Abstract
Systematic reviews of systematic reviews identify good quality reviews of earlier studies of medical conditions. This article describes a systematic review of systematic reviews performed to investigate factors that might influence the risk of rupture of an intracranial aneurysm. It exemplifies the technique of this type of research and reports the finding of a specific study. The annual incidence of subarachnoid haemorrhage resulting from the rupture of intracranial aneurysms is estimated to be nine per 100,000. A large proportion of people who have this bleed, will die or remain dependent on the care of others for some time. Reliable knowledge about the risks of subarachnoid haemorrhage in different populations will help in planning, screening and prevention strategies and in predicting the prognosis of individual patients. If the necessary data were available in the identified reviews, an estimate for the numerical relationship between a particular characteristic and the risk of subarachnoid haemorrhage was included in this report. The identification of eligible systematic reviews relied mainly on the two major bibliographic databases of the biomedical literature: PubMed and EMBASE. These were searched in 2006, using specially designed search strategies. Approximately 2,000 records were retrieved and each of these was checked carefully against the eligibility criteria for this systematic review. These criteria required that the report be a systematic review of studies assessing the risk of subarachnoid haemorrhage in patients known to have an unruptured intracranial aneurysm or of studies that had investigated the characteristics of people who experienced a subarachnoid haemorrhage without previously being known to have an unruptured aneurysm. Reports which included more than one systematic review were eligible and each of these reviews was potentially eligible. The quality of each systematic review was assessed. In this review, 16 separate reports were identified, including a total of 46 eligible systematic reviews. These brought together research studies for 24 different risk factors. This has shown that the following factors appear to be associated with a higher risk of subarachnoid haemorrhage: being a woman, older age, posterior circulation aneurysms, larger aneurysms, previous symptoms, “non-white” ethnicity, hypertension, low body mass index, smoking and alcohol consumption of more than 150 g per week. The following factors appear to be associated with a lower risk of subarachnoid haemorrhage: high cholesterol, diabetes and use of hormone replacement therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The annual incidence of subarachnoid haemorrahge resulting from the rupture of intracranial aneurysms is estimated to be nine per 100,000 [1]. A large proportion of people who have this bleed, will die or remain dependent on the care of others for some time. Reliable knowledge about the risks of subarachnoid haemorrhage in different populations will help in planning, screening and prevention strategies and in predicting the prognosis of individual patients. Reliable knowledge in health care increasingly comes from systematic reviews. These are now common as means of synthesising the findings from research studies. Although the majority of such reviews concern the effects of interventions, not least because of the work of The Cochrane Collaboration [2], there are an increasing number of systematic reviews of other topics such as risk factors, diagnostic test accuracy, disease prognosis and genetic associations [3]. This is also true in stroke care generally and the management of subarachnoid haemorrhage more specifically. For example, the Cochrane Stroke Group has prepared several systematic reviews of interventions following subarachnoid haemorrhage, including antiplatelet drugs [4], calcium antagonists [5] and the timing of treatment [6].
The challenge of the plethora of reports of individual studies stimulated an increase in the number of review articles in the last few decades which, in turn, has now evolved into the challenges of coping with multiple reviews of the same topics. Some of the these reviews are systematic; providing clear details on the eligibility criteria, methods, findings and conclusions; while others continue to make it difficult for the reader to appraise their relevance, quality, and reliability—as was highlighted more than 20 years ago [7].
This systematic review of reviews was prepared as part of the @neurIST project to help overcome this problem. It seeks to identify, appraise and summarise existing reviews of the risk of subarachnoid haemorrhage in patients already known to have an unruptured intracranial aneurysm and of the relationship between patient characteristics and subarachnoid haemorrhage in patients who were not known to have an unruptured aneurysm before it ruptured. Where these were available in the identified reviews, this paper includes an estimate of the relevant risk.
The concept of a systematic review of reviews is relatively new but the methods followed are akin to those used for systematic reviews themselves, such as those in use within The Cochrane Collaboration. Other examples include a systematic review of systematic reviews of prognostic factors in breast cancer [8] and the factors associated with the prediction of pre-term birth [9].
Methods
The eligibility criteria for including reviews in this systematic review were that the target review was itself systematic and that it included studies investigating the relationship between a patient characteristic or other factor and subarachnoid haemorrhage.
To be classified as a “systematic review”, the published research had to describe methods that involved comprehensive searching for studies, the application of inclusion criteria, appraisal of the included studies and some attempt to synthesise the findings of the included studies into a summary of the relationship between a patient characteristic or other factor and subarachnoid haemorrhage. These syntheses could include formal meta-analyses based on aggregate data (either extracted from publications or obtained directly from the original researchers) or could be based on the central collection and analyses of individual patient data. Eligible systematic reviews included both those that assessed the risk of subarachnoid haemorrhage in patients who were previously known to have had an unruptured intracranial aneurysm and those in which the people who had the subarachnoid haemorrhage were not previously known to have had an unruptured intracranial aneurysm.
Published research on risk factors for subarachnoid haemorrhage was sought in the two main indexed bibliographic databases of the health literature: MEDLINE and EMBASE. Searches were designed for these databases by an information specialist experienced in systematic reviews. These searches included a mixture of free text and index terms to try to maximise the retrieval of potentially relevant reports. The searches were run in May 2006. MEDLINE was searched via PubMed using the following search string: (subarachnoid haemorrhag*[Text Word] OR “subarachnoid hemorrhage”[MeSH Terms] OR subarachnoid hemorrhag*[Text Word]) AND systematic[sb]. The term systematic[sb] calls up a set of terms which is available in PubMed to retrieve systematic reviews. The search string used to search EMBASE (using OvidWeb) was: (Subarachnoid Hemorrhage/ OR subarachnoid h?emorrhag$.tw.) AND (review.pt. OR review/ OR meta analysis/ OR “systematic review”/ OR review$ OR meta?analy$ OR overview$).tw. An abridged search, using the EMTREE term “systematic review” in combination with (Subarachnoid Hemorrhage/ OR subarachnoid h?emorrhag$.tw.) was also run on EMBASE to generate a smaller subset of the records from the main search, in order to determine the impact of this restriction.
Although the searches were not limited by publication date or language, a lack of language restrictions does not mean that articles published in languages other than English have the same chance of retrieval as articles published in English. This is because journals in languages other than English are under-represented in databases such as MEDLINE and EMBASE [10].
I checked all retrieved records twice, separated by at least 4 weeks, to reduce the possibility that I would miss relevant records. Research has shown that screening records twice, is less likely to overlook studies for systematic reviews, than screening all records once or three times [11].
