Abstract
Objective
The study sought to investigate the relationship between efavirenz exposure and the CYP2B6 516G→T(*6) genotype in HIV/AIDS outpatients, using pharmacokinetic modelling and simulation.
Methods
Blood samples where obtained from 74 outpatients treated with a combination regimen including 600 mg efavirenz daily for a duration of at least 3 weeks at clinics in Harare, Zimbabwe. The subjects were genotyped for the major CYP2B6 variant, CYP2B6*6, associated with reduced enzyme activity, using a PCR-RFLP method. Efavirenz plasma concentrations were determined by HPLC-UV. Population pharmacokinetic modelling and simulation of the data were performed in NONMEM VI.
Results
A high allele frequency of the CYP2B6*6 allele of 49% was observed. Efavirenz plasma concentrations were above 4 mg/L in 50% of the patients. Genotype and sex were identified as predictive covariates of efavirenz disposition. Pharmacokinetic parameter estimates indicate that a dose reduction to 400 mg efavirenz per day is possible in patients homozygous for the CYP2B6*6 genotype without compromising therapeutic efficacy.
Conclusion
The CYP2B6*6 allele occurs at a high frequency in people of African origin and is associated with high efavirenz concentrations. Simulations indicate that an a priori 35% dose reduction in homozygous CYP2B6*6 patients would maintain drug exposure within the therapeutic range in this group of patients. Our preliminary results suggest the conduct of a prospective clinical dose optimization study to evaluate the utility of genotype-driven dose adjustment in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of highly active antiretroviral therapy (HAART) has been scaled up in sub-Saharan Africa during recent years and is currently recommended by WHO as a first-line treatment [1]. The HAART most countries use consists of two nucleoside analogue reverse transcriptase inhibitors and a non-nucleoside reverse transcriptase inhibitor (NNRTI). There are mainly three FDA-approved NNRTIs that are widely available: efavirenz, nevirapine, and delavirdine [2]. Nevirapine is the most commonly used because of its effectiveness and low cost. The more expensive efavirenz, however, is finding increasing use in patients who develop severe adverse reactions to nevirapine [3–5] and in patients who are undergoing HIV/AIDS and TB co-treatment [6]. The latter practice is based on the likely drug-drug interaction between nevirapine (mainly metabolized by CYP3A4) and rifampicin (major inducer of CYP3A4) compared to between efavirenz (mainly metabolized by CYP2B6) and rifampicin. The treatment of HIV/AIDS-TB co-infections is a challenge in sub-Saharan Africa where over 60% of TB patients are also HIV-positive [7].
Efavirenz pharmacokinetics is associated with a long steady-state half-life of 40–55 h, suitable for once-a-day dosing [8]. Efavirenz was shown to induce its own metabolism [9]. This auto-inducible process was observed to give a three-fold increase in oral clearance after multiple administrations [10]. In vitro, efavirenz is primarily metabolized to 8-hydroxyefavirenz by CYP2B6, with secondary contribution from CYP3A [11]. High plasma concentrations of efavirenz have been significantly associated with the CYP2B6 516G→T (*6) allele single nucleotide polymorphism (SNP), which results in a Gln-to-His amino acid change [12]. The median estimated efavirenz plasma half-lives associated with GG, GT, or TT genotypes were 23, 27, and 48 h, respectively [13]. Increased plasma concentrations and the TT genotype have also been shown to correlate with increased neuropsychological toxicity [14].
The efficacy of efavirenz has been demonstrated in several clinical trials in Caucasians [15–17] and in African patients [18–21]. Efavirenz mid-dosing interval plasma concentrations below 1 mg/L have been associated with treatment failure and may select for viral drug resistance, while concentrations exceeding 4 mg/L increase the risk of adverse neuropsychiatric effects [22]. Due to the large between-subject variability [coefficient of variation (CV) 118%] in drug concentrations, in combination with a narrow therapeutic margin, therapeutic drug monitoring (TDM) has been suggested to be clinically useful during efavirenz treatment [22]. An alternative and less costly conceptual strategy to TDM has been proposed. The target concentration approach aims to explain between-subject variability in concentrations with patient-specific factors such as creatinine clearance, age, weight and/or pharmacogenetics and to let the individually predicted pharmacokinetic parameter estimates guide dosing in order to achieve optimum drug exposure and the target effect [23]. While TDM is an empirical approach, offering no explanation why a patient is having deviating drug concentrations, target concentration intervention uses pharmacokinetic models and knowledge about the concentration-response relationship.
