Abstract
Purpose
To assess the effect of tezosentan, a parenteral dual ET receptor antagonist, on splanchnic and systemic hemodynamics in patients with cirrhosis. In addition, the safety, pharmacokinetics, and pharmacodynamics of tezosentan were evaluated.
Methods
The population consisted of patients with cirrhosis with clinically significant portal hypertension. This was a randomized, double-blind, multicenter study. The patients were randomized 3:1 to tezosentan (3 mg/h for 2–3 h) or placebo. HVPG, hepatic blood flow (HBF, ICG method), and systemic arterial pressures were measured before and after tezosentan administration. Plasma concentrations of tezosentan and ET-1 were determined peripherally and in the hepatic vein.
Results
Eighteen patients received tezosentan and six placebo. Baseline clinical, biochemical, and hemodynamic characteristics were balanced between the two groups. There was no significant treatment effect on HVPG. The extraction ratio (0.31), the plasma clearance of ICG (280 ml/min), and the HBF (1,430 ml/min) did not show any relevant changes during the infusion of tezosentan, and there were no differences between placebo- and tezosentan-treated patients. A linear relationship was observed between the maximum-fold increase in ET-1 concentration and the steady-state tezosentan plasma concentration (r = 0.82). There was a strong correlation (r = 0.88) between plasma clearance of ICG and that of tezosentan (10.2 l/h). Arterial pressure and heart rate did not significantly change in either group.
Conclusion
In patients with cirrhosis, a 2- to 3-h tezosentan infusion was safe and well tolerated but did not change the HVPG. Tezosentan infusion had no influence on the extraction ratio and plasma clearance of ICG and did not change HBF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with cirrhosis, portal hypertension develops as a consequence of both hyperdynamic circulation and increased hepatic vascular resistance mediated by several neurohormones, including endothelins [1, 2]. Endothelin is one of the most potent and long-lasting vasoconstrictors isolated [3]. Endothelin-1, synthesized predominantly by the vascular endothelium, is considered one of the humoral factors modulating intrahepatic vascular resistance and is, therefore, implicated in the pathophysiology of portal hypertension [1]. Elevated plasma concentrations of endothelin-1 and endothelin-3 have been found in patients with cirrhosis [4–9], which may be the result of increased hepatic, splanchnic, and renal production as well as decreased hepatic clearance. Elevated endothelin-1 plasma and hepatic tissue concentrations correlate with the severity of cirrhosis and the hepatic venous pressure gradient (HVPG) [6, 8]. Several experimental studies have shown that oral administration of bosentan, a dual ETA and ETB receptor antagonist, significantly reduced the degree of portal hypertension in cirrhotic rats [10–12]. The effects of this class of drugs have, however, never been evaluated on the splanchnic circulation in patients with cirrhosis and portal hypertension. Thus the aim of this investigation was to assess the effects of tezosentan, a dual ET receptor antagonist optimized for parenteral use [13], on splanchnic and systemic hemodynamics in patients with cirrhosis. In addition, the safety, pharmacokinetics, and pharmacodynamics of tezosentan were evaluated in these patients. Tezosentan was selected as model drug to explore the concept of endothelin receptor antagonism because, in comparison to bosentan, it shows low pharmacokinetic variability, and steady-state conditions can be achieved more rapidly. In healthy subjects, the plasma concentration-time profile of tezosentan is characterized by a pronounced and rapid disposition phase with a half-life of 6 min followed by a slower phase with a half-life of about 3 h [14]. Tezosentan is predominantly excreted via the feces with less than 5% of an administered radiolabeled dose of tezosentan recovered in urine [15]
Patients and methods
Patients
The population consisted of patients with cirrhosis with clinically significant portal hypertension, i.e., HVPG ≥12 mm Hg during the hemodynamic study. Cirrhosis was proved by clinical, chemical, and ultrasonography or histological criteria. Patients were expected to have advanced cirrhosis but be in stable condition. Other inclusion criteria were as follows: age between 18 and 70 years; serum bilirubin <6 mg/dl; supine systolic blood pressure between 90 and 140 mm Hg; supine diastolic blood pressure between 50 and 90 mm Hg; supine mean arterial blood pressure greater than 70 mm Hg; hematology and biochemistry tests within normal range of the ongoing illness; abstained from alcohol consumption for at least 5 days prior to the study; stable concomitant medications; and having given written informed consent. Exclusion criteria were pregnancy; bacterial peritonitis; serum creatinine >1.3 mg/dl; INR >2 or platelets count <50 × 109 cells/L; hepatic encephalopathy (grade >1); paracentesis within 5 days prior to the study; acute gastrointestinal bleeding within 7 days prior to the study; hepatocellular carcinoma; previous surgical or transjugular portosystemic shunts; life expectancy less than 2 months; participation in another clinical study during the month prior to the screening examination; and concomitant medications that may affect blood pressure including beta-blockers, nitrates, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and vasopressors as well as those that may affect the pharmacokinetics of tezosentan such as cyclosporine A and tacrolimus.
