Abstract
Aims
To describe the utilization of antiasthmatic drugs in Sweden and to explore regional variations in drug utilization and adherence to guidelines for rational drug prescribing of antiasthmatics and their rationale.
Methods
Data on antiasthmatic drugs dispensed between July 2005 and December 2008 to all Swedish citizens aged between 18 and 44 years were obtained from the Swedish National Prescribed Drug Register. The period prevalence was determined by analyzing the number of users/1000 inhabitants, and the incidence by analyzing the number of new users after an 18-month drug-free wash-out period. Three drug-related indicators were used to assess the adherence to guidelines. All measures were analyzed by gender and region.
Results
A total of 161,000 patients were dispensed antiasthmatics in 2007, corresponding to a prevalence of 4 and 6% among men and women, respectively; the incidence rates were 2 and 3%, respectively. The total drug utilization and adherence to guidelines varied between regions. The total drug expenditures of antiastmatics were 258 million SEK (28 million euro), with fixed dose combinations accounting for 46% of the expenditure. No relation was found between models for allocating prescribing budgets or clear Drug and Therapeutics Committee recommendations and adherence to guidelines.
Conclusion
There are large regional variations in the utilization of antiasthmatics between Swedish regions, with substantial room for improvement in the adherence to guidelines. New methods of influencing physician behavior may be needed in the future to enhance adherence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Asthma is common in the Western World, with a prevalence of between 5 and 7% among adults in North and West Europe [1]. In Sweden, the prevalence is highest among adolescents (>10%) and lower in middle-aged adults [2]. Effective medicines have been available since the 1970s. Recent guidelines recommend that all patients that need rescue bronchodilation more than twice a week should receive inhaled corticosteroids (ICS) as anti-inflammatory maintenance treatment [2]. In Sweden, the addition of either of two long-acting beta-2-adrenoceptor agonists (LABAs), salmeterol or formoterol, or the leukotriene-receptor antagonist montelukast to the drug therapeutic regimen are recommended for maintenance treatment for patients who fail to reach asthma control with inhaled steroids. Oral corticosteroids and/or the anti-immunoglobulin E compound omalizumab should seldom be used, which is in line with international guidelines [3].
The cost of pharmaceuticals increased significantly in Sweden during the 1990s [4, 5], and this rate of increase was relatively faster than that of other components of the healthcare system. This trend has continued, and in 2006, pharmaceuticals accounted for approximately 11.6% of the total healthcare expenditure [5, 6]. Expenditure is expected to continue growing at approximately 4% annually during the upcoming years [6, 7]. Prescribed drugs represent 74% of the total expenditure for pharmaceuticals in Sweden [6], and antiasthmatics (ATC group R03) represented 5% of the total expenditure for drugs in 2007 (National Corporation of Swedish Pharmacies, Apoteket AB, personal communication), with the cost of the fixed combination of formoterol and budesonide (R03AK07) being on the top ten list of drug expenditures with recent significant increases in expenditure: 9% between 2006 and 2007 [6]. Consequently, drug utilization studies and subsequent interventions to promote best practice are important from a patient, societal, and health-economic point of view.
A number of studies have explored the prescribing of antiasthmatic drugs in Sweden [8–11]. Some studies have focused on equity, safety, and regional variation [12–14], but most are old studies that included only small populations, did not focus on asthma, dealt with children only, and/or were concerned with acute rather than chronic care. Consequently, they are not relevant to any modern analysis of the utilization of antiasthmatic drugs in Sweden.
The establishment of the Swedish National Prescribed Drug Register in 2005 has created new opportunities for studies on the rational prescribing of antiasthmatic drugs [15]. This register includes all drugs dispensed to the entire Swedish population. Each year approximately 90 million prescriptions are recorded for 6 million individuals (two thirds of the Swedish population use prescription drugs). As a result, this register represents one of the largest population-based pharmacoepidemiological databases in the world.
In a previous study, we observed large differences in the utilization of and expenditures for asthma medications between patients attending different primary healthcare centers in the Stockholm area [16]. These differences could only to a small extent be attributed to differences in asthma severity between the patients. Therefore, we wanted to extend the scope of the original study to assess and analyze regional differences in the use of antiasthmatic drugs. In addition, all Swedish regions have their own Drug and Therapeutics Committees (DTCs) [17, 18].
These DTCs use a variety of methods to promote rational prescribing, including the development and dissemination of guideline(s), continuous professional education, and feedback on prescribing patterns [18, 19]. In addition, each region applies a different model for budget devolution to prescribing doctors in an attempt to influence prescribing behavior. The impact of the activities of these DTCs and of the different economic incentives have not been extensively studied.
The aims of the study reported here were, therefore, to describe the utilization of antiasthmatic drugs in Sweden as well as explore regional variations in drug utilization and adherence to guidelines for rational drug prescribing behavior in the treatment of asthma in relation to, for example, models for budget devolution. Adherence to guidelines for asthma treatment is an important issue for patient safety and quality of care. Poor adherence may also have negative economic consequences for the healthcare system.
