an accurate technique for measurement of the specific binding ratio. Eur J Nucl Med Mol Imaging 33(12):1491–1499. doi:10.1007/s00259-006-0155-x
Badiavas K, Molyvda E, Iakovou I, Tsolaki M, Psarrakos K, Karatzas N (2011) SPECT imaging evaluation in movement disorders: far beyond visual assessment. Eur J Nucl Med Mol Imaging 38(4):764–773. doi:10.1007/s00259-010-1664-1
Wang Y, Butros SR, Shuai X, Dai Y, Chen C, Liu M, Haacke EM, Hu J, Xu H (2012) Different iron-deposition patterns of multiple system atrophy with predominant parkinsonism and idiopathetic Parkinson diseases demonstrated by phase-corrected susceptibility-weighted imaging. AJNR Am J Neuroradiol 33(2):266–273. doi:10.3174/ajnr.A2765
Haller S, Badoud S, Nguyen D, Barnaure I, Montandon ML, Lovblad KO, Burkhard PR (2013) Differentiation between Parkinson disease and other forms of parkinsonism using support vector machine analysis of susceptibility-weighted imaging (SWI): initial results. Eur Radiol 23(1):12–19. doi:10.1007/s00330-012-2579-y
Walker Z, Jaros E, Walker RW, Lee L, Costa DC, Livingston G, Ince PG, Perry R, McKeith I, Katona CL (2007) Dementia with Lewy bodies: a comparison of clinical diagnosis, FP-CIT single photon emission computed tomography imaging and autopsy. J Neurol Neurosurg Psychiatry 78(11):1176–1181. doi:10.1136/jnnp.2006.110122
McKeith I, O'Brien J, Walker Z, Tatsch K, Booij J, Darcourt J, Padovani A, Giubbini R, Bonuccelli U, Volterrani D, Holmes C, Kemp P, Tabet N, Meyer I, Reininger C, Group DLBS (2007) Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with Lewy bodies: a phase III, multicentre study. The Lancet Neurology 6(4):305–313. doi:10.1016/S1474-4422(07)70057-1
Antonini A (2007) The role of I-ioflupane SPECT dopamine transporter imaging in the diagnosis and treatment of patients with dementia with Lewy bodies. Neuropsychiatr Dis Treat 3(3):287–292
Roselli F, Pisciotta NM, Perneczky R, Pennelli M, Aniello MS, De Caro MF, Ferrannini E, Tartaglione B, Defazio G, Rubini G, Livrea P (2009) Severity of neuropsychiatric symptoms and dopamine transporter levels in dementia with Lewy bodies: a 123I-FP-CIT SPECT study. Movement Disorders: Official Journal of the Movement Disorder Society 24(14):2097–2103. doi:10.1002/mds.22702
Siepel FJ, Dalen I, Gruner R, Booij J, Bronnick KS, Buter TC, Aarsland D (2016) Loss of dopamine transporter binding and clinical symptoms in dementia with Lewy bodies. Movement Disorders: Official Journal of the Movement Disorder Society 31(1):118–125. doi:10.1002/mds.26327
Weintraub D, Newberg AB, Cary MS, Siderowf AD, Moberg PJ, Kleiner-Fisman G, Duda JE, Stern MB, Mozley D, Katz IR (2005) Striatal dopamine transporter imaging correlates with anxiety and depression symptoms in Parkinson’s disease. J Nucl Med 46(2):227–232
Ziebell M, Andersen BB, Pinborg LH, Knudsen GM, Stokholm J, Thomsen G, Karlsborg M, Hogh P, Mork ML, Hasselbalch SG (2013) Striatal dopamine transporter binding does not correlate with clinical severity in dementia with Lewy bodies. J Nucl Med 54(7):1072–1076. doi:10.2967/jnumed.112.114025
Piggott MA, Marshall EF, Thomas N, Lloyd S, Court JA, Jaros E, Burn D, Johnson M, Perry RH, McKeith IG, Ballard C, Perry EK (1999) Striatal dopaminergic markers in dementia with Lewy bodies, Alzheimer’s and Parkinson’s diseases: rostrocaudal distribution. Brain 122(Pt 8):1449–1468
Perry RH, Irving D, Blessed G, Perry EK, Smith CJ, Fairbairn AF (1990) Dementia in old age: identification of a clinically and pathologically distinct disease category. Adv Neurol 51:41–46
Zecca L, Casella L, Albertini A, Bellei C, Zucca FA, Engelen M, Zadlo A, Szewczyk G, Zareba M, Sarna T (2008) Neuromelanin can protect against iron-mediated oxidative damage in system modeling iron overload of brain aging and Parkinson's disease. J Neurochem 106(4):1866–1875. doi:10.1111/j.1471-4159.2008.05541.x
Gomez-Tortosa E, Newell K, Irizarry MC, Albert M, Growdon JH, Hyman BT (1999) Clinical and quantitative pathologic correlates of dementia with Lewy bodies. Neurology 53(6):1284–1291
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D, Jansen EN, Ballard C, de Vos RA, Wilcock GK, Jellinger KA, Perry RH (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 47(5):1113–1124
Yamamoto R, Iseki E, Marui W, Togo T, Katsuse O, Kato M, Isojima D, Akatsu H, Kosaka K, Arai H (2005) Non-uniformity in the regional pattern of Lewy pathology in brains of dementia with Lewy bodies. Neuropathology 25(3):188–194
Lindboe CF, Hansen HB (1998) The frequency of Lewy bodies in a consecutive autopsy series. Clin Neuropathol 17(4):204–209
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human studies have been approved by the ethics committee of Toho University and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that due to the retrospective nature of the observational study design, informed consent was waived.
Conflict of interest
We declare that we have no conflict of interest.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00234-017-1814-2.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Kamagata, K., Nakatsuka, T., Sakakibara, R. et al. Diagnostic imaging of dementia with Lewy bodies by susceptibility-weighted imaging of nigrosomes versus striatal dopamine transporter single-photon emission computed tomography: a retrospective observational study. Neuroradiology 59, 89–98 (2017). https://doi.org/10.1007/s00234-016-1773-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1773-z