Abstract
Although ergogenic effects and health benefits have been reported for creatine used as nutritional supplement, to date little is known about the mechanism of creatine absorption in the small intestine. Thus the current study was undertaken to elucidate the mechanism of creatine intake in rat jejunum with the use of well-purified brush border membrane vesicles, isolated from jejunal enterocyte. Creatine uptake was found markedly stimulated by inwardly directed Na+ and Cl− gradients, potential-sensitive, strongly reduced by the substitution of Na+ and Cl− with various cations and anions and positively affected by intravesicular K+. Moreover, creatine uptake is: 1) significantly inhibited by creatine stuctural analogs, 2) abolished by low concentrations of 2-aminoethyl methanethiosulfonate hydrobromide (MTSEA), 3) saturable as a function of creatine concentration with an apparent Michaelis-Menten constant of 24.08 ± 0.80 μM and a maximal velocity of 391.30 ± 6.19 pmoles mg protein−1 30 s−1. The transport is electrogenic since at least two Na+ and one Cl− are required to transport one creatine molecule. Western blot analysis showed the same amount of creatine transport protein in the jejunal apical membrane when compared to ileum. Thus, these data demonstrate the existence of a Na+- and Cl−-dependent, membrane potential-sensitive, electrogenic carrier-mediated mechanism for creatine absorption in rat jejunal apical membrane vesicles, which is biochemically and pharmacologically similar to those observed in other tissues. However, in other cell types the stimulatory effect of intravesicular K+ was never detected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracellular phosphocreatine, formed from creatine by creatine kinase, is an essential component of energy metabolism in tissues with high energy demands such as muscles and brain, where the creatine/phosphocreatine system functions as a spatial energy buffer between the cytosol and mitochondria. In mammals, creatine is either synthesized in liver, kidney and pancreas or obtained from the diet by meat-containing products (Walker, 1979; Persky & Bazeau, 2001). In both cases creatine is transported via the blood to the tissues requiring creatine, where the uptake into the cells is carried out by a specific transporter (CT) that facilitates the entry of creatine against a very large concentration gradient (Snow & Murphy, 2001). Two human creatine-transporter genes have been identified. The gene encoding the protein known as “CT1” has been mapped to Xq28 (Sandoval et al., 1996) and is expressed in most tissues, with highest levels in skeletal muscle and kidney. The creatine transporter gene known as “CT2” has been mapped to 16p11 and is expressed in testis only (Iyer et al., 1996). Although there are no functional data for CT2, it is 97% homologous to CT1 and probably provides a source of creatine for normal sperm mobility (Chen, Reith & Quick, 2004). Both transporters belong to the SLC6 family of Na+- and Cl−-dependent neurotransmitter transporters, whose members mediate solute translocation across cell plasma membranes by coupling solute transport to the cotransport of sodium and chloride down their electrochemical gradients (Chen, Reith & Quick, 2004; Hediger et al., 2004).
Diet intake, in normal conditions, supplies about 50% of creatine requirement (Walker, 1979; Persky & Bazeau, 2001); moreover, creatine dietary supplement is increasingly used both as an ergogenic aid to improve athletes’ exercise performance (Wyss & Kaddurrah-Daouk, 2000) and as a possible therapeutic agent in the treatment of various muscle, neurological and neuromuscolar disease conditions (Ferrante et␣al., 2000; Tarnopolsky et al., 2001; Beal, 2003;). Actually, the potential of creatine to be protective has been illustrated in numerous models of neurodegeneration as well as in animal models of traumatic brain injury and cerebral ischemia (Beal, 2003). Moreover, a potential of oral creatine supplementation in lowering plasma homocysteine concentration and thus in indirectly lowering the risk of developing atherosclerotic deseases has been postulated (Wyss & Schulze, 2002).
In spite of the physiological relevance of oral creatine intake, up to now little is known about the mechanisms of intestinal creatine absorption. CT mRNA transcripts were evidenced in human small intestine and colon (Nash et al., 1994). Moreover, Peral-Rubio et al. (2002), besides demonstrating the presence of CT mRNA and protein in mammalian and avian ileum, have functionally characterized creatine transport in chicken isolated enterocytes and in pieces of rat ileum. It has long been established that there is a great deal of heterogeneity of transport functions in different segments of the mammalian small intestine (Turnberg et al., 1970; Murer, Hopfer & Kinne, 1976). So, in view of the functional differences between different regions (e.g., ileum vs. jejunum), aim of the present study was to explore the contribution of the jejunal tract in the creatine absorption process. Furthermore, although the above cited study has provided important information regarding the intestinal creatine uptake process at the tissue/cellular level, for a substrate that undergoes some degree of intracellular metabolism, as is the case with creatine, such studies are best performed using purified membrane vesicle preparations that are devoid of intracellular components. Moreover, up to now no data are available describing the mechanism of creatine transport across the individual membrane domains of the polarized intestinal absorptive cells, i.e., apical and basolateral membrane domains. Since the essential step in creatine absorption is the permeation of the microvillus plasma membrane, we investigated the mechanism of creatine transport across the brush border membrane of enterocyte using jejunal brush-border membrane vesicles.
