Abstract
Background and objective
The validity of using self-reported or parental reported asthma symptoms and/or doctor-diagnosed asthma in the estimation of asthma prevalence among children has been questioned. The aim of this study was to assess the prevalence of dispensed anti-asthmatic medications as a proxy of asthma among children and adolescents aged 0–19 years in Norway.
Methods
Prescription data on subjects aged 0–19 years receiving at least one prescription for an anti-asthmatic during 2004 were retrieved from the nationwide Norwegian Prescription Database.
Results
Overall, 108,719 (9.1% of the Norwegian population aged 0–19 years) individuals received at least one prescription for medication(s) for obstructive airway diseases. The application of criteria that restricted the study population to those receiving inhaled anti-asthmatic medications and those receiving medications reimbursed by the Norwegian health care system for asthma resulted in the identification of 64,458 (5.4%) individuals (4.6% of girls and 6.2% of boys). The prevalence varied by age, with a maximum in both genders at about 2 years of age (7.0% of girls and 10.1% of boys) and a minimum in girls at about 10 years of age (3.3%) and in boys at about 19 years of age (3.5%). Anti-asthmatic inhalants were more frequently prescribed among boys than among girls during the first 15 years of life. Of the children treated, 75% received inhaled glucocorticoids (ICS) in combination with β2-agonists, of whom 38% received a fixed combination in one inhaler.
Conclusions
In 2004, about 1 in 20 Norwegians aged 0–19 years were in need of medical treatment for asthma for at least 3 months, reflecting ongoing and clinically important asthma. A rather high proportion of children received fixed combinations of ICS and long-acting β2-agonists, which may indicate moderate to severe asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is the most common chronic disease among children and adolescents. The prevalence of asthma varies greatly both within and between countries [1, 2]. Most reports on the prevalence of paediatric asthma are based on self-reported or parental reported symptoms, such as wheeze and breathlessness, and/or on doctor-diagnosed asthma. Although there are established standardised questionnaires, several studies have brought into question the use of self-reported asthma or different asthma symptoms as a measure of asthma and asthma prevalence [3–5]. In addition, most of the asthma prevalence studies conducted to date have tended to involve local populations or to have recruited only some age-groups, thereby preventing researchers to generalise the results to asthma prevalence in a whole population. Several industrialised countries have health care administrative databases on prescriptions, and a number of these have shown the feasibility of using the databases to identify individuals with asthma [6–9]. Prescriptions on anti-asthmatic medications may provide an alternative method of assessing asthma prevalence in a population.
The objective of this study was to assess the prevalence of dispensed anti-asthmatic medications as a proxy of asthma among children and adolescents aged 0–19 years in Norway using a nationwide prescription database.
Methods
Norwegian prescription database
Data were drawn from the Norwegian Prescription Database (NorPD). In accordance with a law implemented in January 2004, all Norwegian pharmacies are legally required to send electronic data to this database on all prescription drugs dispensed [10]. All prescriptions irrespective of reimbursement or not are stored in the database. The drugs are classified according to the Anatomical Therapeutic Chemical Classification System (ATC) [11]. Among the data collected are the patient's unique identifying number (encrypted), sex and age, the date of dispensing, information on the drug (brand name, package size, number of packages, ATC-code, defined daily dose, price) and eventual code of reimbursement. In 2004, code §9.2 was reserved for obstructive airway diseases, and it has been suggested that the dispensing of medications with this code may function as a proxy of asthma diagnosis for children and adolescents. The system for general reimbursement in Norway is basically a “positive list” system, based on a list of diseases or conditions for which pharmaceutical treatment can be reimbursed. Reimbursement is granted only under the condition that the patient has a chronic disease for which “long-term” medication (more than 3 months) is necessary [12]. The ceiling of for total co-payments in 2004 was 1550 NOK (190 Euros), and there were no co-payments for children under 7 years of age.
