Abstract
Purpose
Citalopram is a selective serotonin reuptake inhibitor (SSRI) antidepressant that is widely used in clinical practice. Recent data have indicated that high therapeutic citalopram doses may cause electrocardiographic abnormalities, and the regulatory authorities have amended its licenced dosage. The present manuscript reviews the available data concerning citalopram and cardiac toxicity.
Methods
Published data concerning the cardiac effects of citalopram were ascertained, and clinical data were considered separately between adverse effects arising from therapeutic use versus toxicity in the setting of intentional overdose.
Results
The occurrence of electrocardiographic abnormalities has long been recognised as a complication of acute citalopram overdose; a dose-effect relationship for QT prolongation has been described in a number of large case series, including several cases of torsades de pointes. In contrast, few data indicate the occurrence of QT prolongation and arrhythmia after therapeutic doses, and a dose-effect relationship within the therapeutic range has only recently been established. Citalopram is more likely to cause QT prolongation in patients with metabolic disturbance or pre-existing cardiac disease.
Conclusions
A dose-effect relationship for QT prolongation exists across a broad range of citalopram doses, such that caution must be exercised when prescribing high doses or if there are co-existent risk factors for QT effects. The available data illustrate how clinical toxicity data may offer an earlier signal of cardiac effects than ascertained from conventional pharmacovigilance methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Citalopram (Celexa®, Cipramil®) is a widely prescribed selective serotonin reuptake inhibitor (SSRI) that is licensed for use in depressive illness and panic disorder. Recent concerns have been raised about the risk of adverse cardiac effects of citalopram, specifically related to QT prolongation on the electrocardiograph (ECG). In August 2011, the Food and Drug Administration (FDA) issued a safety bulletin advising healthcare professionals and patients that citalopram should no longer be used in doses greater than 40 mg daily, or 20 mg daily in patients >60 years or with established hepatic impairment [1]. An update in March 2012 stated that citalopram should be discontinued in patients with persistent QTc (QT corrected for the effect of heart rate) greater than 500 ms [2]. Similar safety warnings were issued to healthcare professionals in the United Kingdom by the Medicines and Healthcare products Regulatory Authority (MHRA) in October 2011; this lowered the maximum daily dose from 60 to 40 mg, and from 40 mg to 20 mg in patients >65 years or with hepatic impairment (Table 1). The MHRA also advised that citalopram is contraindicated in patients with established QT prolongation or congenital QT syndromes, and that it should be used with caution in patients at risk for QT prolongation as a result of metabolic disturbance, concurrent illness, long QT syndrome, or if receiving medicines that are independently capable of prolonging the QT interval [3]. The maximum recommended dose of citalopram is 20 mg daily for patients that are poor cytochrome 2C19 metabolisers, or receiving concomitant cimetidine or another cytochrome 2C19 inhibitor, because these factors may elevate citalopram concentrations and increase the risk of QT prolongation and torsades de pointes. The basis of these regulatory changes and data concerning the cardiac effects of citalopram are considered.
Information concerning the cardiac effects of citalopram were sought using PubMed, Embase, and Google Scholar databases with search terms {citalopram} AND {adverse OR cardiac OR cardiotoxicity OR electrocardiograph OR QT OR “side effect” OR toxic OR toxicity OR “unwanted effect”}. Relevant data were also sought by examining abstracts of the scientific congresses of the European Association of Poisons Centers and Clinical Toxicologists (EPACCT), and reports submitted to the MHRA via the Yellow Card pharmacovigilance scheme. Preclinical safety data were included if these contained information regarding cardiotoxicity. Clinical data were considered separately between adverse effects arising from therapeutic administration and toxic effects encountered after exposure to higher dosages including intentional overdose.
Relevant pharmacological properties
Citalopram is partially metabolised to demethyl-citalopram (DCT), didemethyl-citalopram (DDCT), and citalopram-N-oxide, all of which possess some SSRI activity, and to an inactive deaminated propionic acid derivative. Citalopram is the predominant compound in plasma, and is subject to hepatic metabolism by P450 cytochromes 2C19, 2D6, and 3A4 [4]. A study of 345 plasma samples from 258 patients receiving 20–360 mg/day found a linear dose-concentration relationship; citalopram and DCT concentrations across typical therapeutic doses of 10 to 60 mg daily are 40 to 110 ng/mL and 14 to 40 ng/mL respectively [5]. Patients aged >65 years had significantly higher dose-corrected citalopram concentrations: mean ± SD 3.1 ± 1.4 ng/mL/mg versus 2.5 ± 2.2 ng/mL/mg (P = 0.03) [5]. The inward rectifier potassium channel is encoded by the human ether-a-go-go-related (hERG) gene, and blockade of this channel is thought to be an important mechanism linked to QTc prolongation and development of torsades de pointes arrhythmia. The channel is larger than several other voltage-gated potassium channels, which renders it subject to interference by a broad range of drugs, including citalopram [6, 7].
