Abstract
Objective
During the past 30 years, various cardiovascular drugs have been implicated as causes of depression or suicide. Although the evidence for causal relationships has generally been conflicting, both β-blockers and angiotensin-converting-enzyme inhibitors (ACE-inhibitors) have been related to depression. Lipid-lowering therapies and calcium-channel blockers have also been linked to an increased risk of suicide. In this study, we investigated the possible association between the use of cardiovascular drugs and suicide using population-based register data.
Methods
We performed a nested case-control study in the county of Funen, Denmark, that consisted of 743 cases of completed suicide identified in a Death Registry for the period 1991–1998 and 14,860 age- and sex-matched controls. Information on previous drug use was retrieved from prescription data and the association between suicide and use of cardiovascular drugs was analysed by conditional logistic regression. Previous exposures to other drugs were used as proxies for potential confounding co-morbidities, including the use of psychotropic drugs to indicate psychiatric illness.
Results
The risk of suicide was not associated with current exposure to lipid-lowering drugs [odds ratio (OR): 1.21; 95% confidence interval (95% CI): 0.45–3.28), calcium-channel blockers (OR: 0.96; 95% CI: 0.63–1.48), β-blockers (OR: 0.76; 95% CI: 0.47–1.25) or ACE-inhibitors (OR: 1.11; 95% CI: 0.68–1.83). Suicide risk was associated with current angiotensin-receptor antagonist use (OR: 3.52; 95% CI: 1.33–9.30) based on five of the cases exposed.
Conclusion
With the exception of the imprecise risk associated with current use of angiotensin-receptor antagonists, the results from our study do not support the hypothesis that other cardiovascular drugs are associated with an increased the risk of suicide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the past 30 years, various cardiovascular drugs have been implicated as causes of depression or suicide [1]. Although the evidence for any causal relationship has generally been conflicting, both β-blockers [2, 3] and angiotensin-converting-enzyme inhibitors (ACE-inhibitors) [4, 5] have been related to depression. Lipid-lowering therapies [6] and calcium-channel blockers [7] have also been linked to an increased risk of suicide.
While various degrees of depression are relatively common and, consequently, fairly accessible to research, the infrequency of suicide makes it difficult to attain the power needed to appropriately investigate associations between drug exposure and this outcome. Depression is clearly associated with suicide, although the relationship may not always be as close as traditionally presumed [8]. Thus, findings from studies on depression may not readily be extrapolated to suicide. To date, there are only a limited number of studies on the association between cardiovascular drugs and suicide, and many of these involve only a few cases. A positive association between the use of calcium-channel blockers and suicide was found in a cohort study involving nine cases [7], but the results were later contradicted by a case-control study involving 38 cases [9]. In another cohort study involving 104 cases, researchers found a tendency for an increased risk of suicide among users of β-blockers with medium and high lipid solubility [10]. Yang et al. conducted a nested case-control study to determine whether lipid-lowering drugs (LLDs) are associated with depression and suicidal behaviour and found no increased risks [11]. Whereas this latter study involved 458 cases of newly diagnosed depression and 105 cases of suicidal behaviour, only eight cases of completed suicide were included.
With the aim of continuing the investigation into a possible association between the use of commonly used cardiovascular drugs and suicide, we have carried out a nested case-control study based on prescription data from 743 cases of completed suicide.
Methods
Study population and drug exposures
We carried out a nested case-control study in the county of Funen (465,000 inhabitants; 9% of the Danish population) based on information from The Danish Registry of Cause of Death (RCD) and a prescription registry, The Odense University Pharmacoepidemiological Database (OPED). Simple and correct linkage between the registries was ensured by the Central Person Register (CPR) number, which is a 10-digit code unique to each Danish citizen. All subjects who committed suicide (ICD-8 diagnoses: E950–959 and ICD-10 diagnoses X60–84, Y87) in the County of Funen during the period from 1991 to 1998 were identified in the RCD. This register provides data on the residence of the deceased (municipality), date of death, ICD-8 or ICD-10 diagnosis referring to suicide method and CPR number. The residence history of all inhabitants of Funen county, regardless of medication status, is maintained and continuously updated as part of OPED. This feature enabled us to select population control subjects in a nested design. For each case of completed suicide, we randomly chose 20 control subjects who were alive and residing in Funen on the date of the suicide (index date). Control subjects were matched for age (within 1 year) and sex, and their index date was identical to the suicide date of the corresponding case. All prescription records prior to the index dates were extracted from OPED. For each prescription, the registry includes information on the CPR number, the date the prescription was redeemed and the brand, quantity, and form of the drug. All drugs are classified according to the anatomic therapeutic chemical (ATC) system. Information on the prescribed dosing and indication is not available.
