Abstract
Purpose
A considerable weakness of current clinical decision support systems managing drug–drug interactions (DDI) is the high incidence of inappropriate alerts. Because DDI-induced, dose-dependent adverse events can be prevented by dosage adjustment, corresponding DDI alerts should only be issued if dosages exceed safe limits. We have designed a logical framework for a DDI alert-system that considers prescribed dosage and retrospectively evaluates the impact on the frequency of statin–drug interaction alerts.
Methods
Upper statin dose limits were extracted from the drug label (SPC) (20 statin-drug combinations) or clinical trials specifying the extent of the pharmacokinetic interaction (43 statin–drug combinations). We retrospectively assessed electronic DDI alerts and compared the number of standard alerts to alerts that took dosage into account.
Results
From among 2457 electronic prescriptions, we identified 73 high-risk statin–drug pairs. Of these, SPC dosage information classified 19 warnings as inappropriate. Data from pharmacokinetic trials took quantitative dosage information more often into consideration and classified 40 warnings as inappropriate. This is a significant reduction in the number of alerts by 55% compared to SPC-based information (26%; p < 0.001).
Conclusion
This retrospective study of pharmacokinetic statin interactions demonstrates that more than half of the DDI alerts that presented in a clinical decision support system were inappropriate if DDI-specific upper dose limits are not considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical decision support (CDS) systems have been developed to safeguard physicians’ actions in a myriad of clinical situations, including the prescription of combination therapy and, consequently, the prevention of drug–drug interactions (DDI) [1]. The identification of DDI is a relevant task for CDS systems because of the shear number of combinations confronting physicians when prescribing more than one drug to a patient. For example, the co-administration of ten drugs will result in 45 drug pairs, all of which have to be scrutinized for potential adverse DDI. Current CDS systems have a number of inherent weaknesses, of which the most important are questionable clinical relevance and the low specificity of presented alerts, which result in a low acceptance by users in routine practice [2]. The presentation of DDI alerts classified by severity has recently been shown to improve user adherence [3]. In order to further enhance the specificity of alerts, we developed a strategy to hold back inappropriate pharmacokinetic DDI alerts in an attempt to personalize alerts more comprehensively to the actual patient situation.
The DDI may alter drug concentration (pharmacokinetic DDI) and thus the exposure of the patient to a drug by orders of magnitude [4]. Because both the safety and the effectiveness of a drug are concentration-dependent, DDI are a major modulator of treatment response, leading to nonresponse or (sometimes fatal) toxicity. Therefore, dose adjustment in these situations is critical.
HMG-CoA-Reductase inhibitors (statins) are widely used and generally well tolerated. They may, however, induce elevated liver enzymes or myopathy, ranging from diffuse muscle pain to potentially fatal cases of rhabdomyolysis. Even though the mechanism leading to myopathy has still not been fully elucidated, considerable evidence suggests that myotoxicity is a dose- and concentration-dependent adverse statin reaction (ADR) [5] that can affect almost any patient if concentrations are high enough [6] or if exposure is increased as a consequence of inhibition of their metabolism by co-medication [7]. However, if doses are adjusted appropriately, even potentially dangerous drug combinations can safely be administered [8, 9].
According to their clearance pathways, individual statins are susceptible to DDI with inhibitors of cytochrome P450 (CYP) 3A4 (simvastatin, lovastatin, atorvastatin), CYP2C9 (fluvastatin), P-glycoprotein (pravastatin [10]), or inhibitors of hepatic uptake transporters (pravastatin, rosuvastatin [11]). As an example, cyclosporine may modify statin kinetics by inhibiting its uptake by the liver [via organic anion transporting peptide (OAPT) 1B1], by p-glycoprotein inhibition, and probably by competitive inhibition of metabolism at CYP3A4 [12]. The development of rhabdomyolysis has indeed been reported for all combinations except fluvastatin–cyclosporine and rosuvastatin–cyclosporine (not yet marketed at the time of the study) [13].
Dosage recommendations for specific DDI are occasionally—albeit rarely—found in the official information sources, such as the drug label [summary of product characteristics (SPC)]. The aim of our study was therefore (1) to extract upper dose limits from pharmacokinetic studies that reported drug exposure with and without DDI, (2) to validate this approach by comparison with upper dose limits provided by the SPC, and (3) to evaluate the impact of considering these individual upper dose limits on the frequency of DDI alerts in a CDS system. We also suggest constraints for the transferability of the proposed method to other metabolic DDI.