Study population
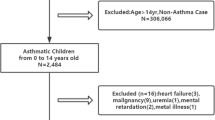
We studied drug utilisation in 2004 in Norwegian children and adolescents aged 0–19 years, corresponding to years of birth between 1985 and 2004 (n = 1,192,841). We included all individuals receiving dispensed drugs for obstructive airway diseases that have the ATC-code R03 [11]. In a second step, we removed all those individuals who received only mixtures with either ephedrine or β2-agonist (ATC-code R03C). Our reasoning for taking this second step was based on the assumption that these drugs are mainly prescribed for incidental, unspecific, acute upper respiratory tract symptoms and infections in preschool children [13]. In a third step, we focused on subjects receiving only inhaled anti-asthmatics reimbursed for the treatment of asthma (§9.2) in accordance with the Norwegian reimbursement scheme: either selective β2-agonists (ATC-code R03AC) and/or glucocorticoids (ATC-code R03BA), and/or long-acting β2-agonists (LABA)/glucocorticoids combined in one inhaler (ATC-code R03AK). The prescription of anti-asthmatic drugs in our study was defined as at least one prescription of the specified drug(s) dispensed from a pharmacy during 2004. A data capture period of 12 months was selected because shorter periods will greatly be influenced by seasonal variation of asthma symptoms. Prevalence figures were calculated using the age- and gender-specific distribution of the mean population in Norway 2004 as the denominator.
Results
Overall, in 2004, 108,719 (9.1% of all Norwegians aged 0–19 years ) Norwegians aged 0–19 years received at least one prescription for medications for obstructive airway diseases – ATC-code R03 (Table 1). The age-specific prevalence was highest in both genders at about 1 year of age (22.5% in girls and 29.0% in boys) and was the lowest in girls at about 10 years of age (4.3%) and in boys at 19 years of age (4.0%); children under 1 year of age were not taken into account (Fig. 1).
The removal of those individuals who received only mixtures with either ephedrine or β2-agonist (ATC-code R03C) resulted in a case cohort of 67,822 individuals (5.7%; 4.9% of girls and 6.4% of boys). When the study population was restricted still further to those receiving reimbursed inhaled anti-asthmatic medications, only 64,458 (5.4%) individuals remained (4.6% of girls and 6.2% of boys) (Table 1). The prevalence varied by age with a maximum in both genders at an age of about 2 years (7.0% of girls and 10.1% of boys) and a minimum in girls at about 10 years of age (3.3 %) and in boys at 19 years of age (3.5%); children younger than 1 year were not taken into account (Fig. 2). Anti-asthmatics were more frequently prescribed to boys than girls during the first 15 years of life, after which an opposite pattern was revealed (Figs. 1 and 2).
Some 1.3% of girls and 1.4% of boys received only inhaled β2-agonists in 2004 (Table 2). Of the children treated children, 75% received glucocorticoids (inhaled glucocorticoids, ICS) alone or in combination with β2-agonists. The prescription of separate devices for ICS and β2-agonists was found for 2.0% of the girls and 3.0% of the boys, while fixed combinations of ICS and long-acting β2-agonists was given to 1.3% of the girls and 1.7% of the boys. Fixed combinations were mainly used in the 9- to 19-year age group.
Discussion
About 9% of all Norwegians between 0 and 19 years of age received at least one medication against obstructive airway diseases in 2004. The prevalence declined to 5.7% when we removed those individuals using only mixtures with either ephedrine or β2-agonists and no other drugs for obstructive airway disease; a subsequent analysis of this group revealed that it consisted primarily of preschool children. A further restriction to those who received reimbursed inhaled anti-asthmatic medication for long-term treatment – i.e. treatment for ≥3 months – changed the prevalence only slightly, from 5.7 to 5.4%. The age-specific prevalence was highest in early life, with a maximum around the age of 2 years. The prevalence was clearly higher in boys than in girls during childhood, but the gender difference was gradually reduced with increasing age, and from the age of 16 years onwards the use of anti-asthmatics was more prevalent in girls than boys. Of the children and adolescents treated, 75% received ICS combined with β2-agonists; this indicates the proportion of moderate to severe asthma among treated children.
The strength of the present study is that it provides age- and gender-specific information on all dispensed prescriptions for anti-asthmatics for the entire child and adolescent population of Norway. This approach eliminates the possibility of selection and recall bias and attenuates any effect of the seasonal variation in asthma, which may be the case of prevalence estimates based on cross-sectional surveys with self-reported or parental reports of asthma symptoms and/or doctor-diagnosed asthma.
