Abstract
Purpose
The reporting of suspected adverse drug reactions (ADRs) is starting to become routine to nurses. The aim of this review is to underline the role of clinical and community health nurses in pharmacovigilance and to promote their effective participation in ADR reporting in different countries and for patients of different ages.
Methods
The PubMed, Scopus and ISI Web of Science databases were searched for research articles published between January 1985 and April 2017 using the search items “pharmacovigilance” AND “nurse;” “adverse drug reaction report” AND “nurse;” “community health nurse” AND “adverse drug reaction.”
Results
A total of 987 articles were identified using our search strategy, of which 180 articles remained over after the removal of duplicate articles. Of these 180 studies, upon full review we identified 24 which met the inclusion/exclusion criteria and included these in our review. ADR reports by clinical nurses in some countries are comparable in quality and number to those submitted by physicians or pharmacists. Data on ADRs reported by community nurses are currently not available. However, numerous publications emphasized the challenges faced by nurses in reporting ADRs and the need to include pharmacovigilance training in both clinical and community health nurse academic education.
Conclusions
Nurses are central actors in pharmacovigilance activities, particularly in identifying ADRs which remain outside the reach of other healthcare providers and in being fundamental to the preservation of the health of patients and of the entire community, with attention to the more vulnerable patients, such as children and the elderly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Between 1999 and 2006 the annual rates of adverse drug reactions (ADRs) in the USA ranged from 0.08/100,000 to 0.12/100,000, which represents a significant increase over time at a rate of 0.0058 per year [1]. This increase in reported ADRs in the USA may result from improvements in the national reporting system, given that in general worldwide ADRs are under-reported [2, 3]. In Europe, serious ADRs cause considerable morbidity and mortality. Bouvy et al. reviewed all epidemiological studies quantifying ADRs in a European setting that had been published between 1 January 2000 and 3 September 2014 and reported a 0.5% rate fatal in-hospital ADRs, which would mean that almost 419,000 people die from fatal ADRs each year in Europe [4]. Although the exact number of ADRs worldwide is not known, whatever the true number is, ADRs represent a significant public health problem that is, for the most part, preventable [5].
Nurses and pharmacovigilance
The spontaneous reporting of ADRs is the basis of drug safety monitoring and should be a coordinated responsibility of all healthcare providers. In addition to medical doctors and pharmacists, nurses–who constantly monitor patients’ responses to drugs —should play a proactive role in pharmacovigilance activities [6, 7]. The inclusion of nurses in pharmacovigilance programs, a relatively recent development, may greatly increase the number of reports [8]. Among healthcare professionals, nurses often have a more direct relationship with the patient due to their unique role both in the assistance and in the education of patients, by administering therapies and being the first to report signs and symptoms of an ADR. It has been estimated that over 350,000 ADRs occur in U.S. nursing homes each year [9]. In 2013 Griffith wrote that “it is essential that nurses must be at the vanguard of adverse reaction reporting if the European Union's pharmacovigilance initiative is to be a success” [10]. Thus, the reporting of suspected ADRs should be incorporated into the daily work routine of the practicing nurse and nurses should receive a proper scientific education on this issue [11, 12]. The prevention of ADR onset should be considered one of the main objectives of healthcare professionals, and in particular for clinical and community health nurses, being fundamental to preservation of the health of patients and of the entire community, with extra attention paid to the more vulnerable subjects, such as children and the elderly. Indeed, the role of the community health nurse extends beyond the simple care of patients in the community and also involves community health promotion and prevention by means of health education programs, organizing at the community level and social reforms [13, 14], in both rural and urban areas.
However, there is always the question of which key indicators for the increased risk of ADRs require vigilance in the community. Certainly, the rate of ADRs grows exponentially with (1) polypharmacy, (2) the advancing age and (3) longer duration of hospital stay [15]. These characteristics should be monitored in the community by public health nurses, who is the healthcare professional closest to the needs of the most vulnerable populations and oriented towards preventive health care [13]. Parameswaran Nair and colleagues developed and validated a score to predict ADR-related hospitalization in elderly community-dwelling patients. Based on this score, the number of administered antihypertensives was the strongest predictor of an ADR, followed by the presence of dementia, renal failure, drug changes in the preceding 3 months and the use of anticholinergic medications [16].