Material and methods
Study design
This is an observational registry study that includes all Swedish citizens aged 18–44 years who redeemed prescriptions of antiasthmatic drugs (ATC group R03) between July 2005 and December 2008. Data were extracted from the National Prescribed Drug register (see below). Since antiasthmatic drugs are also used for the treatment of chronic obstructive pulmonary disease (COPD), and the register does not include diagnoses, we chose to study only patients under the age of 45 years. The objective was to minimize confounding drug treatment for COPD since COPD is usually seen in older patients. All analyses were performed by gender and region, and the data were anonymous. All counties (regions) have at least one DTC, and currently in Sweden there are 21 such counties, varying in size between 60,000 and approximately 2 million inhabitants (Table 1). Each county has its own political administrative body and is able to levy taxes and implement decisions on healthcare organization and patient co-payment for healthcare consultations. The counties are also responsible for the drug budget across sectors although they receive subsidies [20, 28].
Data were also extracted from the regional database for electronic prescriptions within Stockholm County Council. This database contains all electronically transferred prescriptions from healthcare providers in the region to the pharmacies, regardless if the prescription has been redeemed or not. In 2007, the database covered more than 90% of all prescriptions issued in the region. Data from this database on prescribed drugs were compared with data on dispensed drugs from the National Prescribed Drug Register to assess whether the lack of dispensing of ICSs to patients treated with a LABA could be explained by patient behavior or by the doctors’ prescribing patterns.
The Swedish National Prescribed Drug Register
The Swedish National Prescribed Drug Register was established in July 2005 and is regulated by legislation issued by the Swedish government [21]. It contains data on dispensed prescriptions in ambulatory care for the entire Swedish population (99.7% population coverage with patient identities). Stored details include dispensed items and amounts, dates of prescribing and dispensing, age, sex and place of residence of the patient, the prescribers’ profession and practice, and the unique patient identifier (personal identification number) of each patient. All pharmaceuticals in the register are classified according to the Anatomical Therapeutic Chemical classification system (ATC), and defined daily doses (DDD) are included as a measurement of the volume dispensed [22]. The register is managed by the National Board of Health and Welfare (for more information, refer to www.sos.se). Over-the-counter (OTC) medications and drugs used at in-patients settings are not included.
Definitions of variables and analysis
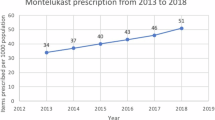
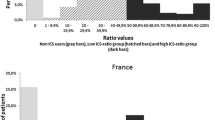
All drugs were classified according to the ATC classification system [23]. The period prevalence was assessed as the proportion of subjects in the Swedish population for whom antiasthmatic drugs were dispensed during the study period, and is expressed as number of users per 1000 inhabitants (patients/1000 inhabitants, PAT/TIN) [24]. The incidence of new users was assessed using the waiting time distribution methodology, identifying first time users of antiasthmatics after a drug free run-in period [25]. In this study, we analyzed drugs dispensed each month from July 2005 and used an 18 month wash-out-period to define new users in order to determine the incidence. The length of this period was selected to exclude prevalent users and to avoid misinterpretation due to seasonal variation (Fig. 1). Lorentz percentiles and Lorentz curves were used to evaluate the skewness of the use of antiasthmatics [25]. The Lorenz curve is a plot with the proportion of subjects purchasing drugs on the x-axis and the proportion of the total volume in DDD on the y-axis. We analyzed the Lorenz 10th and 50th percentiles, i.e. the proportions of the purchased volumes accounted for by the top 10% of users and half of all users, respectively.
a Purchased drugs in the Anatomical Therapeutic Chemical classification system (ATC) group R03 for patients aged 18–44 years from January 2006 until December 2008. Each bar represents first time users. At the beginning of the period, all users purchasing their medicines are classified as “new” users. b Purchased drugs in the ATC groups R03AC (filled diamond), R03AK (filled square), and R03BA (filled triangle) for patients aged 18–44 years from January 2006 until December 2008. Each bar represents first time users. In the beginning of the period, all users purchasing their medicines are classified as “new” users
Regression variables at the regional level
To explore and explain the regional differences in drug utilization observed, we assessed the variation in prevalence, incidence, and chosen indicators for rational drug use in relation to four independent variables: (1) prescribing budget and incentives; (2) the extent of the DTC guidelines; (3) the number of general practitioners (GPs) per inhabitant in the region; (4) the number of pulmonary physicians per inhabitant in the region.
Prescribing budgets and incentives
Most counties have allocated indicative budgets for prescribed ambulatory care drugs [26, 27, 34, 35] to enhance the cost consciousness of physicians following budget devolution to the counties. While some counties still apply a central drug budget, others have decentralized the cost-responsibility to the clinic or primary health care centers (PHCC) of the prescribing physicians. Three models for budget devolution have been used [26, 27]:
-
1.
A population-based model with an age-standardized budget for the population listed in each practice. In this model, the PHCCs are responsible for the costs of non-specialist drugs (accounting for 50–80% of overall costs) for the patients listed, and hospital clinics are responsible for the costs of specialist drugs prescribed by themselves.