Methods
We investigated all currently marketed statins in Germany (atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin).
Maximum recommended therapeutic dose (MRTD) values for specific DDI were compiled from SPCs (MRTDDDI_SPC) and pertinent pharmacokinetic studies (MRTDDDI).
Deduction of MRTDDDI values from pharmacokinetic studies
Pharmacokinetic interaction studies with oral drug administration were identified in MEDLINE and EMBASE using a search strategy with the key words: “Name of the statin” [substance name] AND “pharmacokinetics” [Subheading] AND “drug interactions” [MeSH]. In addition, articles of interest were screened for further references. We excluded case reports, in vitro studies, and animal studies. From suitable DDI trials we extracted the dosages of both interacting active drugs, the number of patients, and the basic pharmacokinetic parameters, including the area under the plasma concentration–time curve (AUC) of the active statin form before and during the interaction.
For oral drugs administered as an immediate release formulation, the AUC is directly proportional to the maintenance dose (D) provided that bioavailability (F) and clearance (Cl) are constant (linear kinetics) (Eq. 1).
A pharmacokinetic DDI can modify drug clearance by inhibiting or inducing the elimination process or alter bioavailability by affecting the absorption in the gut or pre-systemic (first-pass) elimination, or both, and consequently alter AUC. Accordingly, the ratio of the AUC, determined in the absence (AUCmono) and presence of the interaction (AUCDDI), reflects the extent of dosage adjustment (fDDI; Eq. 2) required to maintain exposure within safe and effective limits.
If a statin combination was evaluated in several (n) independent studies, fDDI was calculated using weighted AUC changes considering the number of individuals (i) in each of the studies (Eq. 3). Data were only pooled if the administered dosages and dosage frequencies of both the statin and the co-administered interacting compound were identical and study participants were comparable (i.e., either healthy individuals or patients were studied).
To consider the impact of the DDI and define MRTDDDI values, the regular MRTD values as provided by the regulatory authorities were multiplied by \( \bar{f}_{DDI} \) \( \bar{f}_{DDI} \) (Eq. 4).
To ensure clinical usefulness, we rounded off the calculated MRTDDDI values to the next higher dosage available for administration by considering marketed pharmaceutical formulations (e.g., if the calculated MRTDDDI value was 3.69 mg, we rounded it off to 5 mg if 5 mg tablets were available).
SPC information on dosage adjustments in pharmacokinetic DDI
We used the SPC of the statin’s originator brand as the source of information on the management of statins co-administered with other drugs. Dosage information included information on whether the combination was contraindicated or a specific MRTDDDI_SPC was defined, or whether a general dosage recommendation (e.g. to reduce the dose) was made.
Retrospective detection of DDI in electronic prescriptions
We retrospectively assessed consecutive electronic prescriptions in a tertiary care teaching hospital during a 1-year study period (1 November 2006 to 31 October 2007). Electronic prescriptions were issued either in outpatient clinics (printout on a prescription form) or for patients at discharge (as documented in the discharge letter). Included in the study were electronic prescriptions if they contained at least two oral single drug preparations of which one was an instant release statin with a defined dosage regimen. We regarded all DDI as separate interactions of two active ingredients and did not consider potentially interfering additional DDI or combinations of more than two interacting drugs except for fixed combinations with reliable pharmacokinetic data. All prescriptions were screened with a standard drug interaction knowledge base, including information on 9453 DDI pairs from textbooks [14], electronic data sources [15], SPCs, and information from published clinical trials. We thereby identified DDI of which the resulting ADR was potentially clinically relevant but not serious (moderate DDI alert), or of which an ADR was considered potentially serious but preventable (major DDI alert). We first assessed the number of alerts for moderate and major DDI irrespective of the prescribed dosages. We then re-analyzed the data considering actually prescribed doses and assessed the impact of taking the actually prescribed dosages into account according to (1) the SPC and (2) pharmacokinetic studies on the frequency of DDI alerts.
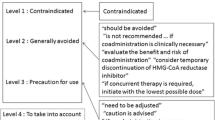
DDI alerts were categorized as appropriate if (1) no information on dosage adjustment was available in the respective source, (2) the SPC only suggested a general dose reduction in the case of co-administration, (3) the prescribed daily dose exceeded the corresponding MRTDDDI_SPC or MRTDDDI value, or (4) the combination was classified as contraindicated according to the SPC. Conversely, an alert was categorized as inappropriate if the administered dose was below MRTDDDI_SPC or MRTDDDI values.
