Abstract
Purpose
Empagliflozin, dapagliflozin, canagliflozin, and ertugliflozin have been shown in randomized controlled trials to improve cardiovascular, metabolic, and renal outcomes in heart failure patients. To date, there has not been any meta-analysis examining the differences in clinical outcomes across different SGLT2 inhibitors in heart failure patients.
Methods
Four electronic databases (PubMed, Embase, Cochrane, SCOPUS) were searched on 13 September 2020 for articles published from 1 January 2000 to 13 September 2020 examining the effect of SGLT2 inhibitors on cardiovascular, renal, and metabolic outcomes in heart failure patients. Frequentist network meta-analysis was performed on extracted data.
Results
Ten randomized controlled trials were included with a combined cohort of 15,373 patients. In heart failure patients, frequentist network meta-analysis demonstrated no demonstrable difference in treatment effect across the SGLT2 inhibitors for heart failure hospitalization, cardiovascular deaths, composite of cardiovascular deaths and heart failure hospitalizations, all-cause mortality, and a composite of cardiovascular deaths and non-fatal myocardial infarction and non-fatal stroke. There was no demonstrable difference in treatment effect for worsening renal function or the weighted mean difference for weight, hemoglobin A1c, and systolic blood pressure.
Conclusions
There were no demonstrable treatment differences across SGLT2 inhibitors across cardiovascular, renal, and metabolic outcomes, although this needs to be interpreted considering the wide confidence intervals, limited number of included studies, and heterogeneity present. Future research of different SGLT2 inhibitors in head-to-head studies is warranted to determine if there is a drug class effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The sodium-glucose cotransporter 2 (SGLT2) inhibitor is a novel class of anti-hyperglycemic drugs [1]. SGLT2 inhibitors work by blocking glucose reabsorption at the proximal renal tubule, hence increasing urinary glucose excretion and lowering blood glucose in diabetic patients. Beyond glycemic control, clinical trials have demonstrated cardiovascular [2,3,4], metabolic [5,6,7], and renal benefits [4, 8] in diabetic patients treated with SGLT2 inhibitors compared to placebo. The efficacy of SGLT2 inhibitors is reflected in the 2019 European Society of Cardiology guideline as a first-line therapy for patients with type 2 diabetes mellitus and established cardiovascular disease [9].
Heart failure is a prevalent public health problem, affecting more than 37 million individuals globally [10]. In addition, it is associated with significant morbidity and mortality and confers a huge financial burden on the healthcare system [11]. Hence, to reduce the huge financial burden attributed to heart failure, cost-effective pharmacological therapy is highly sought after.
Regardless of diabetic status, recent clinical trials of SGLT2 inhibitors have demonstrated similar cardiovascular, metabolic, and renal benefits in heart failure patients. In patients with heart failure, the EMPEROR-Reduced (Empagliflozin Outcome Trial in Patients with Chronic Heart Failure With Reduced Ejection Fraction study) [12], DAPA-HF (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial) [13], and CANVAS (Canagliflozin Cardiovascular Assessment Study) [4] trials demonstrated that SGLT2 inhibitors improve cardiovascular, metabolic, and renal outcomes in heart failure patients. However, the recently published VERTIS CV trial (Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes Trial) [14] that examined the use of Ertugliflozin in diabetic patients with the atherosclerotic disease showed relatively inferior treatment effects compared to other SGLT2 inhibitors. This has generated controversy over the presence of a class effect and whether such a class effect applies across patient populations such as in patients with heart failure [15,16,17,18].
