Abstract
Objectives
To estimate the pharmacokinetic (PK) properties of posaconazole in patients with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) undergoing chemotherapy in a clinical setting.
Methods
Posaconazole concentrations in patients with AML/MDS receiving prophylactic posaconazole were determined by high-performance liquid chromatography. A population PK model with nonlinear mixed effect modeling was developed. The list of tested covariates included age, weight, height, gender, posaconazole dose, ethnicity, co-administration of antineoplastic chemotherapy, ranitidine or pantoprazole, coincident fever, diarrhea, leukocyte counts, and γ-glutamyltransterase plasma activity.
Results
A total of 643 serum concentrations of posaconazole from 84 patients were obtained. A one-compartment model with first order absorption and elimination as the basic structural model appropriately described the data, with an apparent clearance of 56.8 L/h [95% confidence interval (CI) 52.8–60.8 L/h] and an apparent volume of distribution of 2,130 L (95% CI 1,646–2,614 L). Significant effects on apparent clearance (CL/F) were found for presence of diarrhea and for co-medication with proton-pump inhibitors (1.5- and 1.6-fold increase in CL/F, respectively), weight (33.4 L larger apparent volume of distribution per kilogram), and co-administration of chemotherapy (0.6-fold lower apparent volume of distribution).
Conclusion
We developed a prediction basis for mean posaconazole concentrations in AML/MDS patients. Patient weight, presence of diarrhea, and concomitant medication (chemotherapy and pantoprazole) showed significant effects on posaconazole exposure. Corresponding adjustments of the starting dose according to the presence of diarrhea and during the co-administration of chemotherapy or proton-pump inhibitors appear justified before therapeutic drug monitoring results are available. Further investigation of the interaction between different chemotherapeutic regimens and posaconazole is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing induction or consolidation chemotherapy for acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) are at high risk of contracting invasive fungal diseases (IFDs), especially invasive pulmonary aspergillosis [1–3]. As the mortality of IFDs remains high in spite of new treatment options [4, 5], antifungal prophylaxis is an important option in high-risk patients. Recent trials have shown that posaconazole effectively prevents IFDs and death in patients receiving high-dose chemotherapy for AML or MDS as well as in extensive immunosuppressive treatment for graft-versus-host disease after allogeneic stem cell transplantation [6, 7]. Since the publication of these results, many international guidelines have included strong recommendations for its use [8–11].
Immediately after becoming aware of the survival benefit for patients receiving posaconazole prophylaxis, the Department I of Internal Medicine at the University Hospital of Cologne successfully introduced the triazole antifungal as a standard of care adjunct to remission–induction chemotherapy for AML/MDS [2]. In analogy to the randomized trial by Cornely and colleagues [7], patients start prophylaxis with posaconazole 200 mg three times daily during chemotherapy and stop after recovering from neutropenia.
While therapeutic drug monitoring (TDM) was not part of the 2007 randomized trials, TDM is the standard of care for the Department I for Internal Medicine in patients receiving antifungal prophylaxis or treatment with posaconazole. Posaconazole is currently only available as an oral suspension; it has an elimination half-life of 24–31 hours, achieves steady state in 7–10 days, is a potent cytochrome P450 3A4 (CYP3A4) inhibitor, and induces P-glycoprotein in the gut [12, 13]. The pharmacokinetics (PK) of posaconazole show a marked intra- and inter-individual variability, especially in terms of the bioavailability of the oral suspension, which may play a role in the emergence of breakthrough infections in patients receiving posaconazole prophylaxis [14–17]. A recent retrospective analysis proposed target serum levels of posaconazole to prevent breakthrough fungal infections [18]. Nutritional supplements have been proposed as a means of improving the bioavailability of the drug [19]. In a population PK analysis of posaconazole levels in patients undergoing allogeneic stem cell transplantation which we conducted earlier, we found that patient age and presence of diarrhea influence the serum levels of posaconazole [20]. Another recent analysis of the Schering-Plough Research Institute indicated the presence of diarrhea, proton-pump inhibitor (PPI) intake, increased plasma levels of γ-glutamyltransterase (γGT) and bilirubin, and ethnicity as covariates influencing systemic posaconazole exposure in AML/MDS patients [21].