Target population of nurse’s pharmacovigilance
Pharmacovigilance is extremely important in vulnerable subjects, such as pediatric [17] and geriatric [18, 19] patients and thus should be highly encouraged in these individuals because it deals with specific therapeutic aspects, such as the frequent use of off-label or over-the-counter (OTC) drugs. Moreover, especially in the elderly, special attention should be focused on the onset of dangerous pharmacological interactions among the numerous different drugs or herbal medications administered for chronic diseases [20, 21]. In the USA, deaths due to ADR are significantly more likely in individuals older than 55 years, with the highest risk in those aged ≥75 years [1]. In fact, polypharmacy is increasingly common due to multimorbidity, especially among the elderly patient population, and particularly in frail older individuals who are more susceptible to ADRs. Thus, ADRs due to polypharmacy represents a real challenge for hospital and community health nurses, requiring nurses to follow regular education programs and monitor research developments in the field to improve safe healthcare practice [21].
Pharmacovigilance in the community
In terms of studies on pharmacovigilance in the community, there are current no data available specifically on community health nurses but interesting studies involving the role of community pharmacies have been conducted. It is easy for patients, in particular the older ones taking long-term or multiple medications, to visit community pharmacies because of their wide geographical distribution and accessibility without the need for an appointment, with or without prescriptions [22]. In a recently published study by Yu and colleagues [23] about Korean community pharmacies located in rural and metropolitan areas, the clinical manifestations associated with ADRs spontaneously reported by the community pharmacists were mainly associated to the gastrointestinal system and nervous system, including psychiatric disorders, whereas the prevalent causative drugs were those for acid-related disorders, anti-inflammatory products, analgesics and antibacterials. Interestingly, among ADRs caused by OTC drugs, the main symptoms and causative drugs were skin disorders and non-steroidal anti-inflammatory drugs, respectively [23]. In another interesting study, Gurwitz and colleagues investigated adverse drug events (ADEs) occurring in nursing homes [9]. The authors identified 1.89 ADEs per 100 resident-months and, most notable, that 51% of the ADEs were judged to be preventable. Psychoactive medications (antipsychotics, antidepressants and sedatives–hypnotics) and anticoagulants were the most common medications associated with preventable ADEs, whereas the neuropsychiatric events were the most common types of preventable ADEs [9].
Aim of the present review
Although the role of nurses in pharmacovigilance is well established [10], the attitude of nurses towards ADR reporting and their awareness of the importance of pharmacovigilance and of their key role in spontaneous ADR reporting is still a matter of debate. The purpose of this review is to underline the role of clinical and community health nurses in pharmacovigilance, to promote their effective participation in reporting activities in different countries and for patients of different ages to report and, above all, to prevent ADRs in the community.
Methods
Data sources and searches
The PubMed, Scopus and ISI Web of Science (ISI) databases were searched for relevant research articles published between January 1985 and April 2017 using the search terms “pharmacovigilance” AND “nurse;” “adverse drug reaction report” AND “nurse;” “community health nurse” AND “adverse drug reaction.”
Only research articles published in English and French that reported on clinical or community health nurse activity in pharmacovigilance or ADR reports were included in this review. No geographical limitation was adopted: articles were from Asia, Africa, Europe, North and South America and Oceania. Studies conducted in the community, in residential aged care facilities and in a hospital setting were considered.
Inclusion/exclusion criteria
Research studies were included in the review if they met the following inclusion criteria: (1) the study looked at the role of clinical or public/community health nurses in pharmacovigilance; (2) the study examined ADR reporting rates by clinical or public/community health nurses and other health professionals; (3) the study reported data from national and international ADR databases; (d) the study involved questionnaires to nurse populations on pharmacovigilance or ADRs. Publications were excluded if they were narrative reviews, commentaries, editorials or letters to the editor. Additional articles, such as reviews and editorials which dealt with the role of the nurse in pharmacovigilance, community pharmacies, community or public health nurses and general concepts in pharmacovigilance were included into various sections of the review.
Following removal of duplicate studies, the two authors independently reviewed each article for potential eligibility based on the title and abstract. The full text was obtained for articles considered to be eligible by either author.
Data synthesis and analysis
The two authors independently reviewed relevant data from the identified studies. Each study was analyzed and a summary of the findings written down. The results of this review process were compared, and any discrepancies were resolved by consensus following discussion.
Results
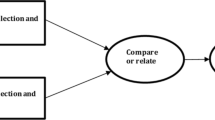
Our literature research strategy and inclusion/exclusion criteria are shown in Fig. 1. Using the search items “pharmacovigilance” AND “nurse” we identified 91, 110 and 91 articles in the PubMed, Scopus and ISI databases, respectively; using the search items “adverse drug reaction report” AND “nurse” we identified 129, 240 and 191 articles in these same three databases, respectively. Finally, using the search items “community health nurse” AND “adverse drug reaction” we identified 68, 47 and 20 articles in PubMed, Scopus and ISI, respectively. After the removal of duplicate studies, we identified and reviewed a total of 180 articles, of which 24 met the inclusion criteria (see Methods) and were included in the study (Table 1).