A 2019 meta-analysis suggested that dapagliflozin, empagliflozin, and canagliflozin might have class effects on cardiorenal outcomes [19]. However, the 2019 meta-analysis compared SGLT2 inhibitors in diabetic patients, rather than heart failure patients. Furthermore, the study was based on only four clinical trials, and no network meta-analysis was performed [2, 4, 20, 21]. Since that publication, multiple randomized controlled trials (RCTs) and relevant subgroup analysis of previous trials were published [12, 14, 22,23,24]. To the best of our knowledge, there has not been any meta-analysis examining the differences in cardiovascular, metabolic, and renal outcomes (henceforth clinical outcomes) across different SGLT2 inhibitors in heart failure patients. Hence, we conducted a systematic review and meta-analysis to compare the clinical outcomes across different SGLT2 inhibitors in heart failure patients. We hypothesized that in heart failure patients, SGLT2 inhibitors have no significant treatment effects across clinical outcomes.
Methods
The meta-analysis was reported according to the Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) guidelines [25]. Searches of four databases (PubMed, Embase, Cochrane, and SCOPUS) were conducted on 13 September 2020 for articles published from 1 January 2000 up to 13 September 2020. A literature search was performed using the following terms in combination: (“empagliflozin” OR “canagliflozin” OR “dapagliflozin” OR “Ertugliflozin”) AND (“trial”).
Randomized controlled trials evaluating the clinical outcomes of SGLT2 inhibitors in heart failure patients were included. Clinical outcomes were classified into cardiovascular, renal, and metabolic outcomes. Cardiovascular outcomes included heart failure hospitalization, cardiovascular deaths, a composite of heart failure hospitalization and cardiovascular deaths, all-cause mortality, and a composite of non-fatal myocardial infarction, non-fatal stroke, and cardiovascular deaths. Renal outcome (henceforth defined as worsening renal function) was a composite of a 40% reduction in estimated glomerular filtration rate, need for renal replacement therapy, or death from renal causes. Randomized controlled trials that substituted a reduction in estimated glomerular filtration rate with doubling of serum creatinine or substituted the need for renal replacement therapy with end-stage renal failure in their composite of worsening renal function were included. Metabolic outcomes included mean weight change, mean change in hemoglobin A1c (HbA1c), and mean change in systolic blood pressure. We included all randomized controlled trials, according to the PICOS inclusion and exclusion criteria (Supplemental Table 1). We excluded all randomized controlled trials which did not report cardiovascular, renal, or metabolic outcomes in heart failure patients. Four reviewers independently performed the literature search and data extraction, and all disagreements were resolved by mutual consensus.
Apart from cardiovascular, renal, and metabolic outcomes, baseline information of heart failure patients was collected for age, sex, smoking status, diabetes mellitus, hypertension, hyperlipidemia, atrial fibrillation, previous stroke, and previous myocardial infarction. Baseline information regarding the use of heart failure medications was also collected, including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers angiotensin receptor-neprilysin inhibitors, and beta-blockers. For the SGLT2 inhibitor regimes, we collected data of the drug name, drug dosage, drug frequency, control group, length of intervention, and mean length of follow-up, as shown in Supplemental Table 2. Quality control was performed by 2 independent reviewers with the Cochrane risk of bias tool [26], as shown in Supplemental Fig. 1. The quality of pooled evidence was evaluated using the modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) system for network meta-analysis, which accounts for statistical inconsistency, publication bias, risk of bias, indirectness, and statistical imprecision, as shown in Table 1 [27]. A PRISMA checklist for reporting of systematic reviews incorporating network meta-analysis [28] is included in Supplemental Fig. 2.
Statistical analysis
Prior to meta-analyses, missing data were imputed using approaches laid out by the Cochrane Handbook [29]. In studies without standard deviations, p-values or confidence intervals were converted to standard deviations [29]. In studies without standard deviations, p-values, or confidence intervals, the square-root of weighted mean variance of all other studies was used to estimate the standard deviation [30]. For panel data or longitudinal outcomes, pre-intervention baseline imbalances were corrected using the simple analysis of change scores method [29].