A list of potentially relevant reports was shared with other people in the @neurIST project in March 2007, to help identify whether any systematic reviews were missing. The full-text articles for all potentially relevant reports were then obtained, assessed for eligibility, and checked to see if they cited any additional potentially relevant systematic reviews.
To assess quality of the included reviews, the following features were recorded for each systematic review judged to be eligible: (1) extent of searching (including databases and any language or time period restrictions); (2) description of the eligibility criteria; (3) source of data for any analyses in the review; (4) assessment of publication bias; (5) assessment of heterogeneity; (6) conduct of sensitivity analyses; and (7) attempts to control for confounders in the analyses of the included studies. Additional information was not sought from the authors of the reviews.
To estimate the risk of subarachnoid haemorrhage, data were extracted from any meta-analyses for particular risk groups and for any statistical comparisons of the relative risk among different risk groups. For example, where available, results would be extracted for men and women separately, and for women compared to men. Additional data were not sought from the authors of the reviews.
I did the assessments of quality and the extraction of data from each eligible review twice, separated by at least 3 weeks, and without access to the information for the earlier check of the article. This assessment, along with the data extraction, formed the basis for deciding on the inclusion of reviews in this report. This work was completed in July 2007.
Results
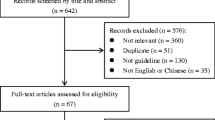
The searches retrieved 120 records (PubMed), 1,928 records (full EMBASE search) and 35 records (abridged EMBASE search). These 35 records were all contained in the full set from EMBASE and some of the records were in both the PubMed and the EMBASE sets. However, I checked the complete set of 2,048 records, without any prior de-duplication, to ensure that potentially relevant articles were not missed.
The screening of the records from the searches identified several systematic reviews relating to risk factors for intracranial aneurysms, their rupture and subsequent prognosis. It also revealed many reports of individual studies of risk, usually because the word “review” had been used to describe the process of checking the records for a case series or cohort of patients with ruptured or unruptured intracranial aneurysms. As set out in the “Methods” section, individual studies were not eligible for this systematic review and no attempt was made to synthesise their findings.
After screening the records from the databases, obtaining potentially relevant articles and checking their references, I identified 16 separate articles [12–27], containing a total of 46 systematic reviews of risk factors for the rupture of intracranial aneurysms. These were published between 1986 and 2006. One additional paper was obtained in full following the assessment of the records retrieved from the databases [28]. This was judged to be ineligible, because it was a general discussion of various aspects of stroke, in particular intracerebral haemorrhage. The 46 eligible systematic reviews investigated previous research for 24 different risk factors. These are shown in Table 1. This, and the discussion of the factors below, is ordered from characteristics of the individual that cannot be changed by an intervention (such as sex and age), through characteristics of their aneurysm, clinical history, family history and other genetic factors, and then temporal factors. One of the eligible systematic reviews[18] is not discussed in detail here, because its updated and expanded version is used instead [15]. Furthermore, four of the eligible reviews make relatively little contribution to this report because of their scope or a lack of sufficient information to assess the quality. These are discussed below and this report is therefore based mainly on 11 systematic reviews. In general, the quality of these reviews was good, and information on their conduct is summarised in Table 2.
The remainder of this “Results” section is structured to show the evidence for each risk factor for which at least one relevant review was identified. Information is provided on the scope and quality of the identified reviews and their conclusions. If a review included meta-analyses combining the results of the included studies, the summary estimates and their precision (where available) for the relationship between the risk factor and subarachnoid haemorrhage are given.
Sex
Sex was identified as an important influence on the risk of subarachnoid haemorrhage in many of the reports identified for this systematic review. Some of the other risk factors were presented separately for men and women, and this is discussed below where relevant.
The most comprehensive review that dealt in detail with the association between sex and subarachnoid haemorrhage was by Rinkel et al. [13]. This sought studies published from 1955 to June 1996 on intracranial saccular aneurysms. The reviewers searched MEDLINE from 1966 onwards and checked the reference lists of all relevant publications, until their cross checking found no new publications. They found that prevalence was lower among men than women. In their combined analysis of 15 angiography studies, there were 61 aneurysms among 1,754 men, giving a prevalence of 3.5% (95% confidence interval (CI) 2.7 to 4.5). Among women, there were 58 aneurysms in 1,254 women, with a prevalence of 4.6% (95% CI 3.5 to 5.9). The relative risk of having an aneurysm for men compared to women was reported to be 0.8 (95% CI 0.5 to 1.1).
In assessing the risk of subarachnoid haemorrhage in patients known to have an unruptured aneurysm, Rinkel et al. found nine studies with a total of 3,907 patient years of follow-up [13], but sex data were not available from all these studies. However, the annual risk of rupture for men was found to be 1.3% (95% CI 0.7 to 2.1), based on 13 ruptures in 1,027 patient years for men. There were 34 ruptures in 1,304 patient years of follow-up for women, giving an annual risk of rupture of 2.6% (95% CI 1.8 to 3.6). The relative risk for women compared to men was 2.1 (95% CI 1.1 to 3.9).
The Linn et al. review of the incidence of subarachnoid haemorrhage in the general population identified six studies that reported the results separately for men and women [12]. The annual incidence for men was found to be 4.5 per 100,000 (95% CI 3.1 to 5.8), compared to 7.1 (5.4 to 8.7) for women. The relative risk for women compared to men was 1.6 (1.1 to 2.3).
A review of studies conducted in Japan was reported by Morita et al. [14]. This reviewed 13 studies on unruptured cerebral aneurysms published by Japanese institutions from 1980 to 2003. The review included 922 patients with unruptured cerebral aneurysms, and 3,801 patient years of follow-up and the authors calculated that the annual risk of rupture for men was 2.2% (95% CI 1.5 to 3.1) and 3.0% (95% CI 2.3 to 4.0) for women. This gave a relative risk for women compared to men of 1.4 (95% CI 0.9 to 2.2).
One report was a review of studies of risk factors and subarachnoid haemorrhage among patients with autosomal dominant polycystic kidney disease [19], and this is discussed in more detail below. Sex was one of the risk factors studied and among people with autosomal dominant polycystic kidney disease having a subarachnoid haemorrhage, the ratio of women to men was 1.1 (lower than that for the general population).