ADR reports by nurses were found to be comparable in quality and number to those submitted by physicians [7]. However, under-reporting of ADRs by nurses has been well-documented. In a recent analysis of 16 published studies, De Angelis et al. concluded that “nurses’ attitudes that hinder reporting include ignorance, insecurity, fear and lethargy” [24].
As an example, two studies conducted in Portugal demonstrated that there were no differences in the reporting of serious ADRs among nurses, physicians and pharmacists, although the nurse’s role and attitude toward the pharmacovigilance system was still underestimated [25, 26]. In Sweden, nurses are the main administrators of drugs and recorders of signs and symptoms of the patients, and thus these healthcare professionals play an important role in the detection of suspected ADRs and contribute to the increase of the total reporting rate [27, 28]. Based on their study using data in the Italian pharmacovigilance database, Conforti and colleagues provided evidence for the potential capacity of nurses to improve the detection of ADRs [29]. In Spain, the ADR reporting rate in the pediatric population has increased since 2004, mostly due to the high proportion of suspected ADR reports related to vaccines, which highlights the important role played by nurses [30].
The results of a pilot study carried out in Ireland in 1995 suggested that nurses could contribute significantly to the spontaneous reporting of suspected ADRs, and their subsequent involvement in research of ADR immediately enriched the process both quantitatively and qualitatively [31]. Data on the reporting rate of nurses have mostly involved adult patients, such as the study by Conforti et al., which showed the impact of reporting by nurses on the Italian pharmacovigilance system [29]. Between 2004 and 2010, the national network of pharmacovigilance received 74,657 reports of ADRs from different categories of health professionals, of which only 1951 reports were from nurses [29]. However, the total number of annual reports increased greatly during the 6 years of the study, with a substantial increase in the reporting rate from 2006 to 2009, followed by a slow decline in 2010 [29]. Bigi and colleagues investigated pediatric ADRs between 2008 and 2012 in the Adverse Events Reporting System database of the FDA and found that of the total pediatric ADRs reported, 32% were reported by medical doctors and 25% were reported by healthcare professionals [32]. However, the highest rate of ADR reporting in neonates and infants was from healthcare professionals [32] .
Numerous studies from different countries and cultures have pointed out the difficulties of nurses in reporting ADRs [24, 26, 33,34,35,36,37,38,39] and the underestimation of the knowledge of pharmacovigilance by them [35, 37, 38, 40, 41].
In this context, Pulford and Malcom [39] reported a survey conducted on healthcare professionals, including also practice and school nurses, in the Ayrshire and Arran regions of Scotland, with the aim to evaluate the knowledge of reporting vaccine ADRs and the attitudes among healthcare professionals on this issue. Although the majority of persons interviewed admitted that it was their responsibility to report suspected ADRs, less than 50% of the respondents declared a good knowledge of the ADR system [39]. Two Iranian studies highlight well the difficulties faced by nurses in terms of knowledge of, attitude to and practice of pharmacovigilance in hospitals [35, 38]. In the first study, conducted between March and October 2005, Hajebi and colleagues distributed a questionnaire to 150 nurses of a Tehran medical hospital on familiarity with pharmacovigilance before and after an ADR educational program [38]. Interestingly, the pharmacovigilance seminar training, which had the aim to increase nurse awareness and the knowledge of nurses, was found to be very effective, especially among female nurses, but it failed to have an impact on the reporting attitude of this professional healthcare category [38]. The authors concluded that there was a need to offer a continuous phamacovigilance educational program until the voluntary reporting of ADRs became a habitual behavior among the hospital nursing staff [38]. Four years later, Hanafi et al. [35] investigated the same issues (knowledge, attitude and practice of nurses towards ADRs) among a larger number of nurses (n distributed questionnaires = 500) in a university hospital of Tehran. About 91% of the interviewed nurses had never reported an ADR, although their attitude towards pharmacovigilance was high. Curiously, the major cause of under-reporting of suspected ADRs was an unawareness of the possibility to directly report the ADR to the national pharmacovigilance center. In this study also, the authors strongly recommended continuous lectures, seminars and/or workshops on pharmacovigilance [35]. A similar experience was reported in a tertiary care hospital in Ajman (United Arab Emirates) by John and colleagues in 2012 [36]. These authors observed a significant correlation between pharmacovigilance knowledge and attitude to reporting by nurses. However, the uncertainty of ADRs, the concern about a potentially wrong report and an inadequate knowledge of ADR reporting procedure were the barriers to pharmacovigilance activity by nurses. Again in this study, training in ADR reporting was considered by the authors to be a key measure to improve ADR reporting [36]. In their very recent study, Abu Hammour and colleagues [12] distributed 670 validated questionnaires, and the results demonstrated that there was a low level of awareness among nurses regarding pharmacovigilance in an Amman Hospital, but also that there was a strong will to report ADRs and to attend educational sessions on pharmacovigilance. Indeed, nurses with training in reporting ADRs are better able to deal with ADRs because they are more likely to have proper pharmacovigilance knowledge and practices, as demonstrated by Masika et al. in Kenya [42]. Nonetheless, there are also examples of a good knowledge of pharmacovigilance among nurses. Rehan and co-workers reported encouraging data from an Indian study in which 100 nurses were interviewed on their awareness of the existing national pharmacovigilance program [37]. Of these 100 nurses, 75% nurses were well aware of how and where to report ADRs, although 96% felt the need for additional information on drugs causing ADRs and their management [37].
