Abstract
Introduction
Treatment with the humanized anti-vascular endothelial growth factor (VEGF) antibody bevacizumab in glioblastoma patients suppresses contrast enhancement via the reduction of vascular permeability, which does not necessarily indicate real reduction of tumor cell mass. Therefore, other imaging criteria are needed to recognize tumor growth under bevacizumab more reliably. It is still unknown, whether quantitative T1 mapping is useful to monitor the effects of anti-angiogenic therapy or to indicate a tumor progression earlier and more reliable compared to conventional magnetic resonance imaging (MRI) sequences. This raised the question whether quantitative T1 mapping is more suitable to monitor treatment effects of bevacizumab.
Methods
Conventional and quantitative MRI was performed on six consecutive patients with recurrent glioblastoma before treatment with bevacizumab and every 8 weeks thereafter until further tumor progression. Quantitative T1 maps before and after intravenous application of contrast agent and quantitative T2 maps were performed to calculate serial differential maps and subtraction maps from one time point, subtracting contrast-enhanced T1 maps from non-contrast T1 maps.
Results
In five illustrative cases, tumor progression was documented earlier in differential T1 relaxation time (DiffT1) and T2 relaxation time (DiffT2) maps before changes in the conventional MRI studies were obvious. Four patients showed previous prolongation of T1 relaxation time in the DiffT1 maps, suggesting tumor progression, and subtraction maps revealed faint contrast enhancement matching with the areas of T1 prolongation.
Conclusion
Our results emphasize that quantitative relaxation time mapping could be a promising method for tumor monitoring in glioblastoma patients under anti-angiogenic therapy. Quantitative T1 mapping seems to detect enhancing tumor earlier than conventional contrast-enhanced T1-weighted images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The management of patients with glioblastomas is still challenging because of the limited value of imaging features for tumor progression, for treatment failure, or treatment-related changes [1–3]. The prognosis of patients with recurrent glioblastoma remains poor with a median survival time of 3–6 months [2, 4]. Strong neoangiogenesis mediated by the vascular endothelial growth factor (VEGF) is a hallmark of highly vascularized glioblastomas, and consequently, anti-angiogenic treatment with bevacizumab, a humanized monoclonal immunoglobulin G antibody against VEGF [5, 6], has become a therapeutic option in patients with recurrent glioblastoma [5, 7, 8].
Under therapy with bevacizumab, glioblastomas show an impressive decrease of contrast enhancement and of vasogenic edema in magnetic resonance imaging (MRI) via the reduction of vascular permeability [5, 9, 10]. Since diagnosis of tumor progression was based on the presence of contrast enhancement in MRI [11, 12], response rates and progression-free survival were much higher compared to historical cohorts [6]. However, decreased contrast enhancement does not necessarily correspond to antitumor activity. The disappearance of contrast enhancement can also indicate a “pseudoresponse” caused by the antiangiogenesis under bevacizumab therapy without reducing tumor cell mass [13, 14]. Apart from ambiguous contrast enhancement, infiltration of glioma cells can be seen on T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences irrespective of tumor vasculature. Consequently, updated response criteria for high-grade gliomas formulated by the Response Assessment in Neuro-Oncology (RANO) working group [15] now also account for significant changes on T2-weighted or FLAIR sequences. However, the detection of non-enhancing tumor and its differentiation from edema on T2-weighted/FLAIR images is still a challenge [16]. In addition, physical MR properties of the tumor tissue also change under this treatment [17, 18] but T2 relaxation times remain always higher in the tumor tissue compared to the normal brain, even under bevacizumab [17]. Mapping of relaxation times also allow for subtracting quantitative values voxelwise from serial relaxation time maps. These “differential maps” help to detect new tumor infiltration and progression in patients under anti-angiogenic therapy [17].
T1 relaxation times are the other most important physical value of MRI. Previous studies revealed that both T1 and T2 relaxation times are increased in brain tumors [19–21]. However, it is still unknown, whether quantitative T1 mapping is useful to monitor the effects of anti-angiogenic therapy or to indicate a tumor progression. In contrast to the immanent T1 relaxation time of the tumor, T1 shortening upon accumulation of gadolinium (Gd)-containing agents is widely exploited for tumor imaging. Subtraction of T1 maps before and after application of a Gd-containing contrast agent may improve detection of blood-brain barrier damage and may have prognostic implications for brain tumor patients [22].