The objective of this study was to assess the PK properties of posaconazole in AML/MDS patients undergoing chemotherapy.
Patients and methods
Study design
This was a non-interventional study using prospectively collected cohort data. Posaconazole prophylaxis was established as the standard of care for AML/MDS patients undergoing remission–induction chemotherapy by our department in January 2006, including trough serum level measurements three times weekly. Clinical data of neutropenic patients are routinely documented in the relational cohort database of the prospective Cologne Cohort of Neutropenic Patients (CoCoNut). Data items include demographic data, co-medication, concomitant chemotherapies, laboratory parameters, and febrile and diarrheal episodes. The CoCoNut uses a documentation platform based on Microsoft SQL Server 2005 and Microsoft Access 2003 (both by Microsoft Corp, Redmond, WA) which was developed in cooperation with System AG für IT-Lösungen, Lohmar, Germany.
Study population
All patients of the CoCoNut receiving posaconazole prophylaxis following the administration of induction or consolidation chemotherapy for AML or MDS with at least one available trough serum level measurement were included into the analysis.
Posaconazole administration
All patients included in this analysis received posaconazole oral suspension 200 mg (5 mL) three times daily as the standard of care. Patients were advised to take posaconazole after their regular meals. Given the lack of evidence for a dose–efficacy relationship during the observational period, there was no guideline proposing a certain target concentration and there was no defined algorithm for dose adjustment according to serum level; however, attending physicians were free to deviate from standard dosing if they chose to. Actual exposure was included into the analysis.
Posaconazole concentration measurements
During the observational period, posaconazole serum level measurements were to be performed twice weekly as the standard of care. Posaconazole trough serum concentrations were measured by high-performance liquid chromatography (HPLC) as described previously [20, 22]. All concentrations measured from the beginning of treatment were used, including samples taken before the expected steady state.
PK analysis
Pharmacokinetic properties of posaconazole were analyzed using the nonlinear mixed effect software NONMEM, as described previously [20].
Ethical considerations
Therapeutic drug monitoring is performed as the standard of care. The CoCoNut is performed as part of a quality assurance program by the Department I of Internal Medicine. The study was strictly non-interventional, and the NONMEM analysis was performed after all patients had completed their treatment.
Model building
Population PK modeling was used to predict posaconazole serum concentrations as described [20].
Based on the structural model, potential covariates were tested. Given the many different drugs used in different doses and regimens for chemotherapy, therapies were pooled in type and intensity categories for analysis. Category 1 included regimens based on cytarabine and daunorubicin, category 2 included regimens based on cytarabine and mitoxantrone or other anthracyclines, and category 3 included regimens based on other drugs than cytarabine. Intensity was rated as 1 for antibody- or small molecule-based regimens, 2 for maintenance therapy, and 3 for induction and consolidation therapy. The list of individual covariates included age (years), weight (kg), height (cm), gender, daily dose of posaconazole (mg, absolute values), ethnicity (Caucasian/other), co-administration of chemotherapy (yes/no), type of chemotherapy (category 1/2/3, see above), intensity of chemotherapy (1/2/3, see above), ranitidine (yes/no), PPIs (yes/no), diarrhea (yes/no), fever (yes/no), γGT levels (U/L, absolute and log values) [21], and number of leucocytes in blood (absolute and log values). Covariates were incorporated in the model in a forward stepwise manner and then removed backwards starting with the covariate that resulted in the largest reduction in the objective function value (OFV). This procedure was repeated until no significant (p < 0.05) drop was obtained in the OFV (corresponding to a ΔOFV of 3.84) by the respective covariate [20].