-
2.
A prescriber-based model with a budget for each clinic/PHCC that is based on its previous prescribing pattern.
-
3.
A central system in which the budget for pharmaceuticals is handled at the regional level.
Model 1 is more common in rural areas, whereas model 2 is more common in major cities.
Access to healthcare professionals
The following data on access to physicians in year 2006 were collected from each region (Table 1):
-
The number of GPs employed in health care per thousand inhabitants in the region.
-
The number of pulmonary physicians employed in health care per thousand inhabitants in the region.
Drug and Therapeutics Committee guidelines for asthma
In Sweden, most DTC guidelines consist of disease-specific recommendations for the use of drugs based on medical efficacy and safety, pharmaceutical suitability, comparative cost effectiveness, experience, and environmental aspects [18, 19]. Recommendations may vary between regions. We studied the impact of DTC guidelines for the initiation of asthma therapy. No region had guidelines that deviated from national guidelines.
Consequently, we recorded a binary variable—presence or absence of clearly stated recommendations in accordance with national guidelines. Twelve of the regions had a clear recommendation stating that the use of antiasthmatics should be stepped up and that fixed combinations should only be prescribed to patients needing a combination of a LABA and ICS to gain asthma control (Table 1).
Quality indicators for asthma treatment
We used the following indicators to assess the adherence to guidelines for rational prescribing of antiasthmatics [2, 3]:
-
The proportion of patients initiated on fixed combinations of LABA and ICS (R03AK) with no prior purchase of antiasthmatics (R03) during the preceding 18 months.
-
The proportion of patients purchasing LABA (R03AC12, R03AC13) who had not dispensed any ICS (R03BA and/or R03AK) concomitantly. According to current guidelines, patients with asthma should not be prescribed a LABA without concomitant anti-inflammatory treatment with an ICS [2].
-
The proportion of patients purchasing antiasthmatic drugs who were also dispensed selective (C07AB, C07FB) and non-selective beta-blocking agents (C07AA, C07AG). Prescribing of non-selective beta-blocking agents to patients with asthma has previously been used as a measure of quality, with low prescribing reflecting high quality [28–30].
Cost and reimbursement
The Pharmaceutical Benefit Scheme, which is mainly tax financed, covers the main costs for drugs in ambulatory care in Sweden. The patient pays the full price for subsidized pharmaceuticals included in the scheme up to a certain level, and then different reductions are obtained for the additional cost. There is a uniform national ceiling on the total amount that a patient pays during a 12-month period (out-of-pocket ceiling) for subsidized pharmaceuticals (SEK 1800, EURO € 195 during a 12-month period). No fixed co-payments or prescription fees are used within the Swedish reimbursement system.
Data on total costs, including patient co-payment, for drugs were obtained from the Swedish National Prescribed Drug Register. These are based on the price list of the National Corporation of Swedish Pharmacies (Apoteket AB) 2007. For purposes of international comparison, 1 EURO (€) = 9.25 SEK (2007)
Statistics
Drug utilization and expenditures were based on the complete dataset for the whole population in Sweden during the period. Microsoft Excel version 2003, SYSTAT II ver. 2004 (SYSTAT Software, Richmond, CA) and SAS ver. 9, 1.3 SP 3, 2004 (SAS Institute, Cary, NC) were used for data handling and statistical analyses. Correlation was calculated using Pearson correlation coefficients. Regression analysis of the incidence and prevalence of asthma in the register data was performed in order to detect regional differences between counties. We performed a stepwise forward linear regression with ordinary least squares (OLS) estimation. To ensure that there was no multicolinearity we also checked the tolerance.
Ethics
The study was approved by the Regional Ethical Review Board in Stockholm, Sweden (2007/1138-31).
Results
Incidence and prevalence of antiasthmatic treatment
In 2007, a total of 161,000 patients aged 18–44 years were dispensed approximately 500 thousand prescriptions for drugs for asthma (Table 2). The incidence of new patients was 2 and 3% among men and women, respectively.
The number of “new” unique patients being dispensed drugs for asthma each month is illustrated in Fig. 1. In the first month of the study, January 2006, all patients purchasing drugs were counted as “new”, and the incidence was determined after a certain drug-free wash-out period. Each year, a peak of new users was observed during the period April–May.
The period prevalence was 4% among men and 6% among women. The prevalence was higher in women than men for the beta-agonists, ICS, and fixed combinations of a LABA and ICS, respectively. Approximately 3.7% of the population were dispensed beta-2-agonists (R03AC), but the majority of these (90%) were only dispensed short-acting beta-2-agonists (SABAs). The use of beta-2-agonists was skewed in the study population, as 10% of the patients accounted for more than half (52%) of the dispensed volume in defined daily doses (DDD). A majority of the patients (about 70–80%) who were dispensed large amounts of beta-2-agonists were also dispensed at least one prescription with an ICS during the period.
