Abstract
We evaluated prospectively the relation between packing and reopening in coiled intracranial aneurysms. Packing, defined as the ratio between the volume of inserted coils and volume of the aneurysm expressed as percentage, was calculated for 82 intracranial aneurysms treated with detachable coils. Aneurysm volume was assessed from 3D angiography. Reopening of the aneurysmal lumen at the 6-month follow-up angiography was dichotomized into present or absent. We assessed whether packing above 24% protected against reopening. Twenty-three of 82 aneurysms (28%) showed reopening. Reopening was caused by compaction in 20 aneurysms and by partial thrombosis, undetected at the time of initial treatment in three aneurysms. Three of 29 aneurysms (10%) with a packing of more than 24% showed reopening. These three aneurysms contained partially intraluminal thrombosis undetected at the time of treatment. We conclude that in coiled intracranial aneurysms packing above 24% protects against reopening by compaction in non-thrombosed aneurysms. Since intraluminal thrombosis may go undetected at the time of treatment, follow-up angiography is still warranted in aneurysms with packing densities greater than 24%.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coiling of intracranial aneurysms has proven to be a safe and effective treatment with low procedural risks and good clinical results [1–3]. However, approximately 25% of coiled aneurysms show reopening of the lumen over time because of compaction or migration of coil mesh into the intraluminal thrombus [3–6]. A previous study showed that packing density, defined as the volume of inserted coils expressed as a percentage of the aneurysm lumen volume, above 24% protects against reopening [7]. However, in this paper, six aneurysms were excluded because of partial thrombosis undetected at the time of initial treatment. Partial thrombosis in these aneurysms was only detected on follow-up angiography 6 months later: reopening of the aneurysm lumen was predominantly caused by translation of a largely unchanged coil mesh rather than the compaction of coils.
In the present study we assessed prospectively whether aneurysms packed for more than 24% remain stable on follow-up angiography.
Patients and methods
Patients
Between October 2001 and December 2002, 132 intracranial aneurysms in 123 consecutive patients were coiled. Thirty patients with 30 aneurysms did not have follow-up angiography for the following reasons: 20 patients had died (procedural death: 3; sequelae of subarachnoid hemorrhage 16; unrelated death: 1). Four patients underwent surgical clipping or parent vessel occlusion after incomplete initial coiling, and six patients declined follow-up angiography. In the remaining 102 aneurysms in 93 patients, 20 aneurysms were excluded for the purpose of this study. We excluded five aneurysms in which partial intrasaccular thrombosis was obvious before treatment on CT or MRI, three aneurysms coiled after failed clipping because volume measurement was hindered by the clip and one patient with a dissecting aneurysm was excluded. Three patients with procedural aneurysm rupture were excluded as coils were placed outside the aneurysmal sac. In five patients with six aneurysms, the 3D data were lost. In one patient, no 3D angiography was performed, and in one patient the 3D angiogram was of inferior quality.
The present study group consists of 76 patients with 82 coiled aneurysms. There were 61 women and 21 men with a mean age of 51.9 years (median 51, range 25–81). Of the 82 aneurysms, 62 had ruptured and 20 had not. Eleven of 20 unruptured aneurysms were additional aneurysms, seven were truly incidental and two presented with symptoms of mass effect. The location of the aneurysms was as follows: anterior communicating artery, 26; posterior communicating artery, 17; basilar tip, 10; posterior cerebral artery,6; ophthalmic artery,4; carotid bifurcation,4; middle cerebral artery,4; pericallosal artery,3; posterior inferior cerebellar artery,2; hypophyseal segment of the carotid artery,2; vertebral artery,2; superior cerebellar artery,1; anterior choroidal artery,1. Estimation of maximum diameter classified 62 aneurysms as small (<10 mm) and 20 aneurysms as large (>10 mm). The median angiographic follow-up interval was 6 months.
Methods
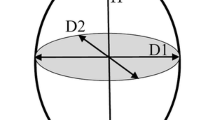
Coiling of aneurysms was performed on a biplane angiographic unit (Integris BN 3000, Philips Medical Systems, Best, The Netherlands) with the use of general anaesthesia and systemic administration of heparin. Intravenously or subcutaneously administered heparin was continued for 48 h after the procedure, followed by orally administered aspirin for 3 months. The aim of coiling was to pack the aneurysm as densely as possible. Coiling was performed with Guglielmi Detachable Coils (GDC-10 and/or 18, all types, Boston Scientific, Fremont, CA). Prior to the coiling procedure a rotational angiography with a 17-cm image intensifier was made. A magnification of 33% of the initial 3D dataset was reconstructed in a matrix of 2563 . In this magnified reconstruction the aneurysm was manually segmented and the volume was calculated using the manufacturer’s software.
The volume of the coils was calculated from the volume per centimeter for each type of coil. Packing was calculated as the ratio of coil volume and aneurysm volume×100%.
At the 6-month follow-up, angiography results were dichotomized into the absence or presence of reopening. This was done by two authors (WR and MSlu) in consensus, without prior knowledge of the initial packing density. In aneurysms showing reopening, the cause was determined to be either compaction or coil mesh migration into intraluminal thrombus. Compaction was defined as a decrease in volume of the coil mesh and more contrast filling of the aneurysm compared to the immediate post-embolization angiogram. Reopening of the aneurysm and translation of a largely unchanged coil mesh were considered to be the result of migration of the coil mesh into the intraluminal thrombus.