Materials and Methods
CREATINE ASSAY
Rodent laboratory chow (standard Vogt-Moller diet) was powdered and creatine, if present, was extracted-with 0.1 N HCl. Samples were incubated at 37°C for 60 min before being spun at 11,000 × g for 5 min. The supernatant was collected, neutralized with NaOH 0.1 N, and the assay was performed according to Fossati, Prencipe and Berti (1983), by using an enzymatic colorimetric method (Sentinel, CH).
BRUSH BORDER MEMBRANE ISOLATION
Male albino rats (Wistar strain, Charles River Italiana) weighing 250–300 g (about two months age), fed on a rodent laboratory chow and tap water, were used. The rats were deeply anesthetized with an injection of 2,2,2-tribromoethanol (0.05 g/250 g body weight I.P.) and then decapitated. Brush border membrane vesicles were isolated from rat jejunum enterocytes by the Mg2+ precipitation method first described by Schmitz et al. (1973). Mucosal scrapings, homogenized in hypotonic solution (50 mM sorbitol and 2 mM Tris Cl, pH 7.1) and incubated with 10 mM MgCl2 for 15 min at 0°C, were centrifuged at 3,000 × g for 15 min. The supernatant was centrifuged at 27,000 × g for 30 min. In order to obtain the desired intravesicular ion composition, the pellet was resuspended in the appropriate buffer and centrifuged at 43,000 × g for 20 min. The final pellet was resuspended in the above solution and subsequently used in the transport studies.
To control the purity of the membrane fraction, as a rule total protein, γ-glutamyltransferase (γ-GT, a marker enzyme for brush border membrane) and Na+, K+-ATPase (a marker enzyme for basolateral membranes) were determined as published (Orsenigo et al., 1985).
UPTAKE EXPERIMENTS
The timed uptake of 14C-creatine (2.035 GBq/mmol, ICN Biomedicals, Italy) was assayed at 28°C in the presence of intra- and extravesicular solutions described for each experiment in the figures legends.
A volume of membrane suspension (1–3 mg protein/ml) was mixed with the proper incubation solution (zero time). Samples were removed at selected times and diluted with 0.8 ml of ice-cold reaction-stopping solution (see individual experiments), filtered on wetted cellulose nitrate filters (0.45 μm pore size) and immediately rinsed with 5 ml of the stop solution. The radioactivity of the filters was counted by liquid scintillation spectrometry (Tri-Carb, Packard, model 1600 TR).
All experiments were performed in voltage-clamp conditions by using either valinomycin and equal or different intra- and extravesicular K+ concentrations or equal intra- and extravesicular NO −3 concentrations. The solutions used were pre-filtered through 0.22 μm pore size filters. Individual uptake experiments, at least in triplicate, representative of more than three repetitions with qualitatively identical results, are presented throughout the paper. Uptake values are presented as means ± SEM.
SDS-PAGE AND IMMUNOBLOTTING OF PROTEINS
Apical membrane proteins from the jejunum and the ileum of four rats were obtained as described above, except for the presence of protease inhibitors (300 μM phenylmethylsulfonyl fluoride (PMSF), 100 μM L-l-chloro-3-[4-tosylamido]-4-phenyl-2-butanone (TPCK), 1.5 μM pepstatin, 1.5 μM leupeptin, 10 μg/ml aprotinin) in the solutions. The final insoluble pellet was resuspended in 250 μl of phosphate buffer saline containing protease inhibitors, 1% nonidet P40 (NP40) and 0.5 % Triton X-100 and solubilized. The protein concentration was measured according to the Bradford method (Bradford, 1976) and equal amounts of proteins (60 μg) were analyzed by SDS-PAGE electrophoresis. Each sample was dissolved in Laemmli sample buffer [final concentration 2% (w/v) sodium dodecyl sulfate (SDS), 50% (v/v) glycerol, 1% (v/v) 2-mercaptoethanol, 50 mM Tris, pH 6.8] and heated at 65°C for 10 minutes.
A 10% polyacrylamide minigel was run in a minigel apparatus (Hoefer SE 250, Amhersham) for 2 h at 120 V. Proteins were electrophoretically transferred to a polyvinylidene difluoride (PVDF) membrane (Miniprotean 3, Biorad). After transfer, the membrane was stained with 0.1% Ponceau (Sigma, Italy) in 5% acetic acid to assess the quality of the transfer and equal loading of the lanes. After blocking with 5% non-fat dry milk in TBST buffer (50 mM Tris, 150 mM NaCl, 0.1% Tween, pH 8) for 2 h at room temperature, the proteins were probed overnight at 4°C with anti N-terminal CT 75446 antibody (kindly supplied by Dr. Oliver Speer, Institute for Cell Biology, Zurich) diluted 1:1000 in 5% non-fat dry milk-TBST buffer. The polyclonal antibody against the N-terminal (NH2-MAKKSAENGIYSVSG-) of the rat and human CRT sequence (Mayser et al. 1992; Nash et al. 1994) was prepared in rabbits, as described by Guerrero-Ontiveros & Wallimann (1998). This sequence did not match that of any protein in the sequence data banks. The primary antibody was detected with a donkey anti-rabbit IgG conjugated to horseradish peroxidase (Amersham N° NA 934), used at a 1:2000 dilution in 5% non-fat dry milk TBST buffer. Sites of antibody-antigen reaction were visualized by using Amersham ECL Plus, according to the manufacturer’s instruction, before exposure to X-ray film (Celbio, Italy).