This raised the question whether quantitative T1 mapping is more suitable to monitor treatment effects of bevacizumab in patients with recurrent glioblastoma compared to conventional MRI sequences. In this study, we monitored recurrent glioblastoma patients under bevacizumab with conventional and quantitative MRI to evaluate if quantitative T1 and T2 mapping reveals tumor progression earlier and more reliable compared to conventional MRI sequences. Quantitative T1 maps were performed before and after intravenous application of contrast agent to perform
-
(1)
“differential maps” from serial T1 mapping (Fig. 1, upper row) and
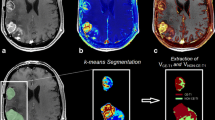
Fig. 1 Diff maps and subtraction maps. In the Diff maps (upper row), voxelwise subtraction of the T1 relaxation time (according to the formula (T1 without CA of time-point x − T1 without CA of time-point 1) / T1 without CA of time-point 1) is performed from two different time points. Time-point 1 indicates the first time point after starting bevacizumab therapy, this time point indicates the baseline for further monitoring. In the subtraction maps (lower row), voxelwise subtraction of the T1 relaxation time is performed from one time point but with and without contrast agent (according to the formula (T1 without CA − T1 with CA) / T1 without CA). The relative shortening of T1 after application of contrast agent quantifies the “contrast enhancement”
-
(2)
“subtraction maps” from one time point, subtracting contrast-enhanced T1 maps from non-contrast T1 maps (Fig. 1, lower row).
Materials and methods
Study design
The study was approved by the local Ethics Committee at the University Hospital Frankfurt [Reference number 4/09-SIN 01/09]. Patients with the histological diagnosis of glioblastoma were enrolled in this prospective non-interventional study. Tumor progression after first-line treatment was radiologically confirmed according to the RANO criteria in all patients, and anti-angiogenic therapy with bevacizumab was started as second- or third-line therapy. Bevacizumab was administered intravenously with a weight-adapted (10 mg/kg body weight) scheme every other week. Written informed consent was obtained from all patients prior to inclusion.
Patients’ characteristics and clinical data are summarized in Table 1.
MRI study protocol
Patients underwent MR examination before treatment and every 8 weeks during therapy until termination of bevacizumab therapy due to radiological or clinical progression or death.
MRI of the brain was performed on a 3T whole body system (MAGNETOM Trio, Siemens Medical AG) with an 8-channel phased array head coil. The MRI protocol included techniques for mapping quantitatively T1 and T2 relaxation times, 3D T1-w FLASH sequences before and after intravenous application of the contrast agent.
T1 mapping was based on a 3D gradient echo (GE) sequence with a fast low-angle shot-echo planar imaging (FLASH-EPI) hybrid readout [23] and fat-insensitive excitation pulses [24]. Acquisition parameters were TR/TE = 16.4 ms/6.7 ms, matrix size 256 × 224 × 160, spatial resolution 1 × 1 × 1 mm3, and BW = 222 Hz/pixel. The acquisition was performed twice, using different excitation angles (α) of 4° and 24°, thus allowing to obtain quantitative T1 values according to the variable flip angle method [25]. The acquisition time was 9:48 minutes. Furthermore, the sensitivity profile B1 of the transmit coil was measured, using the method described in Volz et al. with a duration of 53 s [26]. T1 values were corrected for B1 inhomogeneities and for effects of insufficient spoiling of the transverse magnetization [23, 26], yielding quantitative maps of the longitudinal relaxation time T1, given in milliseconds. (Fig. 1)
T2 mapping was based on the acquisition of five T2-weighted 2D turbo spin echo data sets with different TE. Acquisition parameters were TR = 10 s, TE = 17, 86, 103, 120, and 188 ms, matrix size 256 × 176, 50 adjacent axial slices with a thickness of 2 mm, spatial resolution 1 × 1 × 2 mm3, BW = 100 Hz/pixel. The acquisition time was 2:52 minutes per data set. Data were analyzed via pixel-wise exponential fitting, yielding quantitative maps of the transverse relaxation time T2, given in milliseconds.