Age
Some reviews of other risk factors discussed these in the context of the age of the patient. One review investigated the association between age and subarachnoid haemorrhage in detail for the general population, based on studies published from 1955 to June 1996 on the prevalence and natural history of intracranial saccular aneurysms [13]. The authors found a total of nine studies with 3,907 patient years of follow-up assessing the risk of subarachnoid haemorrhage in patients with unruptured aneurysms and calculated annual risks of rupture for 20-year age groups, using the 40–59 years group as the reference standard. There were no ruptures in the 26 patient years of follow-up in patients aged 20–39 years, giving an estimated annual risk of rupture of 0 (95% CI 0 to 13) for this age group. There were seven ruptures in 203 patient years of follow-up for patients aged 40–59 years (annual risk of rupture 3.5%, 95% CI 1.4 to 7.0). Among patients aged 60–79 years, there were 297 patient years of follow-up and 17 ruptures (annual risk of rupture 5.7%, 95% CI 3.4 to 9.0). The relative risk for patients aged 60–79 years compared to those aged 40–59 was 1.7 (95% CI 0.7 to 4.0). There were no data for patients aged less than 20 years or more than 80 years.
The Morita et al. review of studies from Japanese institutions investigated age [14]. They present the results for patients in two age groups, divided at 60 years of age. For the younger people, the annual risk of rupture was 2.3% (95% CI 1.6 to 3.2). It was 3.0% (95% CI 2.3 to 3.8) for those aged 60 years or older. The relative risk for people over 60 years compared to the younger group was 1.2 (95% CI 0.8 to 1.9).
Gieteling and Rinkel found that patients with polycystic kidney disease had subarachnoid haemorrhage at younger ages than people without this condition. They reported that the mean age at the time of subarachnoid haemorrhage for patients with autosomal dominant polycystic kidney disease was 41 years, compared to around 57 years for the general population [19].
Ethnicity
The Feigin et al. review of ten risk factors included ethnicity, dividing the population into “white” and “non-white” [15]. They searched MEDLINE from 1966 to March 2005, and checked the reference lists of retrieved articles, for studies published in English that reported crude data on risk factors for subarachnoid haemorrhage. Separate estimates were calculated for the longitudinal and the case control studies, and results were reported separately for men and women where this division had been used in the original research. The one longitudinal study included in the review did not include any women and found that the relative risk of subarachnoid haemorrhage for “non-white” men compared to “white” men was 1.8 (95% CI 0.8 to 4.2). The review included two case control studies, which did not provide separate estimates for men and women, and the meta-analysis gave an overall odds ratio of 3.4 (1.0 to 11.9) for “non-white” populations compared to those who were “white”.
As mentioned above, one of the identified reviews focused on studies published by Japanese institutions from 1980 to 2003. This drew descriptive comparisons with other populations and highlighted the higher incidence of rupture of intracranial aneurysms in patients in Japan compared to elsewhere [14]. The review sought studies in MEDLINE (1981 onwards) and the Index of the Japan Medical Abstract Society (1983 onwards), as well as checking the reference lists of all relevant articles for additional studies. Thirteen studies were included, eight that had been published in English and five that had been published in Japanese. A total of 922 patients with unruptured cerebral aneurysms, with 3,801 patient years of follow-up, were included. There were 104 subsequent ruptures, giving an annual risk of rupture of 2.7% (95% CI 2.2 to 3.3). Morita et al. write that this is “relatively high” compared to Europe and North America. They contrast it with the finding from Rinkel et al. of 75 ruptures in 3,907 patient years of follow-up where the annual risk of rupture was 1.9% (95% CI 1.5 to 2.4) [13].
Turning to North America and Europe, the review by Linn et al. highlights the high incidence of subarachnoid haemorrhage in Finland [12]. They sought studies published from 1960 to 1994 by searching MEDLINE (from 1960 onwards) and Science Citation Index (from 1980 onwards). They checked the reference lists of all relevant publications for other studies about the incidence of subarachnoid haemorrhage and stroke more generally. The review includes a total of 18 studies with 10.6 million person years: three studies from Finland (2.2 million person years) and 15 from elsewhere (8.4 million person years). The combined analysis of the three studies from Finland produced an annual incidence of subarachnoid haemorrhage of 21.4 per 100,000 (95% CI 19.5 to 23.4), which is compared to 7.8 per 100,000 (95% CI 7.2 to 8.4) in the other 15 studies. The relative risk for people in Finland compared to people elsewhere was estimated to be 2.7 (95% CI 2.4 to 3.1). This remained significant (2.1) after the reviewers adjusted their analyses to take account of the proportion of diagnoses done with computed tomography and the year of the original study.
I identified one report which focused on studies of stroke in black Americans [16]. However, this provided no information on how papers were searched for, assessed or selected for inclusion in the review; and there is no numerical estimate of the risk of either the formation or rupture of an aneurysm in black Americans. Several studies of stroke in this population were discussed in the report, but given the additional shortcoming (for the purposes of this systematic review) that subarachnoid haemorrhage was not distinguished from stroke in general, no estimates of the risk of intracranial aneuryms or their rupture are available from this report.
Another of the reviews identified for this systematic review, which studied the role of Apolipoprotein E Genotype (APOE) in different types of stroke and is discussed in detail below, reported that information on ethnicity had been extracted from included studies [25]. However, the report does not provide further information on this for the three studies of the relationship between APOE and subarachnoid haemorrhage.
Site of aneurysm
The Rinkel et al. review [13] investigated the association between site and subarachnoid haemorrhage for the general population. In assessing the risk of subarachnoid haemorrhage in patients with known unruptured aneurysms, nine studies with 3,907 patient years of follow-up were found but some of these did not provide data on the site of the ruptured aneurysm. Using the studies that reported these data, they calculated annual risks of rupture for aneurysms on the anterior communicating artery, middle cerebral artery, internal carotid artery and posterior circulation. They used anterior communicating artery aneurysms as the reference standard for their comparisons. There were five ruptures in 464 patient years of follow-up (annual risk of rupture 1.1%, 95% CI 0.4 to 2.5) at this site. For middle cerebral artery aneurysms, there were 17 ruptures in 1,519 patient years (annual risk of rupture 1.1%, 95% CI 0.7 to 1.8); there were 30 ruptures in 2,449 patient years for internal carotid artery aneurysms (annual risk of rupture 1.2%, 95% CI 0.8 to 1.7), and 19 ruptures in 434 patient years for aneurysms on the posterior circulation (annual risk of rupture 4.4%, 95% CI 2.7 to 6.8). The relative risk for rupture compared to the anterior communicating artery was 1.0 (95% CI 0.4 to 2.8) for the middle cerebral artery, 1.1 (95% CI 0.4 to 2.9) for the internal carotid artery and 4.1 (95% CI 1.5 to 11) for the posterior circulation.
