Abstract
Purpose
The present study aimed to investigate the role of expression of daunorubicin-metabolizing enzymes carbonyl reductase 1 and 3 (CBR1 and CBR3) on the in vitro cytotoxicity of daunorubicin in primary acute myeloid leukemia (AML) cells and the effect of genetic variants in CBR1 and CBR3 on the plasma pharmacokinetics of daunorubicin and daunorubicinol (DOL) in AML patients.
Methods
RNA expression of CBR1 and CBR3, intracellular daunorubicin and DOL levels, and in vitro cytotoxicity of daunorubicin were measured in bone marrow mononuclear cells of 104 adult AML patients. Plasma pharmacokinetics of daunorubicin and DOL was measured in 24 patients receiving daunorubicin-based induction chemotherapy for AML.
Results
Increased expression of CBR1 significantly reduced the in vitro cytotoxicity of daunorubicin and also positively correlated with intracellular DOL levels. Polymorphisms in CBR1 and CBR3 did not show any association with intracellular daunorubicin or DOL levels, but there was a trend towards significant increase in plasma daunorubicin systemic exposure in patients with a variant genotype for CBR1 polymorphism rs25678.
Conclusions
This pilot study suggests that CBR1 RNA expression may be helpful in identifying AML patients at risk of developing resistance or toxicity to daunorubicin due to increased formation of DOL. Further confirmation of these findings in a larger sample pool would be required to determine the applicability of these results. Inhibition of CBR1 can be an option to improve the efficacy and prevent toxicity related to the treatment. Influence of daunorubicin and DOL plasma levels on clinical outcome, if any, remains to be evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Daunorubicin and doxorubicin belong to the class of anthracyclines ranked among the most effective antineoplastic drugs ever developed [1]. Though their mechanism of action is similar, daunorubicin is the drug of choice in hematologic malignancies. Daunorubicin enters the cell by passive diffusion and brings about its cytotoxic activity by DNA intercalation, stabilization of DNA-topoisomerase II cleavable complex, and lipid peroxidation leading to reactive oxygen species (ROS) production and apoptosis [2]. Daunorubicin along with cytarabine constitutes the induction chemotherapy of non-M3 acute myeloid leukemia (AML).
AML is a clinically and genetically heterogeneous clonal disorder characterized by the accumulation of somatically acquired genetic alterations in hematopoietic progenitor cells that alter normal mechanisms of self-renewal, proliferation, and differentiation [3]. With the present induction chemotherapy protocols, approximately 75–85 % of patients achieve complete remission. However, the 5 year event-free survival is as low as 25–30 %, and overall survival is dismal. Relapse of the disease and resistance to chemotherapy are regarded as the main causes of treatment failure. Over-expression of drug efflux transporters and metabolizing genes is one of the important factors contributing to primary resistance of chemotherapy in cancer [4, 5].
Daunorubicin is metabolized to the hydroxyl derivative daunorubicinol (DOL), which is less potent than the parent compound, by the carbonyl reductase enzymes (CBR) [6]. CBRs belong to the short dehydrogenase (SDR) family, which is involved in catalyzing the conversion of various endogenous (progesterone and menadione) and exogenous (cytotoxic drugs such as daunorubicin and doxorubicin) carbonyl compounds to their respective alcohol derivatives [7]. Aldoketoreductases (AKR), which belong to the SDR family, have also been linked to metabolism of anthracyclines. However, it has been shown that AKR isoforms AKR1A1 and AKR1B1 are less efficient than CBR in metabolism of daunorubicin [8]. A recent report has revealed that, unlike AKR1A1, AKR1C2, another isoform of AKR, fails to metabolize anthracyclines [9].
CBR enzymes are cytosolic in nature and are ubiquitously expressed in all the tissues with maximum expression in liver [10] and require nicotinamide adenine dinucleotide phosphate (NADPH) as a cofactor for catalysis [7, 11]. To date, four isoforms of CBR are known, of which CBR1 and CBR3 genes, located in chromosome 21, share 79 and 72 % homology with each other in nucleotide and amino acid sequences, respectively [12]. CBR2 is shown to be down-regulated in hepatocarcinoma cells compared to the normal cells [13], while the enzymatic activity and tissue distribution of CBR4 are unclear. It is proposed that over-expression of CBR1 may contribute to resistance towards daunorubicin by increased conversion to DOL as shown by increased survival of K562 cells upon treatment with daunorubicin [14]. Among the enzymes involved in reduction of daunorubicin, CBR1 is found to be the most efficient [8]. In hepatocarcinoma cells, knock-down of CBR1 is shown to increase the sensitivity against doxorubicin. Use of epigallocatechin gallate (EGCG) as a CBR1 inhibitor has been shown to decrease the conversion of daunorubicin to DOL and in turn increase the sensitivity of daunorubicin [15]. CBR1 is shown to be the major enzyme involved in daunorubicin metabolism in AML cells when compared to AKR1A1 [16].