An assessment of the asthma prevalence in an entire population is challenging as no single instrument can be used to identify asthma with certainty. Asthma is a clinical diagnosis made by physicians on the basis of a patient’s medical history, a clinical examination and the exclusion of alternative diagnoses that mimic asthma. Most reports on asthma prevalence among children and adolescents are based on surveys in which parents were asked about asthma symptoms in their children and/or the asthma was diagnosed by a doctor. A Danish study analysed parental-reported children’s use of asthma drugs during the preceding 12 months using data from a population-based database on dispensed drugs as the reference standard [14] and found high validity and agreement between the two data sources. However, several other studies have brought into question the validity of using parental reporting in questionnaires for measuring asthma prevalence [3–5]. Although physician-diagnosed asthma is not the true gold standard of asthma, it has been considered to represent the most appropriate standard for validating methods for epidemiological studies [15]. The purchase of anti-asthma medication represents a common event for most children with asthma in developed countries. Pharmacy data may therefore be a valuable alternative to survey data to assess the extent to which large populations are affected by chronic conditions such as asthma. The validation of dispensed prescriptions of asthma medications as a marker for asthma in individuals ≥17 years of age was demonstrated in a study from Illinois in USA , thereby showing that the use of these databases is warranted [16]. Data on drugs prescribed, rather than those dispensed, can lead to the misclassification of drug exposure due to primary non-compliance [17]. Our data are based on dispensed drugs rather than only prescribed drugs, and this may increase the usefulness of our database.
Before being prescribed asthma medication in Norway, symptoms must be perceived and presented to a doctor, and the doctor has to recognise the symptoms as asthma-like and make a decision to prescribe an anti-asthmatic drug. The threshold for consulting a doctor can vary. However, in general, Norwegians have a high educational level, no or low co-payment fee, a well-developed government-financed health care system and one of the highest rates of practising physicians per 1000 inhabitants in the world [18]. This should ensure a low threshold for seeking medical advice for asthmatic symptoms for most inhabitants. Another advantage is that the NorPD includes prescriptions from all kinds of practising physicians prescribing to patients living outside institutions in Norway, both general practitioners and specialists. Our approach to assessing asthma may underestimate the prevalence of mild undiagnosed asthma in patients not having been prescribed any medication. However, a study from a prescribing database in general practice in the Netherlands found that a prescription of one or more anti-asthmatics identified 95% of adults with an asthma diagnosis [19]. On the other hand, non-asthma patients having been treated with anti-asthmatics will lower the validity of using prescribing data for identifying patients by causing an overestimation of the figures.
In this nationwide population study, 5.4% of the children and adolescents filled a prescription of an inhaled, reimbursed anti-asthmatic drug. This percentage is comparable with the results from a recent Dutch pharmacy-based study in which the prevalence of asthma drug usage was 5% in 0- to 14-year-old children [9] but lower than that in a number of other studies based on self-reported asthma symptoms and/or diagnoses in certain age groups [1, 20–22]. While the population of children for whom medications are dispensed is smaller than that of children labelled as having asthma, the former is more likely consist of children with active disease [23]. Our prevalence figures are, however, quite consistent with recent questionnaire-based findings in a Norwegian birth cohort study (asthma prevalence at 4 years of age (6.4%) and at 10 years of age (5.6%) [24, 25]. The aim of that study was to register the occurrence of children with ongoing doctor-diagnosed asthma, and its endpoint is in reasonable agreement with our endpoint.
The present study confirms a pattern of age and gender distribution of asthma that has been indicated by various studies addressing asthma prevalence in different age groups and with different methods but which – to the best of our knowledge – has never been studied in similar detail in a single population-based study covering all age groups between 0 and 19 years. The higher risk for childhood asthma in boys than in girls and the change to a female dominance at the age of 15–16 years are in accordance with studies that have addressed asthma occurrences in children at different ages [26, 27]. The age variation in the prevalence of anti-asthmatic drugs that we found is in accordance with the view that asthma is a heterogeneous disease that varies in expression with gender and age [28]. The early life peak followed by a decreasing prevalence until the age of 6–7 years probably reflects the importance of viral respiratory infections in bronchial obstruction in the youngest age groups, while allergic factors are relatively more important later in life. The change in gender ratios may be related to both gender differences in growth, immunology and age-dependent hormonal changes, but also to differences in exposure and susceptibility to environmental factors as well as the perception and reporting of respiratory symptoms [26, 29].
