Abstract
Background
Despite the increased use of complementary and alternative medicine (CAM) by breast cancer patients, there is little published information regarding CAM use in the Scottish breast cancer population.
Methods
A questionnaire comprising five sections—demographics; perceived health status, prescribed medicines; use, indications, satisfaction and expenditure on CAMs; attitudes towards and factors associated with CAM use; and attitudinal statements—was issued to patients attending the Aberdeen Breast Clinic.
Results
A total of 453 questionnaires were distributed and 360 (79.5%) returned. Respondents were prescribed a mean of 3.2 medicines (95% CI 2.83–3.47). With regard to CAM use, 33.1% of respondents reported current use, 36.4% prior use, and 30.6% reported never having used CAMs. The key indications for use were general well being, boosting immune system and cancer prophylaxis, with high levels of satisfaction reported. The strongest association for CAM use was use by friends and family and higher educational attainment (p < 0.001). Supplements with estrogenic activity, such as soya or red clover, were taken by 29% of respondents. Herbs (echinacea, pomegranate, peppermint, chamomile, grapefruit, garlic, ginseng) that have the potential to interact with adjuvant endocrine therapies (tamoxifen, anastrazole, letrozole, exemestane) were being taken by 38% of treated patients.
Conclusion
The level of CAM use by Scottish breast cancer patients is similar to that reported from other countries, although there are marked differences in the type, nature and frequency of specific CAM therapies. Higher patient education level and use by family and friends were significantly associated with CAM use. The high level of use of potentially disease modifying or interacting herb supplements may be of concern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alternative therapy, also known as complementary medicine, refers to a variety of therapies and practices that are not usually provided by physicians. The World Health Organisation suggests that the terms “complementary medicine” or “alternative medicine” are commonly used inter-changeably with traditional medicine in some countries and that they refer to a broad set of health care practices that are not part of that country’s own tradition and are not integrated into the dominant healthcare system [1]. These health practices, which include acupuncture, homeopathy, herbal medicine, special diets, aromatherapy, energy flow control within the body and psychological therapies, are frequently used in addition to, and sometimes in place of, conventional treatment. Women are larger consumers of healthcare than men, and this extends to their utilisation of complementary and alternative medicine (CAM) [2].
The reasons why women turn to CAM are unclear. However, the desire to have personal control over one’s own health, dissatisfaction with conventional treatment and the perception that conventional medicine has a disregard for a holistic approach, together with concerns about the side effects of prescribed medications have been cited as some of the reasons. However the majority of CAM users do not appear to be dissatisfied with conventional medicine, but find these health care alternatives more congruent with their own values, beliefs and philosophical orientations toward health and life [3]. Whatever the reasons, the prevalence of CAM use as a self-selected component of a particular patient’s treatment regimen is increasing in developed countries [4], with 8–76% of the general population reporting CAM use [5–7].
A similar situation exists amongst specific patient groups, such as those with cancers of various types, who are also reported to be frequent users of complementary therapies [7–10]. The highest use, however, is reported to be amongst women who have been diagnosed with breast cancer. A high proportion of such patients use CAMs, with figures ranging from 17 to 84% [4, 10–21]. Recent results would further suggest that CAM use has increased significantly over the last decade amongst patients with breast cancer from 67% in 1998 to 74% in 2005 [22]. Caution should be exercised, however, in interpreting the results of different CAM studies due to the lack of clear and consistent definitions of CAM used by the authors. The reasons for the widespread and increasing use of CAMs, despite a lack of evidence for benefit, but with evidence from well conducted studies that various complementary therapies are ineffective or, more importantly, may have harmful effects when used in patients with cancer, are unclear [23–33]. However, it is possible that the tacit acknowledgement /approval of CAM use in European Guidelines [34] for the treatment of breast cancer together with the holistic approach adopted by CAM practitioners, which many patients may find rewarding, may be partially responsible for this increasing usage. Two further issues of importance are the potential for herbal remedies to interact with concomitant drug therapies or to exert an unknown/adverse effect on the disease process. Herb-drug interactions are most likely to occur with herbs which induce or inhibit the cytochrome P450 (CYP450) hepatic enzymes and so alter drug metabolism. In particular this may be of importance when considering drugs such as tamoxifen, exemestane, letrezole and toremifene, agents which rely on the CYP450 enzymes either wholly or in part for metabolism [35]. Many supplements also contain phytoestrogens or isoflavones which possess estrogen-like activity, and the potential roles of such agents in the genesis and treatment of breast cancer is complex and far from clear [36, 37].