Model validation
Beyond visual predictive checks, a significant reduction in the OFV of >3.84 (p < 0.05), appropriate 95% confidence intervals (CIs) for parameter estimates, and physiological plausibility, the validity of the model was assessed by a modified jack-knife evaluation of the potential final model [20, 23]. The estimation of population PK parameters was repeated with reduced data sets randomly excluding 10% of the cases. If a covariate showed a significant influence in individual cases only, it was excluded from the final covariate model.
Results
Patient data
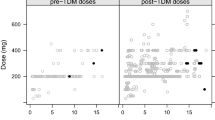
We measured 643 serum concentrations of posaconazole in 84 patients with AML or MDS during routine TDM using HPLC (samples per patient: 1–22, median 5). Demographic data and clinical data on the covariates assessed are shown in Tables 1 and 2. The overall mean ± standard deviation (SD) of all posaconazole concentration measurements was 555 ± 384 μg/L [range: values below the lower limit of quantification (50 μg/l) up to 2,638 μg/L]. Dose deviations from the recommended regimen were recorded in 13 patients: three patients received 200 mg twice daily; one patient 400 mg three times daily for 5 days, then 600 mg four times daily; two patients started with 200 mg twice daily and were later switched to 200 mg four times daily; four patients received 200 mg four times daily for the whole course; one patient received 400 mg three times daily.
All of the patients experienced neutropenia as defined by a neutrophil count ≤500 /μL; of these, 64 patients showed a prolonged neutropenia of >7 days.
Basic structural model
Population PK analysis, using a one-compartment model with first order absorption and elimination as the basic structural model, as described previously [20], was able to describe the collected data appropriately.
Development of the covariate model
The process of modeling activities and the results of covariate screening with NONMEM are given in Tables 3 and 4.
Simultaneous incorporation of weight and co-administration of chemotherapy [on volume of distribution (Vd) divided by the bioavailable fraction of the dose (F) for each] as well as presence of diarrhea and co-medication with PPIs [on clearance (CL)/F for each] as covariates in the basic model (Model 5, as given in Table 4) was associated with a significant and pronounced drop in the OFV (ΔOFV = 86.2). The addition of further covariates to the described model which had significant effects when added as single covariates to the basic model gave equivocal results. Separate inclusion of co-medication with ranitidine or fever showed no significant reduction in OFV. Simultaneous addition of γGT-levels as absolute values led to a significant reduction in OFV (ΔOFV = 32.5), however the 95% CIs included unity.
This potential final model was examined using the modified jack-knife evaluation. All tested covariates maintained stable and statistically significant effects in the truncated data sets.
Final covariate model
Model 5, as given in Table 4, was selected as the final model for the current population PK analysis. The overview of goodness-of-fit-plots for the basic model and the final covariate model is given in Fig. 1.
The parameter estimates and their respective 95% CIs are presented in Table 5. Coefficients of variation (CV%) were used to express the estimates of inter-individual and residual variability. In the final model, the occurrence of diarrhea as well as co-medication with PPIs were both related to a significantly higher apparent clearance (CL/F) of posaconazole, causing a 1.5-fold and a 1.6-fold increase in CL/F, respectively. These changes correspond to a respective decrease in posaconazole exposure. Higher weight was significantly associated with a larger apparent volume of distribution (Vd/F) by 33.4 L per each kilogram of weight. Co-administration of any chemotherapy was related to a 0.6-fold lower Vd/F of posaconazole, while type and intensity of chemotherapy did not contribute further to the explanation of variability. These changes correspond to a respective increase of exposure with co-administration of chemotherapy and a decrease of exposure with increasing weight for a given dose. The remaining inter-individual variability in CL/F not explained by the covariates was characterized by a CV of 25.3 %. The CV for residual variability was 23.2 %.
The basic structural model accounted for 37.3 % of the variability in posaconazole plasma concentrations, calculated as r 2 for the correlation between measured and individual predicted concentrations, while the final model with inclusion of covariates reached 46.7%.