Results
The packing densities versus aneurysm volumes are displayed graphically in Fig. 1. The mean volume of the 82 aneurysms was 199.5 mm3 (median 53.5, range 8–3630 mm3). The mean packing density was 22.8% (median 21.6, range10.6–65.0%). At the 6-month follow-up angiography, 23 of 82 aneurysms (28%) showed reopening. In 20 of these 23 aneurysms reopening was assessed as being caused by compaction of the coil mesh and three by migration of a largely unchanged coil mesh into the thrombus. The overall mean packing density of stable aneurysms was 24.1% (median 23.6, range 11.3–65%) and of reopened aneurysms 19.6% (median 20.1, range 10.6–29.3%).
Three of 29 aneurysms (10%) with packing of more than 24% showed reopening of the lumen of the aneurysm. These were the three aneurysms that showed a translation of the coil mesh, presumably caused by initially undetected intraluminal thrombosis. The remaining 26 aneurysms packed for more than 24% showed stable occlusion. Of the 53 aneurysms packed for less than 24%, 20 (38%) showed reopening of the aneurysmal lumen assessed as being caused by compaction of the coils.
Discussion
In this prospective study we confirmed our previous finding that coiled aneurysms packed above 24% do not show reopening caused by compaction of the coil mesh [7]. However, reopening of aneurysms caused by migration of the coil mesh into the intraluminal thrombus could not be excluded in patients whose aneurysm packing density was above 24% and, therefore, follow-up angiography is indicated in these aneurysms. This is in concordance with a previously published retrospective study in which the partial thrombosis and reopening of 6 of 145 (4%) aneurysms were only detected after the 6-month follow-up angiography [8]. Because reopening in aneurysms with high packing densities is unlikely, it may be justifiable to carry out the follow-up in these patients using less sensitive but non-invasive methods such as MRA [9] or CTA. In addition, the close relationship between high packing density and stability in aneurysms that do not contain thrombosis is potentially important in studies comparing the performance of different types of newly developed coils [10–12]. If it can be shown that higher packing densities can be achieved by using a particular type of coil, then it is likely that long-term angiographic results will be better. Higher packing densities can be achieved by increasing the volume of coils by increasing their thickness or increasing the inserted length. Recently, it has been shown that coils with a primary wire diameter of 0.012 in. pack better than coils of 0.010 in. [13] and that complexly shaped coils allow better aneurysm filling than helical coils [10].
In conclusion, in coiled intracranial aneurysms, high packing densities protect against reopening by compaction in non-thrombosed aneurysms. However, since partial intraluminal thrombosis can be difficult to detect at the time of treatment, it is not justified to omit follow-up imaging of embolised aneurysms based on high packing density alone.
References
Brilstra EH, Rinkel GJ, van der Graaf Y, van Rooij WJ, Algra A (1999) Treatment of intracranial aneurysms by embolization with coils: a systematic review. Stroke 30:470–476
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R (2002) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360:1267–1274
Sluzewski M, van Rooij WJ, Rinkel GJ, Wijnalda D (2003) Endovascular treatment of ruptured intracranial aneurysms with detachable coils: long term clinical and serial angiographic results. Radiology 227:720–724
Byrne JV, Sohn MJ, Molyneux AJ, Chir B (1999) Five-year experience in using coil embolization for ruptured intracranial aneurysms: outcomes and incidence of late rebleeding. J Neurosurg 90:656–663
Cognard C, Weill A, Castaings L, Rey A, Moret J (1998) Intracranial berry aneurysms: angiographic and clinical results after endovascular treatment. Radiology 206:499–510
Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D (2003) Coiling of very large or giant intracranial aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol 24:257–262
Sluzewski M, van Rooij WJ, Slob MJ, Oliván Bescós J, Slump CH, Wijnalda D (2004) The relation between aneurysm volume, packing and compaction in 145 coiled cerebral aneurysms. Radiology 231:653–658
Slob MJ, Sluzewski M, van Rooij WJ, Roks G, Rinkel GJ (2004) Additional coiling of previously coiled cerebral aneurysms: clinical and angiographic results. AJNR Am J Neuroradiol 25:1373–1376
Majoie CB, Sprengers ME, van Rooij WJ, Lavini C, Sluzewski M, van Rijn JC, den Heeten GJ (2005) MR angiography at 3T versus digital subtraction angiography in the follow-up of intracranial aneurysms treated with detachable coils. AJNR Am J Neuroradiol 26:1349–1356
Piotin M, Iijima A, Wada H, Moret J (2003) Increasing the packing of small aneurysms with complex-shaped coils: an in vitro study. AJNR Am J Neuroradiol 24:1446–1448
Cloft HJ, Kallmes DF (2004) Aneurysm packing with hydrocoil embolic system versus platinum coils: initial clinical experience. AJNR Am J Neuroradiol 25:60–62
Kawanabe Y, Sadato A, Taki W, Hashimoto N (2001) Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: correlation between coil packing density and compaction. Acta Neurochir (Wien) 143:451–455
Slob MJ, van Rooij WJ, Sluzewski M (2005) Coil thickness and packing of cerebral aneurysms: a comparative study of two types of coils. AJNR Am J Neuroradiol 26:901–903
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Slob, M.J., Sluzewski, M. & van Rooij, W.J. The relation between packing and reopening in coiled intracranial aneurysms: a prospective study. Neuroradiology 47, 942–945 (2005). https://doi.org/10.1007/s00234-005-1446-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-005-1446-9