The aims of the present study, therefore, were to describe CAM use, reasons for use and factors associated with use by a well described population of women with breast cancer in Scotland, to assess their views and attitudes towards CAM use, and to assess the potential for drug interactions with concomitant adjuvant therapies.
Methods
A questionnaire comprising open and closed questions and attitudinal items on five- or six-point Likert scales was developed to explore the use of CAMs by breast cancer patients who attended the Breast Clinic, Aberdeen Royal Infirmary during a 6 month period. We defined CAM use as referring to “the diagnosis, the treatment, and/or the prevention of illness using any means other than an orthodox or conventional medical approach”. The diagnosis, treatment and prevention of medical conditions by practitioners such as acupuncturists, chiropractors, homeopaths or naturopaths as well as the use of herbal products, natural products, minerals or vitamins purchased from a pharmacy, health food outlet or supermarket without a prescription were considered to be CAM.
The questionnaire was reviewed for face and content validity by five doctors and pharmacists and piloted at the Aberdeen Breast Clinic prior to use. The final questionnaire comprised five sections: demographics (seven items); perceived health status, concurrently prescribed medicines (eight items); use of specific CAMs in the previous 24 months including average cost per month (six items); attitudes towards CAM use in general and factors associated with CAM use (four items); attitudinal statements from the multidimensional health locus of control questionnaire (MHLC) covering three six-item subscales: internality, powerful others externality and chance externality [38].
Nursing staff at the clinic provided patients with a pack containing an introductory letter from the clinic consultant, study information leaflet, questionnaire and reply-paid envelope. Questionnaire distribution took place over a 24 week period. Anonymity precluded follow up of non-respondents. Data were analysed using SPSS for Windows version 17.0 (SPSS, Chicago, IL). Chi-squared test, Student’s t-test and Mann Whitney U-test were used to compare users and non-users of CAMs for parametric and non-parametric data where appropriate. P values <0.05 were considered statistically significant. The potential for CAM-drug and CAM-disease interactions was assessed with reference to the Natural Medicines Comprehensive Database, which grades known interactions as major, moderate oe minor and then discusses the theoretical potential for interactions or disease modification [35]. This study was approved by the North of Scotland Research Ethics Committee.
Results
Demographics
A total of 453 questionnaires were distributed over a period of 6 months to eligible patients attending the breast clinic and 360 (79.5%) were returned. Most respondents were over 55 years of age (255, 70.8%) with their breast cancer diagnosed more than 3 years previously (3 months to 9 years).
Concurrent medication
Respondents reported taking a mean of 3.2 prescribed medicines (95% CI 2.83–3.47). Two hundred and twenty-two patients (61.7%) were currently taking specific adjuvant endocrine treatments (106 tamoxifen, 79 anastrazole, 31 letrozole, 8 exemestane), or trastuzumab (8). Ten patients reported taking two of these medicines concurrently.
Complementary and alternative medicine used
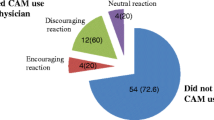
Throughout this paper we classify current and previous CAM users as “Ever Users” and those who have never used CAMs as “Never Users”. One-third (119, 33.1%) of respondents reported current CAM use, and an additional one-third (131, 36.4%) reported use within the previous 24 months. The remainder (110, 30.6%) reported never having used CAMs. Of the CAMs reported used by Ever Users (69.5%, n = 250), the 10 most commonly reported were vitamins and minerals (50.0%), herbal medicines (38.4%), massage (24.4%), reflexology (14.4%), relaxation and visualisation (13.2%), reiki (10.4%), homeopathic medicines (10.0%), aromatherapy (9.6%), acupuncture (6.4%) and chiropractic (3.6%). One-quarter of Ever Users (26.1%) reported the use of other unlisted CAM therapies such as prayer, crystal therapy and yoga. The median number of CAMs reported for Ever Users was 1 [interquartile range (IQR) 1–2]. Table 1 provides detail of the frequency of specific product use by Ever Users. Of the current users, 52.6% were spending up to 10 GBP per month on CAM therapies, 27.6% 11–20 GBP, and 13.8% over 20 GBP per month.