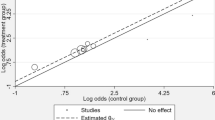
Frequentist network meta-analysis of aggregate data was adopted to compare the four different SGLT2 inhibitors using Stata 16.0 (StataCorp, TX, USA). The network meta-analysis is a method for comparing three or more interventions simultaneously by combining both direct and indirect evidence across a network of studies [31]. This produces estimates of the relative effects between any pair of interventions in the network, which are usually more precise than a single direct or indirect estimate [31]. The assumption of transitivity was evaluated using a global Wald test of consistency. Consistency models were fitted with restricted maximum likelihood models that assumed a common heterogeneity variance τ2 for all treatment contrasts for each clinical outcome when there was little evidence of inconsistency (P > 0.10 from Wald test). The inconsistency model was utilized for clinical outcomes with evidence of inconsistency (P < 0.10 from the Wald test). Treatment estimates were reported as hazard ratios and mean differences for time-to-event and continuous outcomes, respectively. Comparison-adjusted funnel plots of treatment estimates were visually inspected, and observation of asymmetry or points lying outside 95% pseudo-confidence limits was interpreted as publication bias. The geometry of each network plot was also visually and numerically inspected for potential biases. The relative ranking probability of the four treatments was estimated from 1000 draws, and the hierarchy of treatments was analyzed using surface under the cumulative ranking (SUCRA) curves. Higher SUCRA values correspond to greater efficacy. Interpretations regarding the relative efficacy of treatments were based on inspection of 95% confidence intervals in interval plots and supported by analysis of ranking probabilities.
As each treatment arm in the dataset is regarded as an independent treatment for comparison against each other, interval plots generated did not place placebo as the reference category. In such scenarios, to derive the effect estimate of SGLT2i compared to placebo, we took the reciprocal of the effect measure and confidence intervals for hazard ratios and risk ratios. A summary of the effect measures of the different types of SGLT2i against placebo is presented in Supplemental Table 3.
A sensitivity analysis was performed for patients with heart failure reduced ejection fraction and heart failure preserved ejection fraction for outcomes with sufficient observations (three or more randomized controlled trials). Sensitivity analyses were also performed for trials that recruited patients with chronic heart failure and trials with follow-up durations ≥ 1 year. Sensitivity analysis was additionally performed to exclude trials that had missing data imputed using Cochrane’s approaches.
Results
The PRISMA flowchart is presented in Fig. 1. A literature search of the four databases (PubMed, Embase, Cochrane, SCOPUS) retrieved 6626 results, and hand search uncovered 1 additional relevant study. A total of 2432 duplicates were removed. Title and abstract screening excluded a further 4138 articles as they did not include heart failure patients, did not focus on SGLT2 inhibitor use, or were not a randomized controlled trial. Full-text screening excluded 44 articles. Finally, 13 articles were included for the meta-analysis.
Baseline characteristics
Out of the 13 included articles, 4 [32,33,34,35] were secondary analyses of the EMPA-REG Outcome trial [36]. Thus, a total of 10 randomized controlled trials were included, comprising a combined cohort of 15,373 patients. The participant baseline characteristics of the included trials are shown in Table 2. While multiple publications reporting data from the same main trial were included in this meta-analysis in the case of the EMPA-REG OUTCOME trial, each outcome was analyzed only once using the relevant reported trial data. Therefore, there was no overrepresentation of any patient cohort.
Across the 10 randomized controlled trials, the SGLT2 inhibitor drug name, dosage, frequency, control group, length of intervention, and length of follow-up were summarized and are presented in Supplemental Table 2. Empagliflozin, dapagliflozin, canagliflozin, and ertugliflozin were the SGLT2 inhibitors used in three, four, two, and one trials respectively. Empagliflozin was administered at a dosage of 10 mg or 25 mg, and dapagliflozin was administered at a dosage of 10 mg throughout the randomized controlled trials. All regimes were given once daily and compared to a control group receiving a placebo. The length of follow-up ranged from 13 weeks to 4.2 years.
