Abstract
Introduction
Susceptibility-weighted imaging (SWI) is a novel magnetic resonance (MR) technique that exploits the magnetic susceptibility differences of various tissues, such as blood, iron and calcification. This pictorial review covers many clinical conditions illustrating its usefulness.
Methods
SWI consists of using both magnitude and phase images from a high-resolution, three-dimensional fully velocity-compensated gradient echo sequence. Phase mask is created from the MR phase images, and multiplying these with the magnitude images increase the conspicuity of the smaller veins and other sources of susceptibility effects, which is depicted using minimal intensity projection (minIP).
Results
The phase images are useful in differentiating between diamagnetic and paramagnetic susceptibility effects of calcium and blood, respectively. This unique MR sequence will help in detecting occult low flow vascular lesions, calcification and cerebral microbleed in various pathologic conditions and aids in characterizing tumors and degenerative diseases of the brain. This sequence also can be used to visualize normal brain structures with conspicuity.
Conclusion
Susceptibility-weighted imaging is useful in differentiating and characterizing diverse brain pathologies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Susceptibility-weighted imaging (SWI) is a novel magnetic resonance (MR) technique that exploits the magnetic susceptibility differences of various tissues, such as blood, iron and calcification [1]. It consists of using both magnitude and phase images from a high-resolution, three-dimensional (3D) fully velocity-compensated gradient echo sequence [2]. Phase mask is created from the MR phase images, and multiplying these with the magnitude images increases the conspicuity of the smaller veins and other sources of susceptibility effects, which is depicted using minimal intensity projection (minIP) [3].
The term susceptibility-weighted imaging has been used by various authors to indicate sequences that are sensitive to T2*gradient echo (GRE) techniques [4]; it has also been referred to as high-resolution (HR) blood oxygen level-dependent (BOLD) venography [1]. However, in this text, we use SWI to refer to the use of magnitude or phase images, or a combination of both, obtained with a 3D, fully velocity-compensated, gradient echo sequence. This 3D SWI can be used to visualize smaller veins and other sources of susceptibility effects, such as hemosiderin, ferritin and calcium.
In this article we highlight the various clinical applications of this relatively new MR technique.
Magnetic resonance imaging acquisition and image processing
Imaging was performed using a 12-channel phased array head coil on a 1.5 T clinical scanner (Avanto- SQ Engine; Siemens, Erlangen, Germany). The SWI sequence parameters were: TR (repetition time), 48 ms; TE (echo time), 40 ms; Flip angle, 20°; bandwidth, 80 kHz; slice thickness, 2 mm, with 56 slices in a single slab; matrix size, 512 × 256. A TE of 40 ms was chosen to avoid phase aliasing, and a flip angle of 20° was used to avoid nulling of the signal from pial veins located within the cerebral spinal fluid (CSF) [3]. The acquisition time was 2.58 min with the use of iPAT factor-2.
The first step was to remove incidental phase variations in the images due to static magnetic field inhomogeneity. We accomplished this by means of a homodyne processing of the phase images, which uses a low spatial frequency phase map generated from the raw data itself. The Hamming-filtered reconstructed phase images were then subtracted from the original phase images using complex division [2, 3, 5]. For paramagnetic substances, the increase in the magnetic field leads to a positive phase (for a left-handed MR system) relative to the surrounding parenchyma and CSF. As a second step, we created the phase mask and carried out unimodal signal processing. The phase mask was then multiplied with the magnitude data to enhance the visualization of vessels or microbleeds [2]. Finally, nine 12-mm thick minIP images were generated; these could be used to demonstrate tortuous structures and show the continuity of veins across slices. The entire image processing was automated and the phase, magnitude and minIP images were available on the main console.
Usefulness of SWI phase imaging
Phase changes induced by different tissues lead to good image contrast in phase imaging. Paramagnetic substances show positive phase shift in left-handed MR systems, such as the Avanto system of Siemens (Erlangen, Germany). Phase information requires no additional scan time but is an inherent part of an MR image. Rauscher et al. found after high pass filtering and phase unwrapping, phase images displayed small anatomic structures that are not easily visible on corresponding magnitude images, such as small veins, deep nuclei with increased iron content or even white matter, with superb contrast and resolution [6].