Reasons for CAM use and level of satisfaction
The specific reasons for use of CAM products such as herbal medicines and homeopathy are reported in Table 1, highlighting a range of indications including those related to cancer treatment and prophylaxis. The key reasons given for using other CAM therapies were relaxation and general well being (massage, relaxation and visualisation, reiki, aromatherapy), pain and nausea (reflexology, acupuncture) and back pain (chiropractic). Ever Users reported high levels of satisfaction for all CAM modalities [median 4–5, on a scale of 1 (low) to 5 (high)].
Comparison of Ever Users and Never Users
There were no significant differences between Ever Users and Never Users in terms of age, duration of diagnosis, employment status, health score rating, or number of prescribed medicines (Table 2). However, Ever Users were significantly more likely to report a university education (P = 0.007) and CAM use among their close family (P < 0.001) or friends (P < 0.001).
When asked whether they believed that CAM therapy kept them “well”, half (50.8%) of Ever Users and 3.7% of Never Users replied “yes” (P < 0.001; chi-squared). When asked whether CAMs improved their health, 45.6% of Ever Users and 3.8% of Never Users responded “yes” (P < 0.001; chi-squared). Within the Ever User group, further analysis confirmed that a positive response for both statements was significantly more common in current users when compared to previous users (both, P < 0.001, chi-squared)
Attitudes towards CAM use
Table 3 reports the responses of Ever Users and Never Users towards a series of attitudinal statements on aspects of CAM safety and efficacy. Significantly more Ever Users agreed with the statements “using prescription medicine and complementary and alternative medicine is better than using either one alone” (P = 0.05) and “complementary and alternative medicine should be made available through the NHS” (P = 0.01). Significantly more Ever Users also disagreed with the statement that “patients should only use traditional prescription medicines recommended by their doctors, pharmacists or nurses” (P = 0.002).
Multi-dimensional health locus of control
When asked to respond to a series of statement relating to “internal control” (self) over their disease process, there were no significant differences between Ever and Never Users (Appendix 1). However, when asked to rate statements concerning the role of “powerful others” such as doctors in the disease process, significantly more Ever Users agreed with the statement “following doctor's orders to the letter is the best way to keep my condition from getting any worse” (P = 0.041). There were no significant differences between Ever and Never Users for any other MHLC statements. However, irrespective of CAM use, a high proportion of respondents agreed that “powerful others” played a key role in determining disease outcomes.
Potential for interaction with adjuvant endocrine and trastuzumab therapy
Of the 360 respondents, a total of 105 individuals reported the use of a supplement with possible estrogenic activity including soya, evening primrose, chamomile, garlic, black cohosh and red clover. Of the 222 patients who were currently using adjuvant endocrine and trastuzumab therapy, 84 reported concurrent use of herbal CAM therapies, resulting in a total of 119 possible herb-drug interactions (55 with tamoxifen, 66 with anastrazole, 6 with letrozole and 2 with exemestane).
The herbal supplements most commonly implicated were soya, cranberry, echinacea, glucosamine, grapefruit and garlic.
Discussion
This research was carried out within a breast cancer out-patient clinic at Aberdeen Royal Infirmary to determine types of CAM therapies and products being used by patients together with indications, levels of satisfaction and monthly expenditure. In addition, we assessed the attitudes of CAM Ever Users (current and past users of CAMs) and CAM Never Users to a range of attitudinal items relating to aspects of CAM use and personal health beliefs. CAM use by close family (P < 0.001) or friends (P < 0.001), and university education (P = 0.007) were associated with personal CAM use. Most patients (69.4%) had tried at least one form of CAM over the past 24 months, the three most commonly reported being vitamins and minerals (50.0%), herbal medicines (38.4%) and massage (24.4%).