We chose to include only children and adolescents receiving reimbursed inhaled anti-asthmatics as this ensured that the doctor had considered the condition to be chronic and at least in need of 3 months of medication. Inhalation therapy as the method of choice in asthma therapy and also the use of a pressurised metered dose inhalator in preschool children are widely accepted in Norway. The preferential use of inhaled medication in the management of paediatric asthma now appears to be adopted by other European countries as well, such as the Netherlands [9]. The inclusion of children prescribed only mixtures with ephedrine or β2-agonist, without any other anti-asthmatics, as cases would have increased the prevalence to 9%. It is likely that the majority of these were preschool children treated for incidental, unspecific acute upper respiratory tract symptoms and infections and that few of them had a persistent and clinically important asthma. However, for small children, doctors may have set higher thresholds before prescribing the appropriate inhalation devices for aerosols compared to the use of mixtures.
The use of just bronchodilators may indicate the prevalence of mild asthma, while that of inhaled ICS alone or combined with inhaled β2-agonists may indicate the prevalence of moderate to severe asthma [13]. In our study, 75% of children treated with reimbursed, inhaled anti-asthmatics received glucocorticoids (ICS) alone or in combination with β2-agonists. Among these, a rather high proportion of children received fixed combinations of ICS and long-acting β2-agonists, which may indicate more severe asthma since (according to guidelines) fixed combinations should only be prescribed to patients with moderate to severe asthma after treatment with moderate doses of ICS has been tried without obtaining adequate control.
Any prevalence estimate of asthma will depend on how the asthma is defined, and no single definition of asthma is applicable to all studies [30]. Most epidemiological studies have only been able to assess asthma prevalence for one or a few age cohorts and in local populations that not necessarily represent the asthma prevalence in the total population. We argue here that the prevalence of inhaled anti-asthmatics dispensed at pharmacies to all Norwegians aged 0–19 may be a valid prevalence estimate for ongoing and clinical important asthma, showing that about 1 in 20 Norwegian children/adolescents have ongoing asthma. By using the results of this study as a starting point, we may create a cohort of children with asthma to be used for longitudinal population-based surveillance and research.
References
Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC (1998) The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet 351:1225–1232
Anderson HR, Ruggles R, Strachan DP, Austin JB, Burr M, Jeffs D, Standring P, Steriu A, Goulding R (2004) Trends in prevalence of symptoms of asthma, hay fever, and eczema in 12–14 year olds in the British Isles, 1995–2002: questionnaire survey. BMJ 328:1052–1053
Magnus P, Jaakkola JJ (1997) Secular trend in the occurrence of asthma among children and young adults: critical appraisal of repeated cross sectional surveys. BMJ. 314:1795–1799
Crane J, Mallol J, Beasley R, Stewart A, Asher MI (2003) Agreement between written and video questions for comparing asthma symptoms in ISAAC. Eur Respir J 21:455–461
Smeeton NC, Rona RJ, Oyarzun M, Diaz PV (2006) Agreement between responses to a standardized asthma questionnaire and a questionnaire following a demonstration of asthma symptoms in adults. Am J Epidemiol 163:384–391
Osborne ML, Vollmer WM, Johnson RE, Buist AS (1995) Use of an automated prescription database to identify individuals with asthma. J Clin Epidemiol 48:1393–1397
Kozyrskyj AL, Mustard CA, Becker AB (2004) Identifying children with persistent asthma from health care administrative records. Can Respir J 11:141–145
Lynd LD, Guh DP, Pare PD, Anis AH (2002) Patterns of inhaled asthma medication use: a 3-year longitudinal analysis of prescription claims data from British Columbia, Canada. Chest 122:1973–1981
