Abstract
Transient receptor potential vanilloid (TRPV) channels are nonselective cation channels pertinent to diverse physiological functions. Multiple TRPV channel subtypes have been identified in different tissues and cloned. The aim of this study was to investigate the role of TRPV channels in hypoxia-induced proliferation of human pulmonary artery smooth muscle cells (PASMCs) and its possible signal pathway. Reverse transcriptase–polymerase chain reaction, real-time polymerase chain reaction, and Western blot analysis were used to detect the expression of TRPV in human PASMCs. Cell number was determined with a hemocytometer. Cytosolic Ca2+ concentration ([Ca2+]cyt) was measured with a dynamic digital Ca2+ imaging system. The mRNA of TRPV1-4 was detected in human PASMCs and chronic hypoxia up-regulated expression levels of the TRPV1 gene and protein. The ability to proliferate, the resting [Ca2+]cyt, and cyclopiazonic acid–induced capacitative Ca2+ entry in human PASMCs were enhanced significantly by chronic hypoxia compared with the control, and these effects were inhibited in a dose-dependent manner by capsazepine, a TRPV1 channel inhibitor. These results suggest that TRPV1 may be a critical pathway or mediator in chronic hypoxia-induced proliferation of human PASMCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hypoxia-induced pulmonary arterial hypertension (PAH) is closely associated with profound vascular remodeling, especially pulmonary arterial medial hypertrophy and muscularization due to hyperplasia of pulmonary artery smooth muscle cells (PASMCs). The molecular mechanism responsible for the proliferation of PASMCs is extremely complex. High intracellular [Ca2+] is a critical factor responsible for linking external stimuli to cell proliferation and gene expression (Golovina 1999; Landsberg and Yuan 2004). In human PASMC membrane, there are mainly two kinds of calcium channel–mediated Ca2+ entry: voltage-dependent calcium channels, which open in response to membrane depolarization; and voltage-independent calcium channels, which include store-operated channels (SOC) and receptor-operated channels, which can be activated in normal membrane potential with dependence on Ca2+ store depletion or membrane receptors binding to growth factors and mitogenic agonists. Ca2+ influx via voltage-dependent calcium channels represents the major pathway in most excitable cells and in muscle cells. However, Ca2+ influx via voltage-independent calcium channels can be a determinant in the regulation of vascular tone and the proliferation of vascular smooth muscle cells (Remillard and Yuan 2006), especially in pathophysiological conditions. In particular, SOC-mediated capacitive Ca2+ entry (CCE) pathways in PASMCs has been reported to have an important role in pulmonary vascular remodeling and in the proliferation of PASMCs during PAH (Firth et al. 2007; Lin et al. 2004).
The members of the transient receptor potential vanilloid (TRPV) channel family (TRPV1-6), which is widely expressed in various cell types of mammalian organ systems, are nonselective cation channels that are highly permeable to Ca2+. These channels can be activated by capsaicin and a diverse range of biological stimuli, including acid, temperature change, osmolarity, mechanical stress, intracellular concentration of Ca2+, and various inflammatory mediators (Firth et al. 2007; Jia and Lee 2007). Because of the high level of permeability to Ca2+ and sensitivity to various physiological stimuli, TRPV channels are believed to have an important role in the regulation of many cell functions. It has been shown that TRPV1 is expressed in rat PASMCs and could mediate Ca2+ entry and an increase in cytosolic calcium concentration ([Ca2+]cyt) (Minke 2006). TRPV4 has been shown to form a novel Ca2+ signaling complex with ryanodine receptors, and large-conductance Ca2+-activated K+ channels that elicit smooth muscle hyperpolarization and arterial dilation via Ca2+-induced Ca2+ release in response to an endothelial-derived factor. The TRPV4 agonist is capable of evoking significant Ca2+ influx in PASMCs (Earley et al. 2005). These findings provide molecular and physiological evidence that TRPV channels operate as a Ca2+ entry pathway in vascular myocytes. This novel Ca2+ entry pathway may have important roles in the regulation of pulmonary and systemic circulation.