The Morita et al. review of studies on the natural course of unruptured cerebral aneurysms in Japan investigated the site of the ruptured aneurysm and presented results separately for aneurysms on the anterior circulation and posterior circulation only [14]. Patients with an aneurysm on the anterior circulation had an annual risk of rupture of 1.8% (95% CI 1.3 to 2.3). The annual risk was 3.2% (95% CI 2.0 to 5.0) for people with an aneurysm on the posterior circulation. The relative risk for posterior compared to anterior circulation aneurysms was 2.3 (95% CI 1.4 to 3.7).
The Gieteling and Rinkel review [19] of studies in patients with autosomal dominant polycystic kidney disease found that 41% (51) of the 124 ruptured aneurysms with site specified were on the anterior communicating artery, 38% (47) were on the middle cerebral artery, 12% (15) were on the internal carotid artery and 8.9% (11) were on the posterior circulation. They concluded that the site of ruptured aneurysms is similar for patients with and without autosomal dominant polycystic kidney disease, with the anterior communicating artery being the most common site.
Size of aneurysm
The same three reviews that investigated the site of ruptured aneurysms also studied size. The Rinkel et al. review categorised aneurysms into smaller and larger, around 10 mm [13]. They report 27 ruptures in 3,742 patient years of follow-up for aneurysms that were 10 mm or smaller, giving an annual risk of rupture of 0.7% (95% CI 0.5 to 1.0), and 27 ruptures in 675 patient years for larger aneurysms (annual risk of rupture 4.0%, 95% CI 2.7 to 5.8). The relative risk of rupture for aneurysms larger than 10 mm was 5.5 (95% CI 3.3 to 9.5) compared to those of 10 mm or less. Rinkel et al. noted the possibility of a relationship between the size of an unruptured aneurysm and the presence of symptoms (discussed in the next section of this report), which might confound the association between both of these risk factors and subarachnoid haemorrhage. However, they were unable to assess the interdependence of these factors because of insufficient data in the studies in their review.
The Morita et al. review of studies on the natural course of unruptured cerebral aneurysms published by Japanese institutions from 1980 to 2003 also dichotomised the data into aneurysms smaller and larger than 10 mm [14]. For patients with an aneurysm smaller than 10 mm, the annual risk of rupture was 1.5% (95% CI 1.0 to 2.2). The annual risk was 9.3% (95% CI 6.4 to 13.1) for aneurysms larger than 10 mm and the relative risk for larger compared to smaller aneurysms was 6.4 (95% CI 4.0 to 10.4).
A finer categorisation of aneurysm size was used in the review of autosomal dominant polycystic kidney disease and subarachnoid haemorrhage [19]. They sought to use 5-mm bands but found relatively little information on size in the included studies and they could study it for only 40 of the 258 ruptured aneurysms. Among these 40, 20% (8) were smaller than 5 mm; 33% (13) were between 5 and 9 mm; 33% (13) were between 10 and 24 mm and 15% (6) were larger than 25 mm. The authors noted that large aneurysms appeared to more common in patients with autosomal dominant polycystic kidney disease than in people without this condition. In the part of the Gieteling and Rinkel review which studied the prevalence of unruptured aneurysms, they found that 40% (46) of the 114 aneurysms with size specified were smaller than 5 mm; 32% (37) were between 5 and 9 mm; 19% (22) were between 10 and 24 mm and 7.9% (9) were larger than 25 mm. This is in contrast to the prevalence data in the Rinkel et al. review, which also categorised size into 5-mm groups [13]. They found that 72% (257) of the 356 aneurysms in two autopsy and ten angiography studies were smaller than 6 mm; 21% (74) were between 6 and 10 mm; 6.5% (23) were between 10 and 20 mm and 0.56% (2) were larger than 20 mm.
Symptoms before the subarachnoid haemorrhage
Two reviews investigated the presence of symptoms before the subarachnoid haemorrhage [13, 14], as distinct from a previous subarachnoid haemorrhage which is discussed in the next section of this report.
In the Rinkel et al. review, aneurysms were categorised into asymptomatic and symptomatic [13]. They also used an “additional” category for aneurysms found following a subarachnoid haemorrhage from another aneurysm. There were nine ruptures in 1,145 patient years of follow-up for patients with asymptomatic aneurysms (annual risk of rupture 0.8%, 95% CI 0.4 to 1.5) and 30 ruptures in 463 patient years for symptomatic aneurysms (annual risk of rupture 6.5%, 95% CI 4.4 to 9.1). The relative risk of rupture for symptomatic compared to asymptomatic aneurysms was 8.2 (95% CI 3.9 to 17). As noted in the preceding section of this report (“Size of aneurysm”), Rinkel et al. noted that there might be confounding between the size of an unruptured aneurysm and the presence of symptoms, but that there was insufficient data in the included studies to investigate this in their review.
The Morita et al. review of Japanese studies investigated symptoms as a risk factor for subarachnoid haemorrhage in patients with unruptured cerebral aneurysms [14]. Patients without symptoms had an annual risk of rupture of 2.6% (95% CI 2.1 to 3.1). It was 7.3% (95% CI 3.5 to 13.4) if symptoms were present. The relative risk for the presence of symptoms compared to their absence was 2.1 (95% CI 1.1 to 3.9).
Previous subarachnoid haemorrhage
The Morita et al. review of studies in patients with unruptured cerebral aneurysms published by Japanese institutions from 1980 to 2003 investigated whether a previous subarachnoid haemorrhage was a risk factor for a future subarachnoid haemorrhage [14]. Patients without a previous subarachnoid haemorrhage had an annual risk of rupture of 2.7% (95% CI 2.1 to 3.4), similar to that for patients who had had a previous subarachnoid haemorrhage (annual risk of rupture 2.8%, 95% CI 1.8 to 4.0); giving a relative risk for patients with a previous subarachnoid haemorrhage compared to those without one of 1.3 (95% CI 0.85 to 2.0).
Blood pressure
Two of the included systematic reviews presented evidence on the relationship between blood pressure and subarachnoid haemorrhage. One of these was based on the central collection and re-analysis of individual patient data in the Asia Pacific Cohort Studies Collaboration [17]. The other was the review by Feigin et al., which relied mostly on published data [15]. Furthermore, Morita et al. had attempted to investigate hypertension, but were unable to do because insufficient data were available in the studies they identified [14].
The Asia Pacific Cohort Studies Collaboration review combined data from 26 cohort studies: 306,620 participants and 1,898,565 person years of follow-up to investigate a variety of risk factors for subarachnoid haemorrhage (see below) [17]. There were 236 subarachnoid haemorrhage events, 114 of which led to death within 28 days. For their blood pressure analyses, the researchers divided systolic blood pressure into two groups: below 140 mmHg and equal to, or greater than, 140 mmHg. They also analysed it as a continuous variable. The dichotomous analysis found a hazard ratio for subarachnoid haemorrhage of 2.0 (95% CI 1.5 to 2.7) for the higher blood pressure group. The continuous variable analysis found that the risk of subarachnoid haemorrhage increased steeply with blood pressure. Each 10-mmHg increase in systolic blood pressure was associated with a 31% (95% CI 23 to 38) increase in the risk of a subarachnoid haemorrhage.