Statistical analysis
Results are reported as proportions. The McNemar test was used to compare all nominal variables. The correlation of MRTDDDI and MRTDDDI_SPC values was assessed by calculating the Spearman correlation coefficient (SPSS version 16.0; SPSS, Chicago, IL). A p value < 0.05 was considered to be significant.
Results
DDI information in SPCs and pharmacokinetic studies
Screening the German SPCs of the six statin originator brands marketed in Germany revealed the following: (1) the combination of lovastatin is contraindicated with three macrolide antibiotics (i.e., erythromycin, clarithromycin, and telithromycin), two azole antifungals (i.e., itraconazole and ketoconazole), and all human immunodeficiency virus (HIV) protease inhibitors; (2) the same contraindications apply to simvastatin; (3) rosuvastatin is contraindicated with cyclosporine and all HIV protease inhibitors. No other active ingredient was labeled as contraindicated when co-administered with a statin. The SPC provided specific MRTDDDI_SPC values for 20 combinations of a statin with another drug. General dosage information was provided for 17 specific drug combinations and—more generally—for the co-administration of lovastatin, simvastatin, or atorvastatin with CYP 3A4 inhibitors and atorvastatin with CYP 3A4 inductors.
Screening of the literature yielded 72 pharmacokinetic interaction studies with statins; 44 of these reported significant (p < 0.05) changes in the statin AUC (Table 1). These studies covered 43 interacting statin–drug combinations, most of which involved simvastatin (n = 16). The \( \bar{f}_{DDI} \) values derived from the pharmacokinetic studies suggested statin dosage reductions by a minimum of 13% (pravastatin and itraconazole) up to a maximum of 95% (simvastatin and itraconazole) of the regular MRTD value, which was set to 100%.
Defined MRTD values were available in both the SPC and the literature for 14 statin–drug combinations. The MRTD values correlated significantly (Spearman R = 0.77, p = 0.001) (Fig. 1), confirming the theoretical approach to deduce MRTDDDI values from pharmacokinetic studies.
Correlation of maximum recommended therapeutic doses derived from published clinical trials (MRTD DDI ) and summary of product characteristics (MRTDDDI_SPC). Fourteen statin–drug combinations are shown. MRTD DDI_SPC Maximum recommended therapeutic dose for specific drug–drug interactions (DDI) compiled in the summary of product characteristics (SPC), solid line line of identity, CsA cyclosporine
Analysis of DDI alerts in electronic prescriptions
In the 1-year study period, 2457 statin-containing medication regimens, each containing on average four drugs (25% quartile = 3; 75% quartile = 6), matched the inclusion criteria. These prescriptions resulted in 8687 prescribed statin–drug pairs (referring to 879 distinct statin–drug combinations). Classification of DDI severity was available for 206 statin–drug pairs (referring to 38 distinct statin–drug combinations); in 73 of these statin–drug pairs (referring to 16 distinct statin–drug combinations), the DDI and the corresponding alert were classified as moderate or major due to a pharmacokinetic DDI increasing statin toxicity (Table 2).
The SPC provided MRTD information for 70 of these 73 prescribed statin–drug pairs (96%). Three pairs with well-documented interactions were not mentioned in the SPC (atorvastatin with phenytoin and lovastatin with diltiazem, n = 2 prescriptions; appropriate alert). For 39 prescribed statin–drug pairs, the SPC provided general warnings and suggested dosage reduction (appropriate alert). MRTDDDI_SPC values were available for 31 statin–drug pairs, and in 12 of these prescriptions the prescribed daily dose exceeded the corresponding MRTDDDI_SPC values (appropriate alert). Accordingly, for 19 prescribed statin–drug pairs, the DDI alert was inappropriate, with prescribed daily doses ≤MRTDDDI_SPC. Hence, according to SPC information, 54 of the 73 alerts (74%) were classified as appropriate. This result indicates that consideration of the dosage adjustments, as provided in the SPCs, eliminated inappropriate alerts and reduced the total number of DDI alerts by 26%.