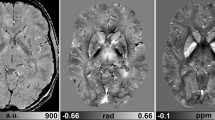
Calcification can be differentiated from hemorrhage based on differences in susceptibility effects – calcium is diamagnetic and blood products show largely paramagnetic susceptibility [6–9] (Fig. 1). This makes MR comparable to computed tomography (CT) in calcium imaging. However, one has to be very careful in inferring magnetic properties from visual image information since the phase patterns associated with these lesions are not only dependent on the susceptibility difference between tissues but also on the geometry of the lesion [10]. MinIP and filtered phase images of the midbrain (Fig. 2a, b) are able to clearly show mineralization of the red nucleus and the substantia nigra. Dentate nucleus mineralization is also best visualized in SWI images (Fig. 2c, d). Mineralization, iron and hemorrhage in the basal ganglia are also clearly visualized on phase images (Fig. 2e, f, 14). This may be useful in demonstrating and quantifying mineral deposition in various degenerative brain diseases.
Mineralizing microangiopathy in a young male patient. a Axial 7-mm-thick non-contrast, enhanced computed tomography (NECT) image showing the calcifications. b High-resolution T2 turbo spin echo (TSE) (TR/TE/TA = 5260 ms/106 ms/3.42 min, matrix = 384 × 384, nex = 4) demonstrating the ‘U’-shaped cortical calcifications in the depth of the sulcus (arrow). c–e Susceptibility-weighted imaging (SWI) – magnitude, phase and minimal intensity projection (minIP) images, respectively. The lesions are hypointense in all the images, suggesting diamagnetic susceptibility due to calcification (see text). Note also the detailed cerebral venous anatomy visualized in the minIP images (e)
a, b SWI minIP and phase images, respectively, through the midbrain of a middle-aged adult. Note the mineralization pattern in the red nucleus (RN), pars compacta (C) and reticulata (R) of the substantia nigra. c, d Similar sequence through the dentate nucleus of the cerebellum. e, f Same sequences at the level of the lentiform nucleus. Note the differential mineralization of the globus pallidus (thick arrow)
Susceptibility effects due to oxy- and deoxyhemoglobin
Hemoglobin (Hb) is the primary blood oxygen carrier and is composed of four protein (globin) subunits. Each protein subunit contains a heme molecule that contains an iron atom (Fe2+) surrounded by a porphyrin ring. Oxyhemoglobin is diamagnetic in nature, with no unpaired electrons, and generates magnetic fields that subtract from the external main magnetic field, whereas deoxy-Hb, being paramagnetic with four unpaired electrons, generates magnetic fields that additively combine with the external magnetic field [2]. This property forms the basis for ‘BOLD’ MR venographic imaging and can also be utilized for imaging the hemoglobin breakdown products.
Susceptibility effects due to non-heme iron and calcium
The major non-heme iron deposition in the human brain is in the form of ferritin [4]. Iron accumulation increases with age and is also observed in various neurodegenerative diseases. Iron is paramagnetic in nature and produces strong susceptibility effects while calcium, being diamagnetic, shows a lower susceptibility effect than iron [7].
Both calcification and iron accumulation in chronic hemorrhage appear as hypointense spots on T2-weighted images and will show a susceptibility effect on T2*imaging. It is not possible to differentiate between these two in conventional MR sequences, and CT is usually required for differentiation. Phase shift of the gradient echo represents an average magnetic field of protons in a voxel, which depends on the susceptibility of this tissues [8]. Yamada et al. showed the phase images to be sensitive to changes in the magnetic field caused by hematoma or calcification and that these differences can be used for differentiating the susceptibility among the tissues [9]. Susceptibility-weighted imaging, with its improved sensitivity in detecting susceptibility effects, can differentiate calcium from hemorrhage and iron deposition with increased sensitivity, as demonstrated in Fig. 1. Calcium is diamagnetic in nature, and the phase shift induced by calcification is opposite to that found with paramagnetic substances like deoxy-Hb, methemoglobin (Met-Hb), hemosiderin and ferritin [7]. Yamada et al. also found all basal ganglia calcifications to exhibit paramagnetic susceptibility and all calcifications outside the basal ganglia to have diamagnetic susceptibility [7]. They proposed that the paramagnetic susceptibility of basal ganglia calcifications might be due to the increased concentration of iron with aging. Gupta et al., in their study of 85 patients with intracranial calcifications and chronic hemorrhages using T2*GRE phase imaging, found the corrected gradient echo phase images to be useful in differentiating calcifications from chronic hemorrhages [8]
Calcification can be differentiated from the enhancing portions of the granuloma on the phase images (Fig. 3).