Study design
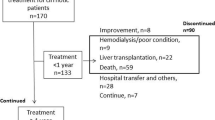
This randomized, double-blind, multicenter study consisted of screening, treatment, and follow-up periods. After providing written informed consent, eligible patients were enrolled into a screening period of less than 4 h in which a medical history was taken and baseline values for clinical laboratory tests, Child-Pugh score, HVPG, and plasma ET-1 levels were obtained. If after screening the patient remained eligible, the patient was randomized 3:1 to tezosentan (0.756 mg/ml), supplied by Actelion Pharmaceuticals, or placebo (normal saline), and study treatment was to be administered as a 3 mg/h continuous intravenous infusion (4 ml/h) over 2–3 h (determined by approval by Ethics Committee). A one-step down-titration to 1 mg/h or permanent discontinuation of study treatment could occur at any time for reasons of tolerability or safety. If, after down-titration, the dose was well tolerated, it was to remain at 1 mg/h until the treatment period was completed.
Vital signs (blood pressure and heart rate) assessments, measurement of occluded and free hepatic venous pressures, and blood drawing for clinical laboratory were performed periodically, and adverse events and concomitant medication were monitored throughout the study (Fig. 1). Blood sampling for tezosentan and ET-1 measurements was performed at screening (ET-1 only), and at 0.25, 0.5, 1, 2, 3, 3.25, 4, 5, 6, and 7 h after start of the tezosentan infusion. Indocyanine green in peripheral and hepatic vein plasma was determined at screening and at 0.5, 1, 2, and 3 h after start of the tezosentan infusion.
The tezosentan dose of 3 mg/h was selected based on experience in cirrhotic patients with tezosentan 0.2–5.0 mg/h given for up to 2 days [16]. In patients with advanced cirrhosis, doses of 0.2, 1, and 5 mg/h administered over 2 days were well tolerated. Therefore, a dose of 3 mg/h was to be administered for 2–3 h in this study, a period considered long enough for a proof-of-concept study and at the same time feasible with respect to the standard of care in this patient population.
Hemodynamics
Hemodynamic measurements were performed in fasting conditions as previously described [17, 18]. Briefly, patients were placed in a supine position for at least 4 h before the study. Catheter was introduced into the right jugular vein using the Seldinger technique under local anesthesia and mild sedation. Under fluoroscopic control, a 5 F balloon-tipped catheter (Medi-Tech; Boston Scientific Cork, Cork, Ireland) was advanced into the main right hepatic vein for repeated measurements of occluded and free hepatic venous pressures. HVPG was calculated as the difference between occluded and free hepatic venous pressures. All measurements were performed at least in duplicate and repeated until two consecutive reliable measurements did not differ by more than 1 mm Hg. The mean of these two measurements was considered the final value.