For the fixed combinations (R03AK), the period prevalence was about 1.3%, with 10% of patients accounting for 29% of the volume. For ICS (R03BA), the period prevalence was approximately 2%, with 10% of the patients accounting for 42% of the volume.
Expenditures
The total expenditure for antiasthmatics (R03) in 2007 for patients aged 18–44 years was 258 million SEK (28€). Beta-2-agonists (R03AC) accounted for 22% of the total, fixed combinations (R03AK) for 46%, and ICSs (R03BA) for 23%. The total drug cost per patient was SEK 1598 for all drugs for asthma (R03) and SEK 468 (€51), 2781 (€301), and 921 (€100) for beta-2-agonists, fixed combinations, and ICSs, respectively. Individuals 18–44 years of age accounted for 16% of the total costs for dispensed antiasthmatics, while those over 45 years of age accounted for 75% and children <18 years for approximately 9% of the total expenditures. On average, in 2007, each patient filled prescriptions three times. In Sweden, the average prescription is for a 3-month supply.
Regional variations and adherence to national guidelines
The prevalence of dispensing drugs for asthma varied considerably between counties, from 41.3 PAT/TIN on the island of Gotland to 67.9 in Norrbotten, the northernmost and most scarcely populated region (Fig. 2). The Lorenz 50th percentile, i.e., the proportion of DDDs accounted for by the half of the population with highest utilization, varied from 74 to 92%.
A significant positive correlation (adjusted 2R = 0.329) was found between the number of GPs per inhabitant and the utilization of fixed combinations (R03AK). The three other independent variables, i.e., devolution of prescribing budgets and incentives, clearly stated county DTC guidelines, and number of pulmonary physicians per inhabitant, did not significantly influence variations observed for any of the drugs prescribed for asthma.
Between 1.1 and 2.3% of patients who were dispensed at least two antiasthmatic prescriptions were dispensed beta-1-selective antagonists alone (C07AB) or as fixed combinations with other antihypertensives (C07FB) (Fig. 3). However, 0.6 and 1.7% of all patients who were dispensed at least two prescriptions for antiasthmatic drugs (R03) were also dispensed non-selective beta-adrenoceptor antagonists alone (C07AA) or in combination with alpha- and beta-adrenoceptor antagonists (C07AG). There were obvious differences between regions.
Between 33 and 58% of the patients initiated on fixed combinations of antiasthmatic drugs (R03AK) had not been dispensed any other antiasthmatic drug during the 18 months preceding the study period (Fig. 4). This parameter showed large regional variations.
Between 18 and 37% of all patients who had been dispensed prescriptions for a LABA (formoterol or salmeterol) in 2007 had not been dispensed any ICS during the same period (Fig. 5) In Stockholm, 23% of the patients were dispensed a LABA without being dispensed a ICS during the same period (Fig. 5). During 2007, 2245 of 2956 patients receiving electronic prescriptions for a LABA also received prescriptions for ICS. Consequently, 24% of patients were prescribed a LABA without a concomitant ICS, which reflects poor adherence to guidelines among primary care physicians in the county.
None of the quality indicators studied (Figs. 3, 4 and 5) were found to be influenced by County Council models for prescribing budget and incentives (data not shown). Nor was any correlation observed between using a LABA and an ICS without having tried an ICS previously, emphasizing the guidelines (Fig. 4) and compliance with the recommendation not to use LABA without concomitant ICS (Pearson r = 0.12).
Discussion
This study describes the utilization of antiasthmatic drugs in Sweden and explores the regional variations in utilization and adherence to guidelines for rational drug prescribing. Large differences were found between healthcare regions in terms of the prevalence and incidence of antiasthmatic drug use. In addition, the adherence to national and regional guidelines with patient safety implications was found to be poor.
The relatively high values for incidence compared to those for period prevalence indicate a high proportion of episodic users of antiasthmatic drugs, which is not surprising since asthma is a variable disease. The waiting-time distribution showed a significant peak in incidence for all antiasthmatic drugs during April–May each year (Fig. 1), which coincides with the pollen season (e.g., high birch-pollen counts) in Sweden. The pollen season was more intense than usual in 2006 [31], and this is reflected by a higher quantity of dispensed asthma drugs in our dataset for spring 2006 than in that for spring 2007.
The majority of patients (59%) were women, in accordance with previous data [32–34] and the fact that female patients with asthma seek care more often than males [35, 36]. Adult women also tend to have more severe asthma than adult men [37]. Consequently, our findings were expected.
There was a striking skewness in the dispensing of prescriptions for inhaled beta-2-agonists, as 10% of the patients accounted for 52% of the volume in DDDs. We suspected this potential overconsumption may be related to insufficient use of anti-inflammatory treatments with an ICS. However, this did not seem to be the case, since most of these patients were also dispensed prescriptions for ICSs. We did, however, not analyze the prescribed doses of ICSs, nor did we analyze the number of prescriptions dispensed. It would be interesting to further characterize this group of individuals in order to explain their bronchodilator treatment pattern [38]. An earlier study showed that overuse of inhaled beta-2-agonists is associated with symptom severity, problems in obtaining asthma medication, and male sex [39]. However, such an analysis would require an analysis of patient identifiable data, which was beyond the scope of this study.