The aim of this study was to investigate clinical correlations of efavirenz plasma concentrations with the CYP2B6*6 genotype in HIV/AIDS outpatients and to include CYP2B6 genetic polymorphism as a covariate in explaining the between-subject variability, using population pharmacokinetic modelling. Findings from this study would make a case as to whether individualization of efavirenz drug therapy could be based on the patient’s genotype rather than the current “one dose fits all” approach.
Materials and methods
HIV/AIDS outpatients
Seventy-four black African HIV-positive patients (26 men and 48 women, age 39 ± 7 years, body weight 60 ± 11 kg) assigned to receive efavirenz (600 mg, once a day) in combination with two nucleoside analogue inhibitors (73 patients were on a combination of stavudine and lamivudine and one patient on a combination of zidovudine and lamivudine) were recruited at the Wilkins and Beatrice Infectious Disease Clinics in Harare, Zimbabwe. Informed consent was obtained from all participants prior to study enrolment. The study was approved by the ethics committees at the Medical Research Council of Zimbabwe and at the Joint Parirenyatwa Hospital and College of Health Science Research, Harare.
Sampling
Samples were collected from patients who had been prescribed efavirenz for at least 3 weeks. Single blood samples were collected in EDTA, BD Vacutainer tubes (Plymouth, UK) at 11–16 h after dose administration. To support that sampling was done at steady state, 12 patients were sampled twice at a 4-week interval. After centrifugation (5 min) at 5,000 rpm, plasma was decanted and heated for 60 min at 60°C to inactivate the HIV virus. The plasma was frozen at −80°C until analyzed for drug concentrations.
Efavirenz analysis
A reversed-phase high-performance liquid chromatography (HPLC) assay was used for the determination of efavirenz steady-state concentrations. The method was validated over the range of 0.47–15 μg/mL. Sample clean-up was performed by protein precipitation of 250 μl plasma using 500 μl acetonitrile followed by centrifugation for 10 min at 20,000 g. A 240-μl supernatant aliquot was then diluted by adding 160 μl water, and 100 μl of the mixture was injected onto a ZORBAX C18 150 × 4.6 mm, 5-μm column set up in a HP1100 HPLC Agilent System with UV detection (247 nm). The mobile phase was a mixture of solutions A and B in a 65:35 proportion. Both solutions A and B consisted of glacial acetic acid, acetonitrile and 25 mM ammonia acetate buffer in proportions 1:900:100 and 1:100:900, respectively. A flow rate of 1 ml/min resulted in an efavirenz retention time of 5.2 min. An external standardization method was used with drug concentration interpolated on a calibration curve (0.47–15 μg/ml) constructed from the spiked plasma standards. Analysis of chromatograms was carried out on an Agilent HP1100 HPLC System, and data acquisition and processing were performed with Chemstation Software (Agilent Technologies, Santa Clara, CA, USA). The lower limit of quantification was 0.47 μg/mL. The inter-day precision was < 8.3 CV% and the recovery ranged from 95 to 103% for low (0.75 μg/mL), intermediate (7.50 μg/mL), and high (11.25 μg/mL) efavirenz concentrations spiked into blank human plasma.
To demonstrate the stability of the samples after inactivation at 60°C, two sets of efavirenz-spiked plasma solutions at three concentration levels (0.75, 7.5, and 11.25 μg/ml) were compared; one set at room temperature (25°C) and the other set in a water bath at 60°C, the temperature used for deactivating the samples, for 1 h. There was no significant difference between the two sets.
Stability studies (freeze-thaw, autosampler, and long-term) were carried out at three concentration levels (0.75, 7.5, and 11.25 μg/ml). The stability was assessed by calculating the percent difference between the nominal concentration and the mean obtained concentration at each concentration level of the spiked samples. The maximum percent differences were found to be 4, 2.67, and 4% for freeze-thaw, autosampler, and long-term stabilities, respectively. These results are indicative of good sample stability under the various conditions used during the study.