Comparison of cardiovascular outcomes across SGLT2 inhibitors
The comparison of cardiovascular outcomes is presented in Fig. 2. Frequentist network meta-analysis demonstrated that there was no significant difference in treatment effect for cardiovascular outcomes across the four SGLT2 inhibitors. Although statistically insignificant, empagliflozin showed the highest efficacy in reducing the hazard rate of heart failure hospitalization, compared to other SGLT2 inhibitors (6 RCTs, 11,556 patients) (Fig. 2a). Although statistically insignificant, compared to other SGLT2 inhibitors, canagliflozin showed the highest efficacy in reducing the hazard rate of cardiovascular deaths (4 RCTs, 10,641 patients) (Fig, 2b), composite of cardiovascular deaths and heart failure hospitalizations (7 RCTs, 14,975 patients) (Fig. 2c), all-cause mortality (5 RCTs, 10,666 patients) (Fig. 2d), and the composite of cardiovascular deaths and non-fatal myocardial infarction and non-fatal stroke (4 RCTs, 5795 patients) (Fig. 2e).
Comparison of worsening renal function across SGLT2 inhibitors
The comparison of worsening renal function is presented in Fig. 3. The three SGLT2 inhibitors that were analyzed are empagliflozin, dapagliflozin, and canagliflozin. The frequentist model demonstrated that there was no significant difference across the three SGLT2 inhibitors in reducing the hazard rate of worsening renal function (5 RCTs, 11,293 patients).
Comparison of metabolic outcomes across SGLT2 inhibitors
The comparison of metabolic outcomes is presented in Fig. 4. The two SGLT2 inhibitors analyzed were empagliflozin and dapagliflozin. In heart failure patients, the frequentist model demonstrated that there was no significant difference between the two SGLT2 inhibitors in the weighted mean difference for weight/kg (3 RCTs, 8530 patients) (Fig. 4a), HbA1c/mmol/mol (3 RCTs, 8530 patients) (Fig. 4b), and systolic blood pressure/mmHg (3 RCTs, 8530 patients) (Fig. 4c).
Sensitivity analysis of SGLT2 inhibitors in heart failure reduced ejection fraction
In a sensitivity analysis of SGLT2 inhibitors in patients with heart failure with reduced ejection fraction, empagliflozin and dapagliflozin did not have a significant demonstrable difference in treatment effect for heart failure hospitalization (3 RCTs, 8737 patients) (Supplemental Fig. 3). There were insufficient studies (less than 3 RCTs) to analyze for all other outcomes.
Sensitivity analysis of SGLT2 inhibitors in chronic heart failure
In a sensitivity analysis of SGLT2 inhibitors in patients with chronic heart failure, Damman 2020 [24] (EMPA-RESPONSE-AHF trial) was excluded as it studied only acute decompensated heart failure patients. Canagliflozin, dapagliflozin, and empagliflozin did not have a significant demonstrable difference in treatment effect for all-cause mortality (4 RCTs, 10,587 patients) (Supplemental Fig. 4). We analyzed all other outcomes using data from trials involving only chronic heart failure patients.
Sensitivity analysis of SGLT2 inhibitors in trials with follow-up durations ≥ 1 year
In a sensitivity analysis of SGLT2 inhibitors in trials with follow-up durations of ≥ 1 year, Nassif 2019 [37] (DEFINE-HF trial) and Damman 2020 [24] (EMPA-RESPONSE-AHF trial) were excluded as their follow-up durations were 13 weeks and 60 days respectively. Canagliflozin, dapagliflozin, and empagliflozin did not have a significant difference in treatment effect for heart failure hospitalization (5 RCTs, 11,293 patients) (Supplemental Fig. 5) and all-cause mortality (4 RCTs, 10,587 patients) (Supplemental Fig. 4). We analyzed all other outcomes using data from trials reporting a follow-up duration ≥ 1 year.