In this context, it is essential to include pharmacovigilance training in nurse undergraduate and graduate education programs, as highlighted by the study of Alan et al. [33]. Ekman and colleagues [40] suggested that the reasons for this trend to under-reporting is related to various factors, such as uncertainty regarding how and what to report, difficulty in finding the correct forms, lack of time or just because physicians suggest no need to report the observed ADR. The results from a questionnaire distributed to 753 nurses revealed that only 15% had ever received, during their professional career, some form of education on how and when to make an ADR report and that only 14% had reported at least one ADR. However, almost 90% of the interviewed nurses said they would be interested in training courses on pharmacovigilance as part of their continuing professional training [40]. Salk and colleagues [43] assessed the attitudes of usage of the U.S. FDA Adverse Event Reporting System (FAERS) among gastroenterology nurse practitioners and physician assistants. Although 98% of the nurse practitioners considered reporting ADRs an important issue in patient safety, only 46% were familiar with the FAERS. Moreover, only 20% of nurse practitioners and 9% of physician assistants had learned about the FAERS in their academic education [43].
Discussion
Economic impact of pharmacovigilance
Adverse drug reactions cause between 3 and 6% of total admissions in healthcare facilities [44], and it has been estimated that during a hospitalization, between 6 and 10% of patients experience at least one adverse reaction [45]. Based on these data, ADRs are a major source of costs to national health systems. In 1997, the annual costs due to ADRs in a U.S. university hospital of 700 beds were estimated at around 5.6 million dollars [46], whereas it has been estimated that the UK will spend 706 million euros each year for extended hospital stays due to ADRs [47]. Sultana and colleagues stated that the impact and the management of ADRs in the USA may cost up to 30.1 billion dollars annually [48]. Increased costs due to ADRs are usually due to higher number of hospitalizations, prolongation of hospital stay and additional clinical investigations in more serious cases. In 2011, Stark et al. calculated the economic burden of ADEs in Germany to be a mean cost per patient of 381 euros, with total healthcare costs related to ADEs of 816 million euros [49]. A recent Chinese study quantified the total socioeconomic cost of 2739 ADR cases which occurred at the First Affiliated Hospital of Bengbu Medical College to be ¥817,401.69 (US$118,292 in March 2017), with direct costs of ¥603252.81 (US$87,301 in March 2017) and indirect costs of ¥214148.88 (US$ 30,992 in March 2017) [50].
Under-reporting of ADRs
Based on the published articles included in this review, we believe that a common problem in pharmacovigilance is the under-reporting of ADRs, also by nurses. Among the explanations put out for this widespread underestimation of pharmacovigilance by nurses, we suggest that there are at least two important points to underline: (1) the limited awareness by nurses of their key professional role in pharmacovigilance and (2) nurses’ own belief that they have inadequate pharmacology knowledge to identify an ADR. Thus, we find it reasonable to suggest that an opportunity for nurses to refresh their knowledge of pharmacology should be provided in order to increase ADR reporting among this healthcare professional category. In our experience, nurses with longer professional experience (who are usually more independent and self-confident) are more familiar with the existing reporting regulations than those with limited experience, also because they have prior reporting experiences. Although no exact estimate of patient reporting is available, it is considered that 95% of healthcare professionals do not report ADRs [3]. In a study by Hazell and colleagues, the median under-reporting rate across 37 studies, using a wide variety of surveillance methods from 12 different countries, was 94% (interquartile range 82–98%), with no significant difference in the under-reporting rates calculated for general practice and hospital-based studies [2]. Palleria and colleagues have recently listed the causes of this major drawback to the pharmacovigilance system, including the incorrect beliefs that (1) very serious ADRs are always well documented by the time a drug is marketed, (2) it is nearly impossible to determine whether a drug is responsible for a ADR and (3) a single case that an individual physician might observe could not contribute to medical knowledge [51]. The fear of legal consequences and the lack of time to complete the forms are other factors associated to under-reporting [51].
