Abstract
We describe the use of a combination of fat-suppression SPIR (spectral inversion recovery) and subtraction FLAIR imaging to aid in detection of abnormal meningeal enhancement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
FLAIR images have an inherent component of T1-weighting [1] that enables visualization of contrast enhancement, and FLAIR has been shown to be particularly sensitive in detecting leptomeningeal contrast enhancement [2–4], related to the T1-shortening effect of gadolinium, slow-flowing superficial vessels, and probably even magnetization transfer effects [2]. SPIR imaging can be used in conjunction with FLAIR for fat suppression of signal within the skull base, scalp, cavernous sinus, and orbits [5, 6], and may result in more homogeneous fat suppression than that typically obtained with conventional T1-weighted (T1-W) images, since the inversion time selected relates to the null point (T1 recovery time) of fat, rather than the precessional frequency [7]. Additionally, subtraction techniques, which involve subtracting the precontrast from the postcontrast image, have been proposed to detect abnormal contrast enhancement on T1-W images underlying hyperintense hemorrhage [8]. A similar concept could be applied to FLAIR sequences, where fat-suppressed SPIR/FLAIR techniques could help delineate abnormal meningeal enhancement, and the subtraction technique could aid in detection of meningeal enhancement in the midst of underlying sulcal hyperintensities present on noncontrast FLAIR.
Technique and representative cases
A group of 15 patients with a high clinical suspicion for meningitis were studied by 22 MR examinations. Sequences included pre- and postcontrast T1-W gradient echo (flip angle 80–90°), and fat-suppressed SPIR/turboFLAIR imaging. Sequences were obtained with 1.5 and 3.0-T magnets, with turboFLAIR sequence parameters: TR/TE/TI 6,500/105/2,000 ms, NEX 2, turbo factor 18, slice thickness 5 mm, gap 1 mm, matrix 256×256. The patients were not moved between the pre- and postcontrast imaging, facilitated by long intravenous tubing, with a 1–2 min delay between pre- and postcontrast imaging. SPIR fat suppression added 5–10 s to the prescan phase, but no additional time during image acquisition. Subtraction was obtained within 1–2 min via postprocessing performed immediately after completing the examination, at the technologist’s workstation, by selecting the subtraction operation, and subtracting the axial turboFLAIR precontrast from the corresponding postcontrast sequence. The technologist instructed the patients to remain still throughout each sequence.
Two staff neuroradiologists jointly reviewed the images to confirm whether abnormal sulcal or dural signal was present on FLAIR or T1-W images prior to and after intravenous contrast administration, or on the subtracted images, and whether or not the subtraction images were interpretable. On the contrast-enhanced FLAIR and subtraction images, the choroid plexus, nasal mucosa, cavernous sinus, pituitary stalk, pineal enhancement, and the occasional cortical venous enhancement were considered normal [9]. Meningitis was confirmed by direct biopsy (n=3) or CSF culture (n=4) in seven patients, with one patient having septic emboli. Other abnormalities included dural lymphoma, vasculitis, tumor, intracranial hypotension, and an unknown cause of leptomeningeal enhancement that spontaneously resolved; the remaining two patients had negative MRI and did not develop meningitis.
Prior to intravenous contrast administration, 12 of the 22 examinations showed abnormal sulcal hyperintensity on precontrast SPIR/FLAIR images (Fig. 1), with leptomeningeal enhancement on 12 postcontrast SPIR/FLAIR images (Fig. 2), and 9 postcontrast T1-W images. Based on only the initial scan, the sensitivity and specificity, respectively, of the sequences for patients with proven meningitis were as follows: 71% (5/7) and 75% (6/8) for noncontrast SPIR/FLAIR imaging, 57% (4/7) and 75% (6/8) for postcontrast SPIR/FLAIR imaging, and 43% (3/7) and 75% (6/8) for postcontrast T1-W imaging. SPIR/FLAIR and T1-W imaging showed equivalent detection of dural enhancement, which was present in 10 of the 22 examinations.
