Abstract
Introduction
Cerebral vasospasm (CV) is one of the most dreaded complications in patients who survive acute subarachnoid haemorrhage (SAH), and conventional cerebral angiography (DSA) is the gold standard for its diagnosis. We evaluated CT angiography (CTA) as a non-invasive alternative for diagnosis of CV and assessed if CTA could have a role in choosing appropriate treatment.
Methods
Consecutive patients with SAH and suspected vasospasm were included when DSA was performed within 24 h from CTA. Two neuro-radiologists retrospectively analysed CTA and DSA studies independently. Assessment included presence of central and peripheral vasospasm and grading of severity of central CV. A treatment recommendation based on CTA was compared to actual treatment received.
Results
Final analysis included 34 patients. CTA was more accurate for diagnosis of central then for peripheral CV with high sensitivity (reader 1, 91%; reader 2, 92%), specificity (reader 1, 73%; reader 2, 90%), accuracy, positive predictive value and negative predictive value for central vasospasm. For grading the severity of CV CTA’s sensitivity, specificity and accuracy were high for most central arteries. The reader’s recommendation of angioplasty according to CTA was significantly predictive of actual receipt of angioplasty but overestimated actual receipt of triple H treatment.
Conclusion
CTA is adequate for detecting central vasospasm in symptomatic SAH patients. A negative result should not prevent further investigation especially when evaluating arterial segments adjacent to metal artefacts from coils or clips. CTA is helpful in treatment decision making specifically regarding the need for balloon angioplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral vasospasm (CV) is one of the most dreaded complications in patients who survive acute subarachnoid haemorrhage (SAH). Its peak incidence is between days 4 and 10 after SAH. CV presents clinically with symptoms of brain ischaemia according to the affected arteries and the region of the brain they supply. Symptoms may include focal neurological deficits or altered level of consciousness. While mild vasospasm may be asymptomatic or present with subtle clinical findings, such as headaches, confusion or drowsiness, moderate and severe vasospasm are more likely to present with blood pressure dependent motor deficits or decreased level of consciousness [1]. CV may result in permanent cerebral ischaemia and is the major cause of death and disability in these patients [2]. Of the patients who survive SAH from a ruptured intracranial aneurysm, 25–30% suffer from ischaemic complications in the ensuing weeks. Ten to 15% of patients with SAH dies or experience permanent disability due to cerebral ischaemia [1, 3]. While up to 70% of patients with SAH experience an angiographic vasospasm, only 20–30% exhibit delayed ischaemic neurological deficits [4, 5].
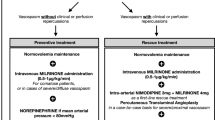
The first line of treatment of symptomatic cerebral vasospasm is medical therapy, which mainly includes hypervolaemia with haemodilution and hypertension (triple H). This is in order to increase the blood flow through the constricted cerebral arteries and to ameliorate the microcirculation [6]. More aggressive therapy is preserved for symptomatic patients that do not respond to conservative medical treatment. This includes intra-arterial infusion of vasodilators or endovascular balloon angioplasty [7–11].
The diagnosis of CV is based on clinical neurological assessment and angiographic findings. The gold standard for the diagnosis of CV is conventional digital subtraction angiography (DSA), an invasive procedure with known risks including 0.5% risk of stroke [12]. Many centres use daily transcranial doppler (TCD) ultrasound as a non-invasive method to detect CV. TCD, however, was reported to have low specificity [13] and is operator dependent. Furthermore, it requires a dedicated operator, who may not be available at all times and institution. CT perfusion (CTP) was suggested in addition to CT angiography (CTA) for early detection of CV [14, 15]; it, however, involves a considerable increase in the amount of radiation. In this study, we investigated the reliability of CT angiography (CTA) as a non-invasive alternative for the diagnosis of cerebral vasospasm and as a tool to make a treatment decision.
Materials and methods
This study retrospectively evaluated consecutive patients that presented with SAH and were suspected clinically to have vasospasm from June 2005 to June 2008. The study was approved by our institutional ethics committee. We included all patients that underwent CTA for this indication and DSA within 24 h.
Currently, in our institution, patients after SAH are monitored for vasospasm using clinical evaluation as well as TCD (TCD is however not available at all times). When there is a high level of suspicion of vasospasm, CTA is performed. In our institution, patients after SAH are routinely treated with nimodipine and euvolemia. Patients do not receive triple H in a prophylactic manner. The first line of treatment for patients with vasospasm is triple H followed by balloon angioplasty for patients that do not respond to triple H. Intra-arterial vasodilators are not used in our institution to treat vasospasm.