Ever Users were significantly more likely to agree that CAMs should be supplied by the NHS and that using CAMs in combination with prescribed medicines was better than using either alone. They were more likely to disagree with the statements that CAM should only be used when recommended by healthcare professionals and that “following doctor’s orders to the letter is the best way to keep my condition from getting any worse”.
The high level of CAM use by Scottish women with a diagnosis of breast cancer, identified in this study, is similar to those reported by studies from Europe, Australasia and North America [4, 5, 10–20], indicating that the relevance and importance of such therapies to individual patients transcends national barriers. The role of education level as a key factor in determining CAM use is also consistent with other multinational studies; however of note there was a marked difference in the frequency with which specific CAM therapies were used by the Scottish population. The Scottish clinic population placed a greater emphasis on specific CAM products such as vitamins and minerals and herbal remedies rather than therapies such as spiritual healing and massage [22, 39, 40]. Similarly differences were noted in the types of specific CAM preparations used [22, 39, 40], which is surprising given that these studies were all reporting on patients with a diagnosis of breast cancer. The reasons for these differences are not clear but may reflect local culture, CAM practice and fads. Given the lack of evidence of benefit and the potential for harm with some therapies [41–43], this high level use of CAM may reflect a widespread patient-perceived need for supportive therapy and help.
In this study the most significant determinant for CAM use was use by family and friends, indicating the potential importance of social networks in determining health behaviours. This finding in relation to CAM use has not been previously reported, and although our study does not allow us to comment further on the causal nature of this association, further studies are required to evaluate this. In this study we did not ask respondents about their sources of information for CAM use. However in light of the report by Schmidt et al. concerning the number of CAM sites on the internet and the extensive use of these sources by patients and CAM users, coupled with the resulting potential for misinformation and ensuing dangers, it is important for the clinician to be alert to these issues [44].
It has been suggested by Astin that patients use CAM because of dissatisfaction with medical treatment and that they offer greater personal autonomy and control and are seen as compatible with their values and beliefs [3]. The results of the attitudinal statements and the MHLC in our population add some support to these suggestions in that Ever Users did believe that the use of CAM together with medical therapies was beneficial and that they did not need professional medical advice prior to use. However, in terms of the MHLC, which assesses the role of self, other people and luck in health, health management and outcomes, few differences were observed between Ever Users and Never Users indicating that personal autonomy is not a major association with CAM use. Paradoxically, Never Users were significantly more likely to agree with the statement that “following doctor’s orders to the letter is the best way to keep my condition from getting any worse”, clearly indicating that patient responses to attitudinal statements such as these are complex and deserve further exploration using a qualitative approach.
The potential for herbs to interact with current drug therapies or to modify disease process is recognised although significantly under researched. Herbal supplements such as soya, red clover and ginseng are reported to have direct estrogenic activity, however their actions appear complex and often contradictory [45]. Nevertheless such supplements could have the potential to promote breast cancer in patients when taken singly or, as is often the case, in combination with other sources of phytoestrogens. At present, however, there is no good evidence to confirm or refute these concerns. A further issue is the use of supplements which may directly affect the metabolism or activity of adjuvant endocrine chemotherapy. In this study 52% of patients were currently using adjuvant endocrine (tamoxifen, anastarzole, letrozole or examestane) and trastuzumab therapy. Of these, 40% were using herbal supplements, either singly or in combination, which reportedly have the potential to disrupt the CYP450 enzyme system. The situation however is complex and far from clear as neither the exact metabolic pathways of the adjuvant chemotherapy or of the herbal supplements used by women in this study have been fully elucidated. The metabolism of tamoxifen, anastrazole, letrozole and examestane appears to rely on a combination of CYP450s including 1A1, 1A2, 2A6, 3A4, 3A5, 2B6, 2 C6 and 2D6 [46–49]. Much of the CYP450 metabolic data have been obtained from in vitro human microsome studies, which may not be directly translatable into clinical practice. Several of the herb supplements commonly used in this study, such as echinacea, garlic, ginkgo biloba, valerian and St Johns Wort, have been reported to possess CYP450 enzyme-inducing activity, raising the possibility of reduced chemotherapeutic plasma levels and treatment failure. Although in the case of tamoxifen, which may act at least as a prodrug, increased therapeutic activity could possibly be observed. Similarly grapefruit, peppermint, chamomile, ginkgo biloba, valerian and black cohosh have been reported to inhibit a variety of CYP450 enzymes raising the possibility of impaired metabolism and resultant toxicity. However the potential for such interactions and the possible therapeutic outcomes have not been formally assessed and are far from clear. In the absence of robust data on the potential outcomes of such herb/medication interactions, it would seem more appropriate to avoid herbal supplements until there is good evidence to ensure that neither safety nor efficacy are impaired.