The Feigin et al. review divided patients into those with hypertension and those without, but the blood pressure cutpoint was not reported [15]. They conclude that higher blood pressure is statistically significantly associated with a higher risk of subarachnoid haemorrhage. Their meta-analyses of the longitudinal studies found that the relative risk of subarachnoid haemorrhage for patients with hypertension compared to those without it was 2.5 (95% CI 2.0 to 3.1) for both sexes combined, 3.3 (95% CI 2.1 to 5.3) for women and 2.3 (95% CI 1.8 to 3.0) for men. Using case control studies, they obtained odds ratios for hypertensive compared to non-hypertensive patients of 2.6 (95% CI 2.0 to 3.1) overall, 3.3 (95% CI 2.6 to 4.3) for women and 2.1 (95% CI 1.4 to 3.2) for men.
Cholesterol
As with high blood pressure, the relationship between cholesterol and subarachnoid haemorrhage was investigated in both the individual patient data meta-analyses by the Asia Pacific Cohort Studies Collaboration [17] and the review by Feigin et al. [11].
The Asia Pacific Cohort Studies Collaboration review divided cholesterol levels into two groups: below 4.5 mmol/L and equal to, or greater than, 4.5 mmol/L.[17] The meta-analysis obtained a hazard ratio for subarachnoid haemorrhage was 0.9 (95% CI 0.7 to 1.3) for the higher cholesterol group compared to the group with less than 4.5 mmol/L.
Feigin et al. divided patients into those with hypercholesterolemia and those without, but did not report the threshold [15]. They conclude that hypercholesterolemia appears to reduce the risk of subarachnoid haemorrhage. They included three longitudinal studies, all of which studied men only and found a relative risk of subarachnoid haemorrhage of 0.8 (95% CI 0.6 to 1.3) for men with hypercholesterolemia compared to those without it. Their meta-analysis of three case control studies produced odds ratios of 0.6 (95% CI 0.4 to 0.9) overall, 1.2 (95% CI 0.5 to 2.5) for women and 0.5 (95% CI 0.2 to 1.9) for men with hypercholesterolemia compared to those without it.
Diabetes
The Feigin et al. review assessed the relationship between diabetes and subarachnoid haemorrhage [15]. It included one longitudinal study and six case control studies in the relevant meta-analyses. The longitudinal study identified for the review found a relative risk of subarachnoid haemorrhage for diabetics compared to non-diabetics of 0.3 (95% CI 0.0 to 2.2) for both sexes combined. It was found to be 0 (95% CI 0.0 to 2.9) for women and 0.7 (95% CI 0.1 to 4.7) for men. The overall odds ratio from the case control studies was 0.7 (95% CI 0.5 to 0.8) for diabetics versus non-diabetics. Data were not available separately for men and women.
Body mass index
The relationship between body mass index (weight divided by square of height) and subarachnoid haemorrhage was investigated in the individual patient data meta-analyses by the Asia Pacific Cohort Studies Collaboration [17] and the review by Feigin et al. [15].
The Asia Pacific Cohort Studies Collaboration review analysed body mass index as dichotomous data (below 22 kg/m2 and equal to, or greater than, 22 kg/m2) and found that the hazard ratio was 1.0 (95% CI 0.7 to 1.3) for the larger group compared to the smaller.
The Feigin et al. review of published data also used this cutpoint for body mass index [15]. As with its other meta-analyses, it included separate meta-analyses for longitudinal studies and case control studies, but the reviewers found it difficult to compare these findings for this risk factor. There was one longitudinal study of body mass index and subarachnoid haemorrhage, but it was restricted to men and provided a relative risk of 0.4 (95% CI 0.2 to 0.4) for the lower body mass index compared to the higher. In contrast, the two case control studies only allowed the reviewers to estimate the relationship for women and for both sexes combined. These gave odds ratios of 1.4 (95% CI 1.0 to 2.0) overall and 1.1 (95% CI 0.7 to 1.9) for women (i.e. increased odds for lower compared to higher body mass index).
Polycystic kidney disease
I identified two systematic reviews of the relationship between polycystic kidney disease and subarachnoid haemorrhage [13, 19]. The earlier report [13] focused on the prevalence of aneurysms in patients with polycystic kidney disease rather than their risk of subarachnoid haemorrhage and its contents were updated by second report [19]. This combined data on 369 autosomal dominant polycystic kidney disease (ADPKD) patients, with 462 intracranial aneurysms, that had been reported in 53 articles. Two hundred and fifty-eight of the ADPKD patients had had a subarachnoid haemorrhage. The authors also report on the presence of ADPKD in patients in their own database of patients treated for subarachnoid haemorrhage between 1978 and 1999: five of these 1,147 patients (0.44%) had ADPKD. The review does not contain an estimate for the risk of having an intracranial aneurysm or a subarachnoid haemorrhage among patients with ADPKD.
Some of the differences between patients with and without ADPKD who have intracranial aneurysm and subarachnoid haemorrhage that were discussed by Gieteling and Rinkel have been noted in earlier sections. They reported differences in sex (contrasting the ratio of women to men of 1.6 in the general population with the 1.1 found for the ADPKD patients in the review), age at subarachnoid haemorrhage (contrasting the mean age of 57 years for patients in general with 41 years in ADPKD patients), the most common site of prevalent aneurysms (the middle cerebral artery in ADPKD patients, compared to the internal carotid artery in people without ADPKD), the size of aneuryms (typically larger for patients with ADPKD) and the proportion of patients with a positive family history (defined as first or second degree relative with subarachnoid haemorrhage or intracranial aneurysms) which was reported in 40% of patients with ADPKD compared to approximately 14% of patients without ADPKD (see below). They also report similarities, including the most frequent site of ruptured aneurysms (the anterior communicating artery in both ADPKD patients and the general population).
Smoking
Smoking was investigated in the individual patient data meta-analyses by the Asia Pacific Cohort Studies Collaboration [17] and the review by Feigin et al. [15]. Morita et al. had intended to investigate smoking, but were unable to do because insufficient data were available in the Japanese studies [14].
The Asia Pacific Cohort Studies Collaboration review categorised smoking into current versus not current, including former and never smokers in the latter [17]. The hazard ratio for current smoking compared to not was found to be 2.4 (95% CI 1.8 to 3.4).
