Abstract
Objectives
This study aimed to assess the prevalence, the change, and the determinants of change in polypharmacy in a population-based sample.
Methods
Baseline (2003–2006) and follow-up (2009–2012) data are from 4679 participants aged between 35 and 75 years (53.5% women, mean age 52.6 ± 10.6 years) from the population of Lausanne, Switzerland. Polypharmacy was defined by the regular use of ≥5 drugs. Four categories of change were defined: never (no polypharmacy at baseline and follow-up), initiating (no polypharmacy at baseline but at follow-up), maintaining, or quitting.
Results
Polypharmacy increased from 7.7% at baseline to 15.3% at follow-up. Cardiovascular drugs were the most prescribed medicines at baseline and follow-up. Gender, age, obesity, smoking, previously diagnosed hypertension, or diabetes or dyslipidemia were significantly and independently associated with initiating and maintaining polypharmacy.
Conclusion
In a population-based sample, prevalence of polypharmacy doubled over a 5.6-year period. The main determinants of initiating polypharmacy were age, overweight and obesity, smoking status, and previously diagnosed cardiovascular risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been a substantial increase in the prescribing of regular medicines in general populations [1]. Subsequently, prevalence of polypharmacy, referred as the simultaneous intake of five or more medications, has been increasing [2] not only among the elderly but also in other ages [3].
Polypharmacy is driven by the increase in age and multimorbidity [4]. Given the current aging of the population and the number of drugs needed to treat age-associated multimorbidity, it is expected that the prevalence of patients on polypharmacy will continue to increase. Polypharmacy can increase the risk of drug-disease interaction in addition to drug-drug interactions; however, polypharmacy may, in many cases such as multimorbidity, be entirely appropriate and inevitable [5,6,7].
Although polypharmacy has become more widespread in recent years, determinants of change in polypharmacy status in longitudinal study are not well studied. Thus, this study aimed (1) to assess the prevalence and the change of polypharmacy and (2) to examine the determinants of change in polypharmacy status as initiation or quitting.
Materials and methods
Study population and design
The CoLaus study is an ongoing prospective survey investigating the biological and genetic determinants of cardiovascular risk factors (CVRFs) and cardiovascular disease (CVD) in the population of Lausanne, Switzerland. The study was approved by the Institutional Ethics Committee of the University of Lausanne (decision reference 33/09). Detailed descriptions of the study design have been reported elsewhere [8]. A simple, non-stratified random sample of the Lausanne population aged between 35 and 75 years was drawn. Inclusion criteria were (a) written informed consent and (b) willingness to take part in the examination and to provide blood samples. Recruitment began in June 2003 and ended in May 2006 and included 6733 participants, with a participation rate of 41%. The baseline evaluation included an interview, a physical exam, blood sampling, and a set of questionnaires. As illustrated in supplemental Fig. 1, of the initial 6733 participants, 6184 (91.8%) provided extended data on their medicines. The follow-up visit was similar to the baseline evaluation and was performed between April 2009 and September 2012, 5.5 years on average after the baseline, and included 5064 participants (75.2% of the initial sample), 4679 of which (69.5% of the initial sample) had complete medication data at baseline and follow-up.
Lifestyle and clinical and biological parameters
Lifestyle factors, CVD, and medication status were assessed by questionnaire. Smoking status was categorized into never, former, and current as reported. Educational level was categorized as low (obligatory school or apprenticeship), medium (high school), or high (university degree). Height and weight were assessed with the participants in light clothes and without shoes using a Seca® scale; body mass index (BMI) was categorized as normal (18.5 < BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), and obese (≥30 kg/m2). As the number of underweight (BMI ≤ 18.5 kg/m2) participants was small, they were included in the normal weight group.
Blood pressure was measured thrice on the right arm, after a rest of at least 10 min in the seated position using an Omron® HEM-907 automated oscillometric sphygmomanometer. The average of the last two blood pressure measurements was used for analyses.
Venous blood samples were drawn after an overnight fast. Clinical chemistry assays were performed at the central laboratory of the University Hospital of Lausanne (CHUV). Total cholesterol, HDL-cholesterol, triglycerides (TGs), and glucose were measured using commercial reagents; low-density lipoprotein (LDL-C) was calculated using the Friedewald formula if TG < 4.6 mmol/L.