TRPV channels have not been characterized systematically in human PASMCs, and very little information regarding the expression and function of these channels in human pulmonary arteries is available. In this study, we sought to identify the subtypes of TRPV channels expressed in human PASMCs as well as to determine the changes in TRPV channel expression and their involvement in high [Ca2+]cyt, store-operated Ca2+ entry and hypoxia-induced proliferation of PASMCs.
Materials and Methods
Reagents and Solutions
Cyclopiazonic acid (CPA), capsazepine (CPZ), and anti-vanilloid receptor-1 antibody were purchased from Sigma-Aldrich (St. Louis, MO); fura 2-acetoxymethyl ester (fura 2-AM) was purchased from Invitrogen (Carlsbad, CA). CPA and fura 2-AM were dissolved separately in dimethylsulfoxide to make stock solutions of 30 mM and 10 mM, respectively. CPZ was dissolved in methanol to make a stock solution of 10 mM. All other chemicals were of analytical reagent grade and were purchased locally. Physiological salt solution (PSS) contained (in mM): 141 NaCl, 4.7 KCl, 1.8 CaCl2, 1.2 MgCl2, 10 HEPES (N-[2-hydroxyethyl] piperazine-N′[2-ethanesulfonic acid]), and 10 glucose (pH 7.4). Ca2+-free PSS was made by replacing CaCl2 with equimolar MgCl2, and ethylene glycol tetraacetic acid was added to a final concentration of 1 mM to chelate any residual Ca2+. Tween-20 Tris-buffered saline (TTBS) contained (in mM): 10 Tris–HCl, pH 7.4, 150 NaCl, and 0.05% (w/v) Tween-20.
Cell Culture
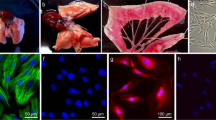
Human PASMCs from normal subjects were purchased from Cascade Biologics (Portland, OR) and routinely cultured in smooth muscle growth medium (SMGM; Cascade Biologics), which consisted of smooth muscle basal medium (SMBM, M231), 5% smooth muscle growth supplement (SMGS), and 1% penicillin/streptomycin at 37°C in a humidified 5% CO2 atmosphere. The SMGS provided final concentrations of 4.9% fetal bovine serum (FBS), 2 ng/ml basic fibroblast growth factor, 0.5 ng/ml epidermal growth factor, 5 ng/ml heparin, 5 mg/ml insulin, and 0.2 mg/ml bovine serum albumin. The growth medium was changed every other day until confluence. Cells were subcultured and plated onto 18-mm coverslips (for measurement of [Ca2+]cyt), 24-well plates (for cell count), or petri dishes (for molecular biology experiments) with 0.25% trypsin/0.02% ethylenediaminetetraacetic acid after cells reached 80–90% confluences. Cells cultured between passages 4 and 8 were used for experiments. All cells were synchronized in serum-free medium for 24 h before experimentation.
Hypoxic Treatment
Growth of human PASMCs was arrested by replacing SMGM with serum-free SMBM 24 h before the experiment, and the cells were divided into two groups. The control group (normoxia) was incubated in 5% CO2 in air (21% O2, 74% N2), and the hypoxia group was incubated in 3% O2, 5% CO2, and 92% N2 for 72 h.
Cell Count
For cell-counting experiments, growth-arrested PASMCs were cultured in 0.5% FBS-SMGM for 72 h with different concentrations of CPZ, a TRPV1 channel inhibitor, under hypoxia. Cell viability was determined with 0.4% trypan blue. Cell number was determined with a hemocytometer. The cell counts in the four 1-mm2 corner squares of the hemocytometer were averaged to calculate the total number of PASMCs (1 × 104/ml) in the suspension.