The 3D GE sequences were acquired before and after application of standardized intravenous contrast agent injection (0.1 mmol/kg gadobutrol).
MR examinations
The following time points were considered for further data analysis:
-
t(0)
before the start of treatment
-
t(1)
first control 8 weeks after the start of treatment
-
t(n-1)
8 weeks before progression
-
t(n)
progression
Follow-up scans were performed until tumor progression and anti-angiogenic therapy had to be stopped.
Table 2 shows the follow-up MR examination for each patient.
Processing of MRI data
The generation of quantitative T1 and T2 maps was performed as described above with custom-built programs written in MATLAB [17, 27].
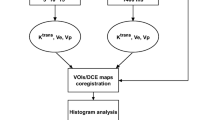
Differential maps
Differential T1 relaxation time maps (DiffT1) and T2 relaxation time maps (DiffT2) were generated according to the method of Ellingson et al. 2012 [28]. These maps are generated by registering the T1 or T2 maps of two time points followed by a voxelwise subtraction of the T1 or T2 relaxation times, respectively. Time-point one, the baseline, was the first MR scan after initiation of bevacizumab therapy in order to detect new tumor progression in the follow-up scans. Each map of a follow-up time point (n) was hence subtracted from the baseline (time-point one). We used linear registration with FLIRT (the FMRIB Linear Image Registration Tool of the Functional Magnetic Resonance Imaging of the Brain facility; Jenkinson, 2012) [29].
The changes of relaxation times on differential maps were color-coded, with yellow/red for an increase in relaxation times and green/blue for the shortening (Fig. 1, upper row).
Subtraction maps
The maps should indicate the shortening of T1 relaxation time upon the accumulation of contrast agent within the tumor tissue. The T1 relaxation time maps which were acquired before application of contrast agent were coregistered with the contrast-enhanced T1 relaxation time maps of the same MR examination and then a voxelwise subtraction according to the formula ((T1-pre-CA − T1-post-CA) / T1-post-CA) was performed (Fig. 1, lower row).
Visual assessment
Two neuroradiologists, one of them with more than 10 years’ experience in tumor imaging, independently evaluated the conventional MR images and maps from quantitative MR. Conventional T2-weighted and T1-weighted images were evaluated for enhancing and non-enhancing tumor progression. Both raters were blinded for the quantitative maps.
Afterwards, the color-coded differential maps of T1 relaxation time (DiffT1) were visually evaluated to identify changes in T1 relaxation times in the follow-up scans compared to the baseline maps. The detectable T1 changes were additionally compared with the subtraction maps from the respective time points.
In addition, T2 relaxation times (DiffT2) were evaluated in the same manner.
Statistics
This pilot study was designed as a proof of principle. Therefore, sample size was small, and no statistical evaluation was targeted. The study remains descriptive to show preliminary data which have to be confirmed in a larger multicenter patient cohort.
Results
Study subjects
Seventeen patients from our institutional tumor board data base were included during the observation period from January 2012 to January 2014. We excluded one patient who died before follow-up examination, four patients due to treatment-emergent adverse events, six patients due to severe movement artifacts. Therefore, this analysis includes six evaluable patients (2 female, 4 male) with a recurrent glioblastoma under bevacizumab treatment. The median age of the patients was 55 years (range, 45–65 years).
Differential T1 and T2 maps for detection of progressive disease
In five illustrative cases, tumor progression was documented earlier in DiffT1 and DiffT2 maps before changes in the conventional MRI studies were obvious. Progressive disease under therapy with bevacizumab was confirmed according to the RANO criteria [15]. Detailed information about the type of tumor progression according to the RANO criteria is given in Table 3. The clinical courses of the five cases are illustrated as figures and are only briefly described here in this section.
Quantitative T1 maps
Four patients showed previous prolongation of T1 relaxation time in the DiffT1 maps, suggesting tumor progression. In all four patients, subtraction maps revealed faint contrast enhancement matching with the areas of T1 prolongation. However, these brain areas appeared normal on conventional MRI. In the follow-up, the patients had a progression of enhancing tumor in conventional MRI in the regions with preceding prolongation of T1 relaxation time.