Clinical or community health nurses and pharmacovigilance
Proximity to patients and community
In the context of pharmacovigilance, an important duty of nurses is to monitor and report ADRs, as stated, for example, by the United Kingdom Nursing and Midwifery Council [52], because of their privileged position to observe, relate and document possible ADRs. In our view, the prevention of ADRs is a key aspect of pharmacovigilance, and the community health nurse may be major actors in this field and not simply extras because they practice in diverse settings, such as community nursing centers, local and state health departments, home health agencies, schools and neighborhood centers. A community health nurse works within the community to improve the overall health of the members of that community. Thus, we consider that direct involvement of these nurses in the practice of spontaneous reporting of ADRs is vital for an efficient pharmacovigilance system. Indeed, community health nurses may provide a unique role within the community by spontaneously reporting the ADRs of drugs such as OTC drugs, which are rarely reported by physicians or clinical nurses. OTC drugs are sold directly to the consumer, but they are not free from causing possible serious ADRs.
Global vision of therapeutic remedies and their ADRs
We also strongly believe that the community health nurse may play a major role in the spontaneous reporting of ADRs after the administration of phytotherapies or complementary and alternative medicine remedies, which are increasingly being used within communities. The use of these compounds is usually not reported by consumers to either their physician or pharmacist. The adverse reactions or pharmacological drug interactions of these types of remedies should not be underestimated, but the current lack of information on this issue is a widespread problem [53]. It is a common belief that herbal remedies have no or fewer side effects than conventional drugs, based on the belief that natural remedies are relatively safe and can be used with less care [54]. Our premise is that community health nurses should concomitantly increase and encourage spontaneous reporting of these remedies, with the aim to help raise the awareness of consumers and patients about the risk–benefit profile of these complementary and alternative drugs.
The impact on community health
The main purpose of reporting an adverse event is to learn from the experience and share that experience with the community so that others can avoid the same unwanted event [55]. We believe that also the community health nurse may contribute greatly to this important concept by (1) facilitating the methods of reporting inside public health facilities, departments or schools; (2) educating subjects and patients on drug safety and on the benefits that the spontaneous reporting system can bring to the community, both in terms of reducing the risk for patients and of saving resources to treat ADRs; (3) creating a permanent network of pharmacovigilance in local areas or communities with rapid availability of the system results (Fig. 2). Thus, in our opinion the role of community health nurse in pharmacovigilance is not limited only to an increased number of spontaneous reports of ADRs, which is a virtuous goal per se, but also to have an impact on the social health of communities through (1) the education of subjects about ADR reports, (2) the creation of a network with other healthcare professionals and, above all, (3) enforcing legislative measures or sanitary precautions made by governments based on an increased number of pharmacovigilance alarms.
Conclusions
Unfortunately, to our knowledge, little data have been published on the number of pharmacovigilance reports made by clinical nurses and there are no articles on such reports made by community health nurses. This lack of information should encourage all of the main actors in the pharmacovigilance process to deeply and urgently investigate this issue and, above all, to better describe their possible specific role in the pharmacovigilance systems. A strong increase in the number of ADR reports and an increase in active research on pharmacovigilance by clinical and community health nurses are needed and highly desirable in order to cover as much as possible any signal of an adverse event by new compounds, OTC drugs and complementary or alternative remedies in the community, thereby preventing any future ADR. Therefore, the improvement of health in the community is also related to the key role of both clinical and community health nurses in pharmacovigilance systems. Increased reporting of ADRs, the education of subjects and the establishment of a community pharmacovigilance network can only strengthen the precautions made by governments based on pharmacovigilance alarms.