Reverse Transcriptase–Polymerase Chain Reaction (RT-PCR)
Total RNA of cultured human PASMCs was extracted with TriZol reagent (Sigma-Aldrich) according to the manufacturer’s instructions. The quality of the RNA isolation was determined from the ratio of absorbance at 260 nm to that at 280 nm (1.7–1.9) and the integrity and distinctness of the 28S and 18S RNA bands appearing on electrophoresis of RNA in 1% agarose gel. Human brain total RNA used as a positive control was purchased from Clontech (Mountain View, CA). RNA was reverse transcribed to synthesize first-strand cDNA, and PCR was performed with an RNA PCR kit (TaKaRa Technologies, Dalian, China). The total RNA was melted in 20 μl of diethylenepyrocarbonate-treated water. RNA was reverse transcribed and used for parallel assays of TRPV1-6 and glyceraldehyde-3-phosphate dehydrogenase mRNA by PCR amplification. The specific sense and antisense primers used are listed in Table 1. PCR was performed with an Icycler Thermal cycler (Bio-Rad, Hercules, CA) under the following conditions: the PCR reaction mixture was subjected to 35 cycles of denaturation at 94°C for 0.5 min, annealing at 56°C for 0.5 min, and extension at 72°C for 0.5 min. This was followed by incubation at 72°C for 10 min to ensure complete product extension. The amplified products were separated by electrophoresis in 2% agarose gel and stained with ethidium bromide. The PCR product bands were visualized under ultraviolet light. All PCR products were sequenced with the ABI PRISM Big Dye Terminator v3.1 Cycle Sequencing Ready Reaction kit and an ABI PRISM 3730XL genetic analyzer (Applied Biosystems, CA).
Real-Time Polymerase Chain Reaction (Real-Time PCR)
The cDNA of human PASMCs was subjected to comparative quantitative real-time PCR with a Brilliant SYBR Green QPCR Master Mix kit (Stratagene, La Jolla, CA) following the manufacturer’s protocols. Primer sequences for TRPV subtypes and the β-actin control are listed in Table 1. The PCR protocol consisted of initial enzyme activation at 95°C for 10 min, followed by 40 cycles of 95°C for 0.5 min, 56°C for 1 min, and 72°C for 0.5 min. Melting curves and agarose gel electrophoresis were performed to verify the specificity of the product. Data were analyzed by MxPro QPCR v3.0 software.
Western Blot Analysis
Human PASMCs incubated under normoxia or hypoxia were washed gently in cold PSS twice; then the cells were collected and lysed in eukaryotic cell lysis buffer (BioDev-Tech, Beijing, China) following the manufacturer’s instructions. Proteins (30 μg) were mixed and boiled in sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) sample buffer for 5 min, separated by SDS-PAGE (10% polyacrylamide gel), and then electrotransferred onto a nitrocellulose membranes by electroblotting in a Mini Trans-Blot. The transferred membrane was washed for 10 min with TTBS followed by the blocking solution with 10% nonfat milk in TTBS for 1 h. The blocked membrane was incubated with primary rabbit anti-vanilloid receptor-1 antibody (Sigma-Aldrich) at a 1:2000 dilution for 3 h at room temperature. For the second antibody, the membranes were incubated with horseradish peroxidase–conjugated goat anti-rabbit IgG (Zsgb-Bio, Beijing, China) at a 1:4000 dilution for 1 h at room temperature. The membranes were washed three times in TTBS after incubation with the primary or secondary antibody. Finally, immunoblotting signals were visualized with a Western luminescent detection kit (Vigorous Bio, Beijing, China). To analyze the protein expression levels of TRPV1, the expression of actin was determined as an internal control. Those membranes blotted with antibodies against TRPV1 were stripped with buffer containing 62.5 mM Tris–HCl, pH 6.7, 100 mM 2-mercaptoethanol, and 2% sodium dodecyl sulfate for 60 min at 55°C with constant shaking. Polyclonal anti-actin (sc-1616, Santa Cruz Bio, CA) was reprobed at a 1:2000 dilution for 3 h at room temperature. The value of the relative absorbance of each band corresponding to TRPV1 was normalized to the value of actin to determine the protein expression level.