The Diff and subtraction maps as well as conventional contrast-enhanced T1-weighted sequences from the four patients are shown in Figs. 2 and 3, Quantitative T2 maps.
Same patient as shown in Fig. 1. After starting bevacizumab, patient no. 1 showed partial response of contrast-enhancing tumor in the left parietal lobe. At time-point 2, a new contrast-enhancing tumor occurred on the lateral margins of the previous enhancing tumor mass. The DiffT1 map (see also Fig. 1) showed prolongation of T1 relaxation times which even extended beyond the new contrast enhancement. Further, an area of increasing T1 relaxation time was seen in the frontoparietal white matter which appeared normal on conventional MRI at time-point 2. Note that the subtraction maps from time-point 2 also showed slight T1 shortening upon contrast enhancement (arrowhead). At time-point 3, these areas (arrows) clearly showed progression of enhancing tumor at both sides: at the lateral margins of the tumor and in the left frontoparietal white matter
Synopses of patient nos. 2, 3, and 4. Patient 2 had a contrast-enhancing tumor in the right temporal lobe which showed partial response at time-points 1 and 2. At time-point 3, contrast-enhancing areas slightly emerged on both sides of the lateral ventricles on conventional contrast-enhanced T1-weighted images. These enhancing areas were more obvious on the subtraction map (arrow tips). The non-contrast DiffT1 map from time-points 3 and 2 not only showed prolongation of T1 relaxation times in the same areas but also along the level of the corona radiata on the right side into the rostral part of the frontal lobe (arrows). In these areas, progression of enhancing tumor was seen 8 weeks later (time-point 4). Patient 3 had decreased contrast-enhancing tumor areas on the right parieto-occipital lobe on conventional MRI after starting bevacizumab. Faint enhancement was seen on conventional T1-weighted image at time-point 2, whereas DiffT1 and subtraction maps showed more extensive changes in the right occipital lobe and next to the trigonum toward the level of the right basal ganglia (arrows). Additionally, slight changes occurred on the left side of the lateral ventricle (arrow tip). Eight weeks later (time-point 3), these areas enhanced on conventional T1-weighted images, with a more curvilinear pattern in the occipitoparietal lobe (arrows) and with a nodular pattern in the ventricles (arrowhead). In contrast, the nodular enhancement of the right ventricle was not seen on preceding DiffT1 or on subtraction maps. Patient 4 showed a partial response with a decrease of contrast-enhancing tumor of the left occipitotemporal lobe after starting bevacizumab. On the conventional follow-up MR studies, the patient presented stable disease until time-point 9, which revealed progression of contrast-enhancing tumor mass on the left occipital lobe (arrows). Tumor progression was confirmed by positron-emission tomography (PET). This area was already conspicuous on preceding DiffT1 and subtraction map at time-point 6 (arrows) (Fig. 3)
One patient did not show a prolongation of T1 relaxation times in the DiffT1 maps. Interestingly, this patient had a long progression-free survival, and only in the sixth MR examination, a progression of non-enhancing tumor infiltration was depicted on T2-weighted images. Six months earlier, the Diff T2 maps revealed diffuse prolongation of the T2 relaxation times in the white matter of the left frontal lobe. The Diff maps in comparison to conventional T2-weighted images are shown in Fig. 4 for this patient.
Patient 5 with a recurrent GBM in the left frontal lobe showed good response after starting bevacizumab with a decrease of hyperintensities at the left frontal lobe at time-point 2 (arrows). The conventional MRI remained stable at time-points 3 and 4. At time-point 5, progressive hyperintensities extended toward the parietal deep white matter and across the genu of corporis callosi to the contralateral frontal lobe (arrows). These areas were already conspicuous at time-point 2 with a prolongation of the T2 relaxation time on the DiffT2 map (arrows)
Dropout of one patient due to failure of the anti-angiogenic effects of bevacizumab
One patient had only one follow-up MR examination due to early progression. In this patient, longer T1 relaxation times corresponded to an increase in contrast-enhancing tumor, and areas of longer T2 relaxation times corresponded to an increase in infiltrative disease with accompanying vasogenic edema and hyperintensities on conventional T2-weighted MRI images. This case is not demonstrated due to therapy failure in the first MRI control.