For each condition (hypertension, dyslipidemia, or diabetes), three categories were defined: (1) absent (neither reported nor newly diagnosed at the baseline examination), (2) reported by the participant, and (3) newly diagnosed at the baseline examination among participants not reporting the condition (supplemental Fig. 2). Newly diagnosed hypertension was defined as a systolic BP (SBP) ≥140 mmHg and/or a diastolic BP (DBP) ≥90 mmHg [9]. Newly diagnosed dyslipidemia was defined as a total cholesterol >6.5 mmol/L and/or LDL-cholesterol >4.1 mmol/L and/or triglycerides >2.0 mmol/L [10]. Newly diagnosed diabetes was defined as a fasting plasma glucose >7 mmol/L [11].
Definitions of polypharmacy and polypharmacy changing status
Participants indicated which medicines they were currently taking. Medicines were coded according to the Anatomical Therapeutics Chemical (ATC) Classification System of the World Health Organization. Medicines were considered if they existed in the ATC; only medications listed in the official Swiss pharmacopeia (compendium.ch) were considered. Other complementary medicines such as non-official phytotherapies, dietary supplements (i.e., shark cartilage, Bach’s flowers), or homeopathy were not considered. Polypharmacy was defined as the use of five or more medicines, including OTC drugs, regardless if a medicine contained one or more effective drugs (i.e., fixed dose combinations) [12].
Changing of polypharmacy status was defined as never (no polypharmacy at baseline and follow-up), initiation (no polypharmacy at baseline but at follow-up), quitting (polypharmacy at baseline but not at follow-up), and maintaining (polypharmacy at baseline and follow-up).
Statistical analysis
Statistical analysis was performed using Stata software version 14.1 (Stata Corp., College Station, TX, USA). Descriptive results were expressed as mean ± standard deviation (SD) or as the number of participants (percentage). Bivariate analysis was performed using chi-squared test for categorical variables and Kruskal-Wallis non-parametric test for age. Multivariate analysis was performed using multinomial (polytomous) logistic regression, and results were expressed as multivariate-adjusted relative risk ratios (RRRs) and 95% confidence interval (CI). Models were adjusted for gender, age groups ([35–50[, [50–65[, and [65–75]), BMI categories (normal, overweight, and obese), educational level (low, middle, high), marital status (living in couple, living alone), country of birth (Switzerland vs. other), smoking categories (never, former, current), being physically active (yes vs. no), hypertension (never, previously diagnosed, and newly diagnosed), dyslipidemia (never, previously diagnosed, and newly diagnosed), and diabetes (never, previously diagnosed, and newly diagnosed). Statistical significance was considered for a two-tailed test with P < 0.05.
As some drugs could combine several pharmacologically different active substances, we ran several sensitivity analyses by checking ATC codes corresponding to combinations of different active substances (supplementary Table 1), excluding combinations of vitamins and minerals (ATC codes A11A, A11C, A11D, A11E, A11G¸ A11J, A12AX, B03AD, and B03AE). As ATC codes were defined with a maximum of five letters in the baseline survey, the same categorization was applied in the follow-up. Categories of “polyactive substances” were defined similarly to polypharmacy, i.e., 0–4 and 5 or more active substances. The same procedure was applied to define categories of change in polyactive substances: never (no polyactive substances at baseline and follow-up), initiation (no polyactive substances at baseline but at follow-up), quitting (polyactive substances at baseline but not at follow-up), and maintaining (polyactive substances at baseline and follow-up). Age-adjusted analyses were conducted using standardization based on the Lausanne population distribution for 2003, obtained from the Canton statistical office http://www.stat.vd.ch/Default.aspx?DocID=7818&DomId=2783. As some age groups initially present at baseline no longer existed at follow-up, calculations were based on age range 40–75, which is common for both baseline and follow-up periods. As no information was available regarding the total number of comorbidities, we used the number of medicines at baseline (categorized into three groups 0–1, 2–3, and 4 or more) as a proxy for adjustment. Two analyses were performed: one on polypharmacy and another on polyactive substances.
Results
Selection and characteristics of participants
The demographic, clinical and functional characteristics of the participants included and excluded are summarized in Supplemental Table 2. Excluded participants were more frequently men, not born in Switzerland, obese, current smokers, and with lower education.