Sensitivity analysis excluding trials that had missing data imputed using Cochrane’s approaches
In Damman 2020 [24], all-cause mortality was reported as a risk ratio rather than a hazard ratio; as Damman 2020 [24] has a short follow-up duration (60 days) and low number of patients lost to follow-up (n = 1), the risk ratio was approximated to hazard ratio. Hence, we excluded Damman 2020 [24] from all-cause mortality as a sensitivity analysis, in which all-cause mortality (4 RCTs, 10,587 patients) (Supplemental Fig. 6). Canagliflozin, dapagliflozin, and empagliflozin did not have a significant demonstrable difference in treatment effect for all-cause mortality.
Discussion
In this frequentist, network meta-analysis of 10 randomized controlled trials in heart failure patients, there was no significant demonstrable treatment difference across SGLT2 inhibitors across cardiovascular, renal, and metabolic outcomes.
Patients with heart failure have an increased risk of heart failure hospitalizations and mortality [38]. In 2014, in the US, there were over 900,000 heart failure hospitalizations and more than 80,000 deaths with primary heart failure [11]. This conferred a significant healthcare burden, with heart failure hospitalizations accounting for an estimated $11 billion in healthcare costs [11]. Hence, there is a growing interest to identify cost-effective pharmacological therapies to reduce the heart failure burden.
The 2019 European Society of Cardiology guideline recommends SGLT2 inhibitors for use in diabetic patients with heart failure [9]. With the completion of recent trials demonstrating consistent clinical benefits of SGLT2 inhibitors in all heart failure patients independent of diabetic status [12, 14, 22,23,24] and a recent network meta-analysis which ranked SGLT2i as the most effective therapy for heart failure reduced ejection fraction when compared among sacubitril/valsartan and vericiguat [39], the inclusion of SGLT2 inhibitors as part of the first-line therapy in heart failure appears imminent. However, across clinical trials, different SGLT2 inhibitors were employed and it remained unknown if there were significant differences in clinical outcomes across SGLT2 inhibitors. In this meta-analysis, we showed that there was no significant demonstrable difference in cardiovascular, renal, and metabolic outcomes across SGLT2 inhibitors. Hence, the decision to choose the type of SGLT2 inhibitors for the treatment of heart failure currently may be dependent on other factors, such as the cost and availability of the individual drug. While a previous network meta-analysis compared the costs of different SGLT2 inhibitor therapies in diabetic patients [40], there are currently no cost comparisons of different SGLT2 inhibitor therapies in heart failure patients.
There exists a lack of randomized controlled trials examining the effects of SGLT2 inhibitors in heart failure patients stratified according to reduced ejection fraction and preserved ejection fraction subgroups. In our meta-analysis of 10 randomized controlled trials, most did not stratify the type of heart failure according to ejection fraction, except for the following three clinical trials: the EMPEROR-Reduced (Empagliflozin Outcome Trial in Patients with Chronic Heart Failure With Reduced Ejection Fraction study) [12], DAPA-HF (Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial) [13], and DEFINE-HF (Dapagliflozin Effects on Biomarkers, Symptoms, and Functional Status in Patients With Heart Failure With Reduced Ejection Fraction) trials [41]. Of the three trials, heart failure hospitalization was the only common reported outcome. Hence, due to the lack of randomized controlled trials, we could neither perform a sensitivity analysis in patients with heart failure with reduced ejection fraction nor for patients with heart failure with preserved ejection fraction. Future trials of SGLT2 inhibitors in heart failure patients should additionally focus on capturing the ejection fraction of heart failure patients, to further ascertain if the efficacy of SGLT2 inhibitors applies to both subgroups of patients.