Potentially co-administered drugs—stavudine, lamivudine, rifampicin, isoniazid, sulfamethoxazole and trimethoprim—did not chromatographically interfere with efavirenz.
CYP2B6*6 genotyping
Patients were genotyped for CYP2B6 516G→T polymorphism using a PCR-RFLP method according to Rotger et al. [14]. Of the 74 HIV/AIDS patients, 71 were genotyped for the CYP2B6*6 polymorphism. Due to a sample processing error, there was no blood available for genotyping the remaining three patients.
Pharmacokinetic modelling
Pharmacokinetic data were evaluated using population mixed effects non-linear regression modelling in NONMEM VI level 1.1 [24]. Population estimates, between-subject variability and residual errors were quantitated using the first-order conditional estimation method with interaction (FOCE-I) for all models tested during model development.
The observed concentration in the ith subject at any measurement j was modelled as a function of the vector of pharmacokinetic model parameters φ i and the set of study design variables x ij for this subject. The random residual error between the observed and the predicted concentration was accounted for by a slope-intercept model in terms of εprop (mean 0, variance \(\sigma ^{2}_{{{\text{prop}}}} \)) and εadd (mean 0, variance \(\sigma ^{2}_{{{\text{add}}}} \)) as expressed in Eq. (1).
The vector of subject-specific model parameters was described as a function of typical population model parameters θ and of known subject-specific covariates z i such as genotype and sex. The log-normally distributed random deviation between the typical parameter values in the population and the individual parameter estimates was expressed by the vector η i (mean 0, variance ω2) as can be seen in Eq. (2).
During model development, single and multi-compartment pharmacokinetic structural models were tried. In order to quantitate the impact of CYP2B6*6 genetic polymorphism on the metabolism of efavirenz, genotype was tested as a categorical covariate on efavirenz oral clearance. Other mechanistically plausible covariates (sex, body weight and age), showing any trend when plotted against the empirical Bayesian parameter estimates obtained from the base model, were included in a stepwise additive forward manner. Suggested covariates were retained in the full model if they were found to be important also after backward deletion using a stricter statistical significance criterion (P < 0.01). For a covariate to be considered clinically relevant, it has to reduce some of the unexplained between-subject variability in the pharmacokinetic parameter. Missing genotype data records were handled by creating a missing genotype category. Clearance values in these individuals were modelled as the weighted average clearance for the GG, GT, and TT genotypes. Missing sampling times were replaced by the median sampling time (12 h). To evaluate the impact of the imputed data, the final model was rerun with the missing data excluded.
In NONMEM, maximum likelihood parameter estimates are obtained after nonlinear regression by the minimization of an objective function value (OFV) approximately equal to -2 × log-likelihood of the data. Discrimination between nested models was achieved by using the log-likelihood ratio where the difference in the OFV between the full and the reduced model is asymptotically chi-square distributed. Differences were evaluated at the P < 0.05 and the P < 0.01 significance levels corresponding to a reduction of 3.84 and 6.63 OFV points, respectively, for one degree of freedom. Diagnostic goodness-of-fit plots and evaluation of parameter precision, including a comparison of estimates derived from a nonparametric bootstrap (n = 200) in PsN 2.2.3 [25], were also guiding model selection. S-plus version 7.0 (Insightful, Seattle, WA, USA) was used to generate goodness-of-fit plots and other graphs. The extent of shrinkage, associated with poor individual parameter estimates, was calculated for clearance using the following equation:
Where SD η CL is the standard deviation of the individual estimates of η for CL and ωCL is the standard deviation of the estimated population variance. If the two values are similar, the extent of shrinkage would be low, which is desirable [26].
Dose individualization
Finally, the developed model was used to evaluate the potential for a priori dose adjustment of efavirenz in poor metabolizers. Simulations of concentration time profiles in virtual subjects (n = 2,000, 50% males) were undertaken to investigate whether a dose reduction from 600 to 500, 400 or 300 mg efavirenz once daily in intermediate and/or poor metabolizers would meet a predefined clinically relevant criterion. In this case it was considered acceptable if at least 95% of patients had concentrations exceeding 1 mg/L at the mid-dose interval and if the proportion of patients reaching concentrations greater than 4 mg/L was minimized.