Prevalence of medicines and polypharmacy
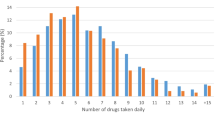
Prevalences of polypharmacy status and of the main drugs at baseline and follow-up (FU) are summarized in Table 1. Polypharmacy increased from 7.7% at baseline to 15.3% at follow-up. Cardiovascular drugs were the most prescribed medicines, both at baseline and follow-up; among cardiovascular drugs, hypolipidemic drugs and statins were the most frequent ones.
Changes and determinants in polypharmacy status
The changes in the polypharmacy status and determinants of changes are presented in Supplemental Table 3 (bivariate analysis) and Table 2 (multivariate analysis). Four hundred fifteen participants (9.6%) initiated; 263 (5.6%) maintained, and only 97 (2.1%) quitted polypharmacy, while 3868 (82.7%) were not on polypharmacy neither at baseline nor at follow-up.
Bivariate analysis showed gender, age, BMI categories, education level, living alone, smoking status, and known hypertension, dyslipidemia, and diabetes to be associated with a change in polypharmacy status. Multivariate analysis indicated that being male and older were associated with any change in polypharmacy status, while overweight and obesity were only associated with initiation and maintaining polypharmacy status. Smoking (current or former) was associated with the initiation of polypharmacy, but only current smoking was associated with maintaining polypharmacy status. Known hypertension was associated with initiating and maintaining polypharmacy status, while no association was found with hypertension diagnosed at baseline. Known dyslipidemia was associated with maintaining polypharmacy status, while no association was found with dyslipidemia diagnosed at baseline. Both known diabetes and diabetes diagnosed at baseline were associated with initiating or maintaining polypharmacy status.
Sensitivity analyses
The crude prevalence rates of polyactive substance use were 8.9 and 17.1% at baseline and follow-up, respectively. The corresponding age-standardized rates for polypharmacy were 8.6% at baseline and 9.6% at follow-up; for polyactive substances, the rates were 9.9 and 13.9%, respectively. The results of the multivariate analysis using change in polyactive substances are provided in supplementary Table 4. Similar associations were found as for polypharmacy.
When the analysis was adjusted for the number of medicines at baseline, similar results were obtained for polypharmacy regarding the determinants of initiation; for maintenance, significant associations persisted for age, BMI categories, and known hypertension, dyslipidemia, and diabetes, while for quitting, all determinants were no longer significant (supplementary Table 5). Finally, for polyactive substances, most determinants of initiation remained significant; for maintenance, significant associations persisted for age, BMI categories, and known hypertension and diabetes, while for quitting, all determinants were no longer significant (supplementary Table 6).
Discussion
In this study, we assessed the baseline determinants of changes in polypharmacy such as BMI, smoking, and presence of specific comorbidities, and we found an absolute increase from 7.7 to 15.3% in polypharmacy over 5.6 years.
Prevalence of medicines and polypharmacy
Cardiovascular drugs were the most prescribed medicines, both at baseline and follow-up. This finding is consistent with a study in a Scottish primary care population [13]. Indeed, cardiovascular drugs not only constitute the greatest part of medicines taken by the population but are also a strong predictor of polypharmacy [14].
Among cardiovascular drugs, hypolipidemic drugs and statins were the most frequent ones and their prevalence almost doubled between baseline and follow-up. Importantly, this increase in hypolipidemic drugs is lower than the increase in dyslipidaemia prevalence [15]. Nevertheless, this doubling of hypolipidemic drugs between baseline and follow-up, with one fifth of participants taking them, is in line with a study conducted in Ireland [1] and also with a wider acceptance of preventive medication for the general population [16]. Contrary to USA, there is no consensus regarding guidelines for cardiovascular prevention in Switzerland. Several equations are used. This lack of consensus could explain a lower statin prescription [17].
Changes and determinants in polypharmacy status
Polypharmacy literally doubled from 7.7% at baseline to 15.3% at follow-up, a finding also observed in the USA (8.2% in 1999–2000 to 15% in 2011–2012) [18]. Although some participants quitted polypharmacy, initiating polypharmacy was more than 4.5-fold more frequent than quitting. Male gender was significantly associated with a lower likelihood of initiating, quitting, or maintaining polypharmacy. A possible explanation is that men utilize less frequently preventive care services than women [19], which would preclude the timely detection of diseases and therefore their treatment. Nevertheless, the effect of gender in polypharmacy changes should be further explored.