Regional variations and adherence to national guidelines
Overall, there were marked regional variations in the rate of drugs prescribed/dispensed for asthma (Fig. 2). The higher prevalence in northern Sweden (e.g., Norrbotten) reflects the higher prevalence of asthma there [34]. A close conformity has indeed been observed between prevalence of asthma and the prescribing of drugs for asthma [40, 41].
It is of interest that the substudy on electronic prescriptions in the Stockholm area showed that use of a LABA without an ICS was due to the failure of doctors to prescribe an ICS rather than the failure of the patients to have their prescriptions dispensed—i.e., to poor doctors’ adherence to guidelines. This pattern of prescribing puts the patient at risk since the safety of LABA treatments has recently been questioned [42, 43], and patients with asthma should not be treated with a LABA without concomitant treatment with a ICS [44].
The regional differences in adherence to guidelines are difficult to explain since the guidelines are national and similar in all regions. Surprisingly, a clear statement that national guidelines recommend ICS before the addition of LABA to the treatment regimen [2, 3], which was distributed with the recommended formulary from the regional DTCs, failed to influence the regional prescribing behavior. Between 33 and 58% of the patients in different regions had a treatment initiated with fixed combinations of an ICS and a LABA without prior utilization of other antiasthmatics. It has been shown that corticosteroid-naïve asthmatics generally do not obtain any increased benefit from the addition of LABA in combination with ICS than from corticosteroids alone [45]. In addition, there are also resource consequences. Consequently, a properly selected target population for combined treatment is only obtained by stepping up treatment and adding a LABA to patients whose disease fails to be controlled by an ICS rather than by initiating treatment with both a LABA and an ICS in corticosteroid-naïve patients. Failure to increase therapy stepwise may also result in inappropriate pharmaceutical costs. A fixed combination with R03 AK treatment is expensive and represents 46% of the total cost for antiasthmatic drugs.
The same pattern was seen both in dispensed prescriptions from the different regions and in the electronic prescriptions sent from physicians in the Stockholm region, indicating that the discrepancy could not be attributed to patients’ primary non-compliance.
The poor compliance with asthma guidelines in this study is disappointing. As early as in 1999, the European Respiratory Society (ERS) together with European Academy of Allergy and Clinical Immunology (EAACI) and GINA addressed these issues with the aim of obtaining effective strategies to better disseminate and implement guidelines [46]. The reasons for poor guideline adherence are generally multiple [47]. A number of different factors that influence GPs' prescribing patterns have been previously described [46, 48, 49]. Therefore, what can be done to improve adherence and subsequent patient care? Several methods have been shown to help enhance rational prescribing, centering on the four Es: education, engineering, economics, and enforcement [15]. This approach includes providing information and continuous medical education in combination with feedback on prescribing patterns. Such activities are often initiated by DTCs and have been shown to impact more on prescribing patterns when they are local and built on personal relations [50]. In addition, a combination of activities enhances the chances of success [15, 49, 51]. Taylor et al. showed that it is important that the patients have received adequate information on their asthma disease, drug regimens, and inhaler technique [51]. It may be in this situation that activities need to be targeted at both patients and physicians to encourage the prescribing on an ICS first before a LABA, especially if there are continued fears about steroid use. This approach builds on successful public campaigns aimed at enhancing physicians' adherence to the Wise Drug List guidance in Stockholm County [15]. The main messages for both the physician and patient within the context of such educational efforts can be concerns with patient safety and the need for rational prescribing. Optimizing cost-effectiveness can also be a key message to physicians, especially as resource pressures grow [52]. Incentive schemes asking physicians to discuss future initiatives to enhance ICS prescribing before a LABA could also be a possibility and builds on current initiatives in Stockholm County [15].
The regression analysis showed that the number of GPs per inhabitant in the regions influenced drug utilization, whereas the access to pulmonary physicians did not. This is perhaps not surprising since it is known that a higher number of GPs leads to the increased prescribing of drugs for asthma. In the USA, the increase in the number of practicing physicians has been described to theoretically predict 86% of the variability in the rise of pharmaceutical expenditures [53]. Supplier-induced demand (SID) is a recognized phenomenon in health economics and refers to the amount of demand created by doctors, which exists beyond what would have occurred in a market in which consumers are fully informed. The lack of knowledge among patients could also lead to a demand from patients to prescribe drugs [54, 55].
However, many studies have shown that guidelines are slowly implemented in healthcare systems [4] and that there is substantial room for improvement with respect to the prescribing doctors’ adherence to guidelines [56–59] as well as patient compliance [60–62].