Discussion
This preliminary study suggests that quantitative mapping of relaxation times is more sensitive to detect progression of recurrent glioblastomas under bevacizumab compared to the conventional MR sequences. Prolongation of T1 relaxation times preceded progression of enhancing tumor or in one patient, it appeared simultaneously with early progression of enhancing tumor. The subtraction of enhanced T1 relaxation time maps from respective pre-contrast maps implicated that the T1 increase resulted from subtle blood-brain barrier (BBB) damage which was still invisible on conventional MRI.
This hypothesis is supported by the one case without prolongation of T1 relaxation times before tumor progression. This case presented as non-enhancing and more diffuse tumor progression. In this patient, only the T2 relaxation time increased before tumor progression was evident on conventional MRI.
The increase of relaxation times was detected by subtracting quantitative T1 or T2 values from two registered parameter maps of consecutive time points. Hereby, even subtle differences of relaxation times can be detected in these differential (Diff) maps. Considering that both relaxation times, T1 and T2, are prolonged in brain tumors, every increase of these relaxation times in the normal-appearing brain tissue should be estimated as tumor progression.
Recurrence or progression of contrast-enhancing tumor under bevazicumab indicates that this tumor should have tumor vasculature with a defective blood-brain barrier. The growth of this tumor type may be a result of a failure of the anti-angiogenic effects of bevacizumab. T1 relaxation times are mainly influenced by the content of interstitial tissue water [30–33]. It could be shown previously that damage of BBB in lesions of MS patients reveal significantly higher T1 relaxation times compared to lesions with intact BBB [30]. In accordance with this observation, increased T1 relaxation times fitted well with subtle contrast enhancement on the subtraction maps (pre-to-post enhanced T1 maps). In contrast to the quantitative subtraction maps, this initially subtle enhancement was only later visible on conventional MRI. The sensitive detection of new contrast enhancement should be of particular importance under bevacizumab because its anti-VEGF effect reduces the BBB damage [34]. Ellingson et al. already reported the value of contrast-enhanced T1-weighted subtraction maps which not only improved visualization but also allowed for better prediction of survival in patient with recurrent GBM treated with bevacizumab [22].
In contrast to our study, Ellingson et al. subtracted conventional T1-weighted images which had to be corrected for coil and magnetic field biases. The quantitative T1 relaxation time mapping has the advantage that all these corrections as well as other influences on the signal intensities (e.g., T2 relaxation time, proton density) are already corrected. Therefore, quantitative T1 mapping seems to be the method of choice especially for tumor monitoring in a multicenter study design.
However, a standardized protocol for quantitative T1 mapping is still missing. There are two different approaches available to acquire quantitative T1 maps: (a) T1 maps based on the acquisition of spoiled fast low-angle shot (FLASH) datasets using variable excitation angles and (b) T1 mapping using spoiled FLASH echo planar imaging (EPI) hybrid sequences with varying flip angles [30, 35, 36]. The development of quantitative T1 measurements with high spatial resolution and short experiment durations is of major interest. T1 mapping on the basis of the variable flip angle approach yields reproducible results which deem its use in clinical studies appropriate [30]. This opinion is also supported by a recent study by Deoni et al. which reports reliable and robust results in a multicenter study [35]. Further, the use of FLASH-EPI hybrid sequences with two echoes per excitation can be used to improve SNR in T1 maps based on the variable excitation angle approach [30]. Therefore, in our institute, T1 mapping using spoiled FLASH-EPI hybrid sequences with two variable flip angles is the method of choice.
Although a multifactorial etiology is likely to cause brain tissue damage in glioblastoma, the disruption of the BBB seems to play a pivotal role [22]. The leakage of the BBB can be detected via a signal enhancement in T1-weighted images following the administration of gadolinium-containing contrast agent (CA). To increase the signal on T1-weighted images, the CA molecules have to pass the BBB and accumulate in the brain interstitium. However, the visibility of enhancement depends strongly on various factors, such as imaging sequence parameters, magnetic field strength, CA dose, and manner of CA administration [37, 38]. Further, enhancement depends on the relation between molecular size of CA (diameter of about 0.9 nm) and the size of the leaks of the BBB. In contrast, water molecules are much smaller compared to the CA molecules. Therefore, the content of interstitial water and thus the T1 relaxation times should increase before enhancement is seen.