Densitometric analysis was performed by using the ImageTool 2.0 software.
STATISTICS
Statistical analysis was done by Student’s t-test or by analysis of variance (ANOVA) followed by Newman-Keul’s Q test.
Results
The creatine assay was performed to determine the dietary content of creatine in the standard rat food used in this laboratory. Results gave evidence for a very small amount of creatine (0.33 ± 0.009 mg/g powdered pellet, 10 determinations) in normal diet conditions.
To focus on the mechanism that supports creatine intake in rat jejunum, well-purified apical membranes were used. Actually, in the brush border membrane fraction, γ-GT-specific activity is enriched about 10 times relative to the value in the starting homogenate (360 ± 16 mU·mg protein−1 in brush border fraction; 37 ± 8 mU·mg protein−1 in the homogenate, 6 determinations) and low basolateral membrane contamination has been detected (235 ± 35 mU·mg protein−1 in brush border fraction; 138 ± 9 mU·mg protein−1 in the homogenate, 6 determinations), taking also into account that for basolateral membranes the ratio of sealed to unsealed vesicles is 2:1 (Orsenigo et al., 1994).
The time course of creatine uptake into brush border membrane vesicles (Fig. 1) shows that, in the presence of both inwardly directed Na+ and Cl− gradients and inside negative electrical membrane potential (PD), creatine transiently accumulates in the intravesicular space with respect to the control. This finding suggests the presence of a creatine transporter in jejunal brush border membrane. The overshoot is reduced, but still present, when clamping the PD at zero, whereas it is annulled in the absence of Na+ and/or Cl− in the extravesicular buffer. Thus, the transport of creatine requires the presence of both Na+ and Cl− in the external medium and is further increased by a superimposed membrane potential. The same protocol of Fig. 1 was carried out using ileal brush border vesicles and similar results were obtained (data not shown).
Effects of Na+ and/or Cl− gradients and/or potential difference on creatine uptake. Membrane vesicles (25 μl) obtained in 100 mM K gluconate and 220 mM mannitol were incubated in 225 μl of 100 mM NaCl and 220 mM mannitol (squares), or 100 mM NaCl, 100 mM K gluconate and 34 mM mannitol (triangles), or 100 mM Na gluconate and 220 mM mannitol (diamonds), or 100 mM TMA-Cl and 220 mM mannitol (stars), or 400 mM mannitol (filled circles), or 100 mM K gluconate and 220 mM mannitol (empty circles, control). All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 20 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin.
Next, experiments were performed on jejunal vesicles to clarify whether Na+ and Cl− effects are elicited by their mere presence in the extravesicular solution or by their electrochemical gradient. Thus, creatine uptake was evaluated under different experimental conditions, in which, besides extravesicular Na+ and Cl−, the two ions were added, together or separately, in the intravesicular medium. Results depicted in Fig. 2 show that with equal intra- and extravesicular ion concentrations, creatine uptake does not differ from the control in the absence of PD, but is stimulated by the PD to a significant extent. In the presence of a PD, the simultaneous Na+ and Cl− gradients stimulate creatine uptake to a maximal extent, whereas Na+ gradient alone is more effective than Cl− gradient.
Role of Na+ and Cl− in creatine uptake. Membrane vesicles (25 μl) obtained in 100 mM K gluconate and 220 mM mannitol (squares and empty circles), or 100 mM TMA-C1, 100 mM K gluconate and 40 mM mannitol (triangles), or 100 mM Na gluconate, 100 mM K gluconate and 40 mM mannitol (filled circles), or 100 mM NaCl, 100 mM K gluconate and 34 mM mannitol (diamonds and stars) were incubated in 225 μl of 100 mM NaCl and 214 mM mannitol (squares, triangles, filled circles and diamonds), or 100 mM NaCl, 100 mM K gluconate and 34 mM mannitol (stars), or 100 mM K gluconate and 220 mM mannitol (empty circles, control). All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 20 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin.
Figure 3 shows the results of an experiment in which Na+- and Cl−-dependent creatine uptake was evaluated in the absence of K+ or in its presence either in both intra- and extravesicular media or only in the inner one. Membrane potential was clamped to zero using the permeant anion NO −3 . Figure 3 provides evidence for a positive effect of intravesicular K+ on Na+- and Cl−-dependent creatine uptake. No change is evident when K+ is added also in the external medium. With a superimposed PD, creatine uptake is further increased. It is known that inwardly directed Na+- and Cl− gradients coupled with outwardly directed K+ gradients serve as driving force for the transport of biogenic amines such as serotonin (5-HT, Rudnick & Clark, 1993). Since evidence was found for the expression of the 5-HT transporter in rat mucosal epithelial cells (Chen et al., 2004), to test for its possible involvement in our results, we carried out competition experiments using 70 μM and 700 μM of either unlabeled creatine or 5-HT. 70 μM and 700 μM unlabeled creatine inhibit creatine uptake by 80% and 98%, respectively, while the same concentrations of 5-HT exert 0% and 13% inhibition, respectively. Thus it is unlikely that the activation of 5-HT transporter could account for the K+ effect depicted in Fig. 3. A K+ stimulatory effect on creatine transport has never been reported in the literature: thus, the same protocol of Fig. 3 was performed using ileal brush border membranes, where a CT1 transporter has been localized (Peral-Rubio et al., 2002), and similar results were obtained (data not shown).