Screening of the literature provided information on pharmacokinetic data for 70 of the 73 prescribed statin–drug pairs. Information from controlled clinical trials was lacking for three prescribed pairs (atorvastatin with phenytoin or fluconazole; n = 2 prescriptions). Data from several case reports suggest an interaction between phenytoin and atorvastatin that is potentially mediated via CYP3A4 induction by phenytoin and which results in reduced statin efficacy. However, because defined upper dose limits of atorvastatin were missing, these alerts were rated as appropriate. Accordingly, calculated MRTDDDI values were available in 70 prescriptions. The statin dosage exceeded the corresponding MRTDDDI value in 30 of these statin–drug pairs; consequently, the alert was appropriate. However, in 40 prescriptions, the statin dosage was below the respective MRTDDDI value and, therefore, the alert was categorized as inappropriate (Fig. 2). Thus, by taking quantitative dosage information from pharmacokinetic studies into consideration, 40 of the 73 alerts were categorized as inappropriate, which reduced the total number of DDI alerts by 55%, i.e., a significantly higher reduction than by MRTDDDI_SPC values (p < 0.001) (Table 2, Fig. 3). Moreover, for statin–drug pairs for which both MRTDDDI and MRTDDDI_SPC values were available, the classification agreement in terms of DDI alerts was high; 27 of 32 DDI alerts were categorized consistently.
Extent of statin overdoses indicated by the ratio between prescribed daily doses and MRTDDDI values for specific statin–drug combinations triggering a drug interaction alert. Each diamond indicates an electronically prescribed statin (as part of a combination therapy) (n = 73). MRTDDDI values are set to 1 (solid line).Diamonds in the dashed area below the solid line indicate that the corresponding drug interaction alert was classified as inappropriate because prescribed daily doses/MRTDDDI were <1
Discussion
The risk of rhabdomyolysis under statin therapy correlates with plasma concentrations [5] and thus increases with higher doses or whenever drugs reducing statin clearance are co-administered [16]. However, the long-term co-administration of statins has been proven to be safe whenever low statin doses are maintained [8, 9], stressing the importance of keeping statin concentrations below a toxic range. We therefore defined upper dose limits in DDI that allow for a safe and effective statin administration in drug combinations as well by using AUC ratios to quantify the impact of an interaction on statin exposure. Indeed, estimated MRTDDDI values for statin–cyclosporine co-administration corresponded well to dosages given in clinical trials without adverse effects [8, 9, 17], suggesting that concentration-dependent ADR of statins may be prevented by taking upper dose limits into account. The definition of upper dose limits will facilitate the selection of clinically relevant DDI and help prevent cases of over-alerting in electronic prescribing systems. In our study, the number of electronic DDI alerts in electronic prescriptions involving statins was reduced by 26% when MRTDDDI_SPC values were used as provided in the respective SPC, and by 55% when MRTDDDI values derived from pharmacokinetic studies were applied. Thus, our results demonstrate the impact of medication characteristics on alert specificity. To further personalize presented alerts, patient characteristics, such as co-morbidity, may need to be considered.
The study described here had a number of general limitations. First, in most interaction studies, the AUC is determined after the administration of a single dose and does not consider changes in drug exposure when multiple doses are given. This may lead to an underestimation of the DDI involving drugs with nonlinear kinetics and an overestimation of the extent in the case of induction. Second, we had no access to unpublished interaction data of the marketing authorization holders that may have formed the basis for the SPC information. Third, except for well-documented triplets, we only analyzed pairs of interacting active ingredients and ignored DDI with multiple combinations with potentially opposing effects, even though the patients took an average of four drugs. To date, little is known about the influence on the plasma concentrations of a substrate if more than one interacting drug (e.g., an inhibitor and an inductor) is given concurrently. Moreover, we did not consider any of the patient characteristics that may potentially increase the susceptibility to experience an ADR (e.g., hereditary muscle diseases) or factors that may modify exposure with the inhibitor or further reduce MRTD values, such as impairment of elimination organ function or pharmacogenetic polymorphisms. However, with the exception of pravastatin, statins are mainly metabolized in the liver, and renal insufficiency does not require dosage adjustment except for rosuvastatin [18]. Simvastatin, lovastatin, and atorvastatin are mainly metabolized via CYP3A4, which does not show any clinically relevant polymorphism. Only fluvastatin and, to a small extent, rosuvastatin are metabolized via polymorphic CYP2C9. For fluvastatin, it has been shown that although the pharmacokinetics of the active enantiomer are altered in poor metabolizers, the cholesterol lowering activity was similar in different genotypes [19], suggesting that this polymorphism influences neither efficacy nor safety.