de Vries TW, Tobi H, Schirm E, van den Berg P, Duiverman EJ, de Jong-van den Berg LT (2006) The gap between evidence-based medicine and daily practice in the management of paediatric asthma. A pharmacy-based population study from The Netherlands. Eur J Clin Pharmacol. 62:51–55
Furu K (2001) Drug utilisation in a public health perspective: Establishing a national prescription register in Norway. Norwegian J Epidemiol 11:55–60
WHO Collaborating Centre for Drug Statistics Methodology (2005) Guidelines for ATC classification and DDD assignment. Norwegian Institute of Public Health, Oslo, Norway
Haga A, Sverre JM (2002) Pricing and reimbursement of pharmaceuticals in Norway. Eur J Health Econ 3:215–220
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. NIH Publication No. 02–3659 Issued January, 1995 (updated 2002). Management Segment (Chapter 7): updated 2005 from the 2004 document. Available at: http://www.ginasthma.com
Wogelius P, Poulsen S, Sorensen HT (2005) Validity of parental-reported questionnaire data on Danish children’s use of asthma-drugs: a comparison with a population-based prescription database. Eur J Epidemiol 20:17–22
von Hertzen L, Haahtela T (2005) Signs of reversing trends in prevalence of asthma. Allergy 60:283–292
Naureckas ET, Dukic V, Bao X, Rathouz P (2005) Short-acting beta-agonist prescription fills as a marker for asthma morbidity. Chest 128:602–608
Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM (1993) Primary non-compliance with prescribed medication in primary care. BMJ 307:846–848
OECD Health Data (2005) A comparative analysis of 30 countries: 2005 edition OECD (Organisation for Economic Co-operation and Development). ISBN 9264008764
Pont LG, van der Werf GT, Denig P, Haaijer-Ruskamp FM (2002) Identifying general practice patients diagnosed with asthma and their exacerbation episodes from prescribing data. Eur J Clin Pharmacol 57:819–825
Selnes A, Nystad W, Bolle R, Lund E (2005) Diverging prevalence trends of atopic disorders in Norwegian children. Results from three cross-sectional studies. Allergy 60:894–899
Tollefsen E, Bjermer L, Langhammer A, Johnsen R, Holmen TL (2006) Adolescent respiratory symptoms-girls are at risk: the Young-HUNT study, Norway. Respir Med 100:471–476
Carlsen KCL, Haland G, Devulapalli CS, Munthe-Kaas M, Pettersen M, Granum B, Lovik M, Carlsen KH (2006) Asthma in every fifth child in Oslo, Norway: a 10-year follow up of a birth cohort study. Allergy 61:454–460
Roberts EM (2003) Does your child have asthma? Parent reports and medication use for pediatric asthma. Arch Pediatr Adolesc Med. 157:449–455
Nafstad P, Magnus P, Jaakkola JJ (2000) Early respiratory infections and childhood asthma. Pediatrics 106:e38
Nafstad P, Brunekreef B, Skrondal A, Nystad W (2005) Early respiratory infections, asthma, and allergy: 10-year follow-up of the Oslo Birth Cohort. Pediatrics 116:e255–e262
Osman M (2003) Therapeutic implications of sex differences in asthma and atopy. Arch Dis Child 88:587–590
Wright AL, Stern DA, Kauffmann F, Martinez FD (2006) Factors influencing gender differences in the diagnosis and treatment of asthma in childhood: The Tucson Children’s Respiratory Study. Pediatr Pulmonol 41:318–325
Stein RT, Martinez FD (2004) Asthma phenotypes in childhood: lessons from an epidemiological approach. Paediatr Respir Rev 5:155–161
Venn A, Lewis S, Cooper M, Hill J, Britton J (1998) Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. BMJ 316:1945–1946
Pekkanen J, Pearce N (1999) Defining asthma in epidemiological studies. Eur Respir J 14:951–957
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Furu, K., Skurtveit, S., Langhammer, A. et al. Use of anti-asthmatic medications as a proxy for prevalence of asthma in children and adolescents in Norway:a nationwide prescription database analysis. Eur J Clin Pharmacol 63, 693–698 (2007). https://doi.org/10.1007/s00228-007-0301-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0301-9