Discussion
In this study, we used population PK methods to establish relevant covariates influencing posaconazole serum levels in patients with AML/MDS receiving the triazole as prophylaxis against IFDs. To the best of our knowledge, this is the first study analyzing population PK of this high-risk patient group outside of clinical trials. Among a broad range of covariates tested, significant effects were found for weight, co-administration of chemotherapy, diarrhea, and co-medication with PPIs.
TDM has been discussed as a means of optimizing outcomes in posaconazole prophylaxis [24–26] ever since publication of the landmark clinical trials showing its efficacy in high-risk patients [6, 7]. A recent retrospective analysis of data from the landmark trials has further stimulated this discussion by proposing effective breakpoint serum levels for posaconazole prophylaxis [18]. The study of population PK enables serum levels to be predicted and provides the means for changing them, both of which are mandatory when trying to achieve serum levels like those proposed by Jang and colleagues. In a comprehensive analysis of PK data from the AML/MDS trial on posaconazole prophylaxis, AbuTarif and colleagues built a model based on a number of covariates available in the original data set [21]. However, clinical trials use strict inclusion and exclusion criteria. Guidelines on the timing of drug intake (including dietary recommendations) and a list of prohibited concomitant medications are usually enforced in such trials. As a consequence, the population PK of new drugs may vary between clinical trials and real-life situations.
A common finding of both previous population PK studies [20, 21] and the study at hand is the reduction of exposure by diarrhea. The reduced systemic exposure to posaconazole oral suspension has been described in earlier PK analyses [16, 17] and has resulted in a recently completed trial on different posaconazole dosing regimens in AML patients with compromised gastrointestinal function [27]. While the present data show that a majority of patients achieved a posaconazole serum concentration of >500 ng/mL despite gastrointestinal impairment, other dosing schedules and/or higher dosages did not increase exposure. The effect of PPIs on the bioavailability of posaconazole is well established and extensively discussed elsewhere [17, 28–31].
Our study is the first to investigate the effect of posaconazole co-administration with anti-cancer chemotherapy on PK. We observed a significant reduction in the apparent posaconazole volume of distribution when it was administered on the same day as chemotherapy. However, a further analysis taking into consideration the drugs and doses of the chemotherapeutic regimens did not demonstrate a significant effect on the final model. This raises questions on possible interactions between posaconazole and some chemotherapeutic drugs that might affect exposure to chemotherapy as well. Posaconazole itself inhibits cytochrome P450 enzymes, and the increased exposure to posaconazole by some chemotherapeutic agents may vice versa increase exposure to other drugs, including chemotherapy as well. As the most commonly used drugs in the observed patients were cytarabine, mitoxantrone, and thioguanine, none of which are known to show a marked interaction with cytochrome P450, other effects may have caused our observation. During the chemotherapy phase, patients may develop nausea and vomiting and other acute toxicities, often leading to the administration of manifold prophylactic and therapeutic supportive drugs. Some of these drugs, such as aprepitant, dexamethasone, and granisetron, resemble posaconazole substrates of CYP3A4.
Ethnicity was identified as a covariate in the NONMEM analysis of data from the phase III trials [21]. Although we included ethnicity into our analysis, the population of our single-center analysis included mostly Caucasians and did not allow detection of smaller inter-racial differences. The effect of γGT plasma activity on the PK model was comparable to that reported by AbuTarif and colleagues, although it was not included into the final model.
An earlier study by our group had demonstrated a significant effect of age on the PK model [20]. While age showed a certain effect on the Vd/F in the study at hand, this covariate was eliminated from the final model. A new observation of our study is that the patients’ body weight influences the Vd/F, which is a common finding of PK studies, but has not yet been described for posaconazole.
Earlier studies have demonstrated that high levels of posaconazole are found in cells of the peripheral blood [32]. We therefore included leukocyte counts as a covariate in our analysis; however, no association of leukocyte counts with posaconazole PK was demonstrated. It is hence unlikely that leukocytes play a relevant role in the PK of posaconazole, although they may be of importance for its pharmacodynamics.