Measurements of Cytosolic Calcium Concentration
The human PASMCs cultured on coverslips were loaded with membrane-permeable fura 2-AM at a concentration of 3 μM for 30 min in the dark at room temperature (22–24°C). The cells were transferred to a recording cell chamber on the microscope stage and superfused (2–3 ml/min) with PSS for 30 min to remove extracellular dye and to allow intracellular cleavage of fura 2-AM to active fura 2. The [Ca2+]cyt of individual cells was measured with a Nikon epifluorescence microscope (TE2000-U, Nikon, Tokyo, Japan) equipped with a xenon lamp (Lambda DG4, Sutter Instruments, CA) and band-pass filters for wavelengths of 340 nm and 380 nm. The 340 nm/380 nm ratio (R) of the fluorescence image was used to calculate [Ca2+]cyt. Resting [Ca2+]cyt, CPA-induced sarcoplasmic/endoplasmic-reticulum (SR/ER) Ca2+ release and SOC-mediated Ca2+ entry upon perfusion with Ca2+-free PSS changing to 1.8 mM Ca2+ PSS were measured for different groups. In most experiments, multiple (5–10) cells were imaged in a single field, and one peripheral cytosolic area from each cell was selected for analysis.
Data Analysis
Data are presented as the mean ± SEM. All experiments were performed with at least six independent PASMC cultures. Comparisons between groups of data were evaluated by Student’s t-test for unpaired samples. Differences were considered to be statistically significant at p < 0.05.
Results
Identification of TRPV Subtypes mRNA Expression in Human PASMCs
Expression of TPRV subtypes in human PASMCs was identified by conventional RT-PCR and real-time PCR. Figure 1a shows that DNA fragments of the expected sizes of 295, 476, 329, and 286 bp were amplified by TRPV1-, TRPV2-, TRPV3-, and TRPV4-specific primers, respectively, from reverse-transcribed cDNA. The nucleotide sequence of these PCR products was demonstrated by DNA sequencing to be completely identical with the corresponding sequence of the human TRPV channel. In contrast, TRPV5 and TRPV6 transcripts were not detected in six separate preparations, despite the detection of clear signals for these subtypes in positive control samples (human brain tissue) under identical amplification conditions (Fig. 1b). The relative expression of TRPV mRNA was determined by comparative quantitative real-time PCR. As shown in Fig. 1c, TRPV4 expression was the highest among all TRPV subtypes in human PASMCs, followed by TRPV2 and TRPV1, while TRPV3 was the least expressed among the TRPV channels.
Molecular identification of transient receptor potential vanilloid (TRPV) mRNA expression in human pulmonary artery smooth muscle cells (PASMCs). (a) Reverse transcriptase–polymerase chain reaction (RT-PCR) analysis of TRPV channel subtypes in human PASMCs. Predicted lengths of PCR products were: TRPV1, 295 bp; TRPV2, 476 bp; TRPV3, 329 bp; TRPV4, 286 bp; TRPV5, 306 bp; TRPV6, 237 bp; and GAPDH (glyceraldehyde-3-phosphate dehydrogenase), 452 bp. (b) Expression of TRPV mRNA in human brain tissue was used as a positive control. (c) Real-time RT-PCR analysis of the relative expression of TRPV mRNA in human PASMCs, n = 6
Chronic Hypoxia Up-Regulated the Expression Level of TRPV1 in Human PASMCs
RT-PCR, real-time PCR, and Western blot analysis were used to investigate the effect of chronic hypoxia on the gene and protein expression levels of TRPVs. The results showed that chronic hypoxia increased the mRNA expression of the TRPV1 gene significantly (Fig. 2), and the protein level of the TRPV1 channel in human PASMCs was also increased significantly under hypoxia compared with normoxia (Fig. 3). The specific TRPV1 bands was detected clearly at 90 kDa and increased after treatment under hypoxia.
Hypoxia increased the expression of transient receptor potential vanilloid (TRPV) 1 mRNA in human pulmonary artery smooth muscle cells (PASMCs). (a) TRPV1, TRPV2, TRPV3, and TRPV4 mRNA were expressed in human PASMCs cultured under normoxia (N) and hypoxia (HP). (b) Real-time reverse transcriptase–polymerase chain reaction analysis of the relative expression of TRPV1-4 mRNA in human PASMCs under normoxia (N) and hypoxia (HP). Values are mean ± SEM, n = 6, * p < 0.05 vs. N
Hypoxia increased the expression of transient receptor potential vanilloid (TRPV) 1 protein in human pulmonary artery smooth muscle cells (PASMCs). (a) Western blot analysis of TRPV1 channel proteins in human PASMCs cultured under normoxia and hypoxia for 72 h. The molecular masses of TRPV1 and actin are 90 and 43 kDa, respectively. (b) A summary of the data showing the protein levels for TRPV1 normalized to the amount of actin in human PASMCs cultured under normoxia and hypoxia for 72 h. The results are presented as mean ± SEM, n = 6, * p < 0.05 vs. N
CPZ Inhibited Hypoxia-Induced Human PASMCs Proliferation in a Dose-Dependent Manner
The mitogenic effect of hypoxia was examined in human PASMCs cultured in low-serum (0.5% FBS) medium. The proliferation of human PASMCs after treatment under hypoxia was enhanced by 36.55% compared with the control group (p < 0.0001) (Fig. 4).