Effect of K+ on creatine uptake. Membrane vesicles (25 μl) obtained in 80 mM KNO3 and 158 mM mannitol (squares and triangles), or 80 mM TMA-NO3 and 158 mM mannitol (filled circles), or 100 mM K gluconate and 220 mM mannitol and preincubated with 25 μM valinomycin (diamonds), or 300 mM mannitol (empty circles) were incubated in 225 μl of 85 mM NaCl and 80 mM TMA-NO3 (squares and filled circles), or 85 mM NaCl and 80 mM KNO3 (triangles), or 100 mM NaCl and 220 mM mannitol (diamonds), or 300 mM mannitol (empty circles). All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 20 μM 14C creatine was in the incubating solutions.
In the presence of inwardly directed Na+ and Cl− gradients, intravesicular K+ and PD, the uptake of 10, 25, 60, 150 and 300 μM creatine was determined as a function of short incubation times, resulting in a linear response for at least 45 s (data not shown). Thus, a 30 s uptake period can be reasonably used for an estimate of initial uptake rate and experiments described below were performed with this incubation time. Moreover, the same data gave evidence for a small binding of creatine on the vesicle surface (about 5% of 30 s uptake for all the conditions tested). Replacement of Na+ by Li+, Cs+, tetramethylammonium+ and replacement of Cl− by acetate, bicarbonate, lactate, or gluconate almost completely abolish creatine uptake, whereas Br− instead of Cl− is tolerated (Fig. 4). Thus, the activity of the creatine transporter seems to be strictly dependent on both extravesicular Na+ and Cl−.
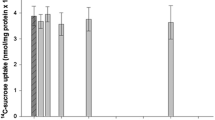
Cation and anion specificity of creatine uptakes. Membrane vesicles (10 μl) obtained in 100 mM K gluconate were incubated for 30 s in 40 μl of a buffer containing 100 mM of one of the salts indicated. (A) Creatine uptake in various cationic buffers. (B) Creatine uptake in various anionic buffers. All solutions contained 220 mM mannitol, 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 10 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Number of experiments: 4.
Methanethiosulfonate reagents (MTS) have been used for probing the structure and function of creatine transporters (Dodd & Christie, 2001). The effect of various concentrations of 2-aminoethyl methanethiosulfonate hydrobromide (MTSEA), sodium (2-sulfonatoethyl) methanethiosulfonate (MTSES) and [2-(trimethylammonium)ethyl] methanethiosulfonate bromide (MTSET) on the initial rate of creatine uptake is depicted in Fig. 5. Low concentrations of MTSEA result in a rapid inactivation of the creatine transporter, whereas MTSES and MTSET exert an inhibitory effect only at high concentrations. The effect of 60 μM MTSEA is not reversed by washing vesicles with reducing agents (10 mM dithiothreitol or 10 mM β-mercaptoethanol), thus suggesting an irreversible action of the inhibitor (data not shown).
Effect of methanethiosulfonate (MTS) reagents on creatine uptake. Membrane vesicles (10 μl) obtained in 100 mM K gluconate and 220 mM mannitol and preincubated at 37 °C for 5 min in the presence of various concentrations of MTS reagents, were incubated for 30 s in 40 μl of 100 mM NaCl and 220 mM mannitol, added or not with the same MTS concentrations. All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 10 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Number of experiments: 4.
Substrate specificity was investigated in the following experiments (Fig. 6). As expected, uptake of radioactive creatine is progressively reduced by increasing concentrations of unlabelled creatine and abolished by a 50 fold excess. The same effect is obtained with β-guanidinopropionate, a well-known structural analogue of creatine, whereas γ-guanidinobutyrate is a less efficient competitor.
Effect of structural analogs of creatine on its uptake. Membrane vesicles (10 μl) obtained in 100 mM K gluconate were incubated for 30 s in 40 μl of 100 mM NaCl, added or not with three concentrations (15, 50, 500 μM) of creatine, or β-guanidinopropionate, or γ-guanidinobutyrate. All solutions contained 220 mM mannitol, 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 10 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Number of experiments: 4.
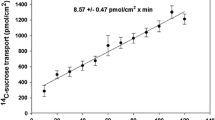
Figure 7 shows the results of an experiment in which the transport of creatine was examined as a function of increasing substrate concentrations in the incubation medium in the presence of inwardly directed Na+ and Cl− gradients, intravesicular K+ and PD. The small binding of creatine on the vesicle surface was subtracted and the Michaelian hyperbolic relationship obtained was linearized by Eadie-Hofstee transformation of the data, showing a good correlation coefficient (r = 0.996, inset of Fig. 7). Calculated parameters were: Km = 24.08 ± 0.80 μM and Jmax = 391.30 ± 6.19 pmoles·mg protein−1 ·30␣s−1.