In this study, we did not demonstrate a significant difference in treatment effects of different SGLT2 inhibitors across cardiovascular, renal, and metabolic outcomes in heart failure patients. While there is no universal definition of class effect, the definition of “class labeling” utilized by the United States Food and Drug Administration (FDA) states that “all products within a class are closely related in chemical structure, pharmacology, therapeutic activity, and adverse reactions” [42]. Due to the similar molecular structure, mechanism of action [1, 43,44,45], and clinical outcomes of SGLT2 inhibitors, some have postulated a potential class effect between the SGLT2 inhibitors, although our study could not conclude this. The number of studies included in this systematic review was small, and the power of comparison was low as demonstrated by the large confidence intervals of the outcomes. The inability to demonstrate differences between the SGLT2 inhibitors studied could also be due to the small sample size or heterogeneity between the studies. The ability to claim a class effect needs to be done with caution, as demonstrated previously with other drugs. The Carvedilol or Metoprolol European Trial (COMET) compared the effects of beta-blockers, namely carvedilol and metoprolol tartrate, on clinical outcomes in chronic heart failure patients [46]. The study demonstrated that carvedilol increased survival as compared with metoprolol tartrate and that there was no class effect between these 2 drugs. Adequately powered, head-to-head randomized controlled trials comparing SGLT2 inhibitors should be considered to explore the hypothesis of a class effect.
Limitations
Our study should be interpreted in due consideration of the limitations. First, there was a difference in the representation of individual SGLT2 inhibitors in clinical trials. Empagliflozin, dapagliflozin, canagliflozin, and ertugliflozin were the SGLT2 inhibitors used in three, four, two, and one trials respectively. Hence, we do not know if the results of the renal outcome apply to ertugliflozin and if that of the metabolic outcomes apply to ertugliflozin and canagliflozin. Second, many trials did not report the baseline characteristics of heart failure patients, such as the ejection fraction of patients. Hence, we were unable to examine if differences in patient characteristics affected study outcomes. Furthermore, we do not know if there is a differential treatment effect of SGLT2 inhibitors in both reduced ejection fraction and preserved ejection fraction patients, although this can be the focus of future studies.
Conclusion
In our frequentist, network meta-analysis of 10 randomized controlled trials in heart failure patients, we did not demonstrate a treatment difference across SGLT2 inhibitors across cardiovascular, renal, and metabolic outcomes. Future research of different SGLT2 inhibitors in head-to-head trials, and in different subgroups of heart failure patients with reduced and preserved ejection fraction, is warranted.
Availability of data and materials
Data used for this study can be accessed upon request from the corresponding author.
Abbreviations
- SGLT2 inhibitors:
-
Sodium-glucose cotransporter 2 (SGLT2) inhibitors
- PRISMA:
-
Preferred Reporting Items of Systematic Reviews and Meta-Analyses
- RCTs:
-
Randomized controlled trials
- HbA1c:
-
Hemoglobin A1c
- SUCRA:
-
Surface under the cumulative ranking (SUCRA) curves
References
Fattah H, Vallon V (2018) The potential role of SGLT2 inhibitors in the treatment of type 1 diabetes mellitus. Drugs 78(7):717–726
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128
Fitchett D, Zinman B, Wanner C, Lachin JM, Hantel S, Salsali A et al (2016) Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J 37(19):1526–1534
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Yoshida A, Matsubayashi Y, Nojima T, Suganami H, Abe T, Ishizawa M et al (2019) Attenuation of weight loss through improved antilipolytic effect in adipose tissue via the SGLT2 inhibitor tofogliflozin. J Clin Endocrinol Metab 104(9):3647–3660
Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF (2013) Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med 11:43
Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, Ptaszynska A (2016) Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Diabetes Endocrinol 4(3):211–220
Mosenzon O, Wiviott SD, Cahn A, Rozenberg A, Yanuv I, Goodrich EL et al (2019) Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Lancet Diabetes Endocrinol 7(8):606–617
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V et al (2020) 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur Heart J 41(2):255–323
Ziaeian B, Fonarow GC (2016) Epidemiology and aetiology of heart failure. Nat Rev Cardiol 13(6):368–378
Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD (2018) National Burden of Heart Failure Events in the United States, 2006 to 2014. Circ Heart Fail. 11(12):e004873-e
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al (2020) Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA et al (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381(21):1995–2008
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U et al (2020) Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med 383(15):1425–1435
Volpe M, Patrono C (2020) Do VERTIS-CV trial results question a class-effect of cardiovascular protection with sodium-glucose cotransporter 2 inhibitors? Eur Heart J 41(44):4232–4233
Koufakis T, Papanas N, Dimitriadis G, Zebekakis P, Kotsa K (2020) Interpreting the results of the VERTIS-CV trial: Is this the end of the “class effect” perspective? J Diabetes 12(12):942–945
Vertis CV (2020) Trial: Heterogeneity in clinical benefits of sodium-glucose cotransporter-2 inhibitors for patients with type II diabetes? [press release]
Vertis CV (2020) Ertugliflozin falls short of SGLT2s on CV outcomes, despite promise in heart failure [press release]. Am J Manag Care
Kluger AY, Tecson KM, Lee AY, Lerma EV, Rangaswami J, Lepor NE et al (2019) Class effects of SGLT2 inhibitors on cardiorenal outcomes. Cardiovasc Diabetol 18(1):99
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM et al (2019) Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380(24):2295–2306
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357
Mordi NA, Mordi IR, Singh JS, McCrimmon RJ, Struthers AD, Lang CC (2020) Renal and cardiovascular effects of SGLT2 inhibition in combination with loop diuretics in patients with type 2 diabetes and chronic heart failure: The RECEDE-CHF Trial. Circulation
Solomon SD, Jhund PS, Claggett BL, Dewan P, Køber L, Kosiborod MN, et al (2020) Effect of dapagliflozin in patients with HFrEF treated with sacubitril/valsartan: the DAPA-HF Trial. JACC Heart Fail
Damman K, Beusekamp JC, Boorsma EM, Swart HP, Smilde TDJ, Elvan A, et al (2020) Randomized, double-blind, placebo-controlled, multicentre pilot study on the effects of empagliflozin on clinical outcomes in patients with acute decompensated heart failure (EMPA-RESPONSE-AHF). Eur J Heart Fail
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Anna Chaimani DMC, Tianjing Li, Julian PT Higgins, Georgia Salanti (2013) Chapter 11: Undertaking network meta-analyses: Corchrane training handbook
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions. Second Edition, The Cochrane Collaboration
Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N (2006) Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol 59(1):7–10
Chaimani A DMC, Li T, PT Higgins J, Salanti G (2020) Chapter 11: Undertaking network meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions version 61
Böhm M, Fitchett D, Ofstad AP, Brueckmann M, Kaspers S, George JT et al (2020) Heart failure and renal outcomes according to baseline and achieved blood pressure in patients with type 2 diabetes: results from EMPA-REG OUTCOME. J Hypertens 38(9):1829–1840
Butler J, Zannad F, Fitchett D, Zinman B, Koitka-Weber A, Von Eynatten M, et al (2018) Empagliflozin and kidney outcomes in patients with or without heart failure at baseline: insights from the EMPA-REG OUTCOME trial. Diabetologia 61:S323
Pellicori P, Pernille Ofstad A, Fitchett D, Zeller C, Wanner C, George J et al (2019) Early benefits of empagliflozin in patients with type 2 diabetes with heart failure are not offset by increased adverse events: results from the EMPA-REG OUTCOME trial. Eur Heart J 40:1586