Meningitis from Klebsiella pneumoniae, with sulcal hyperintensity that does not enhance after subtraction of fat-suppressed SPIR/FLAIR images. Images from a 3.0-T scanner demonstrate diffuse hyperintense signal (arrows) throughout the cerebral sulci on FLAIR images before (a, b) and after (c) contrast administration. Subtraction images do not demonstrate any meningeal enhancement (d, e; arrows). No meningeal enhancement is noted on the post-contrast T1-W image (f). Also note the normal nasal mucosa and cavernous sinus enhancement, and that the typical CSF flow-related artifact in the prepontine cistern is mostly removed after subtraction (d, dashed arrow)
Abnormal leptomeningeal enhancement demonstrated on repeat subtraction imaging in a 16-year-old patient with viral meningitis. Initial 3.0-T MR imaging demonstrates subtle sulcal hyperintensity on pre- and post-contrast turboFLAIR images (after contrast administration: a, black arrows), with no abnormal contrast enhancement on subtraction images (b) or on contrast-enhanced T1-W images (not shown). Note the normal enhancement of the choroid plexus (b, arrows). This was interpreted as suspicious for mild exudates in the clinical setting of meningitis, without abnormal contrast enhancement. CSF protein was mildly elevated, but lumbar puncture cultures were negative. The patient’s symptoms progressed, and repeat imaging 5 days later on the same scanner demonstrated slightly more prominent sulcal hyperintensity on pre- and postcontrast FLAIR imaging (not shown), but new, mild pial enhancement is seen on the subtraction sequence (c, arrows), more prominent on the left, also confirmed on postcontrast coronal T1-W images (d)
Three of the 22 subtractions were considered inadequate, and two were considered equivocal, but interpretable, related to what the authors term “pseudo-enhancement,” a low-level hyperintensity on the subtraction images that was non-vascular and completely followed the sulcal contour (Fig. 3). Subtraction sequences were positive for pial enhancement in 11 MRIs in six patients who had sulcal hyperintensities on pre- and postcontrast images (Fig. 2) in the setting of adequate subtraction. In addition, the subtraction images eliminated unwanted flow artifact on FLAIR images present in the prepontine and basal cisterns, as demonstrated in a patient with tuberculous meningitis (Fig. 3). Regarding dural enhancement, subtraction was adequate in nine of ten MRI scans (in seven patients with dural enhancement), but was of limited use since the enhancement was usually discernible on both SPIR/FLAIR and T1-W images. The exception was a late subacute subdural hematoma, hyperintense on precontrast T1-W and FLAIR images, with an enhancing rim on subtraction images.
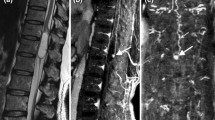
Subtraction FLAIR fat-suppressed images obtained on a 3.0-T MR scanner demonstrate basilar leptomeningeal enhancement in a 37-year-old female with tuberculous meningitis. Noncontrast FLAIR images (a) from the initial scan demonstrate mild prepontine hyperintensity (arrow), which is a common site of CSF-related flow artifact; the area is more hyperintense on the postcontrast image (b, arrow). Subtraction FLAIR images (c) show the underlying contrast enhancement in the prepontine cistern and surrounding the brain stem (arrows), and posteriorly along the cerebellum, also noted to a lesser degree on T1-W images (d). Postcontrast FLAIR images at a higher level demonstrate mild leptomeningeal enhancement (e, solid arrow), while subtraction images show that mild motion causes a subtle “pseudo-“ leptomeningeal hyperintensity (f, dashed arrows), where no sulcal abnormality is present on postcontrast FLAIR (e, dashed arrows), which is discernible from true leptomeningeal enhancement on the right (e, f; solid arrows). Also note that enhancement does not normally occur of the major dural venous sinuses on FLAIR images, but does occur on T1-W images
Discussion
Both leptomeningeal and pachymeningeal abnormalities were well demonstrated on the pre- and postcontrast SPIR/FLAIR images, and in a majority of the subtracted images. Preliminarily, fat-suppressed FLAIR imaging seemed at least equivalent to T1-W imaging in detecting abnormal pial or dural enhancement, but the gradient-echo T1-W imaging used in 13 examinations at 3.0 T in this study may have less contrast-to-noise ratio and enhancement than conventional spin-echo T1-W imaging [10]. Controversy exists as to whether postcontrast T1-W or FLAIR images are more sensitive for leptomeningeal disease [3, 4, 11], which could be addressed by a larger, prospective study of fat-suppressed T1-W versus SPIR/FLAIR imaging.