References
Shepherd G, Mohorn P, Yacoub K, May DW (2012) Adverse drug reaction deaths reported in United States vital statistics, 1999-2006. Ann Pharmacother 46(2):169–175. http://dx.doi.org/10.1345/aph.1P592
Hazell L, Shakir SA (2006) Under-reporting of adverse drug reactions: a systematic review. Drug Saf 29(5):385–396
Al Dweik R, Stacey D, Kohen D, Yaya S (2016) Factors affecting patient reporting of adverse drug reactions: a systematic review. Br J Clin Pharmacol 83(4):875–883. http://dx.doi.org/10.1111/bcp.13159
Bouvy JC, De Bruin ML, Koopmanschap MA (2015) Epidemiology of adverse drug reactions in Europe: a review of recent observational studies. Drug Saf 38(5):437–453. http://dx.doi.org/10.1007/s40264-015-0281-0
Pillans PI (2008) Clinical perspectives in drug safety and adverse drug reactions. Expert Rev Clin Pharmacol 1(5):695–705. http://dx.doi.org/10.1586/17512433.1.5.695
Morrison-Griffiths S, Pirmohamed M (2000) Specialist nurse reporting of adverse drug reactions. Prof Nurse 15(5):300–304
Morrison-Griffiths S, Walley TJ, Park BK, Breckenridge AM, Pirmohamed M (2003) Reporting of adverse drug reactions by nurses. Lancet 361(9366):1347–1348. http://dx.doi.org/10.1016/s0140-6736(03)13043-7
O'Malley PA (2012) Preventing and reporting adverse drug events: pharmacovigilance for the clinical nurse specialist. Clin Nurse Spec 26(3):136–137. http://dx.doi.org/10.1097/NUR.0b013e31825317c4
Gurwitz JH, Field TS, Avorn J, McCormick D, Jain S, Eckler M, Benser M, Edmondson AC, Bates DW (2000) Incidence and preventability of adverse drug events in nursing homes. Am J Med 109(2):87–94
Griffith R (2013) Nurses must report adverse drug reactions. Br J Nurs 22(8):484–485. http://dx.doi.org/10.12968/bjon.2013.22.8.484
De Angelis A, Pancani L, Steca P, Colaceci S, Giusti A, Tibaldi L, Alvaro R, Ausili D, Vellone E (2017) Testing an explanatory model of nurses' intention to report adverse drug reactions in hospital settings. J Nurs Manag 25(4):307–317. http://dx.doi.org/10.1111/jonm.12467
Abu Hammour K, El-Dahiyat F, Abu Farha R (2017) Health care professionals knowledge and perception of pharmacovigilance in a tertiary care teaching hospital in Amman, Jordan. J Eval Clin Pract 23(3):608–613. http://dx.doi.org/10.1111/jep.12683
Kulbok PA, Thatcher E, Park E, Meszaros P (2012) Evolving public health nursing roles: focus on community participatory health promotion and prevention. Online J Issues Nurs 17(2):1
Swider SM, Levin PF, Kulbok PA (2015) Creating the future of public health nursing: a call to action. Public Health Nurs 32(2):91–93. http://dx.doi.org/10.1111/phn.12193
Rydberg DM, Holm L, Engqvist I, Fryckstedt J, Lindh JD, Stiller CO, Asker-Hagelberg C (2016) Adverse drug reactions in a tertiary care emergency medicine ward—prevalence, preventability and reporting. PLoS One 11(9):e0162948. http://dx.doi.org/10.1371/journal.pone.0162948
Parameswaran Nair N, Chalmers L, Connolly M, Bereznicki BJ, Peterson GM, Curtain C, Castelino RL, Bereznicki LR (2016) Prediction of hospitalization due to adverse drug reactions in elderly community-dwelling patients (The PADR-EC Score). PLoS One 11(10):e0165757. http://dx.doi.org/10.1371/journal.pone.0165757
Cliff-Eribo KO, Sammons H, Choonara I (2016) Systematic review of paediatric studies of adverse drug reactions from pharmacovigilance databases. Expert Opin Drug Saf 15(10):1321–1328. http://dx.doi.org/10.1080/14740338.2016.1221921
Pedros C, Formiga F, Corbella X, Arnau JM (2016) Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol 72(2):219–226. http://dx.doi.org/10.1007/s00228-015-1974-0
Kanagaratnam L, Drame M, Trenque T, Oubaya N, Nazeyrollas P, Novella JL, Jolly D, Mahmoudi R (2016) Adverse drug reactions in elderly patients with cognitive disorders: A systematic review. Maturitas 85:56–63. http://dx.doi.org/10.1016/j.maturitas.2015.12.013
van der Stelt CA, van der Windsant- V, Tweel AM, Egberts AC, van den Bemt PM, Leendertse AJ, Hermens WA, van Marum RJ, Derijks HJ (2016) The association between potentially inappropriate prescribing and medication-related hospital admissions in older patients: A nested case control study. Drug Saf 39(1):79–87. http://dx.doi.org/10.1007/s40264-015-0361-1