Given these issues and the view of Ever Users that the use of CAM together with medical therapies was beneficial and that they did not need professional medical advice prior to use, there is a clear need for discussion between patients with breast cancer and healthcare professionals on the safe and informed use of CAMs.
There are several strengths to this study. We have added to the sparse published literature relating to use of CAMs, indications for use, levels of satisfaction, expenditure, and factors associated with patient use of CAMs. A high response rate together with a diverse population in relation to the demographic variables makes findings generalisable to other populations of breast cancer patients. However, there are limitations which we acknowledge. Our sample of patients was clustered around one breast cancer out-patient clinic and hence the findings may reflect medical and patient practice in this centre. Although our response rate was high, non-respondents may have replied very differently, and we had no data to compare respondents and non-respondents in terms of demographics. As there was no standard validated questionnaire in the literature (apart from the MHLC), a specific CAM survey tool was developed and piloted for this study. However before use the questionnaire was tested for face and content validity.
Conclusions
The level of CAM use by Scottish breast cancer patients is similar to that reported from other countries although there are marked differences in the type, nature and frequency of specific CAM therapies and preparations. A higher patient education level and use by family and friends were significantly associated with CAM use. Few differences between views and attitudes towards CAM use and health were observed, however where they did occur they served to underline the complex nature of the patient. The use of specific herbal supplements with the potential to interact with adjuvant endocrine chemotherapy appears common and in light of the paucity of data concerning such interactions the precautionary principle should be adopted.
References
The World Health Organisation (2000) http://www.who.int/medicines/areas/traditional/definitions/en/ Accessed 12.09.2010.
Low Dog T (2009) The use of botanicals during pregnancy and lactation. Altern Ther Health Med 15(1):54–61.
Astin AJ (1998) Why patients use alternative medicine. JAMA 279(19):1548–1553
Bensoussan A, Marigliani R, Zorbas H (2008) Use of complementary therapies by Australian women with breast cancer. Breast 17:387–394
Barnes PM, Powell-Griner E, McFann K, Nahin RL (2004) Complementary and alternative medicine use among adults: United States, 2002. Adv Data 27(343):1–19
Yamashita H, Tsukayama H, Sugishita C (2002) Popularity of complementary and alternative medicine in Japan: a telephone survey. Complement Ther Med 10(2):84–93
Menniti-Ippolito F, Gargiulo L, Bologna E, Forcella E, Raschetti R (2002) Use of unconventional medicine in Italy: a nation-wide survey. Eur J Clin Pharmacol 58(1):61–64
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 83(4):777–782
Goldstein MS, Brown ER, Ballard-Barbash R, Morgenstern H, Bastani R, Lee J et al (2005) The use of complementary and alternative medicine among California adults with and without cancer. Evid Based Complement Alternat Med 2(4):557–565
Morris KT, Johnson N, Homer L, Walts D (2000) A comparison of complementary therapy use between breast cancer patients and patients with other primary tumor sites. Am J Surg 179(5):407–411
Molassiotis A, Scott JA, Kearney N, Pud D, Magri M, Selekerova S et al (2005) Complementary and alternative medicine use in breast cancer patients in Europe. Support Care Cancer 14(3):260–267