Hattingen et al. assumed in their study that an increase in T2 relaxation times in the normal-appearing brain also detects tumor progression with high sensitivity irrespective of the BBB integrity. Increased tissue water and blood volume as well as loss of brain tissue texture from gliosis or tumor infiltration are known to increase T2 relaxation time [17, 39]. Animal models showed lowest T2 relaxation times in a normal brain, intermediate values in tumor tissue, and longest T2 relaxation times in edema [40, 41]. In our cohort, only one of five patients demonstrated non-enhancing progressive tumor under bevacizumab, whereas more patients with non-enhancing or less enhancing tumor progression were included in the larger collective in the study of Hattingen et al. [17]. But, our patients and the previous study suggest that an increase of T2 relaxation time in DiffT2 maps may detect non-enhancing tumor progression more sensitively compared to DiffT1 maps. Another advantage of measuring quantitative relaxation times instead of signal intensities is explained by their inverse effect on the signal in conventional MRI: both values are prolonged in glioblastomas. Prolongation of T1 relaxation time lowers the signal on conventional MRI whereas prolonged T2 relaxation time increases the signal. Although the signal in T2-weighted images is mainly influenced by the T2 relaxation times, T1 relaxation time also has some influence on the signal especially on FLAIR images, for which T1 effects are even more pronounced. Consequently, changes in T1 and T2 relaxation times may yield opposite effects on tumor-related signal changes in conventional MRI so that measuring each parameter separately should improve tumor detectability.
Therefore, changes in T2 relaxation time seem to be a sensitive but relatively nonspecific marker of tissue pathology [17, 31].
Our results emphasize that quantitative relaxation time mapping could be a promising method for tumor monitoring. This especially holds true for glioblastoma patients under anti-angiogenic therapy since detection of tumor progression seems to be more difficult under this treatment [16]. From the clinical point of view, it would be crucial to reliably define the exact time point of progression especially for anti-angiogenic therapies. To date, this is impaired by the huge influence of bevacizumab not only on contrast enhancement but also on T2 sequences [17]. Quantitative MRI and calculated differential or substraction maps could solve this problem. These techniques might allow detection of tumor progression earlier compared to conventional MRI and are able to offer observer-independent parameters (e.g., increase of T1 relaxation time on differential maps) to provide objective parameters of tumor progression. At our brain tumor center and for patients outside clinical trials, we use bevacizumab usually as a last-line regimen when other approved drugs have failed. In these patients, it might be less important to exactly define the time point of progression. Due to missing therapeutic options, we would not stop bevacizumab in a patient without clinical deterioration but subtle signs of progression on MRI anyhow. But, quantitative MRI would be especially relevant for clinical studies to unequivocally define the time point of progression. Among other reasons, bevacizumab did not get EMEA approval due to the uncertainties regarding the definition of PFS.
However, our observations in only five cases should be considered as preliminary results. Larger cohorts are needed to value our hypotheses. Our study number was limited because bevazicumab has not been approved for the first-line therapy in primary glioblastomas. Therefore, we investigated patients with recurrent glioblastomas receiving bevacizumab according to individual treatment decisions. Most of these patients with advanced disease have early relapses or are in clinically poor conditions and unable to perform long MR examination. Therefore, multicenter studies are needed to approve the validity of quantitative differential maps to monitor glioblastoma patients under treatment.
Furthermore, correlation between signal changes detected by quantitative MRI and histopathological findings is missing. Therefore, we compared the results of the quantitative DiffT1 and DiffT2 maps with conventional MR sequences.
Conclusion
Quantitative T1 and T2 mapping are objective methods which have an impact on monitoring glioblastomas especially under bevacizumab therapy. Changes of relaxation times are easily detected on color-coded subtraction maps, indicating even minor tissue changes predicting tumor progression which might be missed on conventional MRI.
Quantitative T1 mapping seems to detect enhancing tumor earlier than conventional contrast-enhanced T1-weighted images. Prolongation of T1 relaxation times represents BBB damage in an earlier stage before contrast agent can accumulate in the brain interstitium.
The interpretation of changes of T2 relaxation times is more challenging because they may be also influenced by different therapy effects. However, non-enhancing tumor infiltration might be also detected more sensitively compared to conventional T2-weighted images.