Kaufman G (2016) Polypharmacy: the challenge for nurses. Nurs Stand 30(39):52–60. http://dx.doi.org/10.7748/ns.30.39.52.s45
Hersberger KE, Messerli M (2016) Development of clinical pharmacy in Switzerland: involvement of community pharmacists in care for older patients. Drugs Aging 33(3):205–211. http://dx.doi.org/10.1007/s40266-016-0353-6
Yu YM, Shin WG, Lee JY, Choi SA, Jo YH, Youn SJ, Lee MS, Choi KH (2015) Patterns of adverse drug reactions in different age groups: analysis of spontaneous reports by community pharmacists. PLoS One 10(7):e0132916. http://dx.doi.org/10.1371/journal.pone.0132916
De Angelis A, Colaceci S, Giusti A, Vellone E, Alvaro R (2016) Factors that condition the spontaneous reporting of adverse drug reactions among nurses: an integrative review. J Nurs Manag 24(2):151–163. http://dx.doi.org/10.1111/jonm.12310
Mendes D, Alves C, Batel Marques F (2014) Nurses' spontaneous reporting of adverse drug reactions: expert review of routine reports. J Nurs Manag 22(3):322–330. http://dx.doi.org/10.1111/jonm.12003
Mendes Marques JI, Polonia JM, Figueiras AG, Costa Santos CM, Herdeiro MT (2016) Nurses' attitudes and spontaneous adverse drug reaction reporting: a case-control study in Portugal. J Nurs Manag 24(3):409–416. http://dx.doi.org/10.1111/jonm.12337
Karlsson SA, Jacobsson I, Boman MD, Hakkarainen KM, Lovborg H, Hagg S, Jonsson AK (2015) The impact of a changed legislation on reporting of adverse drug reactions in Sweden, with focus on nurses' reporting. Eur J Clin Pharmacol 71(5):631–636. http://dx.doi.org/10.1007/s00228-015-1839-6
Ulfvarson J, Mejyr S, Bergman U (2007) Nurses are increasingly involved in pharmacovigilance in Sweden. Pharmacoepidemiol Drug Saf 16(5):532–537. http://dx.doi.org/10.1002/pds.1336
Conforti A, Opri S, D'Incau P, Sottosanti L, Moretti U, Ferrazin F, Leone R (2012) Adverse drug reaction reporting by nurses: analysis of Italian pharmacovigilance database. Pharmacoepidemiol Drug Saf 21(6):597–602. http://dx.doi.org/10.1002/pds.3225
Aldea A, Garcia Sanchez-Colomer M, Fernandez Quintana E, Garcia Saiz M (2012) Paediatric adverse drug reactions reported to the Spanish Pharmacovigilance System from 2004 to 2009. Eur J Clin Pharmacol 68(9):1329–1338. http://dx.doi.org/10.1007/s00228-012-1255-0
Hall M, McCormack P, Arthurs N, Feely J (1995) The spontaneous reporting of adverse drug reactions by nurses. Br J Clin Pharmacol 40(2):173–175
Bigi C, Tuccori M, Bocci G (2017) Healthcare professionals and pharmacovigilance of pediatric adverse drug reactions: a 5-year analysis of Adverse Events Reporting System database of the Food and Drug Administration. Minerva Pediatr. http://dx.doi.org/10.23736/s0026-4946.17.04733-8
Alan S, Ozturk M, Gokyildiz S, Avcibay B, Karatas Y (2013) An evaluation of knowledge of pharmacovigilance among nurses and midwives in Turkey. Indian J Pharmacol 45(6):616–618. http://dx.doi.org/10.4103/0253-7613.121375
dos Santos Pernas SI, Herdeiro MT, Lopez-Gonzalez E, da Cruz e Silva OA, Figueiras A (2012) Attitudes of Portuguese health professionals toward adverse drug reaction reporting. Int J Clin Pharm 34(5):693–698. http://dx.doi.org/10.1007/s11096-012-9675-6
Hanafi S, Torkamandi H, Hayatshahi A, Gholami K, Javadi M (2012) Knowledge, attitudes and practice of nurse regarding adverse drug reaction reporting. Iran J Nurs Midwifery Res 17(1):21–25
John LJ, Arifulla M, Cheriathu JJ, Sreedharan J (2012) Reporting of adverse drug reactions: an exploratory study among nurses in a teaching hospital, Ajman, United Arab Emirates. Daru 20(1):44. http://dx.doi.org/10.1186/2008-2231-20-44
Rehan HS, Sah RK, Chopra D (2012) Comparison of knowledge, attitude and practices of resident doctors and nurses on adverse drug reaction monitoring and reporting in a tertiary care hospital. Indian J Pharmacol 44(6):699–703. http://dx.doi.org/10.4103/0253-7613.103253
Hajebi G, Mortazavi SA, Salamzadeh J, Zian A (2010) A survey of knowledge, attitude and practice of nurses towards pharamacovigilance in Taleqani Hospital. Iran J Pharm Res 9(2):199–206
Pulford A, Malcolm W (2010) Knowledge and attitudes to reporting adverse drug reactions. Br J Nurs 19(14):899–904. http://dx.doi.org/10.12968/bjon.2010.19.14.49048