Limited reports exist on the polymorphisms in CBR1 and CBR3 genes. Four single nucleotide polymorphisms (SNPs) in CBR1 are reported by sequencing of full length cDNA from liver donors: V88I (262G>A, rs1143663), L73L (312G>C, rs25678), A209A (720C>T, rs20572), and V231V (786G>A, rs2230192). In vitro kinetic studies showed that the V88I variant had 50 % lower Vmax than the wild type as reflected by decreased DOL formation in the variant [17, 18]. In CBR3, a commonly occurring coding SNP V244M (rs1056892) positioned in a critical NADPH interaction site is reported to occur at a higher frequency in African and Caucasian populations [19]. A variant of this SNP is shown to have significantly higher Vmax than the wild type by kinetic experiments using menadione as substrate. Also, a variant of this SNP is shown to influence cardiotoxicity in patients who suffered from cancer in childhood and were treated with anthracylines [20]. Polymorphisms in CBR1 and CBR3 have also been shown to influence disposition and toxicity of doxorubicin in breast cancer patients [21, 22].
Interindividual variation in daunorubicin metabolism may have potential implications on the toxicity and efficacy of the drug, making it critical to understand the factors influencing this variability. However, influence of CBR1 and CBR3 RNA expression on ex vivo cytotoxicity of daunorubicin in AML primary cells has not been reported. Further, there are no studies on the polymorphisms of CBR1 and CBR3 in patients with AML and their effect on RNA expression and in vitro cytotoxicity of daunorubicin in AML primary cells. The aim of the present study is to investigate polymorphisms of CBR1 and CBR3 and their RNA expression in AML and to evaluate their effect on in vitro cytotoxicity of daunorubicin. It is also aimed at evaluating the role of SNPs and expression of these genes on plasma pharmacokinetics of daunorubicin in patients receiving induction chemotherapy with daunorubicin in combination with cytarabine.
Patients and methods
Chemicals
Daunorubicin hydrochloride and Tri Reagent were obtained from Sigma Aldrich. Daunorubicinol was from Toronto Research Chemicals, Canada, and 3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazoliumbromide (MTT) was purchased from Biotium (CA, USA). All other reagents and solvents including acetonitrile, chloroform, and n-heptanol were of high performance liquid chromatography (HPLC) grade. Ficol-paque was from GE Healthcare (Uppsala, Sweden).
Patients
One hundred and four adult patients with AML (excluding AML-M3) at diagnosis (and/or relapse) before the initiation of therapy, diagnosed between June 2009 and May 2011 at the Department of Haematology, Christian Medical College, Vellore were included. Written informed consent was obtained from all the patients, and the study was approved by the Institutional Review Board. Peripheral blood samples from 42 healthy volunteers were used as controls for genotyping experiments.
Sampling procedure for pharmacokinetic analysis
Peripheral blood samples were collected at six time points (0, 1, 2, 4, 6, and 24 h) in EDTA tubes as reported previously [23] during the first day of induction chemotherapy (7 + 3) from 24 AML patients undergoing treatment. The blood samples collected in EDTA tubes were centrifuged, and plasma was immediately separated and stored at −80°C for further estimation of daunorubicin and DOL by HPLC.
Pharmacokinetics calculations
The area under the concentration versus time curve (AUC) from time 0 to infinity of plasma daunorubicin and DOL was calculated by noncompartmental methods using a combination of linear and log trapezoidal rule (linear for increasing concentrations, log for decreasing concentrations). Clearance of daunorubicin was calculated by dividing dose by AUC as described previously [24].
Quantitative reverse transcriptase PCR
Bone marrow mononuclear cells (BMMNCs) were isolated by density gradient centrifugation using Ficol-paque. Minimum information for publication of quantitative real-time PCR experiments (MIQE) guidelines were followed for designing and interpreting the results of quantitative real-time PCR [25]. Briefly, total RNA was extracted from the BMMNCs and peripheral blood of normal controls using Tri Reagent. Complementary DNA (cDNA) synthesis was performed with 1 μg RNA using Superscript II reverse transcriptase (Invitrogen, Carlsbad, CA, USA) following the manufacturer’s instructions. TaqMan® gene expression assays (assay ID: Hs00156323_m1 and Hs00154295_m1) were used for quantifying CBR1 and CBR3 expression, respectively, by quantitative PCR on an ABI PRISM 7500 sequence detection system and were normalized to the expression of reference gene GAPDH. Samples were run in duplicates, and relative expression was calculated using 2−ddCT (where dCT = CT of CBR1/CBR3 − CT of GAPDH , and AML001 as reference for both CBR1 and CBR3). To compare the RNA expression between CBR1 and CBR3, dCT was used, where higher dCT corresponds to lower expression. To assess the relative efficiencies of the three RQ-PCR assays, standard curve derived using serial dilution of cDNA prepared using one μg RNA from AML cell line Kasumi-3 with high CBR1 and CBR3 expression was used. The PCR efficiencies of CBR1, CBR3, and GAPDH were all comparable (Fig. S1). CBR3 expression was lower compared to CBR1 as reflected by lack of amplification of CBR3 transcripts at higher cDNA dilutions (both 1:125 and 1:625 dilutions).