Drug exposures of primary interest were the use of statins, LLDs (statins, fibrates, bile acid sequestrants and nicotinic acid and derivatives), calcium-channel blockers, β-blockers (categorized according to their lipid solubility), ACE-inhibitors and angiotensin-receptor antagonists. Based on the prescription date, exposure of the study subjects to the drugs of interest was categorized as current (last prescription = 89 days before the index date) or past (last prescription = 90 days before the index date). As proxies for potential confounding co-morbidities, we used the recording of at least one prescription of thiazides, loop-diuretics, digoxin, nitrates, low-dose acetylsalicylic acid, platelet inhibitors, inhaled β2-agonists, inhaled corticosteroids, inhaled anticholinergics, antidiabetics, oral glucocorticosteroids, thyroid hormones, anti-epileptics, dopaminergic agents and antimigraine drugs within 1 year of the index date. Since prescriptions for most of these drugs are associated with chronic diseases, a minimum of one prescription was considered to indicate the presence of co-morbidity. With regard to antipsychotics, lithium, antidepressants (selective serotonin reuptake inhibitors and tricyclic antidepressants) and drugs used for alcohol dependence, “ever use” was chosen to indicate a history of psychiatric illness in a subject.
Statistical analysis
Multivariable conditional logistic regression was used to estimate odds ratios (ORs) for associations between suicide and treatment with various cardiovascular drugs. Current and past use was compared to never use. All potential confounding variables that had a p < 0.2 in univariate analyses were entered into a multivariate model, and in order to define the final model, a stepwise backward procedure was used to eliminate variables that became insignificant (p ≥ 0.05).
We performed two analyses with restricted data sets in order to assess possible bias and misclassification. Depression may be an intermediate step in the causal pathway between use of a cardiovascular drug and suicide, and adjusting for antidepressant or other psychotropic drug use may therefore introduce a bias towards the null. To rule out this kind of bias, we did a supplementary analysis that resulted in the exclusion of all subjects with ever use of psychotropic drugs. Non-differential misclassification of drug exposure due to incomplete coverage of the prescription data during the first years could also lead to bias towards the null. To assess if such bias was present, we repeated the analysis, limiting the data set to subjects with index dates after 1 January 1992 and at least 1 year of complete observation. All analyses were performed with STATA ver. 8.0 (StataCorp, College Station, Tex.).
Results
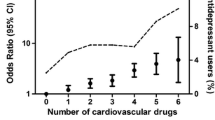
The study population comprised 15,603 subjects, including 743 cases and 14,860 controls. The distribution of patient characteristics for the cases and their matched controls is presented in Table 1. Among the cases, there was a predominance of males (68.2%) and the mean (±SD) ages for males and females were 53.4 (±18.6) and 58.1 (±17.6) years, respectively. Because of the matching procedure, the age and sex distributions among case and controls were identical. Compared with controls, cases differed most prominently with respect to use of antidiabetics and anti-epileptics in the last year, and ever use of psychotropic drugs (i.e. antidepressants, antipsychotics, lithium and drugs used for alcohol dependence).
The results of the multivariate analyses for various exposures are given in Table 2. Apart from the current use of angiotensin-receptor antagonists, none of the cardiovascular drugs we investigated appeared to be associated with an increased risk of suicide. We observed no trend of increasing risk of suicide with increasing degrees of lipid solubility of the β-blockers. Compared to crude ORs, adjustment primarily affected the OR for use of β-blockers with high lipid solubility, where the estimate changed from over unity to below unity.
The first restricted analysis, which excluded subjects with a history of psychotropic drug use, did not unravel any new significant associations. The OR (95% CI) for current use of calcium-channel blockers was 0.58 (0.27–1.26), of β-blockers, 0.68 (0.30–1.55), of ACE-inhibitors, 1.20 (0.62–2.33) and of angiotensin-receptor antagonists, 3.32 (0.93–11.8), all of which were adjusted for antidiabetic and anti-epileptic drug use as in the primary analysis. There were too few exposed cases to estimate the OR for LLDs and to differentiate among β-blockers with different lipid solubility.
The second restricted analysis, which excluded subjects with possible incomplete information about drug use, produced results very similar to the primary analysis (not shown).
Discussion
In the nested case-control study we conducted, the current use of a range of different cardiovascular drugs was not associated with an increased risk of suicide. This is the largest published study of cardiovascular drug use and completed suicide. Hence, our study provides strong support for the safety of these drugs with respect to this outcome.
Given the general coverage of the population-based registries used in our study, it seems reasonable to assume that the majority of cases were identified and that the controls represent a true random sample from the source population. Studies of suicide cases based on the same registers have previously been published [12, 13]. Although data validity is considered to be high, a diagnosis of suicide can be ambiguous, and some non-suicide deaths may have been included as cases leading to an underestimation of associations of risk in our study. With respect to drug exposures, since estimates are based on prescriptions actually redeemed at a pharmacy, our study is likely to have less misclassification in comparison with studies based on medical records of prescriptions. Non-differential misclassification of drug exposure due to incomplete coverage of the prescription data during the first years was not a problem according to our restricted analysis. However, one drawback of the database we used is that it does not contain information on benzodiazepine prescriptions because these are not reimbursed. Also, it should be noted that our study is not restricted to incident users and that it primarily focuses on current and not cumulative exposures.