While quite successful for statins, the extrapolation of our approach to other drug classes requires consideration of the following constraints. Firstly, our approach aims at preventing type A ADR, which are triggered by increased drug exposure as a consequence of pharmacokinetic DDI. We did not consider additive pharmacodynamic effects (e.g., in the case of gemfibrozil) because quantitative information on how to deal with additive or even synergistic drug effects is lacking. Some type A adverse reactions will manifest rapidly whenever a given threshold concentration is reached (e.g., carbamazepine [20]), and these ADR therefore more closely depend on factors modulating absorption rate and peak concentration than parameters affecting total drug exposure as reflected in the AUC. In these cases, our approach may possibly produce false negative alerts. Secondly, the use of AUC ratios to extrapolate dosage adjustments requires linear pharmacokinetics, with the plasma concentrations being proportional to the administered dose range. Thus, this method cannot readily be applied to compounds with non-linear pharmacokinetics. In these cases, the \( \bar{f}_{DDI} \) calculation will have to be modified to consider concentration-dependent changes in clearance. Third, the approach does not fully consider potential dose-dependency of DDI. In particular, if an inhibitor is not very potent, plateau effects may not be reached at low therapeutic doses. In these cases, inhibition effects may increase in a dose-dependent manner, and the extent of expected AUC changes should then also be adapted to the administered doses. Moreover, the approach focuses on pharmacokinetic DDI known to be relevant and most often involving CYP isozymes or drug transporters. In this setting, resulting AUC changes can be used to define dosage adjustments, with the exception of inactive or toxic prodrugs. Our approach may not be applied without modification to pharmacokinetic interactions occurring at the stages of drug release, absorption, and distribution. However, only a minority of these has been considered to be clinically relevant. In particular, pharmacokinetic interactions modifying drug absorption are either of minor clinical relevance (prolongation of t max without changes in total drug exposure) or, if a rapid onset of action is required, avoidable by adhering to a 2-h time gap in administration (e.g., bivalent cations and levodopa [21]).
Conclusion
By deducing the upper dose limits for statins from pharmacokinetic studies, DDI alerts in CDS systems become more specific and may substantially reduce over-alerting. This appears also to be a promising approach for DDI involving other drugs with linear kinetics and a slow onset of action.
References
Kuperman GJ, Bobb A, Payne T, Avery AJ, Gandhi TK, Burns G et al (2007) Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc 14:29–40
van der Sijs H, Aarts J, Vulto A, Berg M (2006) Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc 13:138–147
Paterno MD, Maviglia SM, Gorman PN, Seger DL, Yoshida E, Seger AC et al (2009) Tiering drug-drug interaction alerts by severity increases compliance rates. J Am Med Inform Assoc 16:40–46
Backman JT, Kivistö KT, Olkkola KT, Neuvonen PJ (1998) The area under the plasma concentration-time curve for oral midazolam is 400-fold larger during treatment with itraconazole than with rifampicin. Eur J Clin Pharmacol 54:53–58
Ucar M, Mjörndal T, Dahlqvist R (2000) HMG-CoA reductase inhibitors and myotoxicity. Drug Saf 22:441–457
Thibault A, Samid D, Tompkins AC, Figg WD, Cooper MR, Hohl RJ et al (1996) Phase 1 study of lovastatin, an inhibitor of the mevalonate pathway, in patients with cancer. Clin Cancer Res 2:483–491
Schmassmann-Suhijar D, Bullingham R, Gasser R, Schmutz J, Haefeli WE (1998) Rhabdomyolysis due to interaction of simvastatin with mibefradil. Lancet 351:1929–1930
Imamura R, Ichimaru N, Moriyama T, Shi Y, Namba Y, Nonomura N et al (2005) Long term efficacy of simvastatin in renal transplant recipients treated with cyclosporine or tacrolimus. Clin Transplant 19:616–621