Hepatic blood flow (HBF) was measured using the indocyanine green (ICG) continuous infusion method [19, 20]. Peripheral and hepatic venous samples were drawn simultaneously at 3-min intervals to allow measurement of ICG clearance and extraction. At each available time point, plasma ICG concentrations were determined in three separate samples, and the mean of these three values (Css) was used in the calculations. The ICG extraction ratio was calculated according to the following formula: (ICG peripheral vein plasma concentration – ICG hepatic vein plasma concentration) / (ICG peripheral vein plasma concentration). The plasma clearance of ICG (CLplasma) was determined as infusion rate/Css; the blood clearance (CLblood) as CLplasma/(1 − Ht), where Ht is the hematocrit measured before the start of drug infusion; and the HBF as CLblood/ICG extraction ratio.
Arterial pressure and heart rate were measured using an external sphygmomanometer (Dinamap, Critikon, Tampa, FL). Mean arterial pressure (MAP) was calculated using the following formula: MAP = [systolic arterial pressure + (2 × diastolic arterial pressure)]/3.
Pharmacokinetics and pharmacodynamics
Plasma samples were collected for determination of pharmacokinetic (including the hepatic extraction ratio) and pharmacodynamic (reflected in increases in ET-1 levels) characteristics of tezosentan. Pharmacokinetic evaluations were performed noncompartmentally using WinNonlin version 4.0.1 (Pharsight, Mountain View, CA). Css, the steady-state concentration, was determined as the mean of the two concentration values determined immediately before discontinuation of the drug infusion. CL, the systemic clearance, was estimated by CL = dose/AUC0–t, in which the latter is the area under the plasma concentration-time curve from time point zero to the last sampling time with a concentration above the limit of quantification, calculated according to the linear trapezoidal rule. The extraction ratio of tezosentan was determined as (peripheral vein plasma concentration – hepatic vein plasma concentration) / (peripheral vein plasma concentration). For ET-1 the maximum increase in plasma concentration as compared to the ET-1 concentration before the start of drug infusion was calculated. The ET-1 extraction ratio was determined as for tezosentan.
Bioanalytical assessments
Blood samples were collected in EDTA-containing tubes. Samples were immediately centrifuged at 2–8°C for 30 min and stored at −80°C pending analysis by a central laboratory. Samples were shipped on dry-ice which had been shown previously not to affect their stability.
Quantification of tezosentan in plasma samples was performed by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS) operating in the positive ionization mode [21]. The lower limit of quantification was 0.25 ng/ml. The inter-assay accuracy ranged from 99.4 to 100.6%, whereas imprecision was ≤5.0%.
Plasma concentrations of ET-1 were determined with a commercially available luminescence immunoassay kit (QET00, R&D Systems Europe, Oxon, UK). The lower limit of quantification was 0.32 pg/ml. Imprecision of the assay ranged between 2.5 and 9.9%.
Plasma concentrations of ICG were determined by high performance liquid chromatography with ultraviolet detection, based on a method described previously [22]. The lower limit of quantification was 100 ng/ml. The inter-assay accuracy ranged from 108.4 to 113.1%, whereas imprecision was ≤6.1%.
Safety
Blood pressure, heart rate, standard hematology, and biochemistry laboratory parameters were assessed periodically, and adverse events and concomitant medication were monitored throughout the study.
In patients with persistent hypotension (a decrease in supine mean blood pressure by ≥30% or below 65 mm Hg) at 4 h after discontinuation of study treatment, hourly measurements of blood pressure were continued until blood pressure returned to baseline ± 10%.
After the treatment stop, patients were followed for 24 h for overall safety and up to 28 days for serious adverse events and deaths.
Statistical analysis
The sample size of this study was based on empirical considerations, and no formal hypotheses were set. Exploratory treatment comparisons were performed without multiplicity correction. For continuous endpoints, the t-test and the Wilcoxon Mann-Whitney were carried out. HVPG response rates were analyzed using the two-sided Fisher exact test. Several correlations between pharmacokinetic and pharmacodynamic variables were explored. In each of these analyses, linear regression lines with their 95% confidence intervals and the Pearson correlation coefficient, r, with its associated p-value were determined.
Results
Twenty-four patients were randomized, 18 to receive tezosentan and 6 placebo. All patients received study treatment and completed the study.
Baseline demographic, clinical, and biochemical characteristics (Table 1) as well as hemodynamic values (Table 2) were balanced between the two studied groups.