Image analysis
Two neuroradiologists retrospectively analysed CTA and DSA studies independently. Both readers practice as diagnostic and interventional neuroradiologists. The readers evaluated the CTA and DSA images 2 weeks apart and were blinded to the results of the other modality, the treatment decision made and the clinical findings of each patient. Each reader was required to decide if vasospasm is present, grade its severity and make a treatment recommendation (the latter based upon the assumption that clinical symptoms matched the vascular territory analysed). For assessment of severity of CV and comparison to baseline, CTA or DSA performed at presentation, prior to spasm, was available.
Firstly, each reader assessed the images for the presence or absence of vasospasm. Separate assessment was performed for central and peripheral arteries. Central vasospasm was classified as involvement of the proximal arteries of the circle of Willis [supraclinoid segment of the internal carotid arteries (ICA), the A1 segments of the anterior cerebral arteries (ACA), the M1 segments of middle cerebral arteries (MCA), the P1 segment of posterior cerebral arteries (PCA), the vertebral arteries (VA) and the basilar artery (BA)]. Peripheral vasospasm included involvement of smaller distal branches such as A2 and A3 segments of the ACA, M2 and M3 segments of the MCA, and P2 and P3 segment of the PCA. Secondly, in cases where central vasospasm was present, the readers were required to further grade the severity as mild, moderate, or severe. This evaluation was made by eye balling using the approximate following criteria: mild vasospasm = artery narrowed <30%, moderate vasospasm = artery narrowed ≥30% and <60% and severe vasospasm = artery narrowed ≥60% compared to the original arterial size. Whenever significant artefact from coils or clips was noted adjacent to an arterial segment, the authors indicated they could not evaluate this arterial segment.
As a last step, when CV was present, the readers were required to recommend a proper treatment based on their findings. They had to decide if to recommend conservative medical treatment (triple H) alone, balloon angioplasty or both. In general, triple H alone was recommended for mild vasospasm, while angioplasty was recommended for moderate and severe symptomatic vasospasm. The reader’s treatment recommendations were compared to the actual treatment received by each patient based on the clinical findings.
Imaging protocol
CT angiogram
All CTA examinations were performed with a 64-section multidetector CT scanner (Aquilion 64, Toshiba Medical Systems, Tokyo, Japan). Scanning was performed from the foramen magnum to the vertex. Intravenous contrast (iodixanol, Visipaque 270; GE Healthcare, Mississauga, Canada) was administered with a mechanical injector (StellantCTinjector; Medrad, Indianola, PA, USA). The injection rate was 4 mL/s, for a total volume of 60 mL followed by 20 mL of normal saline. Adequate timing of the CTA acquisition was achieved according to a Sure Start (Toshiba Medical Systems) technique. Acquisition parameters were 300 mA; 120 kV; matrix, 512_512; FOV, 28–32 cm; section thickness, 0.5 mm; pitch, 1.0; and an isotropic voxel size of 0.5 mm. Acquisition time was 11–16 s. Image processing consisted of axial source images as well as standardised coronal, and sagittal multiplanar volume reformatted MIP images (8-mm thickness, 2-mm reconstruction interval) and 3D volume-rendered reconstructions (performed on Advantage Windows Workstation, Version 4.2 or 4.3; GE Healthcare, Milwaukee, WI, USA). All these post-processed images along with the 0.5 mm thick base images were available for interpretation by the reviewers.
Cerebral digital subtraction angiogram
Included in this study are only patients that underwent DSA within 24 h from CTA. Patients that did not get DSA or that had DSA done more than 24 h after CTA were not included. The reasons for delay varied and included the patients’ response to a trial of triple H therapy and the severity of spasm at presentation.
DSA was performed with a dedicated biplane neuroangiography unit (LUA/LCN, GE Medical Systems, Buc, France) and included two- to four-vessel studies with standard frontal and lateral views as well as rotational spin angiograms with 3D reconstructions. A 4 or 5 F Berenstein diagnostic catheter (AngioDynamics, Queensbury, NY, USA) was used with the help of an angled 0.35-in. guide wire (Terumo; Meditech, Watertown, MA, USA). The contrast media used was nonionic (iodixanol, Visipaque 320; GE Healthcare). Injections were performed with a power injector (Mark V ProVis; Medrad). Standard injection rates and volumes were as follows: 4–5 mL/s for 8–10 mL for the ICAs and 3–4 mL/s for 7–8 mL/s for the vertebral arteries.