Preclinical toxicology data
A number of safety studies in animals are reported in the scientific literature. For example, 1 year safety studies in animals have investigated administration of citalopram doses of up to 8 mg/kg in dogs, 320 mg/kg in rats, and 640 mg/kg in mice; these resulted in citalopram concentrations 10- to 40-fold higher than those in patients, and sudden death occurred in five of ten dogs after citalopram 8 mg/kg daily for 17 to 31 weeks [8]. QT prolongation has been described in dogs exposed to serum DDCT concentrations between 810 and 3,250 nmol/L, which are 40 to 150-fold higher concentrations than observed in patients receiving citalopram 60 mg/day [9]. Acute oral administration in dogs of citalopram 20 mg/kg provoked seizures, and intravenous citalopram 10 mg/kg/h provoked seizures after administration of 21 to 27 mg/kg, and fatal respiratory arrest after 42 to 61 mg/kg; no significant electrocardiographic effects were observed [9]. Drug concentrations determined in this study were 20-fold higher than those associated with human therapeutic doses.
Cardiac effects after therapeutic doses
Clinical safety data collected from 3,107 patients across 24 separate clinical trials did not identify cardiac adverse effects or ECG abnormalities, although many of these involved short term studies and comparatively low therapeutic doses [10]. Collective ECG data obtained during drug development included 802 patients that received citalopram and 241 placebo; QTc increased >60 ms from baseline in 1.9 % versus 1.2 % respectively, and QTc >500 ms occurred in 0.5 % versus 0.0 % respectively [4]. A study in healthy men found that citalopram 60 mg/day had no significant effect on QTc interval [11].
A number of clinical reports describe the occurrence of QT prolongation in patients receiving citalopram. For example, an 81-year-old man was found to have prolonged QT (572 ms) and QTc (695 ms) and developed torsades de pointes; the ECG normalised within 3 days of discontinuing citalopram [12]. A 47-year-old woman with pre-existing dilated cardiomyopathy developed sinus bradycardia and prolonged QT interval (463 ms) that was attributed to a recent dose increase from citalopram 20 mg to 40 mg daily; the ECG restored to normal within 24 h [13]. Daily administration of citalopram 80 mg was associated with prolonged QTc and development of torsades de pointes in a 40-year-old woman, in whom no other metabolic disturbance or causative factor was identified; QTc fell from 535 ms to 469 ms 3 days after citalopram discontinuation [14]. Escitalopram, the S-enantiomer of citalopram has been reported to cause significant reversible QTc prolongation, even after only two daily administrations of 5 mg [15].
Citalopram appears capable of evoking cardiac effects in patients rendered susceptible by virtue of co-existing medications or metabolic disturbance. For example, an observational study reported the combination of escitalopram and risperidone was more likely to cause QT prolongation than risperidone and other SSRI antidepressants [16]. Significant QT and QTc prolongation (620 ms and 670 ms) was reported in a patient receiving citalopram 40 mg daily who had developed hypokalaemia and hypomagnesaemia due to concomitant diuretic therapy. Elsewhere, citalopram has been reported to cause symptomatic bradycardia and presyncope in a 60-year-old woman that had been taking citalopram 20 mg daily for 2 weeks, and haemodynamic changes were restored within 48 h of citalopram cessation; QTc remained normal throughout [17]. Decreased R-wave amplitude has also been reported after administration of citalopram 20 to 60 mg per day [18].
A Swedish pharmacovigilance database collected 61,788 adverse drug reports between 1991 and 2006; these included 88 reports of torsades de pointes, and citalopram was implicated in nine (10 %) of these [19]. The Yellow Card pharmacovigilance scheme in the United Kingdom has received a total of 3,636 reports to date from healthcare professionals concerning adverse effects of citalopram [20]. There have been 220 reports of adverse cardiac effects, including 17 cardiovascular fatalities, three reports of QT prolongation, and two reports of torsades de pointes (Table 2).