Strengths and limitations
This study is based on data contained in the Swedish Prescribed Drug Register, which is one of the largest population-based databases on dispensed drugs in the world. We used patient identity drug dispensing data to determine the incidence and prevalence of antiasthmatic drug treatment. It is important to emphasize that dispensing is not the same as prescribing. Nor is it the same as consumption. The relationship between prescribed, dispensed, and consumed drugs has been examined in many studies [11, 63]. Patient primary noncompliance (failure to fill the prescription) provides food for thought when analyzing the behavior of doctors and patients. We could, however, only analyze this issue in one large region, which has a widespread use of electronic prescriptions. This analysis suggests that the problem is mainly poor adherence to guidelines by the doctors, although poor adherence to prescribed and dispensed treatment may still occur at the patient level. Previous studies have shown that longitudinal data on purchases of pharmaceuticals may contribute to the evaluation of patient compliance [11, 15, 60], but patient compliance with dispensed medications was beyond the scope of the present investigation.
One limitation of our study was the lack of diagnoses and indications for the dispensed medicines. Limiting the age range to 18–44 years probably excluded most COPD patients, but it also excluded information on asthma treatment in children and adolescents as well as that on patients older than 44 years. The volume of asthma/COPD drugs per patient increases with age and is about 2.5-fold higher for patients aged 60–69 years than for those aged 20–29 years [41]. The restriction of the study to adults would also eliminate confounding by other obstructive airways diseases restricted to children.
The register had only existed in its present form for 18 months before our study period. This means that, theoretically, patients can have a built-up stock of some medications at home and thus can use pharmaceuticals which were not dispensed during the study period, thus making adherence to guidelines appear smaller than it actually is. However, since our reimbursement system and other factors that can affect patients’ tendencies to keep a large stock of medicines are national, this should not affect the regional variations.
Conclusions
The large regional variation in the use of antiasthmatic drugs observed in this study cannot be easily explained. More importantly, adherence to asthma guidelines was suboptimal with respect to aspects directly related to patient safety and not related to efforts from regional drug and therapeutics committees to promote the recommended guidelines. Furthermore, financial incentive schemes appeared to have a limited impact. This may be due to a variety of reasons, including physician concerns with adherence if more than one inhaler is used as well as patient concerns with ICS safety. New approaches need to be undertaken and researched to determine how to build upon approaches that have been successful in other disease areas and in other countries. In order to enhance the effects of our efforts, we also need more knowledge about factors affecting the adherence of physicians and patients to guidelines.
Abbreviations
- R03:
-
Respiratory system
- R03A:
-
Adrenergics inhalants
- R03AC:
-
Selective beta-2-adrenoreceptor agonists
- R03AK:
-
Adrenergics and other drugs for obstructive airway diseases, combinations
- R03BA:
-
Glucocorticoids
- LABA:
-
Long-acting beta-2-adrenoceptor agonist
- SABA:
-
Short-acting beta-2-agonists
References
Burney PG, Luczynska C, Chinn S, Jarvis D (1994) The European community respiratory health survey. Eur Respir J 7(5):954–960
Läkemedelsverket Medical Products Agency (2007) Farmakologisk behandling vid astma–2007. Tryckt version. 2007(18) Temanummer
Bousquet J, Clark TJ, Hurd S, Khaltaev N, Lenfant C, O'Byrne P et al (2007) GINA guidelines on asthma and beyond. Allergy 62(2):102–112
Henriksson F, Hjortsberg C, Rehnberg C (1999) Pharmaceutical expenditure in Sweden. Health Policy 47(2):125–144
Moise P, Docteur E (2007) OECD Health Working Papers No. 28. Pharmaceutical pricing and reimbursement in Sweden:13 September 2007. Available at: htttp://www.olis.oecd.org/olis/2007doc.nsf/FREDATCORPLOOK/NT00002E52/$ FILE/JTO3231887.PDF (assessed 2 Feb 2008)
Socialstyrelsen (2008) Läkemedelsförsäljningen I Sverige—analys och prognos. Stockholm
Socialstyrelsen (2007) Läkemedelsförsäljningen I Sverige—analys och prognos (September 2007). Stockholm
Brodin H (1987) Regional variations in pharmaceutical consumption in Sweden. Linköping University, Linköping
Gerdtham UG, Hertzman P, Jonsson B, Boman G (1996) Impact of inhaled corticosteroids on acute asthma hospitalization in Sweden 1978 to 1991. Med Care 34(12):1188–1198
Haupt D, Krigsman K, Nilsson JL (2008) Medication persistence among patients with asthma/COPD drugs. Pharm World Sci 30(5):509–514