Statistical analysis
Contingency table analysis was performed to assess the sensitivity, specificity, overall accuracy, positive predictive value and negative predictive value of CTA in diagnosis of central and peripheral vasospasm with DSA being the gold standard. Kappa analysis was used to assess the strength of inter-observer agreement for the assessment of presence and severity of central or peripheral vasospasm as well as individually for specific arterial segment. Chi-square/Fisher’s exact test statistics was also performed to determine whether any relationship exists between the findings of CTA and DSA. Chi-square/Fisher’s exact tests were also performed to assess whether the recommended treatment based on the CTA assessment matched the actual treatment received by the patients. All analyses were carried out using the SAS System v.9.1.3 at an alpha level of 0.05.
Results
During the study period, our neurovascular service treated 412 patients with aneurysmal subarachnoid haemorrhage. Of these, a total of 150 patients underwent CTA due to clinically suspected vasospasm (i.e. the appearance of a new neurological deficit, such as drift, hemiparesis or drowsiness, which was not explained otherwise). Of these, 39 patients had DSA within 24 h of CTA. Five patients were excluded from our final analysis due to poor quality of CTA. This was due to extreme motion artefacts in two patients and because of lack of proper MIP reconstruction on the PACS in three patients.
The final analysis included 34 patients. Six of these were men and 28 women ranging from 36 to 76 years of age (average, 56.5; median, 57). The average time difference between the CTA and DSA was 12.4 h. CTA was performed on the day of onset of clinical vasospasm in all patients. The average time between the patient’s presentation with SAH to the onset of clinically suspected vasospasm was 5 days. Fourteen of the patients were treated with endovascular coiling and 18 with surgical clipping for their aneurysms. One patient had a dissecting aneurysm; his aneurysm did not undergo treatment due to poor clinical condition. Another patient had a SAH from an arteriovenous malformation (AVM) in the posterior fossa, with no aneurysm identified. It was decided to treat this AVM electively. Sixteen patients received angioplasty, and the other 18 received triple H or no treatment. On follow-up analysis, eight patients died and 26 patients were discharged home.
CTA in diagnosis of vasospasm
CTA was first evaluated for the diagnosis of CV. The sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) of CTA compared to DSA in case of central and peripheral vasospasm for readers 1 and 2 are shown in Table 1. The sensitivity, specificity, accuracy, PPV, and NPV of CTA were significantly higher for the diagnosis of central compared to peripheral vasospasm.
Secondly, CTA was evaluated for grading the severity of central vasospasm. The sensitivity, specificity, accuracy, PPV and NPV for different segments for reader 1 varied from 83% to 100%, 64–100%, 63–86%, 57–100% and 67–100%, respectively. For reader 2, these varied from 50% to 100%, 53–92%, 59–74%, 36–83% and 71–100%, respectively (Table 2).
The inter-observer agreement of the diagnosis of vasospasm of both central (Fig. 1) and peripheral vasospasm on CTA was substantial (kappa, 0.79 and 0.66, respectively). Inter-observer agreement for CTA between the two reviewers for the severity of central vasospasm of the various arterial segments ranged from fair to substantial (kappa, 0.40 to 0.72).
A 41-year-old female presented with subarachnoid haemorrhage. CT angiogram performed at admission showed a wide neck right posterior communicating artery (PCom) origin aneurysm and left cavernous carotid aneurysm. The patient underwent surgical clipping of the right PCom aneurysm, which was thought to have ruptured based on the distribution of the haemorrhage. The left cavernous carotid aneurysm remained untreated. Five days later, the patient started to become progressively drowsy. a CTA performed for the suspicion of vasospasm. Both readers agreed on the distribution and severity of diffuse central moderate vasospasm (arrows) involving bilateral supraclinoid internal carotid artery (ICA), M1 segment of bilateral middle cerebral artery (MCA) and A1 segment of bilateral anterior cerebral artery (ACA). Based on CTA, angioplasty was recommended by both readers in our study. b and c DSA performed 3 h later confirmed the severity and distribution of vasospasm (arrows). The patient underwent angioplasty with restoration of the caliber of bilateral supraclinoid ICA and M1 segment of bilateral MCAs
Three patients in the first reader group and six patients in the second reader group who were diagnosed as having no vasospasm on CTA eventually had vasospasm on DSA. Out of these, two patients in the first reader group and three in the second reader group had central vasospasm. The other patients had peripheral vasospasm. Only one patient had a discrepancy in both central and peripheral vasospasm for both readers. All of these patients were diagnosed with mild vasospasm on DSA. None of the patients diagnosed with no vasospasm on CTA was diagnosed with moderate or severe vasospasm on DSA.