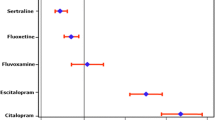
A thorough QT study was undertaken as a randomised multi-centre double-blind placebo-controlled study with cross-over design and moxifloxacin as an active comparator. The study involved administration of placebo, citalopram 20 mg, and citalopram 60 mg in 119 people. With reference to the placebo group, citalopram 20 and 60 mg caused QT prolongation by 8.5 ms (90 % confidence interval 6.2 to 10.8 ms) and 18.5 ms (16.0 to 21.0 ms), respectively (Fig. 1); QT corrected by Fridericia’s formula increased by up to 17 ms [1–3]. The regulatory authorities considered these data to indicate citalopram capable of evoking dose-dependent QT interval prolongation. Moreover, there is a lack of data to support the efficacy of citalopram in doses higher than 40 mg daily, and its maximal effects are typically observed after 20 to 40 mg daily [21]. Both the FDA and MHRA considered that the risk-benefit profile was unacceptable for higher citalopram doses.
Toxicity in the setting of citalopram overdose
A large number of case reports and case series indicate the occurrence of QT prolongation in the setting of citalopram toxicity. For example, QTc prolongation occurred in eight out of 26 patients (31 %) that presented to hospital in the Netherlands due to citalopram overdose [22]. A 21-year-old woman developed QT prolongation (457 ms) after ingestion of citalopram 400 mg, which normalised within 30 h [23]. A 36-year-old woman developed systemic hypotension and transient loss of consciousness due to torsades de pointes around 32 h after ingesting citalopram 1,000 mg; initial QTc was 572 ms and remained prolonged for a further 24 h [24]. Plasma citalopram and desmethylcitalopram concentrations at 33 h post-ingestion were 477 ng/mL and 123 ng/mL respectively, representing at least four-fold higher values than after therapeutic doses. Elsewhere, a series of five patients that presented to hospital after intentional citalopram overdose involving 400–5,200 mg were all found to have prolonged QTc [25]. ECG abnormalities or seizures were observed in patients that ingested citalopram >600 mg, and these occurred in all patients that ingested more than 1,900 mg [26].
A 32-year-old woman that ingested citalopram 800 mg developed hypotension and severe sinus bradycardia within 4 h; temporary cardiac pacing was needed and bradycardia persisted for 6 days [27]. A 31-year-old man developed QTc prolongation and left bundle branch block 13 h after ingestion of citalopram 400 mg; the ECG abnormalities resolved after intravenous administration of sodium bicarbonate, as might normally only occur after tricyclic cardiotoxicity [28, 29]. A 54-year-old woman developed QTc prolongation and ventricular fibrillation more than 10 h after intentional overdose associated with very high serum citalopram drug concentrations [30]. In contrast, acute citalopram exposure in a 10-month-old girl provoked generalised seizures; despite plasma citalopram concentrations of up to 1,400 ng/ml, no ECG abnormalities or QTc prolongation occurred [31].
A retrospective study found that QTc was similar after intentional overdose involving citalopram (427 ms), venlafaxine (420 ms), mirtazapine (423 ms), and nefazodone (419 ms), although the number of patients in each group was comparatively small [32]. Elsewhere, a larger series involving 469 patients with SSRI poisoning found that QTc was significantly higher in cases involving citalopram (450 ms, IQR 436 to 484 ms) than either fluoxetine, fluvoxamine, paroxetine, or sertraline; 68 % of citalopram overdose patients had QTc >440 ms [33]. Moreover, this study population demonstrated that a clear relationship exists between QTc prolongation and citalopram concentrations within a toxic range [34]. In a comparative study involving 541 intentional overdose episodes, citalopram ingestion was more likely to be associated with prolonged QTc >440 ms than overdose involving mirtazapine or venlafaxine (difference = 11 %, 95 % confidence interval 3 to 19 %, P = 0.013) [35].
Discussion
There has been a gradual accumulation of data that indicate a positive correlation between high citalopram doses and QT prolongation, and even torsades de pointes in a small number of cases. In many instances, there are co-existent factors that may predispose to cardiotoxicity, including biochemical disturbances, pre-existing cardiac disease, concomitant drug use, and long QT syndrome [36]. Therefore, a precautionary approach is justified, particularly in patients at high risk of QT prolongation. The duration of QT prolongation is longer than anticipated from published citalopram pharmacokinetic data, suggesting that cardiotoxicity might be attributable to its metabolite DCT [37].