Sample processing for intracellular daunorubicin measurement
Sample processing for intracellular daunorubicin measurement was based on a previously published method [26]. Briefly, BMMNCs (3 × 106 cells) were incubated at 37°C in humidified air containing 5 % CO2 in 1 ml of 10 % RPMI medium overnight. The cells were then treated with 5 μM daunorubicin and incubated for 90 min. After incubation, the cells were washed twice and resuspended in ice cold phosphate buffer saline (PBS), snap frozen, and stored in −80°C till HPLC analysis.
HPLC method for the analysis of daunorubicin and DOL
Daunorubicin and DOL levels were measured using HPLC as described previously [27] with slight modifications. Briefly, cells were lysed by sonication, and 0.5 ml of 0.2 M sodium (dibasic) phosphate buffer (pH 8.4) and 100 ng/ml of idarubicin (internal standard) were added. Four ml of chloroform:n-heptanol (9:1) mixture was added to the above solution and mixed gently in the rotary mixer for 15 min. The resulting mixture was centrifuged at 4,000 rpm for 10 min. The organic phase was separated and 0.25 ml of 0.1 M orthophosphoric acid was added and mixed slowly. The mixture was centrifuged at 3,000 rpm for 3 min; the aqueous phase was taken, and 50 μl of the same was injected for HPLC analysis using an autosampler (Bio-Rad, CA, USA). HPLC (Shimadzu; LC10 AT) coupled with fluorescence detector (Shimadzu; RF10A-XL model) and autosampler (Bio-rad AS 100 model, CA, USA) was used. Phenomenex Luna Cyano column (250 × 4.6 mm × 5 μm) protected with suitable guard column was used as stationary phase. The mobile phase composed of a mixture (35:65 v/v) of acetonitrile and 50 mM monobasic sodium phosphate, adjusted to pH 4.5 with 1 M orthophosphoric acid, was freshly prepared on each day of analysis and was filtered and degassed prior to use. The elution was carried out in an isocratic mode with a flow rate of 0.7 ml/min. Standards (100–2,000 ng/ml) for daunorubicin and DOL (100–500 ng/ml) were included in every batch of samples. The retention times of daunorubicin, DOL, and the internal standard were 8.7, 7.6, and 9.5 min, respectively. The limit of detection (LOD) and limit of quantification (LOQ) for both daunorubicin and DOL were 1 and 10 ng/ml, respectively. The interday and intraday coefficients of variation (CV) were less than 10 % for the concentrations used.
In vitro cytotoxicity assay
In vitro cytotoxicity of daunorubicin was determined using the MTT assay as described previously [28]. Briefly, MNCs were cultured in flat-bottomed 96-well microtitre plates in the presence of increasing concentrations of daunorubicin, ranging from 0.1 to 3.5 μM. Cells without drugs were used as controls, and culture medium alone was used for blanks. The plates were incubated for 48 h at 37°C in humidified air containing 5 % CO2, after which 10 μl of MTT reagent was added, and the plates were incubated for an additional 4 h. Viable cells were able to reduce MTT tetrazolium salt to purple/blue formazan crystals. The formazan crystals were dissolved using acidified SDS (0.01 N HCl, 10 % SDS) and the optical density (OD), which is linearly related to the number of viable cells [29], was measured spectrophotometrically at 570 and 630 nm. IC50 values were calculated using ADAPT5 software [30].
CBR1 and CBR3 resequencing
DNA was extracted from peripheral blood samples of patients as well as normal controls using standard phenol-chloroform method. Fifty ng of DNA was used for each PCR reaction. All three exons, 3′- and 5′-UTR as well as the 5′-upstream region of both CBR1 and CBR3 were subjected to PCR. The primer sequences used for resequencing are listed in Table 1. The PCR products were subjected to automated sequencing using Applied Biosystems 3130 Genetic Analyzer (Foster City, CA, USA). Sequences were aligned and SNPs or deletion/insertions were identified using SeqScape software v2.7 (Applied Biosystems). Potential functional effects of the SNPs were determined by in silico analysis using FASTSNP (http://fastsnp.ibms.sinica.edu.tw/pages/input_CandidateGeneSearch.jsp) as well as TFSEARCH (http://www.cbrc.jp/research/db/TFSEARCH.html) program to identify if the SNPs were creating or disrupting any transcription factor binding sites.
Linkage disequilibrium (LD) analysis
LD calculation and visualization were performed using Haploview [31]. SNPs with minor allele frequency <0.01 and those that failed Hardy-Weinberg equilibrium test (p < 0.001) were excluded from LD calculation. The measure D′ was used to represent LD strength [32] .
Statistical analysis
Statistical analysis was done using GraphPad Prism software (California, USA). Mann-Whitney U test, Kruskal-Wallis test, and Spearman rank correlation analysis were used as appropriate. A p value of <0.05 was considered statistically significant. False discovery rate (FDR) was controlled using the Benjamin-Hochberg procedure to correct multiple comparisons [33].