In seven patients, the readers could not evaluate 12 arterial segments due to adjacent metal artefacts. These represent 3.3% out of the total 369 central arterial segments that were evaluated in this study. These segments include five P1 segments, four A1 segments, two supraclinoid carotids and one M1 segment. In five of the patients, the artefact was produced by coils and in two patients by clips. In all of these patients, the readers were able to evaluate the other arteries and to make a decision regarding treatment recommendation.
Treatment recommendation based on CTA
The inter-observer agreement regarding the recommended treatment for vasospasm with medical therapy (triple H) or balloon angioplasty based on CTA was excellent (kappa, 0.77) and very good (kappa, 0.53) respectively.
The treatment recommendation made by the readers based on CTA was compared with that of the actual treatment given to these patients. For both readers, the CTA recommendation of angioplasty was significantly predictive of actual receipt of angioplasty treatment (reader 1, chi square = 16.90, df = 1, p < 0.0001; reader 2, chi square = 7.56, df = 1, p = 0.0060). The CTA recommendation, however, was not significantly predictive for actual receipt of triple H treatment (p = 1 and 0.55 for readers 1 and 2 respectively). According to CTA, the readers predicted more triple H therapy compared to what patients actually received based on their clinical symptoms.
Discussion
As a result of the development of multi-slice CT scanners, CTA has emerged as an alternative non-invasive modality for imaging of the cerebral arteries. Its utility was demonstrated in the literature for imaging and therapeutic decision making for cerebral aneurysms [16–18]. In this study, we assessed the reliability of CTA as a non-invasive, alternative imaging tool, for the diagnosis of cerebral arterial vasospasm. We also checked if CTA would enable the physician to make a therapeutic decision for this condition, especially regarding invasive therapy such as balloon angioplasty.
CTA has been compared with DSA for assessment of vasospasm in several prospective [19, 20] and retrospective [21–24] studies. These studies showed high accuracy of CTA for the diagnosis of severe and central vasospasm. These studies varied in patient selection criteria and in the definition of the distribution of vasospasm and have thus yielded different sensitivity and specificity of CTA. We could not find studies that have assessed CTA for therapeutic decision making in these patients.
Our study supports previous studies and shows that CTA is useful for diagnosis of central vasospasm but less accurate for diagnosis of peripheral vasospasm. Our study yielded lower sensitivity and specificity for CTA for the diagnosis of peripheral vasospasm as compared to that for central vasospasm. This discrepancy is likely due to the limited spatial resolution of CTA. The peripheral arteries (diameter smaller than 2 mm) are significantly smaller than the proximal central arteries (diameter of 2–5 mm), which makes it difficult to visually depict subtle changes in vessel diameter on planar images.
Since the presence of significant vasospasm carries the risk of stroke, the role of imaging in these patients is not only to reach a diagnosis of vasospasm but mainly to make an appropriate clinical decision regarding the most suitable treatment. Triple H therapy is usually administrated based on clinical suspicion of vasospasm with supporting evidence from imaging. Patients who do not respond to triple H therapy are suspected to suffer from more severe spasm that might require aggressive invasive therapy. Balloon angioplasty is indicated when the patient does not respond to triple H, and there is moderate to severe vasospasm centrally involving the large vessels at the base of skull further leading to critical distal hypoperfusion. This study shows that CTA can diagnose the presence of central spasm and at the same time can make the differentiation between mild and moderate or severe spasm. Thus, CTA is helpful in choosing treatment in these patients and can provide supporting evidence to proceed from triple H to angioplasty. The relatively low sensitivity and negative predictive value for the diagnosis of peripheral vasospasm on CTA suggests that this modality would not be helpful at institutions that use intra-arterial infusion of vasodilators for elevation of peripheral spasm. However, our study suggests that CTA is useful in the diagnosis of severe central vasospasm, which is the condition that warrants invasive treatment with angioplasty.