Results
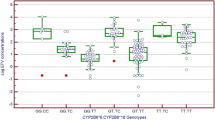
Out of 71 genotyped patients, 30% (12 females), 44% (31 females), and 27% (19 females) were classified as extensive (GG), intermediate (GT), and poor (TT) metabolizers of efavirenz, respectively. A total of 86 concentrations from 74 patients were included in the study database. Concentrations with recorded sampling times (n = 64) were available from 58 of these patients. None of the HIV/AIDS outpatients studied had efavirenz plasma concentrations below 1 mg/L, predicted to be a therapeutically effective level, but approximately 50% of the patients exhibited plasma concentrations exceeding the upper safety limit of 4 mg/L. Observed plasma concentrations grouped by sex and genotype are shown in Fig. 1. With a mean concentration ratio for the patients with two sampling occasions of 1.00 (96%CI 0.87, 1.14), efavirenz plasma concentrations appeared stable.
Box and whiskers plot showing the observed efavirenz plasma concentrations at steady state in 71 HIV/AIDS patients of Zimbabwean origin. GG Extensive metabolizer, GT intermediate metabolizer, TT poor metabolizer. The dotted horizontal lines show the optimum concentration interval (1–4 mg/L). A total of 30% (12 females), 44% (22 females), and 27% (11 females) were classified as GG, GT, and TT genotype, respectively
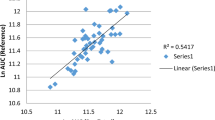
A modified one-compartment pharmacokinetic model with first-order absorption was fitted to the observed concentration-time data. As a best-guess model, clearance was parameterized with genotype as a predictive categorical covariate. This gave a significant decrease in the OFV (13 points), and the unexplained between-subject variability was reduced from 87 to 79%. Further, explorative plots gave evidence of a relationship between the individually predicted clearance values and sex. Inclusion of sex gave a significantly lower OFV (7 points), and the between-subject variability was reduced from 79% to 76%. Oral clearance was estimated at 9.4 (95%CI 6.2, 12.6) L/h for extensive-metabolizing men. The ratio of efavirenz clearance for intermediate- and poor-metabolizing men relative to extensive metabolizers was 0.77 (95%CI 0.46, 1.1) and 0.42 (95%CI 0.21, 0.63), respectively. Females were estimated to have a metabolizing capacity of 70% (95% CI 0.47, 0.94) compared to that in males. The magnitude of the shrinkage for clearance was 5.1%. Pharmacokinetic parameter estimates are presented in Table 1. Basic goodness-of-fit plots for the final model are shown in Fig. 2. An overall diagnostic plot, displaying the differences between the typical concentration-time profiles in the specific subpopulations, is given in Fig. 3.
Basic goodness of fit of the final efavirenz model. The predictions should match the observations. The residuals should be distributed evenly around the reference line over time and should not give a pronounced slope over the predicted concentration range. Upper left panel The observations are plotted versus the population predictions. Upper right panel The observations are plotted against the individual predictions. Lower left panel The individually weighted residuals are plotted versus time after dose. Lower right panel The absolute values of the individually weighted residuals are seen versus the individual predictions. The dashed lines are the lines of identity or the zero reference lines. The solid line is a smooth nonparametric regression line
Overall goodness-of-fit plot of the final model. Observed and predicted efavirenz steady-state concentrations are sorted by sex and genotype. Open circles are the observed concentrations. The solid lines are the model predictions in a typical individual. The dashed horizontal lines show the optimum concentration interval (1–4 mg/L). Note that concentrations without recorded sampling times are imputed at 12 h
Simulations of potential dose adjustments demonstrated that a reduction in the efavirenz dose from 600 to 400 mg once a day would give reduced but acceptable efavirenz exposure in poor metabolizers. In poor-metabolizing females, the dose could be further reduced to 300 mg once a day. A priori dose adjustments were not found to be achievable for intermediate-metabolizing men, but a daily dose of 500 mg would give acceptable exposure in intermediate-metabolizing females (Table 2).