The Feigin et al. [11] review used the following groups: never smoked, former smoker, current smoker and “not current” (i.e. former and never combined) and “ever” (i.e. former and current combined). Five longitudinal studies and 15 case control studies were included in the meta-analyses of smoking in this review and the authors concluded that there is a consistent, statistically significant association between smoking and increased risk of subarachnoid haemorrhage. Among the analyses they reported, current smoking compared to never smoking gave a relative risk of 2.2 (95% CI 1.3 to 3.6) for men and women combined, 2.2 (95% CI 1.7 to 2.8) for women and 2.2 (95% CI 1.7 to 3.0) for men in the longitudinal studies. In the case control studies, current smoking compared to never smoking had an overall odds ratio of 3.1 (95% CI 2.7 to 3.5), with an estimate of 2.4 (95% CI 1.4 to 4.0) for women and 5.2 (95% CI 3.0 to 9.0) for men.
Alcohol consumption
The relationship between alcohol consumption and subarachnoid haemorrhage was investigated in the Asia Pacific Cohort Studies Collaboration’s individual patient data meta-analyses [17] and by Feigin et al. [15].
The Asia Pacific Cohort Studies Collaboration review divided people into current versus not current alcohol drinkers. The latter included both people who had never drank alcohol and who had stopped drinking it [17]. Current alcohol consumption compared to not was found to have a hazard ratio of 1.0 (95% CI 0.7 to 1.4).
The Feigin et al. review sought to distinguish heavy drinkers, other alcohol drinkers and non-drinkers [15]. They divided users of alcohol into those drinking less than 150 g per week and those drinking 150 g or more per week. One standard drink was assumed to contain 12 g of alcohol. The authors concluded that excessive alcohol intake had a statistically significant and consistent association with an increased risk of subarachnoid haemorrhage. The data from five longitudinal studies produced relative risks for subarachnoid haemorrhage among people consuming less than 150 g/week compared to those taking no alcohol of 1.1 (95% CI 0.8 to 1.6) overall, 2.7 (95% CI 1.2 to 5.9) for women and 1.5 (95% CI 0.9 to 2.5) for men. The relative risks for the higher alcohol group (i.e. ≥150 g/week alcohol) compared with no alcohol were greater: 2.1 (95% CI 1.5 to 2.8) overall, 4.0 (95% CI 0.8 to 19.1) for women and 2.2 (95% CI 1.5 to 3.2) for men. In seven case control studies, the odds ratios for the group consuming <150 g/week alcohol compared with the group consuming no alcohol was 0.8 (95% CI 0.7 to 0.9) for all people, 0.6 (95% CI 0.4 to 1.0) for women and 0.5 (95% CI 0.3 to 0.8) for men. Again, subarachnoid haemorrhage was more common in the consumers of more alcohol, with odds ratios of 1.5 (95% CI 1.3 to 1.8) overall, 5.0 (95% CI 1.9 to 14.3) for women and 4.5 (95% CI 2.5 to 8.0) men when people who drank more than 150 g/week were compared with non-drinkers.
Use of aspirin
I identified one report of the relationship between aspirin use and subarachnoid haemorrhage. This had reviewed meta-analyses of the effects of the medium or long term use of aspirin as a treatment or preventative strategy for cardiovascular conditions on risks of subarachnoid and other cerebral haemorrhages [20]. No information was reported on the inclusion criterion for the review or how the studies had been searched for, and assessed for eligibility or inclusion. There was insufficient information in the report to distinguish between different types of stroke and so it is not possible to give an estimate of the risk of subarachnoid haemorrhage. However, the authors did conclude that there is an increased risk of intracranial haemorrhage with aspirin in both the primary and secondary prevention setting.
Use of oral contraceptive
I identified three systematic reviews that assessed the relationship between oral contraceptive use and subarachnoid haemorrhage. This relationship was the focus of one of these reviews [22]. The other two reports looked at a variety of risk factors, including oral contraceptives [15, 18]. I also found an earlier review, published in 1986 in German [21], but did not translate this fully because it preceded the work of the other reviews by several years and did not include a meta-analysis. It concluded “a critical review of the relevant literature revealed that the incidence of subarachnoid haemorrhage is increased in women taking oral contraceptives and the mortality rate is higher”.
The review dedicated to oral contraceptives, by Johnston et al., searched the medical literature from the introduction of oral contraceptives in 1960 using Index Medicus, MEDLINE and Dissertation Abstracts On-line, and checking references in relevant articles [22]. It included 11 independent studies, reported in 17 separate articles. A further ten articles were noted to have been excluded because the risk of subarachnoid haemorrhage could not be calculated from their reports. The meta-analysis produced a relative risk of 1.42 (95% CI 1.12 to 1.80, p = 0.004) for women using oral contraceptives, compared to those not using them.
The original Teunissen et al. review in 1996 combined five studies to produce a non-statistically significant estimate of an increased risk of subarachnoid haemorrhage for women using oral contraceptives [18]. The review was updated in 2005 [15], leading to the addition of some studies including one that had been published too recently for the aforementioned Johnston review [22], but some other studies in that review were not eligible. The longitudinal study had a relative risk for current users of oral contraceptives compared to the combination of never and former users of 5.4 (95% CI 0.7 to 43.5). The odds ratio from the case control studies was 0.8 (95% CI 0.5 to 1.3). The authors concluded that the use of oral contraceptive did not affect the risk of subarachnoid haemorrhage. They contrasted this with the Johnston et al. review [22], writing “our findings concerning the nonsignificant effect of oral contraceptives on the risk of SAH do not confirm the increased risk found in another meta-analysis devoted to only oral contraceptives and SAH. The reason for the discrepancy might be the less stringent study selection criteria (especially for the diagnosis of SAH) in the other review”.
Use of hormone replacement therapy
The Feigin et al. review examined the relationship between hormone replacement therapy use and subarachnoid haemorrhage [15]. They divided women into current and never or former users of hormone replacement therapy, and concluded that this therapy was associated with a reduction in the risk of subarachnoid haemorrhage. The one longitudinal study included in the review had a relative risk for current use versus never/former use of 0.6 (95% CI 0.2 to 1.5). The odds ratio from the two case control studies was 0.6 (95% CI 0.4 to 0.8).
Physical activity
Feigin et al. examined the relationship between regular vigorous exercise and subarachnoid haemorrhage [15]. They concluded that the evidence from the one longitudinal and two case control studies in the review was inconsistent. The relative risk from the longitudinal study was 0.5 (96% CI 0.3 to 1.0) for men taking regular rigorous exercise compared to men who took no regular rigorous exercise, whereas the two case control studies gave a combined odds ratio of 1.2 (96% CI 1.0 to 1.6) for men and women together.