Krigsman K, Moen J, Nilsson JL, Ring L (2007) Refill adherence by the elderly for asthma/chronic obstructive pulmonary disease drugs dispensed over a 10-year period. J Clin Pharm Ther 32(6):603–611
Eckerlund I, Gerdtham UG (1998) Econometric analysis of variation in cesarean section rates. A cross-sectional study of 59 obstetrical departments in Sweden. Int J Technol Assess Health Care 14(4):774–787
Gillissen A (2007) Patients' adherence in asthma. J Physiol Pharmacol 58[Suppl 5]:205–222
Hartz I, Sakshaug S, Furu K, Engeland A, Eggen AE, Njolstad I et al (2007) Aspects of statin prescribing in Norwegian counties with high, average and low statin consumption—an individual-level prescription database study. BMC Clin Pharmacol 7:14
Wettermark B, Hammar N, MichaelFored C, Leimanis A, Otterblad Olausson P, Bergman U et al (2007) The new Swedish prescribed drug register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16(7):726–735
Arnlind MH, Nokela M, Rehnberg C, Jonsson EW (2006) The relationship between pharmaceutical costs, disease severity, and health-related quality of life in asthmatics in Swedish primary care. J Asthma 43(8):585–591
Sjöqvist F, Bergman U, Dahl ML (2002) eaDatcaSeWDI. Drug and therapeutics committees: a Swedish experience. WHO Drug Inf 16:207–213
Wettermark B, Godman B, Andersson K, Gustafsson LL, Haycox A, Bertele V (2008) Recent national and regional drug reforms in Sweden: implications for pharmaceutical companies in Europe. Pharmacoeconomics 26(7):537–550
Godman B, Wettermark B, Hoffmann M, Andersson K, Haycox A, Gustafsson LL (2009) Swedish experience in ambulatory care with multifaceted national and regional drug reforms and initiatives: global relevance. Expert Review. Pharmacoeconomics Outcomes Res 9(1):65–83
Anell A (2005) Swedish healthcare under pressure. Health Econ 14[Suppl 1]:S237–S254
Socialdepartementet (2005) Socialdepartementet förordning (2005:363) om läkemedelsregister hos Socialstyrelsen. Stockholm
World Health Organization (2005) Guidelines for ATC classification an DDD assignment. WHO Collaborating Centre for Drug Statistics Methodology. Available at: www.whocc.no. WHO, Oslo
World Health Organization (2007) Guidelines for ATC classification and DDD assignment. WHO Collaborationg Center for Drug Statistics Methodology 2007: Available at: http://www.whocc.no/
World Health Organization (2003) Introduction to drug utilisation research, NLM classification WB 330. WHO, Oslo
Hallas J, Stovring H (2006) Templates for analysis of individual-level prescription data. Basic Clin Pharmacol Toxicol 98(3):260–265
Bergstrom G, Karlberg I (2007) Decentralized responsibility for costs of outpatient prescription pharmaceuticals in Sweden. Assessment of models for decentralized financing of subsidies from a management perspective. Health Policy 81(2-3):358–367
Jansson S, Anell A (2006) The impact of decentralised drug-budgets in Sweden—a survey of physicians' attitudes towards costs and cost-effectiveness. Health Policy 76(3):299–311
Haaijer-Ruskamp F, HHoven J, Mol P (2004) A conceptual framework for constructing prescribing quality indicators: a poroposal. DURQUIM: Drug Utilization Quality Indicator Meeting. WHO, Mechelen
Hoven JL, Haaijer-Ruskamp FM, Vander Stichele RH (2005) Indicators of prescribing quality in drug utilisation research: report of a European meeting (DURQUIM, 13–15 May 2004). Eur J Clin Pharmacol 60(11):831–834
Socialstyrelsen (2003) Indikatorer för utvärdering av kvaliteten I äldres läkemedelsterapi—socialstyrelsens förslag. Stockholm
Naturhistoriska riksmuseet (2007) Årets pollensäsong—nu börjar det! Available at: htwww.nrm.se/sv/menss/pressmeddelandessmeddelanden/200t spollensasongnuborjardet.1374.html
Ehrs PO, Nokela M, Stallberg B, Hjemdahl P, Wikstrom Jonsson E (2006) Brief questionnaires for patient-reported outcomes in asthma: validation and usefulness in a primary care setting. Chest 129(4):925–932
Kamble S, Bharmal M (2009) Incremental direct expenditure of treating asthma in the United States. J Asthma 46(1):73–80
Läkemedelsverket (2002) Bakgrukumentation—akologisk ndling av astma (database on the Internet). Available at: http://www.lakemedelsverket.se/upload/Hälso-%20och%20sjukvård/behandlingsrek/bakg_dok/astma_bakgrund.pdf
Osborne ML, Vollmer WM, Linton KL, Buist AS (1998) Characteristics of patients with asthma within a large HMO: a comparison by age and gender. Am J Respir Crit Care Med 157(1):123–128
Weiner P, Magadle R, Massarwa F, Beckerman M, Berar-Yanay N (2002) Influence of gender and inspiratory muscle training on the perception of dyspnea in patients with asthma. Chest 122(1):197–201
Abraham B, Antó JM, Barreiro E, Bel EHD, Bousquet J, Castellsagud J, et al (2003) The ENFUMOSA cross-sectional European multicentre study of the clinical phenotype of chronic severe asthma. European Network for Understanding Mechanisms of Severe Asthma. Eur Respir J 22(3):470–477
Diette GB, Wu AW, Skinner EA, Markson L, Clark RD, McDonald RC et al (1999) Treatment patterns among adult patients with asthma: factors associated with overuse of inhaled beta-agonists and underuse of inhaled corticosteroids. Arch Intern Med 159(22):2697–2704