One shortcoming of our study is the absence of data on mucositis and vomiting, which may be important covariates for posaconazole PK. Although these events are included into the CoCoNut and patient files, nurse documentation at our institution is not sufficiently standardized to provide dependable data for a scientific analysis. However, most patients with severe nausea and/or mucositis are not able to swallow posaconazole and are therefore often switched to intravenous antifungals other than posaconazole.
In summary, our study provides further evidence for the reduced posaconazole exposure by diarrhea and concomitant PPI intake. It is the first study showing an interaction between posaconazole levels and chemotherapy administration. Further investigation of this issue is warranted, as our study was not powered to differentiate between the many different drugs and dosing regimens used in AML chemotherapy and the associated supportive care. The quantitative importance of the identified covariates should be re-addressed by hypothesis-driven studies. Overweight patients and patients with diarrhea and/or on concomitant PPIs were at a risk of lower exposure; although changes in posaconazole dosing have not shown promise improving exposure [33], efforts should be taken to administer posaconazole with dietary support and to discontinue PPIs whenever possible. These patients also should be monitored closely for breakthrough infections.
References
Lass-Florl C (2009) The changing face of epidemiology of invasive fungal disease in Europe. Mycoses 52(3):197–205
Vehreschild JJ, Rüping MJGT, Wisplinghoff H, Farowski F, Steinbach A, Sims R, Stollorz A, Kreuzer K-A, Hallek M, Bangard C, Cornely OA (2010) Clinical effectiveness of posaconazole prophylaxis in patients with acute myelogenous leukemia (AML): A six year experience of the Cologne AML Cohort. J Antimicrob Chemother 65:1466–1471
Cuenca-Estrella M, Bernal-Martinez L, Buitrago MJ, Castelli MV, Gomez-Lopez A, Zaragoza O, Rodriguez-Tudela JL (2008) Update on the epidemiology and diagnosis of invasive fungal infection. Int J Antimicrob Agents 32[Suppl 2]:S143–S147. doi:10.1016/S0924-8579(08)70016-5
Reboli AC, Rotstein C, Pappas PG, Chapman SW, Kett DH, Kumar D, Betts R, Wible M, Goldstein BP, Schranz J, Krause DS, Walsh TJ (2007) Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med 356(24):2472–2482. doi:10.1056/NEJMoa066906
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347(6):408–415
Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, Greinix H, Morais de Azevedo W, Reddy V, Boparai N, Pedicone L, Patino H, Durrant S (2007) Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med 356(4):335–347
Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, Helfgott D, Holowiecki J, Stockelberg D, Goh YT, Petrini M, Hardalo C, Suresh R, Angulo-Gonzalez D (2007) Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356(4):348–359. doi:10.1056/NEJMoa061094
Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF (2008) Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 46(3):327–360. doi:10.1086/525258
European LeukemiaNet, European Group for Blood & Marrow Transplantation, European Organization for Research and Treatment of Cancer and International Immunocompromised Host Society (2007). 2007 Update of the ECIL-1 guidelines for antifungal prophylaxis in leukemia patients, including allogeneic HSCT recipients. Available at: http://www.ichs.org/Ecilslides/ECIL2%20%20Antifungal%20prophylaxis%20update%202007.pdf. Accessed 9 Mar 2010