Initial rate (30 s) of creatine uptake versus increasing concentrations of extravesicular creatine. Membrane vesicles (10 μl) obtained in 100 mM K gluconate were incubated for 30 s in 40 μl of 100 mM NaCl and increasing creatine concentrations (5–300 μM). All solutions contained 220 mM mannitol, 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Inset: Eadie Hofstee plot of data.
We examined further the effects of changes in the external concentrations of Na+ and Cl− on the initial rate of creatine uptake. As shown in Fig. 8, the rate of creatine uptake increases sigmoidally when the external concentration of Na+ is varied (with a high and constant Cl− concentration); in contrast, the rate of creatine uptake increases hyperbolically when the external concentration of Cl− is varied (with a high and constant Na+ concentration, Fig. 9). Results presented in Fig. 8 were analyzed by using the Hill plot, which was found to be linear (r = 0.996, inset of Fig. 8). The Hill coefficient for Na+, determined from the slope of the Hill plot, is 1.67 ± 0.06. Approximate values of kinetic parameters are: Km = 111.57 mM and Jmax = 80.00 pmoles·mg protein−1·30 s−1. Results of Fig. 9 were linearized by Eadie-Hofstee transformation of the data (r = 0.994, inset of Fig. 9), giving Km = 15.11 ± 0.69 mM and Jmax = 89.28 ± 0.90 pmoles· mg protein−1·30 s−1.
Dependence of creatine uptake on Na+ concentration. Membrane vesicles (10 μl) obtained in 100 mM K gluconate and 565 mM mannitol were incubated for 30 s in 40 μl of NaCl at different concentrations (0–270 mM), which were made by substitution of NaCl with TMA-Cl. All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 10 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Inset: Hill plot of the data.
Dependence of creatine uptake on Cl− concentration. Membrane vesicles (10 μl) obtained in 100 mM K gluconate and 440 mM mannitol were incubated for 30 s in 40 μl of NaCl at different concentrations (0–270 mM), which were made by substitution of NaCl with Na gluconate. All solutions contained 50 mM HEPES Tris buffer pH 7.5, 0.2 mM PMSF and 0.01% (v/v) ethanol. 10 μM 14C creatine was in the incubating solutions. Vesicles were preincubated with 25 μM valinomycin. Inset: Eadie Hofstee plot of the data.
The presence of the Na+-Cl− creatine transporter has been reported in the brush border of rat small intestine (Peral-Rubio et al., 2002), but the expression in the different tracts was not investigated. Western blot experiments performed on brush border membrane proteins from jejunum and ileum revealed that the previously reported 70 and 55 kDa bands were present in both tissues, as shown in Fig.10. The bands could represent two different creatine transport isoforms, which could result from alternative splicing of mRNA or glycosylation (Tarnopolsky et al., 2001). For both bands, there is no significant difference in the immunoreactivity between the two tracts examined, thus indicating that the same amount of creatine transport protein is present.
(A) Western blot analysis of jejunum (j or J) and ileum (i or I) brush border proteins performed with an anti-CT antibody. Ileal and jejunal tracts were isolated from four rats (labelled 1 to 4 in the figure). Two major bands were visible at 55 and 70 kDa. (B) Densitometric analysis of both bands revealed that there is no statististical difference in the intensity of the signals between ileal and jejunal tracts.
Discussion
In various tissues, over 90% of cellular creatine uptake occurs via a Na+- and Cl−-dependent CT protein (Snow & Murphy, 2001). mRNA transcripts and CT proteins have been found in tissues from rat and rabbit, such as kidney, heart, brain, liver and skeletal muscle (Guimbal & Kilimann, 1994; Schloss, Mayser & Betz, 1994).
A fairly good correlation seems to exist between the CT mRNA level and total creatine kinase (CK) activity (Nash et al., 1994), which, in turn, also correlates with the tissue concentration of total creatine (creatine + phosphocreatine) (Wyss & Kaddurrah-Daouk, 2000). Since cytosolic CK isoenzymes locally regenerate ATP, the CK system may support high-energy phosphoryl transfer between ATP-generating and ATP-consuming processes (Dzeja & Terzic, 2003). Actually, high levels of creatine are found in intestine (Wyss & Kaddurrah-Daouk, 2000), where cytosolic CK isoenzymes have been observed to associate with the cellular cytoskeleton (Walliman & Hemmer, 1994). Since a B-CK isozyme has been localized distinctly in the terminal web region of the intestinal epithelial cell brush border (Walliman & Hemmer, 1994), the mechanism supporting apical creatine intake may supply creatine for enterocyte motility.
Besides that, creatine is absorbed in small intestine. As a matter of fact, dietary creatine supplementation in humans and animals results in at least 3- to 20-fold increase in the serum concentration of creatine (Wyss & Kaddurrah-Daouk, 2000). In particular, it has been demonstrated that creatine feeding raises serum creatine levels in rat (Horn et al, 1998, Ipsiroglu et al., 2001): this evidence has made rat a suitable animal model to investigate the mechanisms that support creatine absorption.