Discussion
In this study, efavirenz plasma concentrations and the prevalence of the CYP2B6*6 variant were investigated in HIV/AIDS outpatients in Zimbabwe. The results showed a prevalence of the CYP2B6*6 allele variant of 49% and a predicted frequency of extensive metabolizers (GG) of 30%, intermediate metabolizers (GT) of 44%, and poor metabolizers (TT) of 27%. There was an association between high efavirenz clinical concentrations and the poor metabolizer genotype. In addition, women were shown to have higher efavirenz plasma concentrations compared to men irrespective of genotype. Pharmacokinetic modelling of the data demonstrated the predictive value of including both sex and genotype data as covariates in the model to explain the between-subject variability of efavirenz exposure.
The high frequency of approximately 50% of the CYP2B6*6 mutation in the outpatients is in agreement with population genotype data showing that the low-activity CY2B6*6 variant is more prevalent in people of African origin compared to Caucasians and Asians [10, 12, 27, 28]. Our finding that women have high plasma concentrations is also in agreement with previous reports that females appear to be more susceptible to efavirenz adverse drug reactions [29]. Furthermore, females have also been seen to have a higher discontinuation rate of efavirenz therapy [30]. The reason for the metabolic difference between men and women is however still not known. A recent study has shown that women of Hispanic origin have increased CYP2B6 metabolic capacity compared to women and men of African and Caucasian origin [31]. This difference was attributed to some SNPs in the regulatory regions of CYP2B6 resulting in Hispanic women having more CYP2B6 mRNA, protein, and enzyme activity compared to males and females of African and Caucasian origin. So, in addition to the need to genotype for other SNPs associated with CYP2B6 reduced activity [32], there is need to genotype for SNPs in the regulatory region that might explain gender differences in CYP2B6 expression and activity.
Several reports have described the impact of race on efavirenz metabolism. Ethnic differences in plasma drug exposure has been observed [33]. Burger et al. identified race as a predictive factor with consistently higher efavirenz plasma concentrations in non-Caucasian patients [27], and lower clearance values were predicted in Asian and black relative to Caucasian subjects [10]. The relationship between CYP2B6*6 genotype and efavirenz pharmacokinetics has been described in several studies [12, 13]. However, genetic polymorphism has, to our knowledge, never been included as a covariate in a pharmacokinetic model explaining the between-subject variability in efavirenz exposure.
In this study, which is the first report describing the population pharmacokinetics of efavirenz in an African population, as many as 50% of the patients were exposed to efavirenz plasma concentrations associated with risk for adverse reactions but none had suboptimum exposure. The data therefore clearly demand a redress of the clinical dosing of efavirenz in HIV/AIDS patients in Zimbabwe. To explain the between-subject variability in efavirenz disposition and to evaluate the impact of seemingly important covariates, we carried out population pharmacokinetic modelling of the data. After inclusion of CYP2B6 genotype and sex, the typical extensive metabolizer was identified to have a two-fold faster oral clearance than the typical poor metabolizer and the typical female patient only 70% of the metabolic capacity compared to the typical male patient.
Due to the large between-subject variability, the effects may be smaller or even greater in the individual patient, as is evident from Fig. 3. Still, the remaining unexplained between-subject variability (76%) is considerable in comparison with the effects of sex and genotype on efavirenz pharmacokinetics. Some of this variability can potentially be reduced by considering any interference of co-medication and drug-drug interactions involving the expression and/or activities of CYP2B6 and CYP3A4, enzymes involved in the metabolism of efavirenz [37]. Unfortunately the use of concomitant medication was not recorded in the present study, but participants in this study were also taking anti-TB drugs, including rifampicin, which is known to be an inducer of CYP3A4 to a major extent and CYP2B6 to a lesser extent.
Post-dose times were based on trust that the participants were all taking their medication at the stipulated time, which could be another source of unexplained variability. Other potential factors affecting efavirenz pharmacokinetics include plasma-protein binding and other pharmacogenetic polymorphisms.
Model parameter estimates expressing oral clearance values were in general well estimated. The estimate in extensive-metabolizing men was in agreement with what has been previously observed in other populations [10, 33–35]. On the contrary, the absorption rate constant and the volume of distribution (V/F) were estimated with a higher level of uncertainty. This may arise from the fact that sparse sampling at steady state was employed. Essentially only one sample was collected from each patient, and few samples were taken during the early concentration-time profile. However, a sensitivity analysis performed with various fixed values of the absorption rate constant and the volume of distribution resulted only in marginal changes in the estimation of clearance and did not alter the OFV. The volume of distribution and absorption rate constant were similar to estimates reported in previous population pharmacokinetic analyses [10, 33–35]. Sparse or uninformative data may also cause the empirical Bayes estimates to shrink towards the mean [26], which can lead to falsely included covariates or failure to identify true covariates. In the present analysis we did not observe any substantial shrinkage for the clearance parameter.