To investigate the role of the TRPV1 channel in hypoxia-induced proliferation of human PASMCs, the effect of the TRPV1 channel inhibitor CPZ was observed at different concentrations. As shown in Fig. 5, CPZ inhibits proliferation of human PASMCs in a dose-dependent manner. At concentrations of 1 μM, 10 μM, and 100 μM, CPZ inhibited cell proliferation significantly (p < 0.001) compared with the control group under hypoxia.
Capsazepine (CPZ) inhibited hypoxia-induced human pulmonary artery smooth muscle cell (PASMC) proliferation in a dose-dependent manner. (a) Human PASMCs were treated for 72 h with smooth muscle basal medium (0.5% fetal bovine serum) in the presence of 0 μM, 0.1 μM, 1 μM, 10 μM, and 100 μM CPZ or methanol (meth, 100 μM) under hypoxia. The results are presented as mean ± SEM, n = 8, *** p < 0.001 vs. 0 group. (b) Dose–response curves of the effect of CPZ on the growth of human PASMCs under hypoxia
CPZ Inhibited Hypoxia-Induced Increase of Cytosolic Calcium Concentration in Human PASMCs
It has been demonstrated that chronic hypoxia-induced proliferation of PASMCs is closely related to the increase of [Ca2+]cyt. However, the increase of [Ca2+]cyt was dependent on Ca2+ influx via increased CCE. We sought to identify the role of TRPV1 in the hypoxia-induced increase of [Ca2+]cyt and CCE. As shown in Fig. 6a, when the extracellular Ca2+ was removed, blockade of SR/ER Ca2+-Mg2+ ATPase with 10 μM CPA evoked a transient increase of [Ca2+]cyt. Restoration of extracellular [Ca2+] to 1.8 mM in the continuous presence of CPA evoked a second increase of [Ca2+]cyt of a similar magnitude. The latter increase in [Ca2+]cyt represents CCE incurred as a result of calcium store depletion by CPA.
Capsazepine (CPZ) (10 μM) inhibited the hypoxia-induced increase of CPA-induced capacitive Ca2+ entry (CCE) in human pulmonary artery smooth muscle cells (PASMCs). (a) Representative [Ca2+]cyt in human PASMCs in the normoxia (N), hypoxia (HP), and hypoxia + CPZ (HP + CPZ) groups. Cyclopiazonic acid (CPA; 10 μM) was applied to cell monolayers growing on a coverslip in Ca2+-free solution for intracellular sarcoplasmic/endoplasmic-reticulum (SR/ER) depletion; then the cells were perfused with solution containing 1.8 mM Ca2+ for inducing CCE. (b) Data for resting [Ca2+]cyt, CPA-inducted ER depletion, and CCE are expressed as mean ± SEM (N group, n ≥ 48; HP group, n ≥ 45; N + HP group, n ≥ 25). *** p < 0.001 vs. N; #p < 0.05 vs. HP
In comparison to normoxic cells, exposure of human PASMC to hypoxia caused a significant increase in resting [Ca2+]cyt (control, 0.61 ± 0.01, n = 48; hypoxia, 0.72 ± 0.02, n = 45, p < 0.001; Fig. 6b). The Ca2+ transients evoked by CPA in the absence (control, 0.44 ± 0.01, n = 57; hypoxia, 0.73 ± 0.04, n = 59, p < 0.001; Fig. 6b) or in the presence (control, 0.63 ± 0.03, n = 49; hypoxia, 1.16 ± 0.07, n = 45, p < 0.001; Fig. 6b) of extracellular Ca2+ were also significantly increased under hypoxia. CPZ (10 μM) decreased CCE by 20.94% under hypoxia (from 1.16 ± 0.07, n = 45, to 0.93 ± 0.05, n = 27, p < 0.05; Fig. 6b).