Hemodynamics
HVPG decreased in some patients (Fig. 2), but the mean value did not change to a relevant extent in either group (Table 2). Accordingly, there was no significant treatment effect.
The extraction ratio, the plasma clearance of ICG, and HBF did not show any relevant changes during the infusion of tezosentan, and there were no changes between placebo- and tezosentan-treated patients (Table 3). At the end of the tezosentan infusion, the correlation between HBF and ICG was significant (r = 0.90, p < 0.05).
Arterial pressure and heart rate did not significantly change in either group (Table 4).
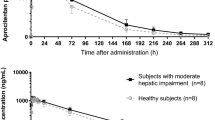
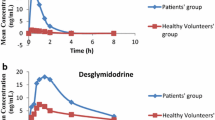
Pharmacokinetics and pharmacodynamics of tezosentan
The mean tezosentan plasma concentration-time profile in patients receiving either a 2- or 3-h infusion is presented in Fig. 3. The geometric mean values (95% CI) of the derived pharmacokinetic parameters were as follows: Css 268 (189, 379) ng/ml; AUC0–t 627 (439, 894), and CL 10.2 (7.3, 14.1) l/h. The arithmetic mean value (SD) for the tezosentan extraction ratio was 0.28 (0.16). The concentration-time profiles indicate that in most but not all patients steady-state conditions were approached at discontinuation of the drug infusion. After termination of the infusion, the concentrations declined rapidly following a biphasic profile. The plasma ET-1 concentration-time profile in patients treated with tezosentan was very similar to that of tezosentan whereas the patients receiving placebo showed no ET-1 response. The maximum plasma ET-1 concentration was only reached towards the end of the infusion, suggesting that steady-state conditions had not yet been attained. Upon discontinuation of the tezosentan infusion, ET-1 concentrations quickly decreased, albeit in a slightly slower fashion than concentrations of tezosentan itself. The descriptive statistics of the derived ET-1 parameters—maximum-fold increase in ET-1 concentration as compared to baseline and the extraction ratio—are shown in Table 5.
Significant but not very strong correlations were found between total bilirubin concentration and tezosentan exposure, i.e., area under the plasma concentration-time curve (r = 0.5–0.6) and between pairs of extraction ratios of tezosentan, ET-1, and ICG (r = 0.4). A linear relationship was observed between the maximum-fold increase in ET-1 concentration and the steady-state plasma tezosentan concentration (r = 0.82, p < 0.05; Fig. 4). A significant correlation was also found between the plasma clearance of ICG and that of tezosentan (r = 0.88, p < 0.05). There was no correlation between the baseline hepatic blood flow and HVPG (r = 0.17).
Safety
A 2- or 3-h infusion of tezosentan 3 mg/h was well tolerated with no indications for a safety concern. No patient experienced hypotension that required down-titration or premature discontinuation (main safety endpoint). Mean decreases in blood pressures were observed in both treatment groups during treatment (changes in MAP at 2 h of −4.7 ± 10.8 and −1.7 ± 6.5 mm Hg in tezosentan and placebo group, respectively) as well as over the subsequent 4 h (−7.3 ± 12 and −8.7 ± 8.5 mm Hg in tezosentan and placebo group, respectively). Changes in pulse rate were small. Very little change was observed in Child-Pugh score. Child-Pugh class worsened in two tezosentan-treated patients because of small changes in albumin and bilirubin. Adverse events were experienced by 27.8 and 16.7% of tezosentan- and placebo-treated patients, respectively. The events reported for tezosentan-treated patients were headache, collapsed vein, and anxiety, occurring during the infusion, and nausea and renal impairment, reported during the 24 h following the end of treatment. Renal function impairment was secondary to renal calculi and returned to normal following surgical management. None of the events were severe or serious, none required a change in study treatment, and all events were resolved at the end of the study. A mild mean increase in serum total bilirubin was observed in the tezosentan-treated group (mean 6.0 ± 10.7 μmol/l); no patient had a marked bilirubin increase. Other changes in clinical laboratory test results were minimal or not considered clinically relevant.