To reinforce this finding, we checked if the treatment recommendation made by our reviewers matched the treatment that the patient received. In most of our patients, treatment recommendation based on CTA matched with the actual treatment received. More specifically, our findings show that the choice of angioplasty according to CTA highly matched the eventual scenario while the choice to administer triple H therapy was overestimated by our readers. This can be explained by the fact that CTA more accurately diagnose central than peripheral vasospasm. While the decision to angioplasty is made on the grounds of significant central spasm, triple H is administered mainly on the basis of clinical evaluation even in the presence of mild radiographic vasospasm. In our study, only three patients in the first reader group and six patients in the second reader group who were diagnosed as having no vasospasm on CTA eventually had vasospasm on DSA. All of these patients were diagnosed with mild vasospasm on DSA, and none were diagnosed with moderate or severe vasospasm on DSA. Patients with mild spasm on DSA would either receive no treatment or triple H alone according to their clinical presentation. The fact that CTA was negative in this group would thus not alter their treatment, which would be based on clinical symptoms.
The most important limitation of our study is a bias in patient’s selection. The patients included were only those who received conventional angiographic evaluation with DSA following their evaluation with CTA. In some patients who underwent CTA for vasospasm, DSA was no longer considered necessary; therefore, the group of patients presented herewith is biased as having (a) more severe vasospasm or (b) clinical vasospasm not responding to medical therapy. Another limitation is that several patients were excluded from this study due to poor image quality or lack of proper post-processing of the images. Poor image quality was usually due to patient movement or poor triggering of contrast injection. Such a scenario would be solved by repeating the CTA with proper sedation or proper triggering of contrast injection, but since this is a retrospective study, these patients had to be omitted. Another possible limitation is that in most of the patients, CTA and DSA were performed in great proximity, but in a few, there was a delay of up to 24 h. Since vasospasm is a dynamic process, the delay between CTA and DSA might have affected some of the inter-modality agreements.
Finally, it is important to mention that imaging for vasospasm is performed usually after clipping or coiling of an aneurysm responsible for the SAH. Streak artefacts from these metal devices could obscure adjacent arteries especially after coiling and influence CTA’s evaluation. In our study, this has occurred during the evaluation of 12 arterial segments (3.3%). This is a limitation of CTA and should be acknowledged when making a decision regarding spasm in an arterial segment adjacent to coil mass or a clip.
Conclusion
CTA is adequate for detecting central vasospasm in symptomatic subarachnoid haemorrhage patients. A negative result should not prevent further evaluation, especially when evaluating arterial segments obscured by metal artefacts from coils or clips. CTA is helpful in the treatment decision making in these patients especially regarding the need to proceed to aggressive endovascular treatment such as balloon angioplasty.
References
Macdonald RL, Weir B (1997) Cerebral vasospasm: prevention and treatment. In: Batjer HH, Caplan LR, Friberg L, Greenlee RG Jr, Kopitnik TA Jr, Young WL (eds) Cerebrovascular disease. Lippincott-Raven, Philadelphia, pp 1111–1121
Suarez JI, Tarr RW, Selman WR (2006) Aneurysmal subarachnoid haemorrhage. N Engl J Med 354:387–396
Kassel NF (1993) The role of vasospasm in overall outcome from aneurysmal subarachnoid haemorrhage. In: Findlay JM (ed) Cerebral vasospasm. Elsevier, Amsterdam, pp 27–28
Kassell NF, Sasaki T, Colohan AR, Nazar G (1985) Cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Stroke 16:562–572
Kodama N, Mizoi K, Sakurai Y, Suzuki J (1980) Incidence and onset of vasospasm. In: Wilkins RH (ed) Cerebral arterial spasm. Williams & Wilkins, Philadelphia, pp 361–365
Awad IA, Carter P, Spetzler RF, Medina M, Williams FC Jr (1987) Clinical vasospasm after subarachnoid hemorrhage: response to hypervolemic hemodilution and arterial hypertension. Stroke 18:365–372