Increased age was significantly and positively associated with initiating, quitting, or maintaining polypharmacy. The increased age-related morbidity is the most obvious explanation for the initiation and maintenance, while the avoidance of any possible drug-drug interaction as well as the limited life expectancy in older adults might explain the positive association with quitting, as discussed in a systematic review [20].
Increased body mass index and current smoking were significantly and positively associated with initiating and maintaining polypharmacy status. Also, similar to our finding, obese subjects had significantly more exposure to multiple drug treatments in population-based studies in Italy and Greece [21, 22]. This might be partly due to the increased number of cardiovascular risk factors among obese subjects [23], although other diseases such as arthrosis and sleep disorders might also contribute to the increased number of drugs in this group. Regarding smoking, in the Greek study, smokers were almost three times more likely to take four or more drugs [22]. Again, a higher prevalence of smoking-associated diseases such as chronic obstructive pulmonary disease might contribute. Unfortunately, no data regarding non-cardiovascular diseases was collected in the CoLaus study to confirm these hypotheses. The most likely explanation is an increased occurrence of obesity-associated and smoking-associated pathologies and corresponding medication. Overall, our results suggest that quitting smoking and preventing obesity might be interesting solutions to decrease the prevalence of polypharmacy.
Consistent with the high prevalence of cardiovascular drugs, participants previously diagnosed with hypertension, dyslipidemia, and diabetes had a higher likelihood of initiating or maintaining polypharmacy status. Similarly, a study conducted in Spain showed that hypertension or dyslipidemia, combined with other medications for the treatment of diabetes or other cardiovascular pathologies, could be considered as a pattern of polypharmacy [24]. However, newly diagnosed risk factors had no effect (with the exception of newly diagnosed diabetes for initiation of polypharmacy). The association with maintenance of polypharmacy was expected, as cardiovascular risk factors need a chronic, lifetime treatment [25]. The fact that existing cardiovascular risk factors were also associated with initiating polypharmacy was less expected, but consistent with the fact that treatment escalation is frequently necessary to maintain acceptable levels. Conversely, only newly diagnosed diabetes was significantly associated with initiating polypharmacy, which is consistent with a longitudinal study in Netherlands indicating that diabetes was a strong predictor of polypharmacy [26]. Interestingly, most of the factors associated with polypharmacy (obesity, hypertension, dyslipidemia, and diabetes) are components of the metabolic syndrome. Hence, our results suggest that participants with metabolic syndrome would be at high risk of polypharmacy. Indeed, a cross-sectional study conducted in Nancy (France) showed people with metabolic syndrome to have a 3.17 higher likelihood of presenting with polypharmacy (≥4 drugs) [27].
Sensitivity analyses
A significant number of drugs contain several active substances; a sensitivity analysis was conducted taking into account the number of active substances rather than the number of drugs (pills) taken. Considering only the number of drugs might underestimate the effect of polypharmacy, and indeed, the prevalence rate of participants taking at least five active substances was higher by approximately 2% than the rate based on drugs. Hence, it is likely that most prevalence rates reported using the number of drugs (pills) are also underestimated, but the magnitude of the underestimation will depend on the availability of drugs with several active substances.
Interestingly, the main determinants of change in the number of active substances were similar to those for polypharmacy. The same findings were obtained after adjusting for the number of medicines at baseline; for instance, age, BMI categories, and known cardiovascular risk factors were positively associated with initiation and maintenance. Hence, our results suggest that, contrary to the prevalence rates, the determinants of polypharmacy and of polyactive substances are identical and that age and BMI categories are the main drivers of initiating and maintaining polypharmacy or polyactive substances. Given the aging and the increase in BMI of the worldwide population, our results suggest that the prevalence of polypharmacy or polyactive substances will considerably increase in the near future. Still, studies assessing both polypharmacy and polyactive drugs in the general population are missing, and it would be of interest that our results be replicated in other settings.