Discussion
In this study, tezosentan 3 mg/h infused for 2 or 3 h proved safe and tolerable in patients with cirrhosis and portal hypertension but did not show a significant effect on the degree of portal hypertension estimated by the HVPG compared with placebo. In the patients studied, HVPG decreased in both treatment groups at all time points assessed. No consistent effect on HVPG was observed. In spite of the small number of patients, the variability was higher than expected based on published data [23]. When results were analyzed by center, it appeared that a greater decrease in HVPG was obtained with tezosentan than placebo at the center with the largest enrollment. The study was not powered to determine efficacy, and all testing of treatment effect was exploratory. A larger proportion of patients in the tezosentan than placebo group showed a response (i.e., ≥20% decrease from baseline HVPG or an HVPG ≤ 12 mm Hg), but the difference was small.
In patients with cirrhosis, the lack of splanchnic hemodynamic effects of tezosentan is unclear. This is in contrast to observations in cirrhotic rats in which bosentan, another dual ETA and ETB receptor antagonist, significantly reduced the degree of portal hypertension [10, 11]. Certain comments, however, can be made. The evaluation of portal hypertension differs between patients with cirrhosis and cirrhotic rats. In patients, the degree of portal hypertension was estimated by the HVPG, while in rats it was directly measured in the portal vein, and it is known that, after drug administration, measurement of the HVPG may not provide a reliable estimation of the changes in portal pressure [24]. In addition, a slight decrease in hepatic vascular resistance may induce an elevation of portal blood flow, which may result in an absence of change in portal hypertension. The lack of significant change in hepatic blood flow following tezosentan administration does not contradict this hypothesis since hepatic blood flow depends on both hepatic arterial and portal blood flows. It is also possible that the dose of tezosentan was too low to induce a reduction of hepatic vascular resistance or the treatment duration was too short to have an effect on the splanchnic circulation. Nevertheless, in this investigation performed in patients with cirrhosis, tezosentan administration had no or only minor effects on the splanchnic and systemic circulation.
The concentration-time profiles of tezosentan in this study indicate that steady-state conditions had not yet been completely attained within 2–3 h. This is in accordance with data suggesting that in cirrhotic patients it takes approximately 6 h before attainment of steady-state conditions [16]. However, since steady-state conditions were approached, it is unlikely that this explains the lack of therapeutic effect in this study. Infusions of longer duration were considered questionable from an ethical point of view. The clearance of tezosentan in this study was approximately 10 l/h, similar to the value obtained in the previous study on cirrhotic patients [16]. The extraction ratio of tezosentan was approximately 0.28. This confirms extraction of tezosentan from the systemic circulation on passage through the liver. On the basis of this extraction ratio, the systemic clearance of tezosentan determined in this study (10 l/h), and the hematocrit value measured (mean of 0.36 at baseline in 18 patients on tezosentan), HBF was estimated to be 930 ml/min, which is slightly lower than the overall value of 1,340 ml/min as determined with the ICG-clearance method in this same study. It has previously been shown that the level of bilirubin is associated with the clearance of tezosentan, probably because both substrates, being di-anions, make use of MRP2 (also called cMOAT), an ATP-binding cassette transporter, for excretion into the bile [25]. In this study, the correlations between exposure to tezosentan and bilirubin levels were not very strong, probably due to the fact that the range of bilirubin levels covered was limited. Patients with bilirubin levels > 100 μmol/l (> 6 mg/dl) were not allowed to enter the study. Bilirubin levels differed somewhat between the start and end of the infusion, which may be due to competition between tezosentan and bilirubin for bile excretion. In patients with cirrhosis, therefore, bilirubin levels may be increased during tezosentan infusion.
