Abstract
Introduction
Our study aimed to elucidate the diagnostic performance of dual-energy CT (DECT) in the detection of contrast enhancement in intracranial haematomas (ICrH) with early phase dual-energy computed tomography angiography (CTA) and compare the results with those obtained by delayed CT enhancement.
Methods
Thirty-six patients with ICrH were retrospectively included in this study. All patients had undergone single-energy non-contrast CT and contrast-enhanced dual-source DECT. DECT images were post-processed with commercial software, followed by obtaining iodine images and virtual non-contrast images and generating combined images that created the impression of 120-kVp images. Two neuroradiologists, blinded to the patients’ data, reviewed two reading sessions: session A (non-contrast CT and combined CT) and session B (non-contrast CT, combined CT, and iodine images) for detection of contrast enhancement in the haematomas.
Results
Contrast leakage or enhancement was detected in 23 (57.5 %) out of 40 haemorrhagic lesions in 36 patients on delayed CT. Three enhanced lesions were depicted only in the DECT iodine images. The sensitivity, specificity, positive predictive value, and negative predictive value of session A were 82.6, 94.1, 95.0, and 80.0 %, respectively, and those of session B were 95.7, 94.1, 95.7, and 94.1 %, respectively.
Conclusion
DECT emphasised the iodine enhancement and facilitated the detection of contrast enhancement or leakage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The presence of an active contrast extravasation into an intracerebral haematoma (ICeH) at the time of CT angiography has been associated with an increased risk of haematoma expansion and mortality in patients with idiopathic ICeH [1, 2].
Additionally, it has been reported that approximately 10 % of all spontaneous ICeH are due to haemorrhages from brain tumours. High attenuation of acute ICeH may mask the contrast enhancement, so it can be difficult to detect the enhancement for tumour identification. Dual-energy CT (DECT) can differentiate between a haematoma and iodine using the attenuation difference between two energies [3]. A recent study showed that DECT is useful in the detection of obscured tumours in patients with unknown-origin ICeH [4], and DECT is also able to differentiate between a haematoma and iodinated contrast leakage in patients after intra-arterial or intravenous contrast administration [5].
The purposes of this study were to elucidate the diagnostic performance of DECT in the detection of contrast enhancement or leakage in haematoma patients on early phase DE-computed tomography angiography (CTA) and to compare the results with those obtained by delayed CT enhancement (reference standard).
Methods and materials
Subjects
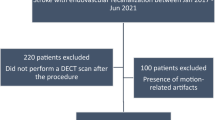
We retrospectively reviewed intracranial haemorrhage (ICrH) patients admitted in our emergency room between April 2010 and January 2012. During this period, there were 205 haemorrhagic patients (134 for traumatic, 71 for intrinsic haemorrhage), and CTA was performed on 75 patients (41 for traumatic, 34 for intrinsic cases) in the acute phase. Amongst 75 patients, dual-energy CT was performed on 56 patients. Thirty-six patients who had undergone single-energy plain CT, dual-energy CTA, and delayed phase CT were included and analysed in this study. Twenty patients with DECT were excluded due to lack of delayed phase CT or patient’s motion artefact which is difficult to evaluate. The patients included 24 men and 12 women, with a mean age of 60 years (range 16–84 years). The patients had the following diagnoses: idiopathic ICeH (16 patients), traumatic haemorrhage (16 patients), subarachnoid haemorrhage with ICeH (2 patients), and intra-tumour haemorrhage (2 patients).
This study was approved by the local institutional review board with a waiver for informed consent.
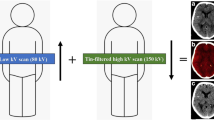
CT acquisition and dual-energy data processing
CT imaging was performed with a dual-source CT unit (Somatom Definition Flash, Siemens Healthcare). All patients had undergone non-contrast CT, dual-source dual-energy CTA (100 and 140 kVp), and delayed phase enhanced CT (2 min after contrast injection). The non-contrast CT was obtained in a single-energy mode with 120 kVp and reconstructed in 5-mm section thickness. The DECT was operated in a dual-energy mode, with tube A at 100 kVp and tube B at 140 kVp, with 360 and 80 effective mAs, respectively, as well as a 0.5-s rotation time, 128 × 0.6-mm collimation with z-flying focal spot, and a pitch of 0.6. The 100- and 140-kVp images were reconstructed separately in 0.6-mm section widths and 0.6-mm increments using a D26 kernel for a 180-mm field of view.