Boon H, Stewart M, Kennard MA, Pud D, Magri M, Selvekerova S et al (2000) Use of complementary/alternative medicine by breast cancer survivors in Ontario: prevalence and perceptions. J Clin Oncol 18(13):2515–2521
Nagel G, Hoyer H, Katenkamp D (2004) Use of complementary and alternative medicine by patients with breast cancer: observations from a health-care survey. Support Care Cancer 12(11):789–796
Shen J, Andersen R, Albert PS, Wenger N, Glaspy J, Cole M et al (2002) Use of complementary/alternative therapies by women with advanced-stage breast cancer. BMC Complement Altern Med 2:8
Helyer LK, Chin S, Chui BK, Fitzgerald B, Verma S, Rakovitch E et al (2006) The use of complementary and alternative medicines among patients with locally advanced breast cancer—a descriptive study. BMC Cancer 6:39
DiGianni LM, Garber JE, Winer EP (2005) Complementary and alternative medicine use among women with breast cancer. J Clin Oncol 20(Suppl 18):34–38
Crocetti E, Crotti N, Feltrin A, Ponton P, Geddes M, Buiatti E (1998) The use of complementary therapies by breast cancer patients attending conventional treatment. Eur J Cancer 34(3):324–328
Rees R, Feigel I, Vickers A, Zollman C, McGurk R, Smith C (2000) Prevalence of complementary therapy use by women with breast cancer: a population-based survey. Eur J Cancer 36:1359–1364
Moschen R, Kemmler G, Schweigkofler H, Holzner B, Dunser M, Richter R et al (2001) Use of alternative / complementary therapy in breast cancer patients—a psychological perspective. Support Care Cancer 9:267–274
Burstein HJ, Gelber S, Guadagnoli E, Weeks JC (1999) Use of alternative medicine by women with early stage breast cancer. N Engl J Med 340(22):1733–1759
Balneaves LG, Bottorff JL, Hislop TG, Herbert C (2006) Levels of commitment: exploring complementary therapy use by women with breast cancer. J Altern Complement Med 12(5):459–466
Boon HS, Olatunde F, Zick SM (2007) Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health 7:4. doi:10.1186/1472-6874-7-4
Vickers AJ, Kup J, Cassileth BR (2006) Unconventional anticancer agents; a systematic review of clinical trials. J Clin Oncol 24(1):136e40
Miller DR, Anderson GT, Stark JJ, Granick JL, Richardson D (1998) Phase I/II trial of the safety and efficacy of shark cartilage in the treatment of advanced cancer. J Clin Oncol 16(11):3649–3655
Moertel CG, Fleming TR, Creagan ET, Rubin J, O’Connell MJ, Ames MM (1985) High dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomised double-blind comparison. N Engl J Med 312(3):137–141
Creagan ET, Moertel CG, O’Fallon JR, Schutt AJ, O’Connell MJ, Rubin J et al (1979) Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N Engl J Med 301(13):687–690
Werneke U, Earl J, Seydel C, Horn O, Crichton P, Fannon D (2004) Potential health risks of complementary alternative medicines in cancer patients. Br J Cancer 90(2):408–413
Cassileth BR, Vickers AJ (2005) High prevalence of complementary and alternative medicine use among cancer patients: implications for research and clinical care. J Clin Oncol 23(12):1–3
Labriola D, Livingstone R (1999) Possible interactions between dietary antioxidants and chemotherapy. Oncology 13(7):1003e8
Boyle FM (1997) Adverse interaction of herbal medicine with breast cancer treatment. Med J Aust 167(5):286
Bairati I, Meyer F, Gelinas M, Fortin A, Nabid A, Brochet F et al (2005) A randomized trial of antioxidant vitamins to prevent second primary cancers in head and neck cancer patients. J Natl Cancer Inst 97(7):481–488