Ekman E, Petersson G, Tagerud S, Backstrom M (2012) Awareness among nurses about reporting of adverse drug reactions in Sweden. Drug Healthc Patient Saf 4:61–66. http://dx.doi.org/10.2147/dhps.s31103
Ehrenpreis ED, Sifuentes H, Ehrenpreis JE, Smith ZL, Marshall ML (2012) Suboptimal reporting of adverse medical events to the FDA Adverse Events Reporting System by nurse practitioners and physician assistants. Expert Opin Drug Saf 11(2):177–183. http://dx.doi.org/10.1517/14740338.2012.650165
Masika CW, Atieli H, Were T (2016) Knowledge, perceptions, and practice of nurses on surveillance of adverse events following childhood immunization in Nairobi. Kenya. Biomed Res Int 2016:3745298. http://dx.doi.org/10.1155/2016/3745298
Salk A, Ehrenpreis ED (2016) Attitudes and usage of the Food and Drug Administration Adverse Event Reporting System among gastroenterology nurse practitioners and physician assistants. Gastroenterol Nurs 39(1):25–31. http://dx.doi.org/10.1097/sga.0000000000000193
Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM (2008) Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med 168(17):1890–1896. http://dx.doi.org/10.1001/archinternmed.2008.3
Davies EC, Green CF, Taylor S, Williamson PR, Mottram DR, Pirmohamed M (2009) Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS One 4(2):e4439. http://dx.doi.org/10.1371/journal.pone.0004439
Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, Small SD, Sweitzer BJ, Leape LL (1997) The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA 277(4):307–311
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 329(7456):15–19. http://dx.doi.org/10.1136/bmj.329.7456.15
Sultana J, Cutroneo P, Trifiro G (2013) Clinical and economic burden of adverse drug reactions. J Pharmacol Pharmacother 4[Suppl 1]:S73–S77. http://dx.doi.org/10.4103/0976-500x.120957
Stark RG, John J, Leidl R (2011) Health care use and costs of adverse drug events emerging from outpatient treatment in Germany: a modelling approach. BMC Health Serv Res 11:9. http://dx.doi.org/10.1186/1472-6963-11-9
Qing-ping S, Xiao-dong J, Feng D, Yan L, Mei-ling Y, Jin-xiu Z, Shu-qiang Z (2014) Consequences, measurement, and evaluation of the costs associated with adverse drug reactions among hospitalized patients in China. BMC Health Serv Res 14:73. http://dx.doi.org/10.1186/1472-6963-14-73
Palleria C, Leporini C, Chimirri S, Marrazzo G, Sacchetta S, Bruno L, Lista RM, Staltari O, Scuteri A, Scicchitano F, Russo E (2013) Limitations and obstacles of the spontaneous adverse drugs reactions reporting: Two "challenging" case reports. J Pharmacol Pharmacother 4[Suppl 1]:S66–S72. http://dx.doi.org/10.4103/0976-500x.120955
Nursing and Midwifery Council (NMC) (2017) Standards for medicines management. In: https://www.nmc.org.uk/standards/additional-standards/standards-for-medicines-management. Accessed 5 April 2017
Schjott J, Erdal H (2014) Questions about complementary and alternative medicine to the Regional Medicines Information and Pharmacovigilance Centres in Norway (RELIS): a descriptive pilot study. BMC Complement Altern Med 14:56. http://dx.doi.org/10.1186/1472-6882-14-56
Lynch N, Berry D (2007) Differences in perceived risks and benefits of herbal, over-the-counter conventional, and prescribed conventional, medicines, and the implications of this for the safe and effective use of herbal products. Complement Ther Med 15(2):84–91. http://dx.doi.org/10.1016/j.ctim.2006.06.007
Leape LL (2002) Reporting of adverse events. N Engl J Med 347(20):1633–1638. http://dx.doi.org/10.1056/NEJMNEJMhpr011493
Acknowledgments
The authors would like to thank Dr. Marco Tuccori.
Contributions of Authors statement
CB and GB participated in the conception of the study, the literature search, the planning of the review and in writing the entire text.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors did not receive financial support for this research.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Bigi, C., Bocci, G. The key role of clinical and community health nurses in pharmacovigilance. Eur J Clin Pharmacol 73, 1379–1387 (2017). https://doi.org/10.1007/s00228-017-2309-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2309-0