Contrast material (300 mg I/mL, 100 mL) was injected via the antecubital vein with an injection rate of 4.0 mL/s. The time between the injection and the CTA data acquisition was determined using a bolus-tracking software at the common carotid artery. The CTA was obtained from the aortic arch to the vertex in a caudocranial direction. A delayed phase CT of the brain was obtained 2 min after the contrast injection.
DECT images were post-processed with commercial software applying a three-material decomposition algorithm for ‘brain haemorrhage’ (materials included iodine, haematoma, and water) to calculate the iodine images and virtual non-contrast images. We also made a fusion image of a colour-coded iodine image and a grey-scale virtual non-contrast image, which was an easy method to represent the contrast enhancement in ICrH. The combined images comprised one half of both the 100- and 140-kVp information that resulted in images with characteristics comparable to those of the 120-kVp CT images.
Image interpretation
Two neuroradiologists, blinded to the patients’ data, independently reviewed the images in two different sessions. In the first session (session A), the non-contrast images and combined images were reviewed. Then, in the second session (session B), the readers reviewed the non-contrast images, the combined images, and the iodine image and virtual non-contrast images generated by the DECT data.
For each case, the presence of contrast enhancement or contrast leakage in ICrH was assessed. If the enhancement was detected in session B, each reviewer decided which was the preferred contrast between the combined images and iodine image or if there was an equal amount of contrast between the two images. In those cases with contrast enhancement, one reviewer selected the circular or eclipse region of interest (ROI, 6–10 mm2 in size) within the contrast-enhanced lesion in the haematoma using the combined images, set the ROI at the same position in the non-contrast CT, and measured the CT value. In each ROI, we compared the absolute CT value of contrast-enhanced CT and the difference between contrast-enhanced CT and non-contrast CT to show the CT value difference among the enhancement status. If a disagreement between the two readers existed, a final decision was made by consensus.
The contrast enhancement of the delayed CT was defined as the reference standard.
Statistical analysis
Statistical analysis was performed using SPSS software, version 17.0 (SPSS, Chicago, IL, USA). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were evaluated. The average CT value difference in the enhanced regions between the enhanced CT and non-contrast CT was compared using the unpaired t test. Kappa statistics were calculated for inter-rater agreement.
Results
Contrast enhancement was detected in 23 (57.5 %; 22 patients) of the 40 haemorrhagic lesions in 36 patients via delayed CT. One lesion showed enhancement on only the delayed CT, but 22 lesions revealed enhancement on both the early and delayed CT images. The sensitivity, specificity, PPV, and NPV are shown in Table 1.
Amongst the 22 contrast-enhanced lesions on early CTA, 3 lesions (later referred to as part of the DECT superior group; Fig. 1) were detected only in the iodine images with DECT; 4 lesions (later referred to as part of the DECT superior group; Fig. 2) had better enhancement on the iodine images, as compared to that of the combined images; and 15 lesions (later referred to as the equal group) had equal contrast enhancement on both image types. The average CT value difference in the enhanced regions is summarised in Table 2. Between the DECT superior group (n = 7) and the equal group (n = 15), the DECT superior group showed a significantly lower enhancement compared to that of the equal group.
A 61-year-old woman with traumatic subdural haematoma (SDH). a Non-contrast CT, b combined CT (120 kVp), c delayed CT, d virtual non-contrast (VNC) image, and e iodine image (fusion with VNC). Faint enhancement in the right SDH was depicted only by the iodine image (e, arrow), and it was difficult to detect by combined image (c)
A 67-year-old woman with a putaminal haemorrhage. a Non-contrast CT, b combined CT (120 kVp), c delayed CT, d virtual non-contrast (VNC) image, and e iodine image (fusion with VNC). The combined image (b) shows two CTA spot signs (arrowhead) in the haematoma. The delayed CT shows contrast extravasation at the medial side of the haematoma. The iodine image (e) shows the CTA spot signs and a faint contrast leakage, which is more clearly seen on the medial side (arrow)
Interobserver agreement between the two readers’ individual review results was excellent (κ = 0.90 for session A; κ = 0.94 for session B).