Results
Patients
A total of 104 AML patients (62 males and 42 females) with a median age of 42 years (range 16–67) were enrolled in the study. Patients were classified into different FAB subtypes based on the cell morphology. Among the 104 patients, 11 were found to have secondary/relapsed AML. AML patients and the normal controls included in the study were of Indian origin and there was equal distribution of north, south, and east Indians. The demographic features of the patients are enlisted in Table 2.
CBR1 and CBR3 expression in AML patients
Median CBR1 mRNA expression was 22.854 (range 0.029–253.15) and that of CBR3 was 414.94 (range 8.24–29,296.67). AML patients had a significantly higher CBR1 expression [median (range) dCT 10.43 (6.96–19.98)] when compared to CBR3 [17.89 (11.75–23.55)], where lower dCT value corresponds to higher expression and vice versa (Fig. 1) as analyzed by Mann-Whitney U test.
CBR1 and CBR3 RNA expression in acute myeloid leukemia (AML) patients. CBR1 and CBR3 expression were calculated by dCT method, where higher dCT implies lower expression and vice versa. Expression was normalized with GAPDH, and dCT of CBR1 and CBR3 was compared. RNA expression of CBR1 and CBR3 was compared using Mann-Whitney U test. The PCR efficiencies of CBR1, CBR3, and GAPDH were comparable
In vitro cytotoxicity of daunorubicin in AML cells
In vitro cytotoxicity of daunorubicin was estimated by MTT assay. The in vitro cytotoxicity data were available only for 93 samples, since there were insufficient cells for 11 samples. IC50 of daunorubicin among AML samples ranged from 0.01 to 3.2 μM. Based on a previously published report [34], AML samples were classified as sensitive (IC50 < 0.5 μM), intermediate (IC50 0.5–1.0 μM), or resistant (IC50 >1.0 μM) to daunorubicin.
Intracellular levels of daunorubicin and DOL in AML cells
Intracellular daunorubicin and DOL levels were measured by HPLC coupled with fluorescence detector (Fig. S2). Intracellular daunorubicin and DOL levels were available for only 85 samples as sufficient cells were not available for 19 samples. Intracellular levels of daunorubicin and DOL showed 95-fold variation (median 451.22 × 103 pg, range 17.98–1,718.14) and 22-fold variation (median 13.14 × 103 pg, range 2.76–62.07), respectively, among the samples screened.
CBR1 RNA expression influences the in vitro cytotoxicity of daunorubicin in AML cells
CBR1 RNA expression was compared with in vitro cytotoxicity of daunorubicin. Kruskal-Wallis test with Bonferroni correction was used to compare CBR1 expression among sensitive, intermediate, and resistant groups of AML samples classified based on the IC50 value. CBR1 expression was significantly higher in daunorubicin-resistant AML samples (IC50 >1 μM; median 103; range 7.8–253.15) compared to those who were daunorubicin-sensitive (IC50 <0.5 μM; median 18.68; range 0.34–105; p = 0.0158) but not with intermediate (IC50 0.5–1 μM; median 29.07; range 0.029–224; p = 0.1200) samples (Fig. 2). CBR3 RNA expression was not significantly associated with daunorubicin in vitro cytotoxicity (p = 0.1843), though the trend was similar to that of CBR1.
CBR1 RNA expression influences in vitro cytotoxicity of daunorubicin in primary acute myeloid leukemia (AML) cells. RNA expression of CBR1 was calculated by ddCT method and relative to that of AML001. CBR1 RNA expression was compared between sensitive and resistant samples. Expression of CBR1 among sensitive (IC50 < 0.5 μM), intermediate (IC50 0.5–1.0 μM) and resistant (IC50 >1.0 μM) was compared using Kruskal-Wallis test
CBR1 and to a lesser extent CBR3 RNA expression correlates with intracellular DOL levels
Spearman correlation rank method was employed to assess the association between CBR1 and CBR3 expression and intracellular DOL. Significant positive correlation (r = 0.5256; p < 0.0001) was found between CBR1 RNA expression and intracellular DOL among the AML samples (Fig. 3a). CBR3 RNA expression also showed a similar correlation (r = 0.3460; p = 0.0015) with intracellular DOL (Fig. 3b), but the association was less strong when compared to CBR1, suggesting that CBR1 is involved in the conversion of daunorubicin to DOL to a greater extent than CBR3.