Discussion
Transient receptor potential (TRP) channels can be divided into the six subgroups: the canonical (TRPC), melastatin (TRPM), ankyrin (TRPA), vanilloid (TRPV), polycystin (TRPP), and mucolipin (PRTML) families (Jordt and Ehrlich 2007). More than 10 TRP isoforms were identified in the vasculature (Firth et al. 2007). There have been extensive studies of the expression and function of TRPC channels recently, but the physiological functions of TRPV channels are much more elusive in vascular smooth muscle. Several studies have revealed that some subtypes of the TRPV channels are expressed and may play different physiological roles in murine vascular smooth muscles (Earley et al. 2005; Muraki et al. 2003; Yang et al. 2006). There is disparity between different subtypes of TRPV expression due to differences among species and cell type. Yang et al. (2006) have identified mRNA for TRPV1, TRPV2, TRPV3, and TRPV4 in both rat PASMC and aortic smooth muscle cells. TRPV1, TRPV2, and TRPV4 genes have been detected in human pulmonary arterial endothelial cells (Fantozzi et al. 2003). Our data demonstrate the expression of TRPV1, TRPV2, TRPV3, and TRPV4 in human PASMCs for the first time.
TRPV1, also referred to as vanilloid receptor 1 (VR1), is a polymodal receptor found originally in sensory neurons of the central nervous system. Recent evidence indicates that TRPV1 is expressed also in nonneuronal tissues, including several cell types in human and animal lungs (Fantozzi et al. 2003; Inoue et al. 2006; Jia and Lee 2007; Yang et al. 2006). It has been reported that TRPV channels participate in the formation of nonselective cation channels. TRPV can be activated by a number of endogenous substances (hydrogen ion, certain lipoxygenase products, etc.) and changes in physiological conditions (e.g., temperature) (Jia and Lee 2007). Activation of VR1 receptors by capsaicin-induced increase of [Ca2+]cyt suggests it may play a critical role in the regulation of several physiological functions, including pulmonary function other than nociceptive transduction (Zhang et al. 2006). With increasing numbers of studies of the TRP superfamily, it has become apparent that the interaction of different TRP subunits confers different properties (physiology, biophysics, pharmacology regulation) to the final channel (Remillard and Yuan 2006). Although the members of the TRPC subfamily are believed to encode for subunits that form SOC channels (Kunichika et al. 2004b; Takahashi et al. 2007; Wang et al. 2006), more and more studies have demonstrated that TRPV and TRPM genes also encode for subunits that participate in the formation of SOC channels in a variety of cell types (Clapham et al. 2001; Fantozzi et al. 2003). On the bases of the results of earlier reports and this study, it is reasonable to speculate that the TRP subunits coassemble into tetramers, potentially as homomeric structures, but more likely as heteromers. TRPV1 may execute its effect related to cell proliferation by participating in the formation of heterotetrameric SOC channels.
Pulmonary vascular medial hypertrophy caused by excessive proliferation of PASMCs is a major cause of the increased pulmonary vascular resistance in patients with idiopathic PAH (Patel et al. 2007; Yu et al. 2004; Zhang et al. 2007). Increased Ca2+ influx, especially increased CCE through SOC, is an important stimulus for the proliferation of PASMCs (Kunichika et al. 2004a; Yu et al. 2004). In the present study, the data show that chronic hypoxia induced proliferation of human PASMCs and an increase of [Ca2+]cyt and CCE. Chronic hypoxia mediated up-regulation of the expression level of the TRPV1 gene and protein. CPZ, an inhibitor of TRPV1, attenuated hypoxia-enhanced [Ca2+]cyt, CCE, and cell proliferation in a dose-dependent manner. These results suggested that hypoxia increased proliferation by enhancing Ca2+ influx via potentially TRPV1-encoded SOC channels in human PASMC.