Discussion
Our results showed that DECT could differentiate iodine enhancement from a haematoma and increase the sensitivity of the contrast enhancement in ICrH. Out of the 22 contrast-enhanced lesions demonstrated via CTA, 3 (13.6 %) lesions were only detected in the iodine images with DECT, thus showing increased sensitivity. DECT was superior in helping to visualise the contrast enhancement of four lesions, as compared to that of the combined image (120-kVP equivalent image); however, 15 lesions (65 %) were easily detected in both the iodine images and combined images.
It is well known that the CT value of ICeH could not exceed 100 HU in 120 kVp [6]. In our case series, most of the patients had idiopathic ICeH (44 %) or a traumatic haemorrhage (44 %). In these patients, most of the enhancement in the haematomas comprised the CTA spot sign, which was considered either a microaneurysm or an extravasation from a ruptured microvessel. In these situations, contrast enhancement or leakage showed high CT values, which were easy to depict by a normal single-energy CT, as well as in the combined image generated by DECT.
Furthermore, the three lesions that were detected only in the iodine images with DECT were a cerebellopontine angle tumour, traumatic subdural haematoma, and a right temporal subcortical haemorrhage. In these cases, the enhancement was faint; however, with a combined CT, it was difficult to find the contrast enhancement. The average CT value difference in these regions was 13.0 HU, so DECT was useful in detecting the slightly enhanced lesions in the haematomas. Using DECT, the contrast enhancement or leakage was detected in 96 % of cases (22/23). Our results speculate the possibility to omit the delayed scan for the detection of contrast leakage and reduce the total radiation dose.
Recently, Flors et al. reported endoleak detection after an endovascular repair of a thoracic aortic aneurysm using a dual-source DECT [7]. Their results showed that virtual non-contrast and late delayed phase images reconstructed from a single DECT can replace a triple-phase enhanced CT, indicating that faint enhancement of the extra aorta by delayed CT can be easily detected with DECT.
It has been reported that using DECT with a brain haemorrhage is useful when utilising iodine in order to visualise a haematoma. After intra-arterial or intravenous contrast administration, DECT can help in the differentiation of iodine extravasation from the haemorrhage [5, 8]; moreover, these cases are increasing because of the widespread use of endovascular interventions in acute stroke. Kim et al. [4] reported that DECT is useful in the detection of underlying tumours and in the differentiation of pure haemorrhages in patients with unknown-origin ICeH. The sensitivity and specificity of detecting brain tumours were significantly increased by DECT. Now, with the ability to enhance tumours, it might be useful to detect this enhancement in a high-density haematoma by DECT. In our case series, two patients were diagnosed with tumour haemorrhage. No enhancement could be detected by both DECT and delayed phase CT in one patient, as diagnosed after operation. We need considerable attention to diagnose a haemorrhagic brain tumour because some tumour enhancement was faint and it was difficult to detect on DECT or usual single-energy CT.
The presence of a CTA spot sign [9–11] or post-contrast CT extravasation [2] into an ICeH has been associated with an increased risk of haematoma expansion and mortality in patients with ICeH. There are few reports on traumatic intracranial haemorrhages regarding the CTA spot sign or extravasation, as well as some case reports that showed active bleeding in traumatic haematomas [12]. Recently, two papers showed that contrast extravasation within ICeH or subdural haematomas predicted poor in-hospital outcomes in the setting of acute traumatic intracranial injuries [13, 14]. Therefore, given the importance of detecting contrast leakage in patients with traumatic ICrH, DECT can help in visualising the iodine in these cases.
There were several limitations in our study. First, we used delayed CT contrast extravasation as a reference standard for the early CTA spot signs or contrast enhancement. We decided to use the delayed CT contrast extravasation as the reference standard on the basis of previous case series which reported that delayed CT contrast extravasation was a more sensitive predictor of ICeH growth with a better NPV than that of the spot sign [15]. To establish the clinical value, additional study is necessary to compare haematoma growth, clinical outcome, and DECT findings.