Calcified granuloma possibly tubercular in origin. a T2-weighted axial TSE (TR/ TE/ TA = 3010 ms/81 ms/2.29 min, matrix = 384 × 239, nex = 1) showing the hypointense lesions in the left frontal lobe with perilesional white matter edema. b NECT confirms the presence of calcified lesions with underlying edema. c SWI minIP images show the lesions to be hypointense with edema highlighted with a ‘FLAIR’ (fluid-attenuated inversion-recovery)-like contrast. d SWI phase images show the central calcified portions of the granuloma with diamagnetic susceptibility (hypointense) and the peripheral ring of hyperintensity (arrow), which probably represents paramagnetic deposits in the wall of the active granuloma. e Contrast-enhanced (CE) fat-suppressed axial T1-weighted SE (spin-echo) images (TR/TE/TA = 776 ms/11 ms/2.05 min, matrix = 256 × 156, nex = 1) showing the corresponding rim enhancement (arrow)
However, one should be aware of the possible limitations of this technique in differentiating calcium and blood, as discussed previously.
Blood oxygen level-dependent MR venography/small vessel imaging
The most widely used techniques for MR angiography (MRA) are time of flight (TOF) and phase-contrast MRA [11], with the former being sensitive to rapidly flowing spins and the latter representing the proton velocity map. Time of flight methods use the inflow of fresh unsaturated blood so that the vessels will appear bright compared with the surrounding tissue. They are usually flow compensated, whereas phase contrast methods are velocity-compensated. However, these methods have limitations in terms of their ability to visualize slow flow blood in small vessels.
Susceptibility-weighted imaging uses the paramagnetic deoxy-Hb as an intrinsic contrast agent [1]. Deoxyhemoglobin causes a reduction in T2* as well as a phase difference between the vessel and its surrounding parenchyma [12–14]. The T1 and T2 properties of blood are dependent on the oxygen saturation of the blood, hematocrit and the state of the red blood cells (RBCs) [2]. At 1.5 T, arterial blood has a T2* of approximately 200 ms, while 70%saturated venous blood has T2* of 100 ms. Hence, Long TEs will help in differentiating arteries from veins [15]. When the phase mask is multiplied with the magnitude images, the venous data is enhanced; when veins are not present, there is no change in the signal. The resultant images are displayed using the minimum intensity projection, highlighting the signal from veins and minimizing the signal of adjacent brain tissues [16]. Figures 1e and 2e demonstrate the ability of SWI to depict smaller caliber veins.
Vascular malformations
Developmental venous anomalies (venous angiomas), telangiectasias and cavernomas are low-flow vascular malformations that are less well imaged with conventional MR sequences. Spin-echo sequences are sensitive for imaging high-flow vessels, as evidenced by the flow void phenomenon, but they have reduced sensitivity in imaging small and low flow vessels. Magnetic resonance venography, such as two dimensional (2D) TOF or phase-contrast MRA, also depicts only large caliber vessels with a poor delineation of slow-flow vessels. The signal intensity of the TOF MRA also diminishes when the direction of blood flow is predominantly within the imaging plane [1]. All of these techniques are sub-optimal for malformed vessels, which exhibit slow multidirectional flow and cause reduced and variable enhancement. Small malformations can be missed entirely due to partial volume effects [1].
While the T2*GRE techniques with small voxel sizes can detect small venous structures, the magnitude and phase information of SWI offers improved sensitivity, revealing low-flow vascular malformations that are invisible on conventional GRE images [1, 17]; this is depicted in Fig. 4. In their study of ten patients, Lee et al. found SWI to be the ideal technique for screening patients with a high clinical suspicion of low-flow vascular malformations [17]. Reichenbach et al. also reported a similar result for developmental venous anomalies [18].