CPZ, the first specific TRPV1 antagonist identified, was developed in 1992 (Bevan et al. 1992). A number of other TRPV1 antagonists have subsequently been identified, almost exclusively with the aim to develop compounds with analgesic effects. Along with the multifunction of TRPV1, the effect of CPZ other than as an analgesic was reported recently. Skogvall et al. (2008) reported that CPZ inhibited the contractile response to several different contractile agonists, and they suggested that CPZ represented a novel class of bronchorelaxants effective in human small airways. Gauden et al. (2007) observed that CPZ protected whole brain vessels from the effects of ischemia–reperfusion. Waning et al. (2007) demonstrated that the TRPV1 channel was an important Ca2+ influx channel required for cell migration, and CPZ could prevent capsaicin-stimulated migration and inhibit capsaicin-sensitive currents. In our study, CPZ was found to inhibit hypoxia-mediated proliferation of human PASMCs by blocking Ca2+ entry through CCE in a dose-dependent manner. This result supports the notion that CPZ may become a useful addition to current drug management as treatment of human PASMCs proliferation in PAH.
In summary, TRPV1 may be an important pathway or mediator in hypoxia-induced enhancement of the cytosolic Ca2+ concentration, CCE, and the proliferation of human PASMC.
References
Bevan S, Hothi S, Hughes G, James IF, Rang HP, Shah K, Walpole CS, Yeats JC (1992) Capsazepine: a competitive antagonist of the sensory neurone excitant capsaicin. Br J Pharmacol 107:544–552
Clapham DE, Runnels LW, Strubing C (2001) The TRP ion channel family. Nat Rev Neurosci 2:387–396
Earley S, Heppner TJ, Nelson MT, Brayden JE (2005) TRPV4 forms a novel Ca2+ signaling complex with ryanodine receptors and BKCa channels. Circ Res 97:1270–1279
Fantozzi I, Zhang S, Platoshyn O, Remillard CV, Cowling RT, Yuan JX (2003) Hypoxia increases AP-1 binding activity by enhancing capacitative Ca2+ entry in human pulmonary artery endothelial cells. Am J Physiol Lung Cell Mol Physiol 285:L1233–L1245
Firth AL, Remillard CV, Yuan JX (2007) TRP channels in hypertension. Biochim Biophys Acta 1772:895–906
Gauden V, Hu DE, Kurokawa T, Sarker MH, Fraser PA (2007) Novel technique for estimating cerebrovascular permeability demonstrates capsazepine protection following ischemia–reperfusion. Microcirculation 14:1–12
Golovina VA (1999) Cell proliferation is associated with enhanced capacitative Ca(2+) entry in human arterial myocytes. Am J Physiol 277:C343–C349
Inoue R, Jensen LJ, Shi J, Morita H, Nishida M, Honda A, Ito Y (2006) Transient receptor potential channels in cardiovascular function and disease. Circ Res 99:119–131
Jia Y, Lee LY (2007) Role of TRPV receptors in respiratory diseases. Biochim Biophys Acta 1772:915–927
Jordt SE, Ehrlich BE (2007) TRP channels in disease. Subcell Biochem 45:253–271
Kunichika N, Landsberg JW, Yu Y, Kunichika H, Thistlethwaite PA, Rubin LJ, Yuan JX (2004a) Bosentan inhibits transient receptor potential channel expression in pulmonary vascular myocytes. Am J Respir Crit Care Med 170:1101–1107
Kunichika N, Yu Y, Remillard CV, Platoshyn O, Zhang S, Yuan JX (2004b) Overexpression of TRPC1 enhances pulmonary vasoconstriction induced by capacitative Ca2+ entry. Am J Physiol Lung Cell Mol Physiol 287:L962–L969
Landsberg JW, Yuan JX (2004) Calcium and TRP channels in pulmonary vascular smooth muscle cell proliferation. News Physiol Sci 19:44–50
Lin MJ, Leung GP, Zhang WM, Yang XR, Yip KP, Tse CM, Sham JS (2004) Chronic hypoxia-induced upregulation of store-operated and receptor-operated Ca2+ channels in pulmonary arterial smooth muscle cells: a novel mechanism of hypoxic pulmonary hypertension. Circ Res 95:496–505