Kobashigawa JA, Murphy FL, Stevenson LW, Moriguchi JD, Kawata N, Kamjoo P et al (1990) Low-dose lovastatin safely lowers cholesterol after cardiac transplantation. Circulation 82[Suppl 4]:281–283
Chen C, Mireles RJ, Campbell SD, Lin J, Mills JB, Xu JJ et al (2005) Differential interaction of 3-hydroxy-3-methylglutaryl-CoA-reductase inhibitors with ABCB1, ABCC2, and OATP1B1. Drug Metab Disp 33:537–546
Hsiang B, Zhu Y, Wang Z, Wu Y, Sasseville V, Yang WP et al (1999) A novel human hepatic organic anion transporting polypeptide (OATP2): identification of a liver-specific human organic anion transporting polypeptide and identification of rat and human hydroxymethylglutaryl-CoA reductase inhibitor transporters. J Biol Chem 274:37161–37168
Asberg A (2003) Interactions between cyclosporin and lipid-lowering drugs. Implications for organ transplant recipients. Drugs 63:367–378
Omar MA, Wilson JP (2002) FDA adverse event reports on statin-associated rhabdomyolysis. Ann Pharmacother 36:288–295
Baxter K (ed) (2007) Stockley’s drug interactions, 8th edn. Pharmaceutical Press, Chicago London
Lendac Data Systems: DRUGDEX® System (database on CD-ROM). Thomson Healthcare, Greenwood Village
Tobert JA (1988) Efficacy and long-term adverse effect pattern of lovastatin. Am J Cardiol 62:28J–34J
Holdaas H, Felström B, Jardine AG, Holme I, Nyberg G, Fauchald P et al, on behalf of the assessment of LEscol in renal transplantation (ALERT) study investigators (2003) Effect of fluvastatin on cardiac outcomes in renal transplant recipients: a multicentre, randomised, placebo-controlled trial. Lancet 361:2024–2031
Launay-Vachar V, Izzedine H, Deray G (2005) Statins’ dosage in patients with renal failure and cyclosporine drug-drug interaction in transplant patients. Int J Clin Cardiol 101:9–17
Kirchheiner J, Kudlicz D, Meisel C, Bauer S, Meineke I, Roots I et al (2003) Influence of CYP2C9 polymorphisms on the pharmacokinetics and cholesterol-lowering activity of (-)-3S, 5R-fluvastatin and (+)-3R, 5S-fluvastatin in healthy volunteers. Clin Pharmacol Ther 74:186–194
Höppener RJ, Kuyer A, Meijer JW, Hulsman J (1980) Correlation between daily fluctuations of carbamazepine serum levels and intermittent side effects. Epilepsia 21:341–350
Haefeli WE (2007) Drug-drug interactions with levodopa modulating treatment responses in Parkinson’s disease. J Neurol 254[Suppl 4]:IV/29–IV/36
Asberg A, Hartmann A, Fjeldså E, Bergan S, Holdaas H (2001) Bilateral pharmacokinetic interaction between cyclosporine A and atorvastatin in renal transplant recipients. Am J Transplant 1:382–386
Hermann M, Asberg A, Christensen H, Holdaas H, Hartmann A, Reubsaet JL (2004) Substantially elevated levels of atorvastatin and metabolites in cyclosporine-treated renal transplant recipients. Clin Pharmacol Ther 75:101–109
Lemahieu WP, Hermann M, Asberg A, Verbeke K, Holdaas H, Vanrenterghem Y et al (2005) Combined therapy with atorvastatin and calcineurin inhibitors: no interactions with tacrolimus. Am J Transplant 5:2236–2243
Amsden GW, Kuye O, Wei GC (2002) A study of the interaction potential of azithromycin and clarithromycin with atorvastatin in healthy volunteers. J Clin Pharmacol 42:444–449
Jacobson TA (2004) Comparative pharmacokinetic interaction profiles of pravastatin, simvastatin, and atorvastatin when coadministered with cytochrome P450 inhibitors. Am J Cardiol 94:1140–1146
Gerber JG, Rosenkranz SL, Fichtenbaum CJ, Vega JM, Yang A, Alston BL, AIDS Clinical Trials Group A5108 Team et al (2005) Effect of Efavirenz on the Pharmacokinetics of Simvastatin, Atorvastatin, and Pravastatin. Results of AIDS Clinical Trials Group 5108 Study. J Acquir Immune Defic Syndr 39:307–312
Siedlik PH, Olson SC, Yang BB, Stern RH (1999) Erythromycin coadministration increases plasma atorvastatin concentrations. J Clin Pharmacol 39:501–504
Backman JT, Luurila H, Neuvonen M, Neuvonen PJ (2005) Rifampin markedly decreases and gemfibrozil increases the plasma concentrations of atorvastatin and its metabolites. Clin Pharmacol Ther 78:154–167