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Wong ET, Hess KR, Gleason MJ et al (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17:2572–2578
Saitta L, Heese O, Förster AF et al (2011) Signal intensity in T2′ magnetic resonance imaging is related to brain glioma grade. Eur Radiol 21(5):1068–1076
Wick W, Puduvalli VK, Chamberlain MC et al (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28(7):1168–1174
Vredenburgh JJ, Desjardins A, Herndon JE et al (2007) Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol 25(30):4722–4729
Friedman HS, Prados MD, Wen PY et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740
Stark-Vance V (2005) Bevacizumab and CPT-11 in the treatment of relapsed malignant glioma [abstract]. Proceedings of the World Federation of Neuro-Oncology Meeting. Neuro-Oncol 7:369
Wagner SA, Desjardins A, Reardon DA et al (2008) Update on survival from the original phase II trial of bevacizumab and irinotecan in recurrent malignant gliomas [abstract]. J Clin Oncol 26:2021
Claes A, Gambarota G, Hamans B et al (2008) Magnetic resonance imaging-based detection of glial brain tumors in mice after antiangiogenic treatment. Int J Cancer 22:1981–1986
Norden AD, Young GS, Setayesh K et al (2008) Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology 70:779–787
Macdonald D, Cascino T, Schold SJ et al (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280
Casanovas O, Hicklin DJ, Bergers G et al (2005) Drug resistance by evasion of antiangiogenic targeting of VEGF signaling in late-stage pancreatic islet tumors. Cancer Cell 8(4):299–309
da Cruz LC H Jr, Rodriguez I, Domingues RC et al (2011) Pseudoprogression and pseudoresponse: imaging challenges in the assessment of posttreatment glioma. Am J Neuroradiol 32(11):1978–1985
Brandsma D, van den Bent MJ (2009) Pseudoprogression and pseudoresponse in the treatment of gliomas. Curr Opin Neurol 22(6):633–638, Review
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972
Pope WB, Hessel C (2011) Response assessment in neuro-oncology criteria: implementation challenges in multicenter neuro-oncology trials. AJNR Am J Neuroradiol 32(5):794–797
Hattingen E, Jurcoane A, Daneshvar K et al (2013) Quantitative T2 mapping of recurrent glioblastoma under bevacizumab improves monitoring for non-enhancing tumor progression and predicts overall survival. Neurooncol 15(10):1395–404
Rieger J, Bähr O, Muller K et al (2010) Bevacizumab-induced diffusion-restricted lesions in malignant glioma patients. Neurooncol 99(1):49–56
Araki T, Inouye T, Suzuki H et al (1984) Magnetic resonance imaging of brain tumors: measurement of T1. Work in progress. Radiol 150(1):95–98
Englund E, Brun A, Larsson EM et al (1986) Tumours of the central nervous system. Proton magnetic resonance relaxation times T1 and T2 and histopathologic correlates. Acta Radiol Diagn 27:653–659
Le Bas JF, Leviel JL, Decorps M et al (1984) NMR relaxation times from serial stereotactic biopsies in human brain tumors. J Comput Assist Tomogr 8:1048–1057
Ellingson BM, Kim HJ, Woodworth DC et al (2014) Recurrent glioblastoma treated with bevacizumab: contrast-enhanced T1-weighted subtraction maps improve tumor delineation and aid prediction of survival in a multicenter clinical trial. Radiology 271(1):200–210
Preibisch C, Deichmann R (2009) T-1 mapping using spoiled FLASH-EPI hybrid sequences and varying flip angles. Magn Reson Imaging 62:240–246
Howarth C, Hutton C, Deichmann R (2006) Improvement of the image quality of T1-weighted anatomical brain scans. Neuroimaging 29:930–937
Venkatesan R, Lin WL, Haacke EM (1998) Accurate determination of spin-density and T-1 in the presence of RF-field inhomogeneities and flip-angle miscalibration. Magn Reson Med 40:592–602
Volz S, Noth U, Rotarska-Jagiela A et al (2010) A fast B1-mapping method for the correction and normalization of magnetization transfer ratio maps at 3T. Neuroimaging 49:3015–3026