Infusion of tezosentan at a rate of 3.0 mg/h resulted in a mean increase in ET-1 plasma concentrations of 5.0-fold, compared with 1.5-fold with placebo. Healthy subjects who were administered tezosentan at 2.5 mg/h showed a 2.2-fold increase in ET-1 [26]. This difference between healthy subjects and cirrhotic patients is in accordance with the higher exposure to tezosentan in the latter. The maximum-fold ET-1 increase and the steady-state plasma tezosentan concentration showed a linear relationship. The mean extraction ratio of ET-1 in tezosentan-treated patients was 0.21, which indicates that ET-1 is extracted by the liver from the systemic circulation. The clearance of ET-1 determined via a radiotracer technique has been shown to be approximately 4.6 l/min [27], which is considerably greater than liver blood flow (1.5 l/min) and approaches total cardiac output (6.0 l/min). The lung has been suggested as the major site of ET-1 clearance since it is able to remove over 40% of the ET-1 presented to it [28]. The results of the present study indicate that, at least in the presence of tezosentan, the liver contributes to ET-1 elimination. Whether or not ETB receptors in the liver represent a high-capacity/clearance site for circulating ET-1 is unknown [28]. In rats, inhibition of both ETA and ETB receptors by bosentan has been shown to increase the plasma half-life of ET-1 and to shift tissue uptake from lung to liver and kidneys [29].
The clearance of ICG and HBF were estimated on the basis of the ICG infusion method, which is considered the gold standard [19, 20]. ICG, a tricarbocyanine dye, is an anionic model compound widely used for studying liver transport. In healthy subjects, its extraction ratio is thought to be greater than 0.7 [19]. In patients with liver disease, the ICG extraction ratio may be considerably lower than in healthy subjects, and it is not valid to equate ICG clearance directly with liver blood flow [19]. Therefore, in this study the extraction ratio of ICG was also determined. Steady-state conditions had been attained before peripheral and hepatic vein samples were taken. An equilibration period of 45 min has previously been shown to be sufficient to reach steady-state conditions [20]. Attainment of steady-state conditions avoided the need to apply a pharmacokinetic model to the plasma ICG concentration-time data [19]. To reduce variability, paired samples were taken at 5-min intervals. A selective high performance liquid chromatography method was used to determine plasma ICG concentrations. This method avoids possible perturbations due to the presence of ICG metabolites or impurities, which may lead to bias when nonspecific spectrophotometric assays are used [30, 31]. The extraction ratio of ICG measured in this study (0.31 at baseline, n = 22) is in close accordance with values of 0.30 determined by Navasa et al. [32] in 26 cirrhotic patients and of 0.26 determined by Gadano et al. [20] in 356 patients with chronic liver disease. The average plasma clearance of ICG at baseline (n = 22) was approximately 280 ml/min as compared with values of 210 ml/min (n = 26) and 182 ml/min (n = 356) obtained by Navasa et al. [32] and Gadano et al. [20], respectively. The fact that patients with severe disease, at least with respect to bilirubin levels, were excluded may explain the higher values in the present study. The range of values obtained was 20-fold. Similar to the ICG extraction ratio profile, the mean plasma clearance of ICG did not show a pattern that would suggest a distinction between the patients treated with tezosentan and placebo. The correlation between the plasma clearance of ICG and that of tezosentan was markedly stronger than for the respective extraction ratios. These data suggest that similar mechanisms are responsible for the elimination of ICG and tezosentan, in line with the fact that both compounds are di-anions. The liver blood flow, HBF, is determined as a ratio of clearance and the extraction ratio of ICG, and, therefore, is prone to variability. Overall, no effect of tezosentan on HBF was detected in this study. The average value in this study (1,430 ml/min at baseline, n = 20) is very similar to that obtained in a large sample of cirrhotic patients (1,260 ml/min, n = 356) and does not differ significantly from the value in healthy subjects (circa 1,200 ml/min for a 70-kg person) [31]. A relatively strong correlation was observed between HBF and ICG clearance. A large sample of 356 cirrhotic patients showed no significant correlation between these variables, in contrast to controls (healthy subjects) and patients with hepatic fibrosis [20]. It has been stated previously [20] that the relationship between liver lesions and HBF is not clear, which has led some authors to conclude that assessment of HBF does not provide any useful information in the evaluation of patients with cirrhosis. Actually, hepatic ICG clearance appeared to be more useful than HBF to assess the severity of liver disease [20]. These findings were also obtained in the present study, albeit with a much lower patient number. It also appears from this study that plasma clearance of ICG is a more useful variable than its extraction ratio and the derived HBF. In a 356-patient study, no correlation was observed between HBF and age, type of cirrhosis, severity of the disease as evaluated by the Child-Pugh score, the degree of portal hypertension, or other hemodynamic variables [20]. Findings of the present study were similar.