Kantola T, Kivistö KT, Neuvonen PJ (1998) Effect of itraconazole on the pharmacokinetics of atorvastatin. Clin Pharmacol Ther 64:58–65
Mazzu AL, Lasseter KC, Shamblen EC, Agarwal V, Lettieri J, Sundaresen P (2000) Itraconazole alters the pharmacokinetics of atorvastatin to a greater extent than either cerivastatin or pravastatin. Clin Pharmacol Ther 68:391–400
Hsyu PH, Schultz-Smith MD, Lillibridge JH, Lewis RH, Kerr BM (2001) Pharmacokinetic interactions between nelfinavir and 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors atorvastatin and simvastatin. Antimicrob Agents Chemother 45:3445–3450
Fichtenbaum CJ, Gerber JG, Rosenkranz SL, Segal Y, Aberg JA, Blaschke T et al, NIAID AIDS Clinical Trials Group (2002) Pharmacokinetic interactions between protease inhibitors and statins in HIV seronegative volunteers: ACTG Study A5047. AIDS 16:569–577
Park JW, Siekmeier R, Lattke P, Merz M, Mix C, Schüler S et al (2001) Pharmacokinetics and pharmacodynamics of fluvastatin in heart transplant recipients taking cyclosporine A. J Cardiovasc Pharmacol Ther 6:351–361
Goldberg R, Roth D (1996) Evaluation of fluvastatin in the treatment of hypercholesterolemia in renal transplant recipients taking cyclosporine. Transplantation 62:1559–1564
Kantola T, Backman JT, Niemi M, Kivistö KT, Neuvonen PJ (2000) Effect of fluconazole on plasma fluvastatin and pravastatin concentrations. Eur J Clin Pharmacol 56:225–229
Kivistö KT, Kantola T, Neuvonen PJ (1998) Different effects of itraconazole on the pharmacokinetics of fluvastatin and lovastatin. Br J Clin Pharmacol 46:49–53
Gullestad L, Nordal KP, Berg KJ, Cheng H, Schwartz MS, Simonsen S (1999) Interaction between lovastatin and cyclosporine A after heart and kidney transplantation. Transplant Proc 31:2163–2165
Olbricht C, Wanner C, Eisenhauer T, Kliem V, Doll R, Boddaert M et al (1997) Accumulation of lovastatin, but not pravastatin, in the blood of cyclosporine-treated kidney graft patients after multiple doses. Clin Pharmacol Ther 62:311–321
Bramer SL, Brisson J, Corey AE, Mallikaarjun S (1999) Effect of multiple cilostazol doses on single dose lovastatin pharmacokinetics in healthy volunteers. Clin Pharmacokinet 37[Suppl 2]:69–77
Azie NE, Brater DC, Becker PA, Jones DR, Hall SD (1998) The interaction of diltiazem with lovastatin and pravastatin. Clin Pharmacol Ther 64:369–377
Kyrklund C, Backman JT, Kivistö KT, Neuvonen M, Laitila J, Neuvonen PJ (2001) Plasma concentrations of active lovastatin acid are markedly increased by gemfibrozil but not by bezafibrate. Clin Pharmacol Ther 69:340–345
Neuvonen PJ, Jalava KM (1996) Itraconazole drastically increases plasma concentrations of lovastatin and lovastatin acid. Clin Pharmacol Ther 60:54–61
Ring BJ, Patterson BE, Mitchell MI, Vandenbranden M, Gillespie J, Bedding AW et al (2005) Effect of tadalafil on cytochrome P450 3A4-mediated clearance: studies in vitro and in vivo. Clin Pharmacol Ther 77:63–75
Becquemont L, Neuvonen M, Verstuyft C, Jaillon P, Letierce A, Neuvonen PJ, Funck-Brentano C (2007) Amiodarone interacts with simvastatin but not with pravastatin disposition kinetics. Clin Pharmacol Ther 81:679–684
Park JW, Siekmeier R, Merz M, Krell B, Harder S, März W et al (2002) Pharmacokinetics of pravastatin in heart-transplant patients taking cyclosporin A. Int J Clin Pharmacol Ther 40:439–450
Regazzi MB, Iacona I, Campana C, Raddato V, Lesi C, Perani G et al (1993) Altered disposition of pravastatin following concomitant drug therapy with cyclosporin A in transplant recipients. Transplant Proc 25:2732–2734
Kyrklund C, Backman JT, Neuvonen M, Neuvonen PJ (2003) Gemfibrozil increases plasma pravastatin concentrations and reduces pravastatin renal clearance. Clin Pharmacol Ther 73:538–544
Neuvonen PJ, Kantola T, Kivistö KT (1998) Simvastatin but not pravastatin is very susceptible to interaction with the CYP3A4 inhibitor itraconazole. Clin Pharmacol Ther 63:332–341