Second, in our study, we selected patients with various types of ICrH, including spontaneous, traumatic, and tumour related. Great variability existed amongst the selected patients, but we believe this had little effect on demonstrating the technical advantage of DECT in the detection of iodine enhancement in a haematoma. Furthermore, while reading session B, we reviewed a non-contrast CT, a combined CT, and an iodine image produced by DECT. In a clinical situation, we would not interpret an iodine image alone and would always evaluate the enhancement of a non-contrast CT, a combined CT, and an iodine image. Hence, we think session B is more applicable to the usual clinical setting.
Conclusion
DECT was able to differentiate iodine contrast medium from a haematoma and facilitates the detection of contrast.
Abbreviations
- ICrH:
-
Intracranial haematoma
- ICeH:
-
Intracerebral haematoma
- DECT:
-
Dual-energy CT
- ROI:
-
Region of interest
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- HU:
-
Hounsfield units
References
Thompson AL, Kosior JC, Gladstone DJ et al (2009) Defining the CT angiography 'spot sign' in primary intracerebral hemorrhage. Can J Neurol Sci 36:456–461
Ederies A, Demchuk A, Chia T et al (2009) Postcontrast CT extravasation is associated with hematoma expansion in CTA spot negative patients. Stroke 40:1672–1676
Johnson TR, Krauss B, Sedlmair M et al (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517
Kim SJ, Lim HK, Lee HY et al (2012) Dual-energy CT in the evaluation of intracerebral hemorrhage of unknown origin: differentiation between tumor bleeding and pure hemorrhage. AJNR Am J Neuroradiol 33:865–872
Phan CM, Yoo AJ, Hirsch JA, Nogueira RG, Gupta R (2012) Differentiation of hemorrhage from iodinated contrast in different intracranial compartments using dual-energy head CT. AJNR Am J Neuroradiol 33:1088–1094
New PF, Aronow S (1976) Attenuation measurements of whole blood and blood fractions in computed tomography. Radiology 121:635–640
Flors L, Leiva-Salinas C, Norton PT, Patrie JT, Hagspiel KD (2013) Endoleak detection after endovascular repair of thoracic aortic aneurysm using dual-source dual-energy CT: suitable scanning protocols and potential radiation dose reduction. AJR Am J Roentgenol 200:451–460
Gupta R, Phan CM, Leidecker C et al (2010) Evaluation of dual-energy CT for differentiating intracerebral hemorrhage from iodinated contrast material staining. Radiology 257:205–211
Huynh TJ, Demchuk AM, Dowlatshahi D et al (2013) Spot sign number is the most important spot sign characteristic for predicting hematoma expansion using first-pass computed tomography angiography: analysis from the PREDICT study. Stroke 44:972–977
Demchuk AM, Dowlatshahi D, Rodriguez-Luna D et al (2012) Prediction of haematoma growth and outcome in patients with intracerebral haemorrhage using the CT-angiography spot sign (PREDICT): a prospective observational study. Lancet Neurol 11:307–314
Park SY, Kong MH, Kim JH, Kang DS, Song KY, Huh SK (2010) Role of 'spot sign' on CT angiography to predict hematoma expansion in spontaneous intracerebral hemorrhage. J Korean Neurosurg Soc 48:399–405
Dalfino JC, Boulos AS (2010) Visualization of an actively bleeding cortical vessel into the subdural space by CT angiography. Clin Neurol Neurosurg 112:737–739
Romero JM, Kelly HR, Delgado Almandoz JE et al (2013) Contrast extravasation on CT Angiography predicts hematoma expansion and mortality in acute traumatic subdural hemorrhage. AJNR Am J Neuroradiol 34:1528–1534
Letourneau-Guillon L, Huynh T, Jakobovic R, Milwid R, Symons SP, Aviv RI (2013) Traumatic intracranial hematomas: prognostic value of contrast extravasation. AJNR Am J Neuroradiol 34:773–779
Hallevi H, Abraham AT, Barreto AD, Grotta JC, Savitz SI (2010) The spot sign in intracerebral hemorrhage: the importance of looking for contrast extravasation. Cerebrovasc Dis 29:217–220
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watanabe, Y., Tsukabe, A., Kunitomi, Y. et al. Dual-energy CT for detection of contrast enhancement or leakage within high-density haematomas in patients with intracranial haemorrhage. Neuroradiology 56, 291–295 (2014). https://doi.org/10.1007/s00234-014-1333-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1333-3