CBR1 and CBR3 resequencing
In total, 3,095 base pairs (bp) of CBR1 and 2,286 bp of CBR3 covering three exons with flanking introns, 5′ and 3′UTR, and the proximal promoter region of CBR1 and CBR3 each were amplified using seven PCR reactions. The allelic frequencies of the CBR1 and CBR3 polymorphisms in normal controls and AML samples are listed in Table 3. A 31 bp deletion variant in the 5′UTR region (rs41563015) was identified with the allele frequency of 0.09 only in the AML samples and none of the normal controls screened. Two SNPs, rs20572 (exon 3; 627C>T) and rs9024 (3′UTR; +967G>A), in CBR1 were found to be in complete linkage disequilibrium, and both these SNPs showed more than 80 % linkage disequilibrium with rs25678 (in the exon 1 of CBR1) with a D′ of 0.8 (Fig. 4a). On the other hand, two nonsynonymous, three synonymous, one intronic, and one 3′UTR SNPs were identified in CBR3 (Table 3). Among the three synonymous SNPs, rs881711 and rs881712 were located in exon 1 and another synonymous SNP, rs17849671 (exon 3 in CBR3), was in linkage disequilibrium with the SNP rs12626192 in the intron of CBR3 with a D′ of 0.9 (Fig. 4b). The pharmacogenetic profiles of both CBR1 and CBR3 did not differ between AML samples and normal controls, except for the 31 bp deletion polymorphism in CBR1 5′-region.
Effect of CBR1 and CBR3 SNPs on RNA expression, intracellular DOL, and IC50 of daunorubicin
Association between the SNPs in CBR1 or CBR3 and RNA expression was analyzed together with daunorubicin IC50 and intracellular daunorubicin and DOL levels. The 5′UTR 31 bp deletion (rs41563015) variant in CBR1 showed a trend of association with lower CBR1 expression (median 13.68; range 0.029–107.22) compared to wild type (median 24.06; range 0.34–253.15; p = 0.1008). None of the other CBR1 SNPs showed significant association with CBR1 RNA expression or intracellular DOL levels. In addition, rs20572 in CBR1 (linked with rs9024, Fig. 4a) showed significant association with daunorubicin IC50 (p = 0.04) at FDR <20 %. Among the CBR3 SNPs, a variant of rs17849671 located in exon 3 showed a trend to higher CBR3 expression than the wild type [median expression of variant 1,299 (335.4–5,682) vs. wild type 389.6 (8.24–29,297); p = 0.0775). None of the other polymorphisms showed significant association with RNA expression, intracellular DOL, or IC50 of daunorubicin. Notably, given the small number of multiple tests and the nature of candidate gene approach, our choice of using nominal p < 0.05 as a cut-off gave us a reasonable level of false discovery rate of 20 %.
Linkage disequilibrium (LD) analysis of CBR1 and CBR3. LD was calculated using Haploview. All common SNPs survived Hardy-Weinberg equilibrium test (p > 0.001). a LD pattern for CBR1: SNPs, rs20572, and rs9024 are in complete LD with each other. These two SNPs are linked to rs25678 (D' = 0.77). b LD pattern for CBR3: rs12626192 and rs17849671 are in LD
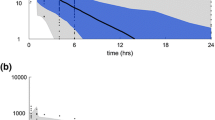
Plasma daunorubicin pharmacokinetics
AUC of daunorubicin and DOL in plasma samples ranged from 51 to 2,076 ng·h/ml and 59.5 to 2,119.6 ng·h/ml, respectively, while clearance of daunorubicin ranged from 43.34 to 1,785.95 L/h. Unlike intracellular DOL, plasma DOL AUC did not show any significant association with CBR1 and CBR3 expression. In patients with variant rs25678 genotype, daunorubicin AUC was higher [median 224 (51.4–2,076)] (Fig. 5) and clearance was lower [median 359.7 (43.34–1,752 L/h)] compared to the wild type [median daunorubicin AUC 139.1 (59.8–756); median daunorubicin clearance 610.8 (99.20–1,785.95 L/h)], though not reaching statistical significance (p = 0.178 and 0.2839 for daunorubicin AUC and clearance, respectively). None of the other polymorphisms of CBR1 and CBR3 showed any significant association with AUC of daunorubicin and DOL and clearance of daunorubicin.
Discussion
This is the first report showing the influence of CBR1 and CBR3 RNA expression on in vitro cytotoxicity of daunorubicin and the possible role of CBR1 SNP rs25678 in CBR1 and CBR3 on plasma pharmacokinetics of daunorubicin in AML patients. We showed that elevated RNA expression of CBR1 but not CBR3 confers in vitro chemoresistance towards daunorubicin in AML cells. Also, this study shows a positive correlation between CBR1 and CBR3 RNA expression with intracellular DOL levels, suggesting that increased conversion of daunorubicin to DOL is one of the factors affecting cytotoxicity of daunorubicin in AML patients.
Interindividual variation in expression of genes involved in metabolism of a drug can affect the efficacy of the drug and drug-associated toxicity. In the present study, CBR1 and CBR3 RNA expression showed wide interindividual variation, and CBR1 RNA expression was higher than CBR3 among AML patients. Previously it has been shown that the protein level of CBR1 is higher than CBR3 in the cytosol [35].