Simulation of clinical trials is a powerful predictive tool and has been shown to be useful for optimum dose selection, optimization of study design and for hypothesis-generating purposes [36]. In the present analysis, we sought to simulate possible dose adjustments by genotype and sex. Simulations assessed that a reduction in the dose in poor metabolizers would maximize the percentage of patients reaching target plasma concentrations without compromising the therapeutic efficacy of efavirenz therapy. An a priori dosing regimen of 400 mg once a day would be a suitable initial dose adjustment in these patients. Based on feedback observations, further dose individualization is possible in each individual if required. Since the upper bound of the 95% CI describing sex differences is close to 1, no specific dose adjustments are proposed for females although simulations suggested that dose reductions to 500 and 300 mg are feasible for intermediate- and poor-metabolizing females, respectively.
In conclusion, modelling and simulation are important tools in pharmacogenetically guided optimization of pharmacotherapy. Understanding the effect of CYP2B6 pharmacogenetic variability on the population pharmacokinetics of efavirenz can assist in adopting a priori individualized efavirenz dosage in routine clinical care. The possibility of individualizing efavirenz dosage in poor metabolizers should ultimately be confirmed in combination with pharmacodynamic variables in directed prospective clinical trials.
References
WHO (2003) Scaling up antiretroviral therapy in resource-limited settings: treatment guidelines for a public health approach, 2003 revision. http://www.who.int/pub/prev_care/en/arvrevision2003en.pdf. Cited April 25, 2007
De Clercq E (2007) Anti-HIV drugs. Verh K Acad Geneeskd Belg 69:81–104
Hahn JA, Maier M, Byakika-Tusiime J, Oyugi JH, Bangsberg DR (2007) Hepatotoxicity during nevirapine-based fixed-dose combination antiretroviral therapy in Kampala, Uganda. J Int Assoc Physicians AIDS Care (Chic Ill) 6(2):83–86
Jamisse L, Balkus J, Hitti J, Gloyd S, Manuel R, Osman N, Djedje M, Farquhar C (2007) Antiretroviral-associated toxicity among HIV-1-seropositive pregnant women in Mozambique receiving nevirapine-based regimens. J Acquir Immune Defic Syndr 44(4):371–376
Rivero A, Mira JA, Pineda JA (2007) Liver toxicity induced by non-nucleoside reverse transcriptase inhibitors. J Antimicrob Chemother 59(3):342–346
Harries AD (2006) HIV/AIDS and TB. Trop Doct 36(2):65–67
Maher D, Harries A, Getahun H (2005) Tuberculosis and HIV interaction in sub-Saharan Africa: impact on patients and programmes; implications for policies. Trop Med Int Health 10(8):734–742
Smith PF, DiCenzo R, Morse GD (2001) Clinical pharmacokinetics of non-nucleoside reverse transcriptase inhibitors. Clin Pharmacokinet 40:893–905
Adkins JC, Noble S (1998) Efavirenz. Drugs 56(6):1055–1064
Barrett J, Joshi AS, Chai M, Ludden TM, Fiske WD, Pieniaszek HJ (2002) Population pharmacokinetic meta-analysis with efavirenz. Int J Clin Pharmacol Ther 40:507–519
Ward BA, Gorski JC, Jones DR, Hall SD, Flockhart DA, Desta Z (2003) The cytochrome P450 2B6 (CYP2B6) is the main catalyst of efavirenz primary and secondary metabolism: implication for HIV/AIDS therapy and utility of efavirenz as a substrate marker of CYP2B6 catalytic activity. J Pharmacol Exp Ther 306:287–300