Hattingen E, Jurcoane A, Bähr O et al (2011) Bevacizumab impairs oxidative energy metabolism and shows antitumoral effects in recurrent glioblastomas: a 31P/1H MRSI and quantitative magnetic resonance imaging study. Neurooncol 13(12):1349–1363
Ellingson BM, Cloughesy TF, Lai A et al (2012) Quantification of edema reduction using differential quantitative T2 (DQT2) relaxometry mapping in recurrent glioblastoma treated with bevacizumab. J Neurooncol 106(1):111–119
Jenkinson M, Beckmann CF, Behrens TE et al (2012) FSL Neuroimaging 62(2):782–790
Jurcoane A, Wagner M, Schmidt C et al (2013) Within-lesion differences in quantitative MRI parameters predict contrast enhancement in multiple sclerosis. J Magn Reson Imaging 38(6):1454–1561
Mottershead JP, Schmierer K, Clemence M et al (2003) High field MRI correlates of myelin content and axonal density in multiple sclerosis—a post-mortem study of the spinal cord. J Neurol 250:1293–1301
Seewann A, Vrenken H, van der Valk P et al (2009) Diffusely abnormal white matter in chronic multiple sclerosis: imaging and histopathologic analysis. Arch Neurol 66:601–609
van Waesberghe JH, Kamphorst W, De Groot CJ et al (1999) Axonal loss in multiple sclerosis lesions: magnetic resonance imaging insights into substrates of disability. Ann Neurol 46:747–754
Chiba Y, Sasayama T, Miyake S et al (2008) Anti-VEGF receptor antagonist (VGA1155) reduces infarction in rat permanent focal brain ischemia. Kobe J Med Sci 54(2):136–146
Deoni SC, Peters TM, Rutt BK (2004) Determination of optimal angles for variable nutation proton magnetic spin-lattice, T1, and spin-spin, T2, relaxation times measurement. Magn Reson Med 51:194–199
Deichmann R (2006) Fast structural brain imaging using an MDEFT sequence with a FLASH-EPI hybrid readout. Neuroimaging 33:1066–1071
Katz D, Taubenberger JK, Cannella B et al (1993) Correlation between magnetic resonance imaging findings and lesion development in chronic, active multiple sclerosis. Ann Neurol 34:661–669
Brück W, Bitsch A, Kolenda H et al (1997) Inflammatory central nervous system demyelination: correlation of magnetic resonance imaging findings with lesion pathology. Ann Neurol 42:783–793
Oh J, Cha S, Aiken AH et al (2005) Quantitative apparent diffusion coefficients and T2 relaxation times in characterizing contrast enhancing brain tumors and regions of peritumoral edema. J Magn Reson Imaging 21(6):701–708
Hoehn-Berlage M, Tolxdorff T, Bockhorst K et al (1992) In vivo NMRT2 relaxation of experimental brain tumors in the cat: a multiparameter tissue characterization. Magn Reson Imaging 10(6):935–947
Eis M, Els T, Hoehn-Berlage M (1995) High resolution quantitative relaxation and diffusion MRI of three different experimental brain tumors in rat. Magn Reson Med 34(6):835–844
Acknowledgments
We thank Stefanie Pellikan and Maurice Harth of the Institute of Neuroradiology and the staff and nurses of the Dr. Senckenberg Institute of Neurooncology who supported this study. Excellent technical assistance was provided by Professor Ralf Deichmann and his staff from the Brain Imaging Center Frankfurt. The Dr. Senckenberg Institute of Neurooncology is supported by the Dr. Senckenberg Foundation and the Hertie Foundation.
Ethical standards and patient consent
We declare that all human and animal studies have been approved by the local Ethics Committee at the University Hospital Frankfurt [Reference number 4/09-SIN 01/09] and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
OB has served as a consultant for Roche, the European distributer of bevacizumab and has received travel grants from Roche.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(GIF 417kb)
Rights and permissions
About this article
Cite this article
Lescher, S., Jurcoane, A., Veit, A. et al. Quantitative T1 and T2 mapping in recurrent glioblastomas under bevacizumab: earlier detection of tumor progression compared to conventional MRI. Neuroradiology 57, 11–20 (2015). https://doi.org/10.1007/s00234-014-1445-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1445-9