Shankar JJ, Dos Santos PM, Deus-Silva L, Lum C (2011) Angiographic evaluation of the effect of intra-arterial milrinone therapy in patients with vasospasm from aneurysmal subarachnoid hemorrhage. Neuroradiology 53(2):123–128
Elliott JP, Newell DW, Lam DJ, Eskridge JM, Douville CM, Le Roux PD, Lewis DH, Mayberg MR, Grady MS, Winn HR (1998) Comparison of balloon angioplasty and papavarin infusion for the treatment of vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg 88:277–284
Terry A, Zipfel G, Milner E, Cross DT 3rd, Moran CJ, Diringer MN, Dacey RG Jr, Derdeyn CP (2006) Safety and technical efficacy of over the wire balloons for the treatment of subarachnoid hemorrhage induced cerebral vasospasm. Neurosurg Focus 21:1–7
Jun P, Ko NU, English JD, Dowd CF, Halbach VV, Higashida RT, Lawton MT, Hetts SW (2010) Endovascular treatment of medically refractory cerebral vasospasm following aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol 31(10):1911–1916
Suzuki S, Ito O, Sayama T, Goto K (2010) Intra-arterial colforsin daropate for the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neuroradiology 52(9):837–845
Willinsky RA, Taylor SM, terBrugge K, Farb RI, Tomlinson G, Montanera W (2003) Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature. Radiology 227:522–528
Gahn G, Gerber J, Hallmeyer S, Reichmann H, von Kummer R (1999) Noninvasive assessment of the circle of Willis in cerebral ischemia: the potential of CT angiography and contrast-enhanced transcranial color-coded duplexsonography. Cerebrovasc Dis 9:290–294
Aralasmak A, Akyuz M, Ozkaynak C, Sindel T, Tuncer R (2009) CT angiography and perfusion imaging in patients with subarachnoid hemorrhage: correlation of vasospasm to perfusion abnormality. Neuroradiology 51(2):85–93
Dankbaar JW, Rijsdijk M, van der Schaaf IC, Velthuis BK, Wermer MJ, Rinkel GJ (2009) Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology 51(12):813–819
Agid R, Lee SK, Willinsky RA, Farb RI, terBrugge KG (2006) Acute subarachnoid hemorrhage: using 64-slice multidetector CT angiography to “triage” patients’ treatment. Neuroradiology 48:787–794
Westerlaan HE, Gravendeel J, Fiore D, Metzemaekers JD, Groen RJ, Mooij JJ, Oudkerk M (2007) Multislice CT angiography in the selection of patients with ruptured intracranial aneurysms suitable for clipping or coiling. Neuroradiology 49:997–1007
Schuknecht B (2007) High-concentration contrast media (HCCM) in CT angiography of the carotid system: impact on therapeutic decision making. Neuroradiology 49(Suppl 1):S15–S26
Chaudhary SR, Ko N, Dillon WP, Yu MB, Liu S, Criqui GI, Higashida RT, Smith WS, Wintermark M (2008) Prospective evaluation of multidetector-row CT angiography for the diagnosis of vasospasm following subarachnoid hemorrhage: a comparison with digital subtraction angiography. Cerebrovasc Dis 25:144–150
Goldsher D, Shreiber R, Shik V, Tavor Y, Soustiel JF (2004) Role of multisection CT angiography in the evaluation of vertebrobasilar vasospasm in patients with subarachnoid hemorrhage. AJNR Am J Neuroradiol 25:1493–1498
Takagi R, Hayashi H, Kobayashi H, Kumazaki T, Isayama K, Ikeda Y, Teramoto A (1998) Three-dimensional CT angiography of intracranial vasospasm following subarachnoid haemorrhage. Neuroradiology 40:631–635
Anderson GB, Ashforth R, Steinke DE, Findlay JM (2000) CT angiography for the detection of cerebral vasospasm in patients with acute subarachnoid hemorrhage. AJNR Am J Neuroradiol 21:1011–1015
Otawara Y, Ogasawara K, Ogawa A, Sasaki M, Takahashi K (2002) Evaluation of vasospasm after subarachnoid hemorrhage by use of multislice computed tomographic angiography. Neurosurgery 51:939–942, discussion 942–943
Yoon DY, Choi CS, Kim KH, Cho BM (2006) Multidetector-row CT angiography of cerebral vasospasm after aneurysmal subarachnoid hemorrhage: comparison of volume-rendered images and digital subtraction angiography. AJNR Am J Neuroradiol 27:370–377
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 23 kb)
Rights and permissions
About this article
Cite this article
Shankar, J.J.S., Tan, I.Y.L., Krings, T. et al. CT angiography for evaluation of cerebral vasospasm following acute subarachnoid haemorrhage. Neuroradiology 54, 197–203 (2012). https://doi.org/10.1007/s00234-011-0876-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-011-0876-9