With the help of SWI, more cavernomas are identified that otherwise would not be visualized with conventional T2* techniques, as seen in Fig. 5. The visualization of more lesions may have clinical implications when surgical removal of the lesions for seizure control is being considered. Essig et al. showed SWI to be superior to conventional TOF MR angiography in detecting small arteriovenous malformations [19].
Venous thrombosis
Susceptibility-weighted imaging with both phase and magnitude information facilitates the detection of cortical venous thrombosis which are otherwise difficult to detect in conventional spin-echo T2 images. Lin et al. showed the differentiation of small patent venous structures originating from thrombosis using sequential pre- and post-contrast SWI and the phase pattern in SWI phase images [20]. Figure 6 demonstrates the usefulness of phase images in identifying thrombosed cerebral veins, especially the cortical veins and those of the deep system.
Venous sinus thrombosis. a, b Axial routine 2D GRE. Left temporal and bithalamic hemorrhage (thick arrows). Note the prominent left vein of Labbe, which is thrombosed (thin white arrow). c minIP- SWI showing the bithalamic bleed much more clearly. d) Axial phase image at the temporal region showing the thrombosed left vein of Labbe (thin white arrow) and the normal right vein of Labbe (thin black arrow) which are in opposite phases. Note also the left temporal hemorrhage (thick arrow). e Axial phase image at the thalamic level showing the thrombosed internal cerebral veins (thin white arrow) and the patent great vein of Galen (thin black arrow), which are also in opposite phases. f CE MR venography (V) showing the non-opacified internal cerebral veins
Brain tumors
Various imaging characteristics that have been suggested to be predictors of glioma grade in humans, including heterogeneity, contrast enhancement, mass effect, cyst formation or necrosis, metabolic activity and cerebral blood volume [21, 22]. In human glioma cells, the levels of ferritin and transferrin receptors detected during immunohistochemical analysis have been shown to correlate with tumor grade [23]. Bagley et al. found T2*-weighted GRE MR images to be valuable in the preoperative grading of gliomas due to the increased susceptibility artifacts caused by hemorrhages [24]. Seghal et al. found SWI to be equivalent to T1 contrast-enhanced (CE) images in the majority of cases studied and, in a few cases, to visualize the lesions better than T1 CE images [25]. These researchers also found an increased sensitivity of non-contrast SWI relative to non-contrast spin echo sequences. Christoforidis et al. have observed that the identification of microvascuarity in glioblastoma multiforme is facilitated due to the high resolution on the T2*GRE image in 8T MR [26]. Susceptibility-weighted imaging also provides FLAIR-like contrast because the CSF is suppressed while edema is enhanced relative to the normal tissue [3]. This unique contrast combination of T2* effects and edema within a single image allows for improved detection of space-occupying lesions, as shown in Fig. 7.
Susceptibility-weighted imaging is better able to define the internal architecture of the lesion in comparison to conventional MR sequences as well as to CE T1-weighted images [3]. Figure 8 illustrates the hemoglobin breakdown products within the tumor not detected in conventional images.
Hemorrhage can mimic neoplastic venous vasculature in a tumor due to the similar paramagnetic susceptibility effect produced by both. However, hemorrhage can be distinguished from veins if SWI is used both before and after the administration of the contrast agent [20]. Blood vessels change their signal intensity, but regions of inactive hemorrhage do not.
Phase images of SWI are needed to differentiate tumor vasculature from calcifications since both show hypointensity on minIP images. Calcium, being diamagnetic, shows negative phase (in left-hand MR systems) and is thereby hypointense in phase images. Tumor vasculature due to the presence of increased deoxy-Hb shows a paramagnetic effect with a resultant positive phase on phase SWI images, as demonstrated in Fig. 9.