CBR is shown to be involved in the metabolism of a variety of physiological and xenobiotic carbonyl compounds to their respective metabolites including anthracyclines (13 hydroxy derivatives), which are less cytotoxic than the parent compound. Thus, increased expression leads to decreased efficacy of the drug. In the present study, CBR1 RNA expression showed positive correlation with in vitro cytotoxicity of daunorubicin in AML cells from 95 patients. In a recent study, it has been shown that CBR1 is the important enzyme involved in metabolism of daunorubicin in AML [16]. However, the influence of the CBR1 and CBR3 RNA expression and polymorphisms on in vitro chemoresistance of daunorubicin in primary AML cells was not studied. The authors could not find any significant association between CBR1 RNA expression with DOL levels and only with protein level. This may be attributed to the method used to estimate DOL levels as well as the smaller sample size. In the present study, the intracellular DOL levels were measured but not the enzymatic activity of CBR1. With respect to CBR3, there was no significant association between CBR3 expression and in vitro cytotoxicity of daunorubicin, which might be due to lower expression of CBR3 compared to CBR1.
Patients having a 31 bp deletion polymorphism (rs41563015) located in 5′UTR of CBR1 showed lower CBR1 RNA expression compared to wild type. This could be due to hypermethylation leading to decreased RNA expression of the variant compared to the wild type [36]. Also, by in silico analysis (FastSNP), this SNP is predicted to have a very low to moderate effect on gene expression. Interestingly, the SNP was observed only in the AML patients but not in any of the normal controls screened in the present study.
In CBR1, two SNPs (rs20572 and rs9024) were completely in linkage disequilibrium. Both the SNPs were in 84 % linkage disequilibrium with a SNP in exon 1 (rs25678), and allele frequencies of these SNPs were similar both in normal controls and AML patients. Previously, in Asian breast cancer patients and in normal controls these polymorphisms were shown to be in linkage disequilibrium, and the frequency of the variants was similar to the present data. These SNPs were shown to affect doxorubicin pharmacokinetics in breast cancer patients [22]. Also, recent studies have depicted a trend towards higher mRNA and protein levels in samples with wild type compared to that of variant of rs9024 in liver tissue [37]. However, in the present study we could not see any association of rs9024 with mRNA expression of CBR1 in AML samples. Among the CBR1 SNPs, synonymous polymorphism rs20572 was found to influence in vitro cytotoxicity of daunorubicin in AML samples, which has not been reported previously. None of the other CBR1 SNPs showed any association with RNA expression and in vitro cytotoxicity of daunorubicin. Since most of these SNPs have been shown to affect protein activity, the CBR1 enzymatic assay needs to be carried out to further understand the role of these SNPs in the metabolism of daunorubicin.
Seven nonsynonymous SNPs were reported previously in CBR3 and were shown to alter the enzymatic activity of CBR3 [38]. In the present study, among the seven coding SNPs only rs8133052 and rs1056892 were found to be frequent and the other five (rs9282628, rs2835285, rs16993929, rs4987121, and rs11701643) were not detected at all in our cohort of patients and normal controls. Among the synonymous polymorphisms, rs881711, rs881712, and rs17849671 were found to be frequent, and the allele frequency was similar to the Asian breast cancer patients [22]. The other two SNPs (rs2835284, rs45458797) were not detected. Samples with a variant of synonymous SNP rs17849671 were found to have higher CBR3 expression compared to the wild type, which has not been reported previously. Functional analysis needs to be carried out to identify the role of the SNP in altering CBR3 RNA expression.
To further explore the roles of CBR1, CBR3 mRNA expression, and their SNPs on efficacy and cytotoxicity of daunorubicin, we examined the association between plasma pharmacokinetics of daunorubicin and expression and SNPs in CBR1 and CBR3 in a subset of AML patients who underwent induction chemotherapy. AUC of daunorubicin, DOL, and clearance of daunorubicin showed wide interindividual variation among AML patients and were comparable to previously published studies [23, 39]. CBR1 and CBR3 mRNA expression did not show significant association with plasma AUC of daunorubicin and DOL. Among the SNPs of CBR1 and CBR3, a variant form of SNP rs25678 showed a trend to higher plasma daunorubicin AUC and lower clearance compared to patients with the wild type of the SNP. Synonymous polymorphisms have been shown to affect the mRNA stability and translational efficiency, leading to alteration in drug disposition [40]. In earlier reports in Asian breast cancer patients [22], it has been shown that the diplotype carrying at least one variant allele of rs25678 or rs9024 was shown to have higher exposure and lower clearance of doxorubicin. However, in the present study such association was not observed, and this may be attributed to the small sample size. The effect of mRNA levels of these genes on intracellular AUC of daunorubicin and DOL needs to be further investigated.
To conclude, we have investigated the role of RNA expression and polymorphisms of CBR1 and CBR3 in primary cells from AML patients and found wide interindividual variation in the RNA expression of CBR1 and CBR3. Increased RNA expression of CBR1 causes ex vivo chemoresistance towards daunorubicin in AML cells. Increased RNA expression of CBR1 and to a lesser extent CBR3 leads to increased conversion of daunorubicin to DOL. Thus, inhibition of CBR1 could be an option to improve the efficacy of the treatment and also prevent toxicity related to the treatment. CBR1 genetic variants seem to have an effect on plasma daunorubicin, and the influence of daunorubicin and DOL plasma levels on clinical outcome, if any, remains to be evaluated.