Minke B (2006) TRP channels and Ca2+ signaling. Cell Calcium 40:261–275
Muraki K, Iwata Y, Katanosaka Y, Ito T, Ohya S, Shigekawa M, Imaizumi Y (2003) TRPV2 is a component of osmotically sensitive cation channels in murine aortic myocytes. Circ Res 93:829–838
Patel HH, Zhang S, Murray F, Suda RY, Head BP, Yokoyama U, Swaney JS, Niesman IR, Schermuly RT, Pullamsetti SS, Thistlethwaite PA, Miyanohara A, Farquhar MG, Yuan JX, Insel PA (2007) Increased smooth muscle cell expression of caveolin-1 and caveolae contribute to the pathophysiology of idiopathic pulmonary arterial hypertension. FASEB J 21:2970–2979
Remillard CV, Yuan JX (2006) TRP channels, CCE, and the pulmonary vascular smooth muscle. Microcirculation 13:671–692
Skogvall S, Dalence-Guzman MF, Berglund M, Svensson K, Mesic A, Jonsson P, Persson CG, Sterner O (2008) Discovery of a potent and long-acting bronchorelaxing capsazepinoid, RESPIR 4–95. Pulm Pharmacol Ther 21:125–133
Takahashi Y, Watanabe H, Murakami M, Ohba T, Radovanovic M, Ono K, Iijima T, Ito H (2007) Involvement of transient receptor potential canonical 1 (TRPC1) in angiotensin II-induced vascular smooth muscle cell hypertrophy. Atherosclerosis 195:287–296
Wang J, Weigand L, Lu W, Sylvester JT, Semenza GL, Shimoda LA (2006) Hypoxia inducible factor 1 mediates hypoxia-induced TRPC expression and elevated intracellular Ca2+ in pulmonary arterial smooth muscle cells. Circ Res 98:1528–1537
Waning J, Vriens J, Owsianik G, Stuwe L, Mally S, Fabian A, Frippiat C, Nilius B, Schwab A (2007) A novel function of capsaicin-sensitive TRPV1 channels: involvement in cell migration. Cell Calcium 42:17–25
Yang XR, Lin MJ, McIntosh LS, Sham JSK (2006) Functional expression of transient receptor potential melastatin- and vanilloid-related channels in pulmonary arterial and aortic smooth muscle. Am J Physiol Lung Cell Mol Physiol 290:L1267–L1276
Yu Y, Fantozzi I, Remillard CV, Landsberg JW, Kunichika N, Platoshyn O, Tigno DD, Thistlethwaite PA, Rubin LJ, Yuan JX (2004) Enhanced expression of transient receptor potential channels in idiopathic pulmonary arterial hypertension. Proc Natl Acad Sci USA 101:13861–13866
Zhang Y, Xiang B, Li YM, Wang Y, Wang X, Wang YN, Wu LL, Yu GY (2006) Expression and characteristics of vanilloid receptor 1 in the rabbit submandibular gland. Biochem Biophys Res Commun 345:467–473
Zhang S, Patel HH, Murray F, Remillard CV, Schach C, Thistlethwaite PA, Insel PA, Yuan JX (2007) Pulmonary artery smooth muscle cells from normal subjects and IPAH patients show divergent cAMP-mediated effects on TRPC expression and capacitative Ca2+ entry. Am J Physiol Lung Cell Mol Physiol 292:L1202–L1210
Acknowledgments
This study was supported by the National Science and Technology Pillar Program in the Eleventh Five-year Plan Period (grant 2006BAI01A06), the Natural Science Foundation of Beijing (grant 7082012), the Scientific Research Common Program of Beijing Municipal Commission of Education (grant KM200710025002), the Key Project of Science Foundation of Ministry of Education of China (grant 208002), and the Ministry of Science and Technology of China (grant 2009CB522107).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Wang, Y.X., Wang, J., Wang, C. et al. Functional Expression of Transient Receptor Potential Vanilloid-Related Channels in Chronically Hypoxic Human Pulmonary Arterial Smooth Muscle Cells. J Membrane Biol 223, 151–159 (2008). https://doi.org/10.1007/s00232-008-9121-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00232-008-9121-9