Cornely OA, Bohme A, Buchheidt D, Einsele H, Heinz WJ, Karthaus M, Krause SW, Kruger W, Maschmeyer G, Penack O, Ritter J, Ruhnke M, Sandherr M, Sieniawski M, Vehreschild JJ, Wolf HH, Ullmann AJ (2009) Primary prophylaxis of invasive fungal infections in patients with hematologic malignancies. Recommendations of the infectious diseases working party of the German society for haematology and oncology. Haematologica 94(1):113–122. doi:10.3324/haematol.11665
National Comprehensive Cancer Network (2009) National Comprehensive Cancer Network clinical practice guidelines in oncology: prevention and treatment of cancer-related Infections v.2.2009. Available at: http://www.nccn.org/professionals/physician_gls/PDF/infections.pdf. Accessed 8 Apr 2010
Lipp HP (2011) Posaconazole: clinical pharmacokinetics and drug interactions. Mycoses 54:32–38. doi:10.1111/j.1439-0507.2010.01984.x
Farowski F, Vehreschild J, Cornely OA (2007) Posaconazole: a next-generation triazole antifungal. Future Microbiol 2(3):231–243. doi:10.2217/17460913.2.3.231
Rodriguez MM, Pastor FJ, Calvo E, Salas V, Sutton DA, Guarro J (2009) Correlation of in vitro activity, serum levels, and in vivo efficacy of posaconazole against Rhizopus microsporus in a murine disseminated infection. Antimicrob Agents Chemother 53(12):5022–5025. doi:10.1128/AAC.01026-09
Kishel JJ, Sivik J (2008) Breakthrough invasive fungal infection in an immunocompromised host while on posaconazole prophylaxis: an omission in patient counseling and follow-up. J Oncol Pharm Pract 14(4):189–193. doi:10.1177/1078155208094123
Krishna G, Martinho M, Chandrasekar P, Ullmann AJ, Patino H (2007) Pharmacokinetics of oral posaconazole in allogeneic hematopoietic stem cell transplant recipients with graft-versus-host disease. Pharmacotherapy 27(12):1627–1636. doi:10.1592/phco.27.12.1627
Krishna G, AbuTarif M, Xuan F, Martinho M, Angulo D, Cornely OA (2008) Pharmacokinetics of oral posaconazole in neutropenic patients receiving chemotherapy for acute myelogenous leukemia or myelodysplastic syndrome. Pharmacotherapy 28(10):1223–1232
Jang SH, Colangelo PM, Gobburu JV (2010) Exposure-response of posaconazole used for prophylaxis against invasive fungal infections: evaluating the need to adjust doses based on drug concentrations in plasma. Clin Pharmacol Ther 88(1):115–119. doi:10.1038/clpt.2010.64
Krishna G, Ma L, Vickery D, Yu X, Wu I, Power E, Beresford E, Komjathy S (2009) Effect of varying amounts of a liquid nutritional supplement on the pharmacokinetics of posaconazole in healthy volunteers. Antimicrob Agents Chemother 53(11):4749–4752. doi:10.1128/AAC.00889-09
Kohl V, Muller C, Cornely OA, Abduljalil K, Fuhr U, Vehreschild JJ, Scheid C, Hallek M, Ruping MJ (2010) Factors influencing pharmacokinetics of prophylactic posaconazole in patients undergoing allogeneic stem cell transplantation. Antimicrob Agents Chemother 54(1):207–212. doi:10.1128/AAC.01027-09
AbuTarif MA, Krishna G, Statkevich P (2010) Population pharmacokinetics of posaconazole in neutropenic patients receiving chemotherapy for acute myelogenous leukemia or myelodysplastic syndrome. Curr Med Res Opin 26(2):397–405. doi:10.1185/03007990903485056
Muller C, Arndt M, Queckenberg C, Cornely OA, Theisohn M (2006) HPLC analysis of the antifungal agent posaconazole in patients with haematological diseases. Mycoses 49[Suppl 1]:17–22. doi:10.1111/j.1439-0507.2006.01297.x
Lindbom L, Pihlgren P, Jonsson EN (2005) PsN-Toolkit–a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 79(3):241–257. doi:10.1016/j.cmpb.2005.04.005
Lebeaux D, Lanternier F, Elie C, Suarez F, Buzyn A, Viard JP, Bougnoux ME, Lecuit M, Jullien V, Lortholary O (2009) Therapeutic drug monitoring of posaconazole: a monocentric study with 54 adults. Antimicrob Agents Chemother 53(12):5224–5229. doi:10.1128/AAC.00939-09