Right frontal oligodendroglioma. a NECT. Note the calcified cortical based lesion (thick arrow). b Axial 2D GRE showing the calcification (thick arrow). c SWI minIP showing the calcification (thick arrow) and the peripheral vessel (thin arrow), both of which are hypointense. d CE fat-suppressed axial T1-weighted image showing the enhancing peripheral vein (thin arrow). e SWI – phase showing the calcification (thick arrow) and the deoxy-Hb in the peripheral vein (thin arrow) showing opposite phase information; consequently, the two will be differentiated
Susceptibility-weighted imaging can also differentiate intraaxial tumors from extraaxial tumors by demonstrating the shift of vessels around the mass, as seen in Fig. 10. SWI can also be used to differentiate acoustic schwanommas from cerebellopontine angle meningiomas with the improved detection of microhemorrhages within schwanommas, which are not observed in the meningiomas [27] (Fig. 11).
Trauma
About 10% of the CT-proven hematomas show no trace of hemosiderin on routine spin-echo MRI [28]. Diffuse axonal injury (DAI), a form of traumatic brain injury, is caused by shearing stress, primarily in the white matter [29]. The extent of axonal injury has been correlated with poor outcome [30]. Magnetic resonance imaging is more effective than CT in detecting and classifying injury patterns in DAI when hemorrhagic or non-hemorrhagic [31]. The presence of hemorrhage within the DAI indicates a poor prognosis when compared to lesions without hemorrhage [32]. T2*GRE images enable a better detection of the hemorrhage than conventional MRI techniques [33]. However, recent studies have demonstrated that SWI is more sensitive than GRE imaging for detecting suspected DAI [34]. Figure 12 demonstrates the utility of SWI in detecting punctuate hemorrhages in a patient with a history of trauma and altered sensorium.
Stroke
Acute infarct with or without hemorrhage occurs due to thromboembolism or atherosclerotic stenosis. Susceptibility-weighted imaging is exquisitely sensitive in detecting the presence or absence of hemorrhage within an infarct [35] (Fig. 13). Thromboembolism can also change susceptibility by decreasing arterial flow, thus increasing the amount of deoxy-Hb [36].
Left basal ganglia acute infarct. a Diffusion-weighted axial image showing the hyperintense acute infarct. b ADC map showing restricted diffusion. c TOF MRA showing occlusion of the left middle cerebral artery. d SWI minIP showing the early detection of microhemorrhages within the infarct (d, arrow), which is not shown by a CT taken at the same time (e)
The demonstration of bleed within the infarct may influence the subsequent treatment decisions. However, it is not clear at present whether detecting microbleeds within infarcts, which are not picked up by CT, will alter the management.
Cerebral microbleeds (CMB)
Cerebral microbleeds (CMB) are observed in various conditions, such as chronic systemic hypertension [37], cerebral amyloid angiopathy [38], cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) [39, 40 ], and in cases of cerebral vasculitis [41]. Computed tomography and conventional MR techniques usually fail to identify the cerebral microbleeds, which are, in contrast, well visualized in gradient T2*-weighted images [42]. Three-dimensional SWI, with its higher sensitivity, identifies numerous microbleeds (Figs. 14, 15) unidentified on routine gradient images.
Lesnik et al. found cerebral microbleeds in 31% of the symptomatic CADASIL mutation carriers, and they also identified that vascular risk factors, such as hypertension, do not account for the microbleeds [39]. Figure 15
Martin et al., in their study of 16 symptomatic patients with CADASIL, found a high frequency of microbleeds in CADASIL patients and showed cerebral microbleeds and T2-hyperintense ischemic lesions to be independent manifestations of the underlying angiopathy [40].
Subarachnoid hemorrhage and pial siderosis
Susceptibility-weighted imaging can demonstrate subacute and chronic subarachnoid hemorrhage, which are usually difficult to be identified with CT and/or conventional MR sequences. Susceptibility-weighted imaging reveals the pial staining of hemosiderrin and ferritin in chronic subarachnoid hemorrhage (SAH) not demonstrated even with FLAIR images, as shown in Fig. 16.