The presence of a CT transporter has been detected in chicken small intestine and rat ileum (Peral-Rubio et al., 2002). In view of the segmental differentiation of the absorptive processes, taking into account the segmental heterogeneity of intestinal features, the present study focuses on jejunal mechanisms of creatine absorption, since differences in apical creatine transport along the longitudinal axis of the gut could be a determinant for overall creatine absorption. To test for the existence of regional differences in creatine intake along the small intestine, this investigation was carried out on rat jejunum, using isolated apical membranes in order to directly explore the brush border membrane-bound transport mechanism.
From the study reported here, first of all we can exclude the presence of a conductive pathway for creatine in jejunal brush border membrane because in the absence of Na+ and Cl−, control creatine uptake is unaffected by an imposed PD (Fig. 1). On the other hand, our experimental results provide evidence that the apical membrane of rat jejunal enterocyte possesses a creatine transporter that shares some functional properties with the members of the CT family, in that jejunal creatine transport is electrogenic and Na+- and Cl−-dependent (Daly & Seifter, 1980; Loike, Somes & Silverstein, 1986; Guimbal & Kilimann, 1993; Wyss & Kaddurrah-Daouk 2000; Garcia-Delgado et al., 2001; Snow & Murphy, 2001; Peral-Rubio et al., 2002;); both Na+ and Cl− must be present in the extravesicular buffer in order to permit the transporter activation by means of ionic and/or electrical gradients (Fig. 2). We can exclude a simple regulative role for Na+ and Cl−, since with equal intra- and extravesicular ion concentrations creatine uptake does not differ from the control (in the absence of PD): thus Na+ and Cl− are likely to be transported as well as creatine. It is also evident that Na+ gradient is more effective than Cl− gradient in stimulating creatine uptake. A new insight of this study is the stimulatory effect of intravesicular K+ on creatine transporter that, however, is still operative in the absence of this cation (Fig. 3). Data of Fig. 3 indicate that K+ gradient does not drive creatine uptake and therefore K+ is not transported by the exchanger, but rather may stimulate it by an allosteric interaction. Since we found that such a regulative role is apparent also in ileal brush border membranes (data not shown), where a CT1 protein has been evidenced, we can argue that possibly this is a common feature of CT transporters. Actually, K+ has been mostly used in addition to valinomycin to clamp membrane potential, but, although present, its role on creatine transporter was never investigated in the literature.
Reported ion selectivity (Fig. 4) is very similar to observations mostly made with the members of the CT family (Guimbal & Kiliman, 1993; Wyss & Kaddurrah-Daouk, 2000; Walzel et al, 2002).
To get more insight on jejunal creatine tansporter features, we investigated its sensitivity to MTS. Actually, it is known from the literature that all mammalian creatine transporters contain a cysteine residue (Cys144) in the third transmembrane domain, that is not present in other members of the Na+, Cl−-dependent family of neurotransmitter transporters (Guimbal & Kilimann, 1993). This cysteine residue is an important functional determinant of creatine transport, since it likely forms part of the substrate permeation path, and its modification with MTSEA leads to rapid inactivation of the transporter (Dodd & Christie, 2001). Results reported in Fig. 5 indicate that jejunal transporter shares the sensitivity to MTSEA with the members of the CT family. Another characterizing aspect of CT transporters is their specificity with respect to different creatine structural analogues, which act as competitive inhibitors of creatine uptake systems. The most efficient blocking agent in all mammalian creatine transport systems studied till now (Daly & Seifter, 1980; Loike, Somes & Silverstein, 1986) is β-guanidinopropionate, while γ-guanidinobutyrate has a smaller effect on creatine transport. Once again, the degree of inhibition of jejunal transporter by creatine analogues (Fig. 6) is consistent with data shown in several reports.
Kinetic studies demonstrate that creatine transport is saturable at low extravesicular concentrations (Fig. 7); the saturable component of creatine uptake into the mammalian tissues examined so far displays Km values for creatine of 15–128 μM (Wyss & Kaddurrah-Daojuk, 2000): thus, our results are in good agreement with literature data. In addition to the saturable component of creatine uptake, kinetic analysis often reveals a non-saturable component, which may represent passive diffusion (Wyss & Kaddurrah-Daouk, 2000). This component is not apparent in our experimental conditions.
Results of Figs. 8 and 9 reveal that at least two Na+ and one Cl− are required to transport one creatine molecule: this results in the transfer of a positive charge across the membrane, in agreement with the stoichiometry exhibited by creatine transporters in other tissues (Garcia-Delgado et al., 2001; Snow & Murphy, 2001, Peral-Rubio et al., 2002).
To sum up, the present study gives evidence for the presence of a creatine transporter in the apical membrane of rat jejunal enterocyte that shares functional features with the members of the CT family. Although the pattern of creatine transporter expression (Fig. 10) and activity is similar in both ileal and jejunal intestinal tract, regional functional differences for intestinal (jejunal-ileal) CT cannot be at the present ruled out. In fact, functional characterization of ileal creatine transporter was carried out using pieces of rat ileum (Peral-Rubio et al., 2002), where a smooth muscle layer is present. Actually, a saturable uptake for creatine was identified also in smooth muscle cells (Daly & Seifter, 1980; Nakayama & Clark, 2003), so its contribution to the overall results reported for ileum must be taken into account. This is the reason why we have confirmed the presence of the creatine transporter at the apical pole of ileal enterocyte using isolated membranes (data not shown).