Haas DW, Smeaton LM, Shafer RW, Robbins GK, Morse GD, Labbe L, Wilkinson GR, Clifford DB, D’Aquila RT, De Gruttola V, Pollard RB, Merigan TC, Hirsch MS, George AL Jr, Donahue JP, Kim RB (2005) Pharmacogenetics of long-term responses to antiretroviral regimens containing efavirenz and/or nelfinavir: an adult AIDS clinical trials group study. J Infect Dis 192:1931–1942
Ribaudo H, Haas DW, Tierney C, Kim RB, Wilkinson GR, Gulick RM, Clifford DB, Marzolini C, Fletcher CV, Tashima KT, Kuritzkes DR, Acosta EP (2006) Pharmacogenetics of plasma efavirenz exposure after treatment discontinuation: an adult aids clinical trials group study. Clin Infect Dis 42:401–407
Rotger M, Colombo S, Furrer H, Bleiber G, Buclin T, Lee BL, Keiser O, Biollaz J, Décosterd L, Telenti A and the Swiss HIV cohort study (2005) Influence of CYP2B6 polymorphism on plasma and intracellular concentrations and toxicity of efavirenz and nevirapine in HIV-infected patients. Pharmacogenet Genomics 15(1):1–5
Staszewski S, Morales-Ramirez J, Tashima KT, Rachlis A, Skiest D, Stanford J, Stryker R, Johnson P, Labriola DF, Farina D, Manion DJ, Ruiz NM (1999) Efavirenz plus zidovudine and lamivudine, efavirenz plus indinavir, and indinavir plus zidovudine and lamivudine in the treatment of HIV-1 infection in adults. Study 006 Team. N Engl J Med 341:1865–1873
Robbins GK, De Gruttola V, Shafer RW, Smeaton LM, Snyder SW, Pettinelli C, Dube MP, Fischl MA, Pollard RB, Delapenha R, Gedeon L, van der Horst C, Murphy RL, Becker MI, D’Aquila RT, Vella S, Merigan TC, Hirsch MS; AIDS Clinical Trials Group 384 Team (2003) Comparison of sequential three-drug regimens as initial therapy for HIV-1 infection. N Engl J Med 349:2293–2303
Bartlett JA, Johnson J, Herrera G, Sosa N, Rodriguez A, Liao Q, Griffith S, Irlbeck D, Shaefer MS (2006) Long-term results of initial therapy with abacavir and lamivudine combined with efavirenz, amprenavir/ritonavir, or stavudine. J Acquir Immune Defic Syndr 43:284–292
Daneil C, Moh R, Anzian A, Abo Y, Chenal H, Guehi C, Gabillard D, Sorho S, Rouet F, Eholie S, Anglaret X (2006) Tolerance and acceptability of an efavirenz-based regimen in 740 adults (predominantly women) in west Africa. J Acquir Immune Defic Syndr 42(1):29–35
Wester CW, Kim S, Bussman H, Ndwapi N, Peter TF, Gaolathe T, Mujugira A, Busang L, Vanderwarker C, Cardiello P, Johnson O, Thior I, Mazonde P, Moffat H, Essex M, Marlink R (2005) Initial response to highly active antiretroviral therapy in HIV-1C infected adults in a public sector treatment program in Botswana. J Acquir Immune Defic Syndr 40:336–343
Kebba A, Atwine D, Mwebaze R, Kityo C, Nakityo R, Peter M (2002) Therapeutic responses to AZT + 3TC + EFV in advanced antiretroviral naive HIV type 1-infected Ugandan patients. IDS Res Hum Retroviruses 18:1181–1187
Coetzee D, Hildebrand K, Boulle A, Maartens G, Louis F, Labatala V, Reuter H, Ntwana N, Goemaere E (2004) Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa. AIDS 18:887–895
Marzolini C, Telenti A, Decosterd LA, Greub G, Biollaz J, Buclin T (2001) Efavirenz plasma levels can predict treatment failure and central nervous system side effects in HIV-1-infected patients. AIDS 5:71–75
Holford N (1999) Target concentration intervention: beyond Y2K. Br J Clin Pharm 48:9–13
Beal SL, Sheiner LB, Boeckmann AJ (eds) (1986–2006) NONMEM users guides. Icon Development Solutions, Ellicot City, MD, USA
Lindbom L, Pihlgren P, Jonsson EN (2005) PsN-toolkit—a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 79(3):241–257
Savic RM, Wilkins JJ, Karlsson MO (2006) (Un)informativeness of empirical Bayes estimate-based diagnostics. AAPS J 8(S2):abstract T3360