Strengths and limitations
The major strength of this study is that it is one of the few prospective studies assessing the determinants of change in polypharmacy in a population-based sample. This study has also some limitations. First, participation rate was low (41%), but in line with other epidemiological studies [28]. Second, recall bias might occur, as participants might have indicated only the most important medications. Hence, polypharmacy prevalences might be underestimated. Still, our results provide a conservative estimation of the already considerable prevalence (15% at follow-up) of polypharmacy in this group. Also, recent studies suggest that self-reported medication use closely relates with pharmacy records [29]; hence, recall bias might be reduced.
Conclusion
In a population-based sample, prevalence of polypharmacy doubled over a 5.6-year period. The main determinants of initiating polypharmacy were age, overweight and obesity, smoking status, and previously diagnosed cardiovascular risk factors.
References
Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T (2015) Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 5(9):e008656
Gnjidic D, Hilmer SN, Blyth FM, Naganathan V, Waite L, Seibel MJ, McLachlan AJ, Cumming RG, Handelsman DJ, Le Couteur DG (2012) Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol 65(9):989–995
Arnoldo L, Cattani G, Cojutti P, Pea F, Brusaferro S (2016) Monitoring polypharmacy in healthcare systems through a multi-setting survey: should we put more attention on long term care facilities? J Public Health Res 5(3)
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B (2012) Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380(9836):37–43
Hughes CM, Cooper JA, Ryan C (2014) Going beyond the numbers—a call to redefine polypharmacy. Br J Clin Pharmacol 77(6):915–916
Payne RA, Abel GA, Avery AJ, Mercer SW, Roland MO (2014) Is polypharmacy always hazardous? A retrospective cohort analysis using linked electronic health records from primary and secondary care. Br J Clin Pharmacol 77(6):1073–1082
Lindblad CI, Hanlon JT, Gross CR, Sloane RJ, Pieper CF, Hajjar ER, Ruby CM, Schmader KE, Panel MC (2006) Clinically important drug-disease interactions and their prevalence in older adults. Clin Ther 28(8):1133–1143
Firmann M, Mayor V, Vidal PM, Bochud M, Pecoud A, Hayoz D, Paccaud F, Preisig M, Song KS, Yuan X, Danoff TM, Stirnadel HA, Waterworth D, Mooser V, Waeber G, Vollenweider P (2008) The CoLaus study: a population-based study to investigate the epidemiology and genetic determinants of cardiovascular risk factors and metabolic syndrome. BMC Cardiovasc Disord 8:6. doi:10.1186/1471-2261-8-6
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA (2013) 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219. doi:10.1093/eurheartj/eht151
Moser M, Gencer B, Rodondi N (2014) Recommendations for management of dyslipidemia in 2014. Rev Med Suisse 10 (420):518, 520-514
Association AD (2014) Diagnosis and classification of diabetes mellitus. Diabetes care 37 (Supplement 1):S81-S90
Viktil KK, Blix HS, Moger TA, Reikvam A (2007) Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br J Clin Pharmacol 63(2):187–195. doi:10.1111/j.1365-2125.2006.02744.x
Payne RA, Avery AJ, Duerden M, Saunders CL, Simpson CR, Abel GA (2014) Prevalence of polypharmacy in a Scottish primary care population. Eur J Clin Pharmacol 70(5):575–581. doi:10.1007/s00228-013-1639-9
Volpe M, Chin D, Paneni F (2010) The challenge of polypharmacy in cardiovascular medicine. Fundam Clin Pharmacol 24(1):9–17. doi:10.1111/j.1472-8206.2009.00757.x
Antiochos P, Marques-Vidal P, Waeber G, Vollenweider P (2015) Five year trends in dyslipidaemia prevalence and management in Switzerland: the CoLaus study. Nut Metab Cardiovasc Dis: NMCD 25(11):1007–1015. doi:10.1016/j.numecd.2015.07.011
Goldacre B, Smeeth L (2014) Mass treatment with statins. BMJ (Clinical research ed) 349:g4745
Stewart J, Manmathan G, Wilkinson P (2017) Primary prevention of cardiovascular disease: a review of contemporary guidance and literature. JRSM Cardiovasc Dis 6:2048004016687211. doi:10.1177/2048004016687211