In a clinical toxicology context, the potential for citalopram to evoke cardiotoxicity has long been recognised, and to a greater extent than anticipated for other SSRI antidepressants. There are a striking number of reports of QT prolongation in the context of intentional citalopram overdose, often with analytical confirmation, and a dose-effect relationship has been established across a very wide dose range. Therefore, it is somewhat surprising that QT effects of high therapeutic dosages have only recently been recognised. This might perhaps be due to the smaller magnitude of QT effect that might occur after therapeutic administration, even at the upper parts of the normal dose range. Nonetheless, the disparity between clinical toxicology data versus those collected by conventional pharmacovigilance methods indicates that earlier signal detection might occur if both sources of data were given greater consideration by regulatory authorities. Clinical toxicology data are not routinely collected in any systematic way, and may be more difficult to interpret due to the effect of various confounding factors [38]. Nonetheless, such data are important in understanding the overall risk-benefit in a clinical setting [39]. A recent example of where toxicology data have informed the regulatory assessment is co-proxamol, a fixed dose combination of paracetamol and dextropropoxyphene, where drug-induced cardiotoxicity and fatalities are readily observed in the setting of intentional overdose despite little observed effects within the normal therapeutic range [39, 40].
Conclusions
Data concerning the effects of citalopram indicate a dose-effect relationship with QTc, and this relationship exists across a wide range of therapeutic and toxic dosages. QTc effects have been detected earlier in a clinical toxicology context than might have been ascertained from conventional pharmacovigilance methods, suggesting that these data should play a greater role in informing regulatory safety assessment.
References
US Food and Drug Administration (2012) Abnormal heart rhythms associated with high doses of celexa (citalopram hydrobromide). Available from: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm269481.htm (accessed 12/06/2012)
US Food and Drug Administration (2012) Celexa (citalopram hydrobromide) drug safety communication: revised recommendations, potential risk of abnormal heart rhythms. Available from: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm297624.htm (accessed 12/06/2012)
Medicines and Healthcare products Regulatory Agency (2011) Citalopram and escitalopram: QT interval prolongation: new maximum daily dose restrictions (including in elderly patients), contraindications, and warnings information. Available from: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769 (accessed 12/06/2012)
Pollock BG (2001) Citalopram: a comprehensive review. Expert Opin Pharmacother 2:681–698
Le Bloc’h Y, Woggon B, Weissenrieder H, Brawand-Amey M, Spagnoli J, Eap CB, Baumann P (2003) Routine therapeutic drug monitoring in patients treated with 10–360 mg/day citalopram. Ther Drug Monit 25:600–608
Mitcheson JS (2003) Drug binding to HERG channels: evidence for a “non-aromatic” binding site for fluvoxamine. Br J Pharmacol 139:883–884
Witchel HJ, Pabbathi VK, Hofmann G, Paul AA, Hancox JC (2002) Inhibitory actions of the selective serontonin re-uptake inhibitor citalopram on HERG and ventricular L-type calcium currents. FEBS Lett 512:59–66
Fredricson Overø K (1982) Kinetics of citalopram in test animals; drug exposure in safety studies. Prog Neuropsychopharmacol Biol Psychiatry 6:297–309
Boeck V, Overø KF, Svendsen O (1982) Studies on acute toxicity and drug levels of citalopram in the dog. Acta Pharmacol Toxicol 50:169–174
Muldoon C (1996) The safety and tolerability of citalopram. Int Clin Psychopharmacol 11(Suppl 1):35–40
Rasmussen SL, Overo KF, Tanghoj P (1999) Cardiac safety of citalopram: prospective trials and retrospective analyses. J Clin Psychopharmacol 19:407–415
Kanjanauthai S, Kanluen T, Chareonthaitawee P (2008) Citalopram induced torsades de pointes, a rare life threatening side effect. Int J Cardiol 131:e33–e34
Favre MP, Sztajzel J, Berschy G (1999) Bradycardia during citalopram treatment: a case report. Pharmacol Res 57:149–150
Deshmukh A, Ulveling K, Alla V, Abuissa H, Airey K (2012) Prolonged QTc interval and torsades de pointes induced by citalopram. Tex Heart Inst J 39:68–70
Tseng PT, Lee Y, Lin YE, Lin PY (2012) Low-dose escitalopram for 2 days associated with corrected QT interval prolongation in a middle-aged woman: a case report and literature review. Gen Hosp Psychiatry 34:210