Aberg JA, Rosenkranz SL, Fichtenbaum CJ, Alston BL, Brobst SW, Segal Y, ACTG A5108 team et al (2006) Pharmacokinetic interaction between nelfinavir and pravastatin in HIV-seronegative volunteers: ACTG Study A5108. AIDS 20:725–729
Kyrklund C, Backman JT, Neuvonen M, Neuvonen PJ (2003) Effect of rifampicin on pravastatin pharmacokinetics in healthy subjects. Br J Clin Pharmacol 57:181–187
Busti AJ, Bain AM, Hall RG 2nd, Bedimo RG, Leff RD, Meek C et al (2008) Effects of atazanavir/ritonavir or fosamprenovir/ritonavir on the pharmacokinetics of rosuvastatin. J Cardiovasc Pharmacol 51:605–610
Simonson SG, Raza A, Martin PD, Mitchell PD, Jarcho JA, Brown CD et al (2004) Rosuvastatin pharmacokinetics in heart transplant recipients administered an antirejection regimen including cyclosporine. Clin Pharmacol Ther 76:176–177
Cooper KJ, Mertin PD, Dane AL, Warwick MJ, Raza A, Schneck DW (2003) The effect of erythromycin on the pharmacokinetics of rosuvastatin. Eur J Clin Pharmacol 59:51–56
Schneck DW, Birmingham BK, Zalikowski JA, Mitchell PD, Wang Y, Martin PD et al (2004) The effect of gemfibrozil on the pharmacokinetics of rosuvastatin. Clin Pharmacol Ther 75:455–463
Cooper KJ, Martin PD, Dane AL, Warwick MJ, Schneck DW, Cantarini MV (2003) Effect of itraconazole on the pharmacokinetics of rosuvastatin. Clin Pharmacol Ther 73:322–329
Kiser JJ, Gerber JG, Predhomme JA, Wolfe P, Flynn DM, Hoody DW (2008) Drug/drug interaction between lopinavir/ritonavir and rosuvastatin in healthy volunteers. J Acquir Immune Defic Syndr 47:570–578
Nishio S, Watanabe H, Kosuge K, Uchida S, Hayashi H, Ohashi K (2005) Interaction between amlodipine and simvastatin in patients with hypercholesterolemia and hypertension. Hypertens Res 28:223–237
Dingemanse J, Schaarschmidt D, van Giersbergen PLM (2003) Investigation of the mutual pharmacokinetic interactions between bosentan, a dual endothelin receptor antagonist, and simvastatin. Clin Pharmacokinet 42:293–301
Ichimaru N, Takahara S, Kokado Y, Wang JD, Hatori M, Kameoka H et al (2001) Changes in lipid metabolism and effect of simvastatin in renal transplant recipients induced by cyclosporine or tacrolimus. Atherosclerosis 158:417–423
Arnadottir M, Eriksson LO, Thysell H, Karkas JD (1993) Plasma concentration profiles of simvastatin 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase inhibitory activity in kidney transplant recipients with and without ciclosporin. Nephron 65:410–413
Watanabe H, Kosuge K, Nishio S, Yamada H, Uchida S, Satoh H et al (2004) Pharmacokinetic and pharmacodynamic interactions between simvastatin and diltiazem in patients with hypercholesterolemia and hypertension. Life Sci 76:281–292
Mousa O, Brater DC, Sunblad KJ, Hall SD (2000) The interaction of diltiazem with simvastatin. Clin Pharmacol Ther 67:267–274
Kantola T, Kivistö KT, Neuvonen PJ (1998) Erythromycin and verapamil considerably increase serum simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther 64:177–182
Backman JT, Kyrklund C, Kivistö KT, Wang JS, Neuvonen PJ (2000) Plasma concentrations of active simvastatin acid are increased by gemfibrozil. Clin Pharmacol Ther 68:122–129
O’Brien SG, Meinhardt P, Bond E, Beck J, Peng B, Dutreix C et al (2003) Effects of imatinib mesylate (STI571, Glivec) on the pharmacokinetics of simvastatin, a cytochrome p450 3A4 substrate, in patients with chronic myeloid leukaemia. Br J Cancer 89:1855–1859
Kyrklund C, Backman JT, Kivistö KT, Neuvonen M, Laitila J, Neuvonen PJ (2000) Rifampin greatly reduces plasma simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther 68:592–597
Acknowledgments
The work was supported in part by the chamber of pharmacists, Baden-Wuerttemberg, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hanna Marita Seidling and Caroline Henrike Storch contributed equally to the work
Rights and permissions
About this article
Cite this article
Seidling, H.M., Storch, C.H., Bertsche, T. et al. Successful strategy to improve the specificity of electronic statin–drug interaction alerts. Eur J Clin Pharmacol 65, 1149–1157 (2009). https://doi.org/10.1007/s00228-009-0704-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0704-x