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL (2015) Trends in prescription drug use among adults in the United States from 1999-2012. JAMA 314(17):1818–1831. doi:10.1001/jama.2015.13766
Vaidya V, Partha G, Karmakar M (2012) Gender differences in utilization of preventive care services in the United States. J Women's Health (Larchmt) 21(2):140–145. doi:10.1089/jwh.2011.2876
Jokanovic N, Tan EC, Dooley MJ, Kirkpatrick CM, Bell JS (2015) Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc 16 (6):535. e531-535. e512
Degli Esposti E, Sturani A, Valpiani G, Di Martino M, Ziccardi F, Rita Cassani A, Baraccani C, Gentile M, Puglia MG, Degli Esposti L (2006) The relationship between body weight and drug costs: an Italian population-based study. Clin Ther 28(9):1472–1481. doi:10.1016/j.clinthera.2006.09.016
Pappa E, Kontodimopoulos N, Papadopoulos AA, Tountas Y, Niakas D (2011) Prescribed-drug utilization and polypharmacy in a general population in Greece: association with sociodemographic, health needs, health-services utilization, and lifestyle factors. Eur J Clin Pharmacol 67(2):185–192. doi:10.1007/s00228-010-0940-0
Davin C, Vollenweider P, Waeber G, Paccaud F, Marques-Vidal P (2012) Cardiovascular risk factors attributable to obesity and overweight in Switzerland. Nutr Metab Cardiovasc Dis 22(11):952–958. doi:10.1016/j.numecd.2011.01.004
Calderon-Larranaga A, Gimeno-Feliu LA, Gonzalez-Rubio F, Poblador-Plou B, Lairla-San Jose M, Abad-Diez JM, Poncel-Falco A, Prados-Torres A (2013) Polypharmacy patterns: unravelling systematic associations between prescribed medications. PLoS One 8(12):e84967. doi:10.1371/journal.pone.0084967
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WM (2016) 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 37(29):2315–2381. doi:10.1093/eurheartj/ehw106
Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM (2000) The development of polypharmacy. A longitudinal study. Fam Pract 17(3):261–267
Husson N, Watfa G, Laurain MC, Perret-Guillaume C, Niemier JY, Miget P, Benetos A (2014) Characteristics of polymedicated (>/= 4) elderly: a survey in a community-dwelling population aged 60 years and over. J Nutr Health Aging 18(1):87–91. doi:10.1007/s12603-013-0337-8
Galea S, Tracy M (2007) Participation rates in epidemiologic studies. Ann Epidemiol 17(9):643–653. doi:10.1016/j.annepidem.2007.03.013
Drieling RL, LaCroix AZ, Beresford SA, Boudreau DM, Kooperberg C, Heckbert SR (2016) Validity of self-reported medication use compared with pharmacy records in a cohort of older women: findings from the Women's Health Initiative. Am J Epidemiol 184(3):233–238. doi:10.1093/aje/kwv446
Author information
Authors and Affiliations
Contributions
NA wrote most of the manuscript. PMV collected data, made the statistical analysis, and reviewed the manuscript for important intellectual content. JC designed the study and reviewed the manuscript for important intellectual content. PV and GW revised the manuscript for important intellectual content. PMV had full access to the data and is the guarantor of the study. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The CoLaus study was and is supported by research grants from GlaxoSmithKline, the Faculty of Biology and Medicine of Lausanne, and the Swiss National Science Foundation (grants 33CSCO-122661, 33CS30-139468, and 33CS30-148401). Nazanin Abolhassani is supported by an excellence scholarship from the Swiss Federal Government (Reference No. 2016.1098). The funding sources had no contribution to the study design, analysis, and interpretation, as well as writing the report and decision to submit the article for publication.
Electronic supplementary material
Supplementary 1
(DOCX 28 kb)
Supplemental table 2
(DOCX 26 kb)
Supplemental table 3
(DOCX 29 kb)
Supplementary table 4
(DOCX 29 kb)
Supplementary table 5
(DOCX 29 kb)
Supplementary table 6
(DOCX 29 kb)
Supplemental figure 1
(DOCX 31 kb)
Supplemental figure 2
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Abolhassani, N., Castioni, J., Marques-Vidal, P. et al. Determinants of change in polypharmacy status in Switzerland: the population-based CoLaus study. Eur J Clin Pharmacol 73, 1187–1194 (2017). https://doi.org/10.1007/s00228-017-2288-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2288-1