Anyway, CT might be regulated in the ileum differently from the way it is regulated in the jejunum and an increase of dietary creatine or sodium might play a role in a regional adaptive response, as is the case for sodium-induced increase of SGLT1 appearance in the colon of chicken (Bindslev et al., 1997). Since in our experimental conditions rat diet contains very little creatine, we can argue that CT is normally present in the jejunal apical membrane and it is not induced by oral creatine supplementation. The low Km value, the Na+- and Cl−-dependence and the electrogenicity of the jejunal transporter make it suitable to absorb efficiently even small amounts of luminal creatine by utilizing Na+ and Cl− gradients, intracellular K+ and membrane potential at the brush border level.
References
M.F. Beal (2003) ArticleTitleBioenergetic approaches for neuroprotection in Parkinson’s disease Ann. Neurol. 53 539–548
N. Bindslev B.A. Hirayama E.M. Wright (1997) ArticleTitleNa/D-glucose cotransport and SGLT1 expression in hen colon correlates with dietary Na+ Comp. Biochem. Physiol. A 118 219–227
M.N. Bradford (1976) ArticleTitleA rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye-binding Anal. Biochem. 72 248–254 Occurrence Handle10.1006/abio.1976.9999 Occurrence Handle1:CAS:528:DyaE28XksVehtrY%3D Occurrence Handle942051
N.H. Chen M.E. Reith M.W. Quick (2004) ArticleTitleSynaptic uptake and beyond: the sodium- and chloride-dependent neurotransmitter transporter family SLC6 Pfluegers Arch. 447 519–531
M.M. Daly S. Seifter (1980) ArticleTitleUptake of creatine by cultured cells Arch. Biochem. Biophys. 203 317–324
J.R. Dodd D.L. Christie (2001) ArticleTitleCysteine 144 in the third transmembrane domain of the creatine transporter is located close to a substrate-binding site J Biol. Chem. 276 46983–46988
P.P. Dzeja A. Terzic (2003) ArticleTitlePhosphotransfer networks and cellular energetics J. Exp. Biol. 206 2039–2047
R.J. Ferrante O.A. Andreassen B.G. Jenkins A. Dedeoglu S. Kuemmerle J.K. Kubilus R. Kadurrah-Daouk S.M. Hersch M.F. Beal (2000) ArticleTitleNeuroprotective effects of creatine in a transgenic mouse model of Huntington’s disease J. Neurosci. 20 4389–4397
P. Fossati L. Prencipe G. Berti (1983) ArticleTitleEnzymic creatinine assay: a new colorimetric method based on hydrogen peroxide measurement Clin. Chem. 29 1494–1496
M. Garcia-Delgado M. J. Peral M. Cano M.L. Calonge A. Ilundain (2001) ArticleTitleCreatine transport in brush-border membrane vescicles isolated from rat kidney cortex J. Am. Soc. Nephrol. 12 1819–1825
H-L. Guerrero-Ontiveros T. Wollimann (1992) ArticleTitleCreatine supplementation in health and disease. Effect of chronic creatine ingestion in vivo: downregulation of the expression of creatine transporter isoforms in skeletal muscle Mol. cell. Biochem. 184 427–437
C. Guimbal M.W. Kilimann (1993) ArticleTitleA Na+-dependent creatine. transporter in rabbit brain, muscle, heart and kidney. cDNA cloning and functional expression J. Biol. Chem. 268 8418–8421
C. Guimbal M.W. Kilimann (1994) ArticleTitleA creatine transporter cDNA from Torpedo illustrates structure/function relationships in the GABA/Noradrenaline transporter family J. Mol. Biol. 241 317–324
M. Hediger M.F. Romero J.B. Peng A. Rolfs H. Takanaga E.A. Bruford (2004) ArticleTitleThe ABCs of solute carriers: physiological, pathological and therapeutic implications of human membrane transport proteins Pfluegers Arch. 447 465–468
M. Horn S. Frantz H. Remkes A. Laser B. Urban A. Mettenleiter K. Schnackerz S. Neubauer (1998) ArticleTitleEffects of chronic dietary creatine feeding on cardiac energy metabolism and on creatine content in heart, skeletal muscle, brain, liver and kidney J. Mol. Cell. Cardiol. 30 277–284
O.S. Ipsiroglu C. Stromberger J. Ilas H. Höger A. Mühl S. Stökler-Ipsiroglu (2001) ArticleTitleChanges of tissue creatine concentrations upon oral supplementation of creatine-monohydrate in various animal species Life Sci. 69 1805–1815
G.S. Iyer R. Krahe L.A. Goodwin N.A. Doggett M.J. Siciliano V.L. Funanage R. Proujansky (1996) ArticleTitleIdentification of a testis-expressed creatine transporter gene at 16p11.2 and confirmation of the X-linked locus to Xq28 Genomics 34 143–146