In conclusion, in patients with portal hypertension secondary to cirrhosis, a 2- or 3-h tezosentan infusion was safe and well tolerated but did not reduce the HVPG. The increase in plasma ET-1 concentration correlated with tezosentan exposure. Tezosentan infusion had no influence on the extraction ratio and plasma clearance of ICG and did not change HBF.
Abbreviations
- CL:
-
Clearance
- E:
-
Extraction ratio
- HBF:
-
Hepatic blood flow
- HR:
-
Heart rate
- HVPG:
-
Hepatic venous pressure gradient
- ICG:
-
Indocyanine green
- MAP:
-
Mean arterial pressure
References
Iwakiri Y, Grisham M, Shah V (2008) Vascular biology and pathobiology of the liver: report of a single-topic symposium. Hepatology 47:1754–1763
Rockey D (1997) The cellular pathogenesis of portal hypertension: stellate cell contractility, endothelin, and nitric oxide. Hepatology 25:2–5
Yanagisawa M, Kurihara H, Kimura Y, Tomobe Y, Kobayashi M, Mitsui Y et al (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415
Moore K, Wendon J, Frazer M, Karami J, Williams R, Badr K et al (1992) Plasma endothelin immunoreactivity in liver disease and the hepatorenal syndrome. N Engl J Med 327:1774–1778
Uchihara M, Izumi N, Sato C, Marumo F (1992) Clinical significance of elevated plasma endothelin concentration in patients with cirrhosis. Hepatology 16:95–99
Hartleb M, Kirstetter P, Moreau R, Soupison T, Pussard E, Hadengue A et al (1994) Relations entre les concentrations plasmatiques d’endotheline et la severite de la cirrhose. Gastroenterol Clin Biol 18:407–412
Salo J, Francitorra A, Follo A, Navasa M, Ginès A, Jiménez W et al (1995) Increased plasma endothelin in cirrhosis. Relationship with systemic endotoxemia and response to changes in effective blood volume. J Hepatol 22:389–398
Moller S, Gülberg V, Henriksen JH, Gerbes AL (1995) Endothelin-1 and endothelin-3 in cirrhosis: relations to systemic and splanchnic haemodynamics. J Hepatol 23:135–144
Bernardi M, Gülberg V, Colantoni A, Trevisani F, Gasbarrini A, Gerbes AL (1996) Plasma endothelin-1 and -3 in cirrhosis: relationship with systemic hemodynamics, renal function and neurohumoral systems. J Hepatol 24:161–168
Sogni P, Moreau R, Gomola A, Gadano A, Cailmail S, Calmus Y et al (1998) Beneficial hemodynamic effects of bosentan, a mixed ETA and ETB receptor antagonist, in portal hypertensive rats. Hepatology 28:655–659
Reichen J, Gerbes AL, Steiner MJ, Sägesser A, Clozel M (1998) The effect of endothelin and its antagonist bosentan on hemodynamics and microvascular exchange in cirrhotic liver. J Hepatol 28:1020–1030
Rockey DC, Weisiger RA (1996) Endothelin-induced contractility of stellate cells from normal and cirrhotic rat liver: implications for regulation of portal pressure and resistance. Hepatology 24:233–240
Clozel M, Ramuz H, Clozel JP, Breu V, Hess P, Löffler BM et al (1999) Pharmacology of tezosentan, new endothelin receptor antagonist designed for parenteral use. J Pharmacol Exp Ther 290:840–846
Dingemanse J, Clozel M, van Giersbergen PLM (2002) Entry-into-human study with tezosentan, an intravenous dual endothelin receptor antagonist. J Cardiovasc Pharmacol 39:795–802
Treiber A, van Giersbergen PLM, Dingemanse J (2003) In vivo and in vitro disposition profile of tezosentan, an intravenous dual endothelin receptor antagonist, in humans. Xenobiotica 33:399–414