Zinman B, Inzucchi SE, Lachin JM, George J, Mattheus M, Parigi Ad, et al (2016) Abstract 16903: Consistent effect of empagliflozin on cardiovascular death in subgroups by type of cardiovascular disease: results from EMPA-REG OUTCOME. Circulation 134(suppl_1):A16903-A
Nassif ME, Windsor S, Tang F, Khariton Y, Husain M, Inzucchi S, et al (2019) Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction. Circulation 140(18)
Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. Nat Rev Cardiol 8(1):30–41
Aimo A, Pateras K, Stamatelopoulos K, Bayes-Genis A, Lombardi CM, Passino C, et al (2020) Relative efficacy of sacubitril-valsartan, vericiguat, and SGLT2 inhibitors in heart failure with reduced ejection fraction: a systematic review and network meta-analysis. Cardiovasc Drugs Ther
Johnston R, Uthman O, Cummins E, Clar C, Royle P, Colquitt J et al (2017) Canagliflozin, dapagliflozin and empagliflozin monotherapy for treating type 2 diabetes: systematic review and economic evaluation. Health Technol Assess 21(2):1–218
Nassif ME, Windsor SL, Tang F, Khariton Y, Husain M, Inzucchi SE et al (2019) Dapagliflozin effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: the DEFINE-HF Trial. Circulation 140(18):1463–1476
Furberg CD (2000) Class effects and evidence-based medicine. Clin Cardiol 23(7 Suppl 4):Iv15–9
Mancia G, Cannon Christopher P, Tikkanen I, Zeller C, Ley L, Woerle Hans J et al (2016) Impact of empagliflozin on blood pressure in patients with type 2 diabetes mellitus and hypertension by background antihypertensive medication. Hypertension 68(6):1355–1364
Kluger AY, Tecson KM, Lee AY, Lerma EV, Rangaswami J, Lepor NE, et al (2019) Class effects of SGLT2 inhibitors on cardiorenal outcomes. Cardiovasc Diabetol 18(1):99
Javed Z, Papageorgiou M, Deshmukh H, Rigby AS, Qamar U, Abbas J et al (2019) Effects of empagliflozin on metabolic parameters in polycystic ovary syndrome: a randomized controlled study. Clin Endocrinol (Oxf) 90(6):805–813
Poole-Wilson PA, Swedberg K, Cleland JGF, Di Lenarda A, Hanrath P, Komajda M et al (2003) Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. The Lancet 362(9377):7–13
Rådholm K, Figtree G, Perkovic V, Solomon SD, Mahaffey KW, de Zeeuw D et al (2018) Canagliflozin and Heart Failure in Type 2 Diabetes Mellitus: results From the CANVAS Program. Circulation 138(5):458–468. https://doi.org/10.1161/CIRCULATIONAHA.118.034222
Butler J, Zannad F, Fitchett D, Zinman B, Koitka-Weber A, von Eynatten M et al (2019) Empagliflozin improves kidney outcomes in patients with or without heart failure. Circulation: Heart Failure 12(6):e005875. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005875
Sarraju A, Li J, Cannon CP, Chang TI, Agarwal R, Bakris GL et al (2020) Canagliflozin (CANA) reduces cardiovascular (CV) and renal events independent of baseline heart failure (HF): a credence secondary analysis. J Am Coll Cardiol 75(11):1018. https://doi.org/10.1016/S0735-1097(20)31645-4
Singh JSS, Mordi IR, Vickneson K, Fathi A, Donnan PT, Mohan M et al (2020) Dapagliflozin versus placebo on left ventricular remodeling in patients with diabetes and heart failure: the REFORM trial. Diabetes Care 43(6):1356–1359. https://doi.org/10.2337/dc19-2187
Funding
C.S. was supported by the National University of Singapore Yong Loo Lin School of Medicine’s Junior Academic Faculty Scheme.
Author information
Authors and Affiliations
Contributions
Y.H.T., C.S.Y.Y., N.L.S., Y.N.T., and C.S. designed the study and developed the study protocol and tools. Y.H.T., C.S.Y.Y., Y.N.T., and J.Y.A.C. were responsible for data collection. Y.H.T., Y.N.T., C.S.Y.Y., N.L.S., and C.S. analyzed data and wrote the manuscript. All authors contributed to the conceptualization of the research questions, interpretation of the results, and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Teo, Y.H., Yoong, C.S.Y., Syn, N.L. et al. Comparing the clinical outcomes across different sodium/glucose cotransporter 2 (SGLT2) inhibitors in heart failure patients: a systematic review and network meta-analysis of randomized controlled trials. Eur J Clin Pharmacol 77, 1453–1464 (2021). https://doi.org/10.1007/s00228-021-03147-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03147-4