Sala M, Vicentini A, Brambilla P, Montomoli C, Jogia JR, Caverzasi E, Bonzano A, Piccinelli M, Barale F, De Ferrari GM (2005) QT interval prolongation related to psychoactive drug treatment: a comparison of monotherapy versus polytherapy. Ann Gen Psychiatry 4:1
Isbister GK, Prior FH, Foy A (2001) Citalopram-induced bradycardia and presyncope. Ann Pharmacother 35:1552–1555
Slavícek J, Paclt I, Hamplová J, Kittnar O, Trefný Z, Horácek BM (1998) Antidepressant drugs and heart electrical field. Physiol Res 47:297–300
Aström-Lilja C, Odeberg JM, Ekman E, Hägg S (2008) Drug-induced torsades de pointes: a review of the Swedish pharmacovigilance database. Pharmacoepidemiol Drug Saf 17:587–592
Medicines and Healthcare products Regulatory Agency (2012) Citalopram drug analysis print. Available from: http://www.mhra.gov.uk/home/groups/public/documents/sentineldocuments/dap_1335337465722.pdf (accessed 12/06/2012)
Montgomery SA (1995) Selecting the optimum therapeutic dose of serotonin reuptake inhibitors: studies with citalopram. Int Clin Psychopharmacol 10(Suppl 1):23–27
Jimmink A, Caminada K, Hunfeld NG, Touw DJ (2008) Clinical toxicology of citalopram after acute intoxication with the sole drug or in combination with other drugs: overview of 26 cases. Ther Drug Monit 30:365–371
Catalano G, Catalano MC, Epstein MA, Tsambiras PE (2001) QTc interval prolongation associated with citalopram overdose: a case report literature review. Clin J Neuropharmacol 24:158–162
Tarabar AF, Hoffman RS, Lelson LS (2008) Citalopram overdose: late presentation if torsdae de pointes with cardiac arrest. J Med Toxicol 4:101–105
Grundemar L, Wohlfart B, Lagerstedt C, Bengtsson F, Eklundh G (1997) Symptoms and signs of severe citalopram overdose. Lancet 349:1602
Personne M, SjÖberg G, Persson H (1997) Citalopram overdose: review of cases treated in Swedish hospitals. J Toxicol Clin Toxicol 35:237–240
Rothenhäusler HB, Hoberl C, Ehrentrout S, Kapfhammer HP, Weber MM (2000) Suicide attempt by pure citalopram overdose causing long-lasting severe sinus bradycardia, hypotension and syncopes: successful therapy with a temporary pacemaker. Pharmacopsychiatry 33:150–152
Engebretsen KM, Harris CR, Wood JE (2003) Cardiotoxicity and late onset seizures with citalopram overdose. J Emerg Med 25:163–166
Chan CY, Waring WS (2007) Images in cardiovascular medicine. Tricyclic cardiotoxicity treated with sodium bicarbonate. Circulation 115:e63–e64
Liotier J, Coudoré F (2011) Drug monitoring of a case of citalopram overdosage. Drug Chem Toxicol 34:420–423
Masullo LN, Miller MA, Baker SD, Bose S, Levsky M (2006) Clinical course and toxicokinetic data following isolated citalopram overdose in an infant. Clin Toxicol 44:165–168
Kelly CA, Dhaun N, Laing WJ, Strachan FE, Good AM, Bateman DN (2004) Comparative toxicity of citalopram and the newer antidepressants after overdose. J Toxicol Clin Toxicol 42:67–71
Isbister GK, Bowe SJ, Dawson A, Whyte IM (2004) Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose. J Toxicol Clin Toxicol 42:277–285
Friberg LE, Isbister GK, Duffull SB (2006) Pharmacokinetic-pharmacodynamic modelling of QT interval prolongation following citalopram overdoses. Br J Clin Pharmacol 61:177–190
Waring WS, Graham A, Gray J, Wilson AD, Howell C, Bateman DN (2010) Evaluation of a QT nomogram for risk assessment after antidepressant overdose. Br J Clin Pharmacol 70:881–885
de Gregorio C, Morabito G, Cerrito M, Dattilo G, Oreto G (2011) Citalopram induced long QT syndrome and torsade de pointes: role for concomitant therapy and disease. Int J Cardiol 148:226–228
Priskorn M, Larsen F, Segonzac A, Moulin M (1997) Pharmacokinetic interaction study of citalopram and cimetidine in healthy subjects. Eur J Clin Pharmacol 52:241–242
Wall AJ, Bateman DN, Waring WS (2009) Variability in the quality of overdose advice in Summary of Product Characteristics (SPC) documents: gut decontamination recommendations for CNS drugs. Br J Clin Pharmacol 67:83–87
Waring WS, McGettigan P (2011) Clinical toxicology and drug regulation: a United Kingdom perspective. Clin Toxicol 49:452–456
Hawton K, Bergen H, Waters K, Murphy E, Cooper J, Kapur N (2011) Impact of withdrawal of the analgesic Co-proxamol on nonfatal self-poisoning in the UK. Crisis 32:81–87
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooke, M.J., Waring, W.S. Citalopram and cardiac toxicity. Eur J Clin Pharmacol 69, 755–760 (2013). https://doi.org/10.1007/s00228-012-1408-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1408-1