Burger D, van der Heiden I, la Porte C, van der Ende M, Groeneveld P, Richter C, Koopmans P, Kroon F, Sprenger H, Lindemans J, Schenk P, van Schaik R (2005) Interpatient variability in the pharmacokinetics of the HIV non-nucleosid reverse transcriptase inhibitor efavirenz: the effect of gender, race and CYP2B6 polymorphism. Br J Clin Pharm 61:148–154
Haas DW, Ribaudo HJ, Kim RB, Tierney C, Wilkinson GR, Gulick RM, Clifford DB, Hulgan T, Marzolini C, Acosta E (2004) Pharmacogenetics of efavirenz and central nervous system side effects: an adult AIDS clinical trials group study. AIDS 18:2391–2400
van Twillert G, van Santen G, Godfried MH (2005) Severe psychosis in an African woman due to the antiretroviral agent efavirenz. Ned Tijdschr Geneeskd 26:2687–2689
Spire B, Carrieri P, Garzot MA, L’Henaff M, Obadia Y, TRT-5 Group (2004) Factors associated with efavirenz discontinuation in a large community-based sample of patients. AIDS Care 16:558–564
Lamba V, Lamba J, Yasuda K, S Strom, J Davila, Hancock ML, Fakenthal JD, Rogan PK, Ring B, Wrighton SA, Schuetz EG (2003) Hepatic CYP2B6 expression: gender and ethnic differences and relationship to CYP2B6 genotype and CAR(constitutive androstane receptor) expression. J Pharmacol Exp Ther 307(3):906–922
Wolbold R, Klein K, Burk O, Nüssler AK, Neuhaus P, Eichelbaum M, Schwab M, Zanger UM (2003) Sex is a major determinant of CYP3A4 expression in human liver. Hepatology 38(4):978–988
Csajka C, Marzolini C, Fattinger K, Decosterd LA, Fellay J, Telenti A, Biollaz J, Buclin T (2002) Population pharmacokinetics and effects of efavirenz in patients with human immunodeficiency virus infection. Clin Pharm Ther 73:20–30
Pfister M, Labbé L, Hammer SM, Mellors J, Bennett KK, Rosenkrantz S, Sheiner LB (2003) Population pharmacokinetics and pharmacodynamics of efavirenz, nelfinavir and indinavir: adult AIDS clinical trial group study 398. Antimicrob Agents Chemother 47:130–137
Kappelhoff BS, Huitema AD, Yalvac Z, Prins JM, Mulder JW, Meenhorst PL, Beijnen JH (2005) Population pharmacokinetics of efavirenz in an unselected cohort of HIV-1-infected individuals. Clin Pharmacokinet 44:849–861
Holford NHG, Kimko HC, Montleone JPR, Peck C (2000) Simulation of clinical trials. Annu Rev Pharmacol Toxicol 40:67–95
Turpeinen M, Raunio H, Olavi P (2006) The functional role of CYP2B6 in human drug metabolism: substrates and inhibitors in vitro, in vivo and in silico. Curr Drug Metab 7:705–714
Acknowledgements
We are grateful to the Wilkins and Beatrice Infectious Disease Clinics for assistance with sample collection. We are grateful to AstraZeneca, Mölndal, DMPK Development Section and Dr. Xueqing Li for hosting Christopher Nyakutira for a 3-month bioanalytical training. Emmanuel Chigutsa is a recipient of a master’s fellowship from the International, Clinical and Operational Health Services Research Training Award (ICOHRTA) for AIDS and TB. Tafadzwa Mhlanga’s assistance with the CYP2B6*6 genotyping work is also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Christopher Nyakutira and Daniel Röshammar made equal contributions to this work.
Rights and permissions
About this article
Cite this article
Nyakutira, C., Röshammar, D., Chigutsa, E. et al. High prevalence of the CYP2B6 516G→T(*6) variant and effect on the population pharmacokinetics of efavirenz in HIV/AIDS outpatients in Zimbabwe. Eur J Clin Pharmacol 64, 357–365 (2008). https://doi.org/10.1007/s00228-007-0412-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0412-3