Neurodegenerative diseases
Increased iron deposition is found in Parkinson’s disease, Huntington’s disease, Alzheimer’s disease, multiple sclerosis, amyotropic lateral sclerosis and pantothenate kinase-associated neurodegeneration (PKAN) [43–46]. The capability to measure the amount of non-heme iron in the brain will facilitate a better understanding of the disease progression and will also help in predicting the treatment outcome. Minerals such as calcium (diamagnetic) and iron (paramagnetic) exert different degrees of susceptibility effects, thereby enabling SWI to be a more sensitive means of detecting mineral deposits (Fig. 17). Filtered phase images have been shown to be useful for observing the increased iron content in the brain [47]. However, in any one patient, it will be difficult to differentiate between normal and abnormal mineralization. Haacke et al. recently determined the baseline phase behavior patterns due to mineralization in various brain regions on SWI [48]. Further research is needed to determine its usefulness in differentiating between normal and abnormal mineral deposition in the human brain.
Multiple sclerosis
Multiple sclerosis is usually studied with FLAIR and CE T1 imaging. Susceptibility-weighted imaging can show the perivenular distribution of the demyelinating lesions [49]. Chronic lesions may show evidence of iron deposition within them, which may be better picked up by SWI than by conventional GRE.
High-resolution MR BOLD venography using T1-reducing contrast agent
Lin et al. [19] found a 26% reduction in data acquisition time while both maintaining the visibility of cerebral venous vessels and reducing the susceptibility artifacts with the use of T1-reducing contrast agent with the SWI. The TE can be reduced from 40 to 25 ms and the TR can be reduced from 57 to 42 ms, thus allowing for an overall time reduction in acquisitions. Reducing the TE minimizes the susceptibility artifacts induced by air-tissue interfaces; this reduction in TR decreases the overall time of acquisition.
High-field SWI
Reichenbach et al. observed an improved resolution and delineation of smaller vessels using high-field 3T MRI instead of low-field MRI [50]. The TE can also be reduced with high field strengths. A higher field strength has the advantage of obtaining images of superior spatial resolution in anatomical venous networks or pathological lesions, such as microbleeds and mineralization, compared to the 1.5T system. However, it is also important to recognize the potential artifacts on SWI at high field strengths due to their higher sensitivity to susceptibility effects. This disadvantage can be offset with optimized protocols; as such, high-field SWI appears to be the future – at least in brain imaging.
Conclusion
Susceptibility-weighted imaging appears to be a promising MR imaging sequence for delineating cerebral microvasculature and detecting foci of micro- and macrohemorrhages and low-flow vascular malformations. It also facilitates the characterization of cerebral tumors and degenerative cerebral diseases as well as the differentiation between calcification and bleed in the brain.
References
Reichenbach JR, Venkatesan R, Schillinger DJ et al (1997) Small vessels in the human brain. MR venography with deoxyhemoglobin as an intrinsic contrast agent. Radiology 204:272–277
Reichenbach JR, Haacke EM (2001) High-resolution BOLD venographic imaging: a window into brain function. NMR Biomed 14:453–467
Seghal V, Delproposto Z, Haacke EM et al (2005) Clinical application s of neuroimaging with susceptibility-weighted imaging. J Magn Reson Imaging 22:439–450
Liang L, Korogi Y, Sugahara T, Shigematsu Y, Okuda T, Ikushima I, Takahashi M (1999) Detection of intracranial hemorrhage with susceptibility-weighted MR sequences. AJNR Am J Neuroradiol 20:1527–1534
Wang Y, Yu Y, Li D et al (2000) Artery and vein separation using susceptibility-dependent phase in contrast enhanced MRA. J Magn Reson Imaging 12:661–670