I also identified a report written in Chinese, with an English abstract, in which Qiu and Meng summarised literature on exercise-related sudden death [23]. This could not be assessed in full but, in summary, the authors searched MEDLINE and the China Journal full-text database for 1993 to 2004 as well as some un-named journals. Their review was based on 16 articles: five reviews of exercise-related sudden death, seven investigations of sudden death, and four detailed accounts of cases of exercise-related sudden death. Deaths from cardiovascular disease, cerebral haemorrhage and subarachnoid haemorrhage are mentioned but there is insufficient information to estimate the risk for the relationship between exercise and subarachnoid haemorrhage.
HIV/AIDS
The Bulsara et al. report was a review of disparate cases associating HIV and AIDS with subarachnoid haemorrhage, describing each of 14 children that they had identified from nine separate papers [24]. This was a very different approach to the reviews of studies of case series or cohorts, which was typical of the other reviews in this systematic review; and no information was given on how the case reports had been searched for, assessed or selected for inclusion in the review. Furthermore, the review did not include a numerical estimate of the risk that people with HIV would develop an intracranial aneurysm or have this rupture or of the relative risks for people with HIV/AIDS compared to people without HIV/AIDS.
Family history
The Rinkel et al. review compared the risk of intracranial aneurysms in patients with a positive family history, those with autosomal dominant polycystic kidney disease, people screened because of a suspected pituitary adenoma, atherosclerosis, a brain tumour or other indications for angiography [13]. They had data on a total of 45 aneurysms in 476 patients with a family history of subarachnoid haemorrhage (prevalence 9.5%, 95% CI 7.0 to 12). Patients with a suspected pituitary adenoma or atherosclerosis were used as the reference standard in this review and the relative risk for patients with a family history compared to these was 4.0 (95% CI 2.7 to 6.0).
The Gieteling and Rinkel review mentioned family history in its study of autosomal dominant polycystic kidney disease (ADPKD) and subarachnoid haemorrhage [19]. They reported that a higher proportion of patients with ADPKD (40%) had a first or second degree relative with subarachnoid haemorrhage or intracranial aneurysm, compared to patients without ADPKD (14%).
Apolipoprotein E gene
Sudlow et al. examined the apolipoprotein E gene (APOE) in a broader review of stroke [20]. This covered ischemic stroke and intracerebral haemorrhage as well as subarachnoid haemorrhage, and found relatively few case control studies on subarachnoid haemorrhage. APOE is one of the most widely studied in vascular and neurogenerative diseases and produces a glycoprotein, apoE, which has three common isoforms. These are encoded by three alleles of the gene, ɛ2, ɛ3 and ɛ4. Genotypes that contain the ɛ4 allele (ɛ4+) are associated with higher cholesterol levels than the relatively common ɛ3/ɛ3 genotype, while ɛ2+ genotypes are associated with lower levels. Sudlow et al. included three studies (237 cases and 1,655 controls) relevant to subarachnoid haemorrhage and their meta-analyses found a small, statistically significant increase in the odds of being a case rather than a control for people with the ɛ4 allele (OR 1.42, 95% CI 1.01 to 1.99). Their meta-analysis for the ɛ2+ genotypes obtained a non-significant odds ratio of 1.14 (95% CI 0.75 to 1.76).
Time of day, weekday and season
Two reviews reported the relationship between either the time of day, day of the week, season, or a combination of these and subarachnoid haemorrhage.
Vermeer et al. searched MEDLINE from 1966 to 1995 and checked the reference lists of all publications for other articles [26]. They also included data from 422 subarachnoid haemorrhage patients that had been registered in their own database, at the Utrecht University Hospital, from 1989 and 1995. The authors pooled the data from ten identified studies with their own data to produce a dataset of 2,778 patients, which they examined in various time intervals on the 24-h clock. They concluded “our study shows that the risk of aneurysmal rupture is low during the night, starts to rise in the early morning, remains high during the day with a small nadir around noon, and decreases in the evening.” The authors used 12.00–18.00 as the reference standard, and found the relative risk for a subarachnoid haemorrhage during 00.00–06.00 to be 0.46 (95% CI 0.41 to 0.52) and, during 06.00–12.00, it was 1.2 (95% CI 1.1 to 1.3). A relative risk was not reported for 18.00–24.00 but it was said to be not statistically significant.
Feigin et al. investigated the relationships between time of day, weekday and season for subarachnoid haemorrhage [22]. They searched MEDLINE (from 1966) and EMBASE (from 1980) up to 2001. In their analyses of time of day, they studied four time periods (00.00–05.59, 06.00–11.59, 12.00–17.59 and 18.00–23.59). Three studies (1,148 patients) contributed to this meta-analysis giving a relative risk for subarachnoid haemorrhage of 3.19 (95% CI 3.03 to 3.36) during 06.00–11.59, 2.63 (95% CI 2.47 to 2.80) during 12.00–17.59 and 2.30 (95% CI 2.15 to 2.47) during 18.00–23.59; compared to the reference standard of 00.00–05.59.
The weekday of the subarachnoid haemorrhage was available for 829 patients in two studies in the Feigin et al. review [27]. They used Monday as the reference standard and they found one statistically significant relative risk: for Sunday. The relative risk for a subarachnoid haemorrhage on this day compared to Monday was 1.22 (95% CI 1.09 to 1.37). Vermeer et al. also studied the days of the week on which people had a subarachnoid haemorrhage. They wrote that they “did not find a preferred day of the week” for the onset of subarachnoid haemorrhage [26].
In the Feigin et al. review of seasons of the year, they used the following for studies from the northern hemisphere: June to August (summer), September to November (autumn), December to February (winter) and March to May (spring). For the southern hemisphere, they used December to February (summer), March to May (autumn), June to August (winter) and September to November (spring). Information on the season was available from six studies (2,046 patients), and summer was the reference standard. The relative risk for subarachnoid haemorrhage was 1.10 (95% CI 1.02 to 1.17) in winter and 1.07 (95% CI 1.01 to 1.13) in spring. The result for autumn was said to be not significantly different to summer.
Discussion
This systematic review of reviews of the relationship between risk factors and subarachnoid haemorrhage is based on literature searches done in the first half of 2006. It shows that the quality of these systematic reviews is generally good and it allows a summary of these risks to be made available in one place. Numerical estimates of the risks are given above, where these were available in the original reviews.