Cassidy A (2003) Are herbal remedies and dietary supplements safe and effective for breast cancer patients? Breast Cancer Res 5(6):300–302
Meijerman I, Beijnen JH, Schellens (2006) Herb-drug interactions in oncology: focus on mechanisms of induction. Oncologist 11(7):742–752
Baum M, Ernst E, Lejeune S, Horneber M (2006) Role of complementary and alternative medicine in the care of patients with breast cancer: report of the European Society of Mastology (EUSOMA) Workshop, Florence, Italy, December 2004. Eur J Cancer 42:1702–1710
Therapeutic Research Faculty (2011) Natural medicines comprehensive database. http://naturaldatabase.therapeuticresearch.com/home.aspx?cs=&s=ND. Accessed August 2011
Dong JY, Qin LQ (2011) Soy isoflavones consumption and risk of breast cancer incidence or recurrence: a meta-analysis of prospective studies. Breast Cancer Res Treat 125:315–323
Patisaul HB, Jefferson W (2010) The pros and cons of phytoestrogens. Front Neuroendocrinol 31:400–419
Wallston KA (2007) The multidimensional health locus of control. http://www.vanderbilt.edu/nursing/kwallston/mhlcscales.htm. Accessed 2011
Myers CD, Jacobsen PB, Huang Y, Frost MH, Patten CA, Cerhan JR, Sellers TA (2008) Familial and perceived risk of breast cancer in relation to use of complementary medicine. Cancer Epidemiol Biomarkers Prev 17(6):1527–1534
Mueller CM, Mai Pl, Bucher J, Peters JA, Loud JT, Greene MH (2008) Complementary and alternative medicine use among women at increased genetic risk of breast and ovarian cancer. BMC Complement Altern Med 8:17
Werneke U, Earl J, Seydel C, Horn O, Crichton P, Fannon D (2004) Potential health risks of complementary alternative medicines in cancer patients. Br J Cancer 90:408–413
Monroe KR, Murphy SP, Kolonel LN, Pike MC (2007) Prospective study of grapefruit intake and risk of breast cancer in postmenopausal women: the Multiethnic Cohort Study. Br J Cancer 97:440–445
Spencer EA, Key TJ, Appleby PN, van Gils CH, Olsen A, Tjonneland A, Clavel-Chapelon F, Boutron-Ruault MC, Touillaud M, Sanchez MJ, Bingham S, Khaw KT, Slimani N, Kaaks R, Riboli E (2009) Prospective study of the association between grapefruit intake and risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Causes Control 20(6):803–809
Schmidt K, Ernst E (2004) Assessing websites on complementary and alternative medicine for cancer. Annal Oncol 15:733–742
Helferich WE, Andrade JE, Hoagland MS (2008) Phytoestrogens and breast cancer: a complex story. Inflammopharmacology 16:219–226
Kamdem LK, Liu Y, Stearns V et al (2010) In vitro and in vivo oxidative metabolism and glucuronidation of anastrozole. Br J Clin Pharmacol 70(6):854–869
Desta Z, Ward BA, Flockhart DA (2005) In vitro letrozole N-dealkylation is mainly catalyzed by human cytochrome P450 (CYP) 3A. Clin Pharm Ther 77:79
Kamdem LK, Flockhart DA, Desta Z (2011) In vitro cytochrome P450-mediated metabolism of exemestane. Drug Metab Dispos 39(1):98–105
Crewe HK, Notley LM, Wunsch RM et al (2002) Metabolism of tamoxifen by recombinant human cytochrome P450 enzymes: formation of the 4-hydroxy, 4′-hydroxy and N-desmethyl metabolites and isomerization of trans-4-hydroxytamoxifen. Drug Metab Dispos 30(8):869–874
Conflict of interest
All authors state that they have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Rights and permissions
About this article
Cite this article
McLay, J.S., Stewart, D., George, J. et al. Complementary and alternative medicines use by Scottish women with breast cancer. What, why and the potential for drug interactions?. Eur J Clin Pharmacol 68, 811–819 (2012). https://doi.org/10.1007/s00228-011-1181-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1181-6