Dingemanse J, Halabi A, van Giersbergen PLM (2009) Influence of liver cirrhosis on the pharmacokinetics, pharmacodynamics, and safety of tezosentan. J Clin Pharmacol 49:455–464
Lebrec D, Sogni P, Vilgrain V (1997) Evaluation of patients with portal hypertension. Clin Gastroenterol 11:221–241
Bosch J, Navasa M, Garcia-Pagan JC, DeLacy AM, Rodes J (1989) Portal hypertension. Med Clin North Am 73:931–953
Burns E, Triger DR, Tucker GT, Bax ND (1991) Indocyanine green elimination in patients with liver disease and in normal subjects. Clin Sci 80:155–160
Gadano A, Hadengue A, Vachiery F, Moreau R, Sogni P, Soupison T et al (1997) Relationship between hepatic blood flow, liver tests, haemodynamic values and clinical characteristics in patients with chronic liver disease. J Gastroenterol Hepatol 12:167–171
Van Giersbergen PL, Wipfli P, Dingemanse J (2003) Determination of tezosentan, a parenteral endothelin receptor antagonist, in human plasma by liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 792:369–373
Dorr MB, Pollack GM (1989) Specific assay for the quantitation of indocyanine green in rat plasma using high-performance liquid chromatography with fluorescence detection. J Pharm Sci 78:328–333
Keiding S, Vilstrup H (2002) Intrahepatic heterogeneity of hepatic venous pressure gradient in human cirrhosis. Scand J Gastroenterol 37:960–964
Valla D, Bercoff E, Menu Y, Bataille C, Lebrec D (1984) Discrepancy between wedged hepatic venous pressure and portal venous pressure after acute propranolol administration in patients with alcoholic cirrhosis. Gastroenterol 86:1400–1403
Dingemanse J, van Giersbergen PLM (2004) Influence of mild liver impairment on the pharmacokinetics of tezosentan, a drug excreted unchanged into bile. Br J Clin Pharmacol 57:344–348
Dingemanse J, Gunawardena KA, van Giersbergen PL (2006) Comparison of the pharmacokinetics, pharmacodynamics and tolerability of tezosentan between Caucasian and Japanese subjects. Br J Clin Pharmacol 61:405–413
Parker JD, Thiessen JJ, Reilly R, Tong JH, Stewart DJ, Pardey AS (1999) Human endothelin-1 clearance kinetics revealed by a radiotracer technique. J Pharmacol Exp Ther 289:261–265
Dupuis J, Steward DJ, Cernacek P, Gosselin G (1996) Human pulmonary circulation is an important site for both clearance and production of endothelin-1. Circulation 94:1578–1584
Burkhardt M, Barton M, Shaw SG (2000) Receptor- and non-receptor-mediated clearance of big-endothelin and endothelin-1: differential effects of acute and chronic ETA receptor blockade. J Hypertension 18:273–279
Meijer DKF, Weert B, Vermeer GA (1988) Pharmacokinetics of biliary excretion in man. VI. Indocyanine green. Eur J Clin Pharmacol 35:295–303
Soons PA, Kroon JM, Breimer DD (1990) Effects of single-dose and short-term oral nifedipine on indocyanine green clearance as assessed by spectrophotometry and high performance liquid chromatography. J Clin Pharmacol 30:693–698
Navasa M, Chesta J, Bosch J, Rodes J (1989) Reduction of portal pressure by isosorbide-5- mononitrate in patients with cirrhosis. Effects on splanchnic and systemic hemodynamics and liver function. Gastroenterology 96:1110–1118
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lebrec, D., Bosch, J., Jalan, R. et al. Hemodynamics and pharmacokinetics of tezosentan, a dual endothelin receptor antagonist, in patients with cirrhosis. Eur J Clin Pharmacol 68, 533–541 (2012). https://doi.org/10.1007/s00228-011-1157-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1157-6