Cockcroft DW, Davis BE (2006) Airway hyperresponsiveness as a determinant of the early asthmatic response to inhaled allergen. J Asthma 43(3):175–178
Hasselgren M, Arne M, Lindahl A, Janson S, Lundback B (2001) Estimated prevalences of respiratory symptoms, asthma and chronic obstructive pulmonary disease related to detection rate in primary health care. Scand J Prim Health Care 19(1):54–57
Nilsson JLG, Haupt D, Krigsman K, Moen J (2009) Asthma/COPD drugs reflecting disease prevalence, patient adherence and persistence. Expert Review (serial on the Internet)
Beasley R, Martinez FD, Hackshaw A, Rabe KF, Sterk PJ, Djukanovic R (2009) Safety of long-acting beta-agonists: urgent need to clear the air remains. Eur Respir J 33(1):3–5
Cates CJ, Cates MJ, Lasserson TJ (2008) Regular treatment with formoterol for chronic asthma: serious adverse events. Cochrane Database Syst Rev 4:CD006923
GINA Guidelines. (2008) Pocket guide for asthma management and prevention 2008: Available at: http://www.ginasthma.com/Guidelineitem.asp??l1=2&l2=1&intId=1562
Ni CM, Greenstone IR, Ducharme FM (2005) Addition of inhaled long-acting beta2- agonists to inhaled steroids as first line therapy for persistent asthma in steroid- naive adults. Cochrane Database Syst Rev 2:CD005307
Partridge MR, Fabbri LM, Chung KF (2000) Delivering effective asthma care—how do we implement asthma guidelines? Eur Respir J 15(2):235–237
Wiener-Ogilvie S, Huby G, Pinnock H, Gillies J, Sheikh A (2008) Practice organisational characteristics can impact on compliance with the BTS/SIGN asthma guideline: qualitative comparative case study in primary care. BMC Fam Pract 9:32
Eccles MP, Soutter J, Bateman DN, Campbell M, Smith JM (1996) Influences on prescribing in non-fundholding general practices. Br J Gen Pract 46(406):287–290
Mansouri M, Lockyer J (2007) A meta-analysis of continuing medical education effectiveness. J Contin Educ Health Prof 27(1):6–15
Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA (1998) Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. Br Med J 317(7156):465–468
Taylor DM, Auble TE, Calhoun WJ, Mosesso VN Jr (1999) Current outpatient management of asthma shows poor compliance with International Consensus Guidelines. Chest 116(6):1638–1645
Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L et al (2004) Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 8(6):1–72
Brown MM, Brown GC, Sharma S, Hollands H, Smith AF (2001) Physician manpower and health care expenditures in the United States: a thirty-year perspective. J Health Care Finance 27(4):55–64
Folland S, Goodman A, Stano M (eds) (2004) The ecoonomics of health and health care. Pearson Prentice Hall, Upper Saddle River
Leonard C, Stordeur S, Roberfroid D (2009) Association between physician density and health care consumption: A systematic review of the evidence. Health Policy 91:121–34
Grol R, Grimshaw J (2003) From best evidence to best practice: effective implementation of change in patients' care. Lancet 362(9391):1225–1230
Grol R, Wensing M (2004) What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust 180[Suppl]:S57–S60
Wettermark B, Haglund K, Gustafsson LL, Persson PM, Bergman U (2005) A study of adherence to drug recommendations by providing feedback of outpatient prescribing patterns to hospital specialists. Pharmacoepidemiol Drug Saf 14(8):579–588
Wisnivesky JP, Lorenzo J, Lyn-Cook R, Newman T, Aponte A, Kiefer E et al (2008) Barriers to adherence to asthma management guidelines among inner-city primary care providers. Ann Allergy Asthma Immunol 101(3):264–270
Cochrane GM, Horne R, Chanez P (1999) Compliance in asthma. Respir Med 93(11):763–769
Lindberg M, Ekstrom T, Moller M, Ahlner J (2001) Asthma care and factors affecting medication compliance: the patient's point of view. Int J Qual Health Care 13(5):375–383
Stallberg B, Nystrom Kronander U, Olsson P, Gottberg L, Ronmark E, Lundback B (2003) Living with asthma in Sweden–the ALMA study. Respir Med 97(7):835–843
Krigsman K, Melander A, Carlsten A, Ekedahl A, Nilsson JL (2007) Refill non-adherence to repeat prescriptions leads to treatment gaps or to high extra costs. Pharm World Sci 29(1):19–24
Acknowledgements
The authors are grateful to Andrejs Leimanis, EpC, The National Board of Health and Welfare, and Anders Hansson and Bengt Sjöborg, Department of Drug Management and Informatics, Stockholm County Council, for their invaluable contributions with the data extractions. We also acknowledge Brian Godman for valuable comments on this manuscript. The study was supported by the Centre for Allergy Research at Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arnlind, M.H., Wettermark, B., Nokela, M. et al. Regional variation and adherence to guidelines for drug treatment of asthma. Eur J Clin Pharmacol 66, 187–198 (2010). https://doi.org/10.1007/s00228-009-0731-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0731-7