References
Weiss RB (1992) The anthracyclines: will we ever find a better doxorubicin? Semin Oncol 19(6):670–686
Rabbani A, Finn RM, Ausio J (2005) The anthracycline antibiotics: antitumor drugs that alter chromatin structure. Bioessays 27(1):50–56
Frohling S, Scholl C, Gilliland DG, Levine RL (2005) Genetics of myeloid malignancies: pathogenetic and clinical implications. J Clin Oncol 23(26):6285–6295
Schiffer CA, McIntyre OR (1993) Age related changes in adults with acute leukemia. Adv Exp Med Biol 330:215–229
Burnett AK, Mohite U (2006) Treatment of older patients with acute myeloid leukemia–new agents. Semin Hematol 43(2):96–106
Kuffel MJ, Reid JM, Ames MM (1992) Anthracyclines and their C-13 alcohol metabolites: growth inhibition and DNA damage following incubation with human tumor cells in culture. Cancer Chemother Pharmacol 30(1):51–57
Oppermann U (2007) Carbonyl reductases: the complex relationships of mammalian carbonyl- and quinone-reducing enzymes and their role in physiology. Annu Rev Pharmacol Toxicol 47:293–322
Plebuch M, Soldan M, Hungerer C, Koch L, Maser E (2007) Increased resistance of tumor cells to daunorubicin after transfection of cDNAs coding for anthracycline inactivating enzymes. Cancer Lett 255(1):49–56
Takahashi RH, Bains OS, Pfeifer TA, Grigliatti TA, Reid RE, Riggs KW (2008) Aldo-keto reductase 1C2 fails to metabolize doxorubicin and daunorubicin in vitro. Drug Metab Dispos 36(6):991–994
Kassner N, Huse K, Martin HJ, Godtel-Armbrust U, Metzger A, Meineke I et al (2008) Carbonyl reductase 1 is a predominant doxorubicin reductase in the human liver. Drug Metab Dispos 36(10):2113–2120
Forrest GL, Gonzalez B (2000) Carbonyl reductase. Chem Biol Interact 129(1–2):21–40
Watanabe K, Sugawara C, Ono A, Fukuzumi Y, Itakura S, Yamazaki M et al (1998) Mapping of a novel human carbonyl reductase, CBR3, and ribosomal pseudogenes to human chromosome 21q22.2. Genomics 52(1):95–100
Liu S, Ma L, Huang W, Shai Y, Ji X, Ding L et al (2006) Decreased expression of the human carbonyl reductase 2 gene HCR2 in hepatocellular carcinoma. Cell Mol Biol Lett 11(2):230–241
Gonzalez B, Akman S, Doroshow J, Rivera H, Kaplan WD, Forrest GL (1995) Protection against daunorubicin cytotoxicity by expression of a cloned human carbonyl reductase cDNA in K562 leukemia cells. Cancer Res 55(20):4646–4650
Huang W, Ding L, Huang Q, Hu H, Liu S, Yang X et al (2010) Carbonyl reductase 1 as a novel target of (-)-epigallocatechin gallate against hepatocellular carcinoma. Hepatology 52(2):703–714
Bogason A, Masquelier M, Lafolie P, Skogastierna C, Paul C, Gruber A et al (2010) Daunorubicin metabolism in leukemic cells isolated from patients with acute myeloid leukemia. Drug Metab Lett 4(4):228–232
Gonzalez-Covarrubias V, Ghosh D, Lakhman SS, Pendyala L, Blanco JG (2007) A functional genetic polymorphism on human carbonyl reductase 1 (CBR1 V88I) impacts on catalytic activity and NADPH binding affinity. Drug Metab Dispos 35(6):973–980
Bains OS, Karkling MJ, Grigliatti TA, Reid RE, Riggs KW (2009) Two nonsynonymous single nucleotide polymorphisms of human carbonyl reductase 1 demonstrate reduced in vitro metabolism of daunorubicin and doxorubicin. Drug Metab Dispos 37(5):1107–1114
Lakhman SS, Ghosh D, Blanco JG (2005) Functional significance of a natural allelic variant of human carbonyl reductase 3 (CBR3). Drug Metab Dispos 33(2):254–257
Blanco JG, Leisenring WM, Gonzalez-Covarrubias VM, Kawashima TI, Davies SM, Relling MV et al (2008) Genetic polymorphisms in the carbonyl reductase 3 gene CBR3 and the NAD(P)H:quinone oxidoreductase 1 gene NQO1 in patients who developed anthracycline-related congestive heart failure after childhood cancer. Cancer 112(12):2789–2795
Fan L, Goh BC, Wong CI, Sukri N, Lim SE, Tan SH et al (2008) Genotype of human carbonyl reductase CBR3 correlates with doxorubicin disposition and toxicity. Pharmacogenet Genomics 18(7):621–631
Lal S, Sandanaraj E, Wong ZW, Ang PC, Wong NS, Lee EJ et al (2008) CBR1 and CBR3 pharmacogenetics and their influence on doxorubicin disposition in Asian breast cancer patients. Cancer Sci 99(10):2045–2054