Thompson GR 3rd, Rinaldi MG, Pennick G, Dorsey SA, Patterson TF, Lewis JS 2nd (2009) Posaconazole therapeutic drug monitoring: a reference laboratory experience. Antimicrob Agents Chemother 53(5):2223–2224. doi:10.1128/AAC.00240-09
Neubauer WC, Engelhardt M, Konig A, Hieke S, Jung M, Bertz H, Kummerer K (2010) Therapeutic drug monitoring of posaconazole in hematology patients: experience with a new high-performance liquid chromatography-based method. Antimicrob Agents Chemother 54(9):4029–4032. doi:10.1128/AAC.00150-10
Cornely OA, Helfgott D, Krishna G, Carmelitano P, Martinho M, McCarthy M (2010) Pharmacokinetics of different dosing strategies of oral posaconazole, poster A1-042. In: Interscience Conf Antimicrobial Agents and Chemotherapy. Boston
Krishna G, Moton A, Ma L, Medlock MM, McLeod J (2009) Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Ch 53(3):958–966. doi:10.1128/Aac.01034-08
AbuTarif MA, Krishna G, Statkevich P (2010) Population pharmacokinetics of posaconazole in neutropenic patients receiving chemotherapy for acute myelogenous leukemia or myelodysplastic syndrome. Curr Med Res Opin 26(2):397–405. doi:10.1185/03007990903485056
Shields RK, Clancy CJ, Vadnerkar A, Kwak EJ, Silveira FP, Massih RCA, Pilewski JM, Crespo M, Toyoda Y, Bhama JK, Bermudez C, Nguyen MH (2011) Posaconazole serum concentrations among cardiothoracic transplant recipients: factors impacting trough levels and correlation with clinical response to therapy. Antimicrob Agents Ch 55(3):1308–1311. doi:10.1128/Aac.01325-10
Alffenaar JWC, van Assen S, van der Werf TS, Kosterink JGW, Uges DRA (2009) Omeprazole significantly reduces posaconazole serum trough level. Clin Infect Dis 48(6):839–839. doi:10.1086/597110
Farowski F, Cornely OA, Vehreschild JJ, Hartmann P, Bauer T, Steinbach A, Rüping MJGT, Müller C (2010) Intracellular concentrations of posaconazole in different compartments of the peripheral blood. Antimicrob Agents Chemother 54:2928–2931
Cornely OA, Helfgott D, Krishna G, Ma L, Carmelitano P, Martinho M, McCarthy M (2010) Pharmacokinetics of different dosing strategies of oral posaconazole, poster 1237). ICAAC, Boston
Transparency declaration
Carsten Müller, Farowski Fedja, Uwe Fuhr, Michael Hallek, and Victoria Kohl have no conflicts to declare.
JJV has served on the speakers’ bureau of Astellas, Gilead, Merck/Schering-Plough, and Pfizer, and received research grants from Merck/Schering-Plough and Pfizer.
Maria Vehreschild has served on the speakers’ bureau of Astellas, Gilead, Merck/Schering-Plough and Pfizer.
Oliver A Cornely is supported by the German Federal Ministry of Research and Education (BMBF grant 01KN0706), has received research grants from Actelion, Astellas, Basilea, Bayer, Biocryst, Celgene, F2G, Genzyme, Gilead, Merck/Schering, Miltenyi, Optimer, Pfizer, Quintiles, and Viropharma, is a consultant to Astellas, Basilea, F2G, Gilead, Merck/Schering, Mölnlycke, Optimer, and Pfizer, and has received lecture honoraria from Astellas, Gilead, Merck/Schering, and Pfizer.
KAK is a consultant to and has received financial or material support from Merck.
Funding
No funding of any kind was received for this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vehreschild, J.J., Müller, C., Farowski, F. et al. Factors influencing the pharmacokinetics of prophylactic posaconazole oral suspension in patients with acute myeloid leukemia or myelodysplastic syndrome. Eur J Clin Pharmacol 68, 987–995 (2012). https://doi.org/10.1007/s00228-012-1212-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1212-y