J.D. Loike M. Somes S.C. Silverstein (1986) ArticleTitleCreatine uptake, metabolism, and efflux in human monocytes and macrophages Am. J. Physiol. 251 C128–C135
W. Mayser P. Schloss H. Betz (1992) ArticleTitlePrimary structure and functional expression of a choline transporter expressed in the rat nervous system FEBS Lett. 305 31–36
H. Murer U. Hopfer R. Kinne (1976) ArticleTitleSodium/proton antiport in brush-border-membrane vesicles isolated from rat small intestine and kidney Biochem. J. 154 597–604
S. Nakayama J.F. Clark (2003) ArticleTitleSmooth muscle and NMR review: an overview of smooth muscle metabolism Mol. Cell. Biochem. 244 17–30
S.R. Nash B. Giros S.F. Kingsmore J.M. Rochelle S.T. Suter P. Gregor M.F. Seldin M.G. Caron (1994) ArticleTitleCloning, pharmacological characterization, and genomic localization of␣the human creatine transporter Receptors Channels 2 165–174
M.N. Orsenigo M. Tosco G. Esposito A. Faelli (1985) ArticleTitleThe basolateral membrane of rat enterocyte: its purification from brush border contamination Anal. Biochem. 144 577–583
M.N. Orsenigo M. Tosco A. Faelli (1994) ArticleTitleRat jejunal basolateral membrane Cl/HCO3 exchanger is modulated by a Na-sensitive modifier site J. Membrane Biol. 138 47–53
M.J. Peral-Rubio M. Garcia-Delgado M.L. Calonge J.M. Duran M.C. La Horra ParticleDe T. Wallimann O. Speer A.A. Ilundain (2002) ArticleTitleHuman, rat and chicken small intestinal Na+-Cl−-creatine transporter: functional, molecular characterization and localization J. Physiol. 545 133–144 Occurrence Handle10.1113/jphysiol.2002.026377 Occurrence Handle1:CAS:528:DC%2BD3sXktFersA%3D%3D Occurrence Handle12433955
A.M. Persky G.A. Bazeau (2001) ArticleTitleClinical pharmacology of the dietary supplement creatine monohydrate Pharmacol. Rev. 53 161–176
G. Rudnick J. Clark (1993) ArticleTitleFrom synapse to vesicle: the reuptake and storage of biogenic amine neurotransmitters Biochim. Biophys. Acta 1144 249–263
N. Sandoval D. Bauer V. Brenner J.F. Coy B. Dresher P. Kioschis B. Korn G. Nyakatura A. Poustka K. Reichwald A. Rosenthal M. Platzer (1996) ArticleTitleThe genomic organization of human creatine transporter (CRTR) gene located in Xq28 Genomics 35 383–385
P. Schloss W. Mayser H. Betz. (1994) ArticleTitleThe putative rat choline transporter CHOT1 transports creatine and is highly expressed in neural and muscle-rich tissues Biochem. Biophys. Res. Comm. 198 637–654
J. Schmitz H. Preiser D. Maestracci B.K. Ghosh J.J. Cerda R.K. Crane (1973) ArticleTitlePurification of the human intestinal brush border membrane Biochim. Biophys. Acta 323 98–112
R.J. Snow R.M. Murphy (2001) ArticleTitleCreatine and the creatine transporter: A review Mol. Cell. Biochem. 224 169–181
M.A. Tarnopolsky A. Parshad B. Walzel U. Schlattner T. Wallimann (2001) ArticleTitleCreatine transporter and mitochondrial creatine kinase protein content in myopathies Muscle Nerve 24 682–688
L.A. Turnberg F.A. Bieberdorf S.G. Morawski J.S. Fordtran (1970) ArticleTitleInterrelationships of chloride, bicarbonate, sodium, and hydrogen transport in the human ileum J. Clin. Invest. 49 557–567
J. Walker (1979) ArticleTitleCreatine: biosynthesis, regulation and function Adv. Enzym. 50 177–242
T. Wallimann W. Hemmer (1994) ArticleTitleCreatine kinase in non-muscle tissues and cells Mol. Cell. Biol. 133-134 193–220
B. Walzel O. Speer O. Boehm S. Kristiansen S. Chan K. Clarke J.P. Magyar E.A. Richter T. Wallimann (2002) ArticleTitleNew creatine transporter assay and identification of distinct creatine␣transporter isoforms in muscle Am. J. Physiol. 283 E390–E401
M. Wyss R. Kaddurrah-Daouk (2000) ArticleTitleCreatine and creatinine metabolism Physiol. Rev. 80 1107–1213
M. Wyss A. Schulze (2002) ArticleTitleHealth implications of creatine: can oral creatine supplementation protect against neurological and atherosclerotic disease? Neuroscience 112 243–260 Occurrence Handle10.1016/S0306-4522(02)00088-X Occurrence Handle1:CAS:528:DC%2BD38XktVartbg%3D Occurrence Handle12044443
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tosco, M., Faelli, A., Sironi, C. et al. A Creatine Transporter Is Operative at the Brush Border Level of the Rat Jejunal Enterocyte. J Membrane Biol 202, 85–95 (2004). https://doi.org/10.1007/s00232-004-0721-8
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00232-004-0721-8