The subtraction technique was performed with minimal postprocessing time, in a manner identical to that commonly used for postcontrast neck MR angiography, which is readily available on most commercial scanners. The pitfall of the technique appears to be either mild patient motion or CSF pulsation. Although the patients held relatively still, in some patients there appeared to be mild translation between pre- and postcontrast sequences, and sulcal signal possibly related to brain/CSF motion, or expansion-contraction related to cardiac systole [12]. This occurred in four of the first six MR scans in this study where the postcontrast T1-W imaging was performed prior to FLAIR, improving in most of the subsequent examinations where the FLAIR sequence was performed as the last precontrast and the first postcontrast sequence. In the near future, alternative techniques such as PROPELLER (periodically rotated overlapping parallel lines with enhanced reconstruction [13, 14]), or a recently developed adaptive motion autocorrection algorithm [15], could correct for patient motion, but these techniques are not yet routinely available with most commercial scanners.
References
Hendrick RE, Raff U (1992) Image contrast and noise. In: Stark DD, Bradley WG (eds) Magnetic resonance imaging, 2nd edn. Mosby-Yearbook, St. Louis, pp 123–129
Mathews VP, Caldemeyer KS, Lowe MJ, Greenspan SL, Weber DM, Ulmer JL (1999) Brain: gadolinium-enhanced fast fluid-attenuated inversion-recovery MR imaging. Radiology 211:257–263
Splendiani A, Puglielli E, Amicis RD, Necozione S, Masciocchi C, Gallucci M (2005) Contrast-enhanced FLAIR in the early diagnosis of infectious meningitis. Neuroradiology 47:591–598
Tsuchiya K, Katase S, Yoshino A, Hachiya J (2001) FLAIR MR imaging for diagnosing intracranial meningeal carcinomatosis. AJR Am J Roentgenol 176:1585–1588
Jackson A, Sheppard S, Laitt RD, Kassner A, Moriarty D (1998) Optic neuritis: MR imaging with combined fat- and water-suppression techniques. Radiology 206:57–63
Jackson A, Sheppard S, Johnson AC, Annesley D, Laitt RD, Kassner A (1999) Combined fat- and water-suppressed MR imaging of orbital tumors. AJNR Am J Neuroradiol 20:1963–1969
Westbrook C, Kaut-Roth C, Talbot J (2005) MRI in practice, 3rd edn. Blackwell, Oxford, pp 217–226
Melhem ER, Mehta NR (1999) Dynamic T1-weighted spin-echo MR imaging: the role of digital subtraction in the demonstration of enhancing brain lesions. J Magn Reson Imaging 9:503–508
Goo HW, Choi CG (2003) Post-contrast FLAIR MR imaging of the brain in children: normal and abnormal intracranial enhancement. Pediatr Radiol 33:843–849
Fischbach F, Bruhn H, Pech M, Neumann F, Ricke J, Felix R, Hoffmann KT (2005) Efficacy of contrast medium use for neuroimaging at 3.0 T: utility of IR-FSE compared to other T1-weighted pulse sequences. J Comput Assist Tomogr 4:499–505
Galassi W, Phuttharak W, Hesselink JR, Healy JF, Dietrich RB, Imbesi SG (2005) Intracranial meningeal disease: comparison of contrast-enhanced MR imaging with fluid-attenuated inversion recovery and fat-suppressed T1-weighted sequences. AJNR Am J Neuroradiol 26:553–559
Feinberg DA, Mark AS (1987) Human brain motion and cerebrospinal fluid circulation demonstrated with MR velocity imaging. Radiology 163:793–799
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
ForbesKP, Pipe JG, Bird CR, Heiserman JE (2001) PROPELLER MRI: clinical testing of a novel technique for quantification and compensation of head motion. J Magn Reson Imaging 14:215–222
Manduca A, McGee KP, Welch EB, Felmlee JP, Grimm RC, Ehman RL (2000) Autocorrection in MR imaging: adaptive motion correction without navigator echoes. Radiology 215:904–909
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McKinney, A., Palmer, C., Short, J. et al. Utility of fat-suppressed FLAIR and subtraction imaging in detecting meningeal abnormalities. Neuroradiology 48, 881–885 (2006). https://doi.org/10.1007/s00234-006-0145-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-006-0145-5