This systematic review of reviews might be subject to publication bias—in that the findings of the reviews that have been published might be systematically different to the results of any reviews that have been conducted but not published. The availability of a review for this report required that the original reviewers had written up and published their work, by the time of the searches in 2006, and that it had either been included in MEDLINE, PubMed or EMBASE, or referenced by one of articles checked while doing this review. It is possible, therefore, that some reviews were missed. However, this cannot be assessed in the absence of a prospective register of systematic reviews, such as those being compiled for randomised trials [3].
References
de Rooij NK, Linn FHH, van der Plas JA, Algra A, Rinkel GJE (2007) Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J NeurolNeurosurg Psychiat 78:1365–1372
Allen C, Clarke M, Tharyan P (2007) International activity in Cochrane Review Groups with particular reference to India. Natl Med J India 20:250–255
Moher D, Tetzlaff J, Tricco AC, Sampson M, Altman DG (2007) Epidemiology and reporting characteristics of systematic reviews. PLoS Medicine 4:e78
Dorhout Mees SM, van den Bergh WM, Algra A, Rinkel GJE (2007) Antiplatelet therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database of Systematic Reviews Issue 4. Art. no.: CD006184. DOI 10.1002/14651858.CD006184.pub2
Dorhout Mees SM, Rinkel GJE, Feigin VL, Algra A, van den Bergh WM, Vermeulen M, van Gijn J (2007) Calcium antagonists for aneurysmal subarachnoid haemorrhage. Cochrane Database of Systematic Reviews Issue 3. Art. no.: CD000277. DOI 10.1002/14651858.CD000277.pub3
Whitfield PC, Kirkpatrick PJ (2001) Timing of surgery for aneurysmal subarachnoid haemorrhage. Cochrane Database of Systematic Reviews, Issue 2. Art. no.: CD001697. DOI 10.1002/14651858.CD001697
Mulrow CD (1987) The medical review article: state of the science. Ann Intern Med 106:485–488
Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, Glanville J, Gray A, Harris A, Johnston K, Lodge M (2006) Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy. Health Technol Assess 10(34):1–204
Smith V, Devane D, Begley CM, Clarke M, Higgins S (2007) A systematic review and quality assessment of systematic reviews of fetal fibronectin and transvaginal cervical length for predicting preterm birth. Eur J Obstet Gynecol Reprod Biol 133(2):134–142
Pilkington K, Boshnakova A, Clarke M, Richardson J (2005) “No language restrictions” in database searches: what does this really mean. J Altern Complement Med 11:205–207
Edwards P, Clarke M, DiGuiseppi C, Pratap S, Roberts I, Wentz R (2002) Identification of randomized controlled trials in systematic reviews: accuracy and reliability of screening records. Stat Med 21:1635–1640
Linn FHHH, Rinkel GJE, Algra A, van Gijn J (1996) Incidence of subarachnoid hemorrhage. Stroke 27:625–629
Rinkel GJE, Djibuti M, Algra A, Van Gijn J (1998) Prevalence and risk of rupture of intracranial aneurysms: a systematic review. Stroke 29:251–256
Morita A, Fujiwara S, Hashi K, Ohtsu H, Kirino T (2005) Risk of rupture associated with intact cerebral aneurysms in the Japanese population: a systematic review of the literature from Japan. J Neurosurg 102:601–606
Feigin VL, Rinkel GJE, Lawes CMM, Algra A, Bennett DA, van Gijn J, Anderson CS (2005) Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke 36:2773–2780
Ruland S, Gorelick PB (2005) Stroke in black Americans. Curr Cardiol Rep 7:29–33
Feigin V, Parag V, Lawes CMM, Rodgers A, Suh I, Woodward M, Jamrozik K, Ueshima H (2005) Smoking and elevated blood pressure are the most important risk factors for subarachnoid hemorrhage in the Asia-Pacific region: an overview of 26 cohorts involving 306 620 participants. Stroke 36:1360–1365
Teunissen LL, Rinkel GJE, Algra A, Van Gijn J (1996) Risk factors for subarachnoid hemorrhage: a systematic review. Stroke 27:544–549
Gieteling EW, Rinkel GJE (2003) Characteristics of intracranial aneurysms and subarachnoid haemorrhage in patients with polycystic kidney disease. J Neurol 250:418–423
Gorelick PB, Weisman SM (2005) Risk of hemorrhagic stroke with aspirin use: an update. Stroke 36:1801–1807
Auff E, Zeiler K, Holzner F, Wimmer S, Deecke L (1986) The significance of oral contraceptive use as a risk factor in cerebrovascular disease. Wiener Klinische Wochenschrift 98:304–310
Johnston SC, Colford JM, Gress DR (1998) Oral contraceptives and the risk of subarachnoid hemorrhage: a meta-analysis. Neurology 51:411–418
Qiu N-M, Meng Z-Q (2005) Relationship between physical exercise and sudden death and the physiological mechanism. Zhongguo Linchuang Kangfu 9:160–161
Bulsara KR, Raja A, Owen J (2005) HIV and cerebral aneurysms. Neurosurg Rev 28:92–95
Sudlow C, Martinez Gonzalez NA, Kim J, Clark C (2006) Does apolipoprotein E genotype influence the risk of ischemic stroke, intracerebral hemorrhage, or subarachnoid hemorrhage? Systematic review and meta-analyses of 31 studies among 5961 cases and 17,965 controls. Stroke 37:364–370
Vermeer SE, Rinkel GJE, Algra A (1997) Circadian fluctuations in onset of subarachnoid hemorrhage: new data on aneurysmal and perimesencephalic hemorrhage and a systematic review. Stroke 28:805–808
Feigin VL, Anderson CS, Rodgers A, Bennett DA (2002) Subarachnoid haemorrhage occurrence exhibits a temporal pattern—evidence from meta-analysis. Eur J Neurol 9:511–516
Woo D, Broderick JP (2002) Spontaneous intracerebral hemorrhage: epidemiology and clinical presentation. Neurosurg Clin N Am 13:265–279
Acknowledgements
This systematic review of reviews was prepared as part of the @neurIST project, a European Union funded project (contract number FP6-IST-027703). I am grateful to the several people within @neurIST (www.aneurist.org) who commented on the documents as it was being prepared for that use. I am also grateful to Anne Eisinga at the UK Cochrane Centre who designed and ran the searches of PubMed and EMBASE.
Conflict of interest statement
I declare that I have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Professor Mike Clarke is Director of the UK Cochrane Centre, part of the international Cochrane Collaboration, which is the world’s largest organisation producing systematic reviews of the effects of healthcare interventions.
Rights and permissions
About this article
Cite this article
Clarke, M. Systematic review of reviews of risk factors for intracranial aneurysms. Neuroradiology 50, 653–664 (2008). https://doi.org/10.1007/s00234-008-0411-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-008-0411-9