Rauscher A, Sedlacik J, Barth M, Haacke EM, Reichenbach JR et al (2005) Magnetic susceptibility-weighted MR phase imaging of the human brain. AJNR Am J Neroradiol 26:736–742
Yamada N, Imakita S, Sakuma T et al (1996) Intracranial calcification on gradient -echo phase image:Depiction of Diamagnetic susceptibility. Radiology 198:171–178
Gupta RK, Rao SB, Rajan J et al (2001) Differentiation of calcification from chronic hemorrhage with corrected gradient echo phase imaging. J Comput Assist Tomogr 25:698–704
Yamada N, Imakita S, Sakuma T et al (1990) Evaluation of the susceptibility effect on the phase images of a simple gradient echo. Radiology 175:561–565
Deistung A, Mentzel HJ, Rauscher A, Witoszynskyj S, Kaiser WA, Reichenbach JR (2006) Demonstration of paramagnetic and diamagnetic cerebral lesions by using susceptibility weighted phase imaging (SWI). Z Med Phys 16:261–267
Dumoulin CL, Hart HJ (1986) Magnetic resonance angiography. Radiology 161:717–720
Thulborn KR, Waterton JC, Matthews PM et al (1982) Oxygenation dependence of the transverse relaxation time of water protons in whole blood at high field. Biochim Biophys Acta 714:265–270
Li D, Waight DJ, Wang Y (1998) In vivo correlation between blood T2* and oxygen saturation. J Magn Reson Imaging 8:1236–1239
Gomori JM, Grossman RI, Yu-Ip C et al (1987) NMR relaxation times of blood: dependence on field strength, oxidation state, and cell integrity. J Comput Assist Tomogr 11:684–690
Haacke EM, Satin W (1993) Fast imaging and vessel contrast. In: Potchen EJ, Haacke EM, Siebert JE, Gottaschalk A (eds) Magneticresonanceangiography. Mosby, St. Louis, pp 46–51
Reichenbach JR, Venkatesan R, Yablonsky DA et al (1997) Theory and application of static field inhomogenity effects inn gradient echo imaging. J Magn Reson Imaging 7:266–279
Lee BCP, Vo KD, Kido DK et al (1999) MR high resolution blood oxygenation level dependent venography of occult (low-flow) vascular lesions. AJNR Am J Neuroradiol 20:1239–1242
Reichenbach JR, Jonetz-Mentzel L, Fitzek C et al (2001) High resolution blood oxygen-level dependent MR venography. Neuroradiology 43:364–369
Essig M, Reichenbach JR, Schad JR et al (1999) High resolution MR venography of cerebral arteriovenous malformations. Magn Reson Imaging 17:1417–1425
Lin W, Mukherjee P, An H et al (1999) Improving high resolution MR bold venographic imaging using a T1 reducing contrast agent. J Magn Reson Imaging 10:118–123
Dean Bl, Drayer BP, Bird CR, Flora RA, Hodak JA, Coons SW, Carey RG (1990) Gliomas:classification with MR imaging. Radiology 174:411–415
Ding B, Ling HW, Chen KM, Jiang H, Zhu YB (2006) Comparison of cerebral blood volume and permeability in preoperative grading of intracranial glioma using CT perfusion imaging. Neuroradiology 48:773–781
Recht L, Torres CO, Smith TW et al (1990) Transferrin receptor in normal and neoplastic brain tissue :implications for brain tumor immunotherapy. J Neurosurg 72:941–945
Bagley L, Grossman RI, Judy KD et al (1997) Gliomas: correlation of magnetic susceptibility artifact with histologic grade. Radiology 202:511–516
Seghal V, Delproposto Z, Haddar D et al (2006) Susceptibility-weighted imaging to visualise blood products and improve tumor contrast in the study of brain masses. J Magn Reson Imaging 24:41–51
Christoforidis GA, Kangarlu A, Abduljalil AM et al (2004) Susceptibility-based imaging of glioblastoma Microvascularity at 8T.: correlation of MR imaging and postmortem pathology. AJNR Am J Neuroradiol 25:756–760
Krishnamoorthy T, Radhakrishnan VV, Thomas B et al (2006) Microhemorrhages in vestibular schwannomas: prospective study with T2* weighted gradient-echo sequence. In: Proc Am Soc Neurorad (ASNR). San Diego, USA
Wardlaw JM, Statham PF (2000) How often is haemosiderin not visible on routine MRI following traumatic intracerebral haemorrhage? Neuroradiology 42:81–84
Gentry LR, Godersky JC, Thompsonn B (1988) MR imaging of head trauma:review of the distribution and radiopathologic features of traumatic lesions. AJR Am J Roentgenol 150:663–672