Kokenberg E, Sonneveld P, Sizoo W, Hagenbeek A, Lowenberg B (1988) Cellular pharmacokinetics of daunorubicin: relationships with the response to treatment in patients with acute myeloid leukemia. J Clin Oncol 6(5):802–812
Poonkuzhali B, Srivastava A, Quernin MH, Dennison D, Aigrain EJ, Kanagasabapathy AS et al (1999) Pharmacokinetics of oral busulphan in children with beta thalassaemia major undergoing allogeneic bone marrow transplantation. Bone Marrow Transplant 24(1):5–11
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M et al (2009) The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55(4):611–622
Borg AG, Burgess R, Green LM, Scheper RJ, Liu Yin JA (2000) P-glycoprotein and multidrug resistance-associated protein, but not lung resistance protein, lower the intracellular daunorubicin accumulation in acute myeloid leukaemic cells. Br J Haematol 108(1):48–54
Fogli S, Danesi R, Innocenti F, Di Paolo A, Bocci G, Barbara C et al (1999) An improved HPLC method for therapeutic drug monitoring of daunorubicin, idarubicin, doxorubicin, epirubicin, and their 13-dihydro metabolites in human plasma. Ther Drug Monit 21(3):367–375
Pieters R, Loonen AH, Huismans DR, Broekema GJ, Dirven MW, Heyenbrok MW et al (1990) In vitro drug sensitivity of cells from children with leukemia using the MTT assay with improved culture conditions. Blood 76(11):2327–2336
Klumper E, Pieters R, Kaspers GJ, Huismans DR, Loonen AH, Rottier MM et al (1995) In vitro chemosensitivity assessed with the MTT assay in childhood acute non-lymphoblastic leukemia. Leukemia 9(11):1864–1869
D'Argenio DZ, Schumitzky A, Wang X (2009) ADAPT 5 user's guide: pharmacokinetic/pharmacodynamic systems analysis software. Biomedical Simulations Resource, Los Angeles
Barrett JC, Fry B, Maller J, Daly MJ (2005) Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21(2):263–265
Lewontin RC (1964) The interaction of selection and linkage. I. General considerations; heterotic models. Genetics 49(1):49–67
Hochberg Y, Ba Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B: Methodol 57(1):11
Speth PA, Linssen PC, Boezeman JB, Wessels HM, Haanen C (1987) Leukemic cell and plasma daunomycin concentrations after bolus injection and 72 h infusion. Cancer Chemother Pharmacol 20(4):311–315
Terada T, Sugihara Y, Nakamura K, Mizobuchi H, Maeda M (2003) Further characterization of Chinese hamster carbonyl reductases (CHCRs). Chem Biol Interact 143–144:373–381
Zhang Y, Rohde C, Tierling S, Jurkowski TP, Bock C, Santacruz D et al (2009) DNA methylation analysis of chromosome 21 gene promoters at single base pair and single allele resolution. PLoS Genet 5(3):e1000438
Gonzalez-Covarrubias V, Zhang J, Kalabus JL, Relling MV, Blanco JG (2009) Pharmacogenetics of human carbonyl reductase 1 (CBR1) in livers from black and white donors. Drug Metab Dispos 37(2):400–407
Bains OS, Karkling MJ, Lubieniecka JM, Grigliatti TA, Reid RE, Riggs KW (2010) Naturally occurring variants of human CBR3 alter anthracycline in vitro metabolism. J Pharmacol Exp Ther 332(3):755–763
Galettis P, Boutagy J, Ma DD (1994) Daunorubicin pharmacokinetics and the correlation with P-glycoprotein and response in patients with acute leukaemia. Br J Cancer 70(2):324–329
Sauna ZE, Kimchi-Sarfaty C, Ambudkar SV, Gottesman MM (2007) Silent polymorphisms speak: how they affect pharmacogenomics and the treatment of cancer. Cancer Res 67(20):9609–9612
Acknowledgments
We gratefully acknowledge the help provided by Dr. Carl J Panetta, Department of Pharmaceutical Sciences, St. Jude Children's Research Hospital, Memphis, TN in checking our noncompartmental PK analysis and providing his valuable input in revising this manuscript. We also acknowledge Dr. Eunice S. Edison and Ms. M. Ezhilpavai for critically reviewing the revised manuscript. This study was supported by the Department of Biotechnology, India, grant no: BT/01/COE/08/03. Ajay Abraham is supported by a grant from the University Grants Commission, India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varatharajan, S., Abraham, A., Zhang, W. et al. Carbonyl reductase 1 expression influences daunorubicin metabolism in acute myeloid leukemia. Eur J Clin Pharmacol 68, 1577–1586 (2012). https://doi.org/10.1007/s00228-012-1291-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1291-9