Medana IM, Esiri MM (2003) Axonal damage: a key predictor of outcome in human CNS diseases. Brain 126:515–530
Orrison WW, Gentry LR, Stimac GK et al (1994) Blinded comparison of cranial CT and MR in closed head injury evaluation. AJNR Am J Neuroradiology 15:351–356
Paterakis K, Karantanas AH, Komnos A et al (2000) Outcome of patients with diffuse axonal injury: the significance and prognostic value of MRI in the acute phase. J Trauma 49:1071–1075
Atlas SW, Mark AS, Grossman RI et al (1988) Intracranial Hemorrhage: gradient echo MR imaging at 1.5 T.-comparison with spin echo imaging and clinical applications. Radiology 168:803–807
Tong KA, Ashwal S, Holshouer B et al (2003) Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: improved detection and initial results. Radiology 227:332–339
Wycliffe ND, Chose J, Holshouser B et al (2004) Reliability in detection of hemorrhage in acute stroke by a new three-dimensional gradient recalled echo susceptibility-weighted imaging technique compared to computed tomography: a retrospective study. J Magn Reson Imaging 20:372–377
Mammen EF (1992) Pathogenesis of venous thrombosis. Chest 102:640s–644s
Kidwell CS, Saver JL, Villablanca JP et al (2002) Magnetic resonance imaging detection of microbleeds before thrombolysis:an emerging application. Stroke 33:95–98
Greenberg SM, O’Donnel HC, Schaefer PW et al (1999) MRI detection of new hemorrhages:potential marker of progression in cerebral amyloid angiopathy. Neurology 53:1135–1138
Lesnik OAJ, Van Den Boom R, Van buchem A et al (2001) Cerebral microbleeds in CADASIL. Neurology 57:1066–1070
Martin D, Makus H, Jurgen H et al (2002) Cerebral microbleeds in CADASIL: a gradient echo MRI and autopsy study. Stroke 33:67–71
Campi A, Benndorf G, Filippi M, Reganati P, Martinelli V, Terreni MR (2001) Primary angiitis of the central nervous system: serial MRI of brain and spinal cord. Neuroradiology 43:599–607
Gerrnberg SM, Finklestein SP, Schaefer et al (1996) Petechial hemorrhages accompanying lobar hemorrhage:detection by gradient echo MRI. Neurology 46:1751–1754
Bartzokis G, Tishler TA (2000) MRI evaluation of basal ganglia ferritin iron and neurotoxicity in Alzheimers and huntingtons disease. Cell Mol Biol 46:821–833
Bartzokis G, Cummins J, Markham Ch et al (1999) MRI evaluation of brain iron in earlier and later onset Parkinsons disease and normal subjects. Magn Reson Imaging 17:213–222
Hecht MJ, Fellner C, Schmid A, Neundorfer B, Fellner FA (2005) Cortical T2 signal shortening in amyotrophic lateral sclerosis is not due to iron deposits. Neuroradiology 47:805–808
Vymazal J, Righini A, Brooks RA et al (1999) T1 and T2 in the brain of healthy subjects,patients with Parkinson disease and patients with multiple system atrophy: relation to iron content. Radiology 211:489–495
Ogg RJ, Langston JW, Haacke EM et al (1999) The correlation between phase shifts in gradient-echo MR images and regional brain iron concentration. Magn Reson Imaging 17:1141–1148
Haacke EM, Ayaz M, Khan A, Manova ES, Krishnamurthy B, Gollapalli L, Ciulla C, Kim I, Petersen F, Kirsch W (2007) Establishing a baseline phase behavior in magnetic resonance imaging to determine normal vs. abnormal iron content in the brain. J Magn Reson Imaging 26:256–264
Tan IL, van Schijndel RA, Pouwels PJ, van Walderveen MA, Reichenbach JR, Manoliu RA, Barkhof F (2000) MR venography of multiple sclerosis. AJNR Am J Neuroradiol 21:1039–1042
Reichenbach JR, Barth M, Haacke M et al (2000) High-resolution MR venography at 3.0 tesla. J Comput Assist Tomogr 24:949–957
Acknowledgements
We thank Siemens Medical Systems for providing with the SWI sequence and the post-processing tools. We also thank the Director, SCTIMST, for the permission to publish this paper.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, B., Somasundaram, S., Thamburaj, K. et al. Clinical applications of susceptibility weighted MR imaging of the brain – a pictorial review. Neuroradiology 50, 105–116 (2008). https://doi.org/10.1007/s00234-007-0316-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-007-0316-z