Similar to results reported for earlier studies, full control for possible confounding variables, in particular in terms of the underlying disease and co-morbidities, has probably not been achieved. Apart from the matched variables (calendar time, age and sex), only potential confounders associated with a prescription could be adjusted for. While several variables associated with psychiatric co-morbidities were included in the statistical model, most cardiovascular covariates associated with cardiovascular disease (e.g. digoxin, loop-diuretics and nitrates) did not meet the criteria for inclusion. Restricting the analysis to non-users of psychotropic drugs produced results similar to those of the primary analysis, thus ruling out that adjustment for antidepressant or other psychotropic drug use introduced any important bias. Because information was not available for other potential confounders, such as body mass index (BMI), lipid levels, physical activity, psychosocial stress or smoking, we were not able to adjust for these. However, the lack of control for most of these covariates would not be expected to cause an underestimation of the effect of cardiovascular drug exposure. Surprisingly, the use of antidiabetics, a factor traditionally considered to be associated with increased risk of cardiovascular disease, was inversely associated with suicide.
Even if some of our estimates are imprecise, our results seem to corroborate the reassuring findings of two recent observational studies investigating the use of LLDs and potential adverse psychological effects. In a study on the effect of long-term statin use on psychological well-being, an association with reduced risk of anxiety, depression and hostility was observed [14]. Yang et al. also did not find an association between the use of statins or other LLDs and depression or suicide [11]. On the contrary, compared with hyperlipidemic nonuse, a reduced risk of depression was observed among current users of statins. These researchers also excluded patients with risk factors for the outcomes of interest from the study population. Overall, the numbers of cases diagnosed with depression or suicidal behaviour were reasonably large; however, the study only included eight cases of completed suicide. It is worth noting that, in comparison to our study on completed suicides and involving a minority of women (31.8%), in the study by Yang et al. there was a predominance of women (61.9%) among patients with suicidal behaviour.
Based on the results of a cross-sectional ecological study and a population-based cohort study, Lindberg et al. concluded that the use of calcium channel blockers may increase the risk of suicide [7]. In the ensuing debate, the methodology used was criticized on several points [15–17], and later studies could not find this association [9, 10]. In this context, our results seem to be in keeping with previous negative studies. In terms of β-blockers and ACE-inhibitors, studies have primarily investigated the risk of depression. The degree of lipid solubility of a β-blocker has been suggested to be of importance in relation to potential adverse effects on the central nervous system [18]. Indeed, in a cohort study involving 104 suicides, there was a trend indicating a positive correlation between the risk of suicide and the degree of lipid solubility of the used β-blocker [10]. In our study, the adjusted ORs for current use of various β-blockers did not reveal a similar trend. It should be noted that propranolol, a widely used and highly lipid-soluble β-blocker, has many indications, such as migraine and tremor. Consequently, for this particular drug, there is a substantial risk of generating spurious associations through “confounding by indication”. The change in direction, when the OR for high lipid-solubility β-blockers is adjusted, could be a reflection of such a relationship. On the other hand, our negative finding with respect to ACE-inhibitors is completely in accordance with the study by Sorensen et al. [10]. Lastly, we unexpectedly found that current use of an angiotensin-receptor blocker appeared to be associated with an increased risk of suicide. Although there is one report of a case of suicide attempt associated with treatment with valsartan and hydrochlorthiazide [19], in the light of the low number of exposed cases and losartan’s purported antidepressive properties [20], we believe that the association should be cautiously interpreted.
A balanced assessment of a treatment must always take into account both potential benefits and risks. Hence, negative findings in observational studies involving large populations and commonly used drugs are of importance to public health. However, reassuring findings do not always rule out the possibility of the existence of vulnerable subgroups of patients [8, 21] or of late effects as consequence of a high cumulative exposure. In conclusion, the findings in our nested case-control study do not support the hypotheses that the current use of lipid-lowering drugs, calcium-channel blockers, β-blockers or ACE-inhibitors are associated with an increased risk of suicide.
References
Jepsen P, Johnsen SP, Sorensen HT (2003) Risk of suicide in users of cardiovascular drugs: a review of the epidemiological evidence. Am J Cardiovasc Drugs 3:163–167
Patten SB (1990) Propranolol and depression: evidence from the antihypertensive trials. Can J Psychiatry 35:257–259
Rathmann W, Haastert B, Roseman JM, Giani G (1999) Cardiovascular drug prescriptions and risk of depression in diabetic patients. J Clin Epidemiol 11:1103–1109
Hallas J (1996) Evidence of depression provoked by cardiovascular medication: a prescription sequence symmetry analysis. Epidemiology 7:478–484
Patten SB, Williams JV, Love EJ (1996) Case-control studies of cardiovascular medications as risk factors for clinically diagnosed depressive disorders in a hospitalized population. Can J Psychiatry 41:469–476
Muldoon MF, Manuck SB, Matthews KA (1990) Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. Br Med J 301:309–314
Lindberg G, Bingefors K, Ranstam J, Rastam L, Melander A (1998) Use of calcium channel blockers and risk of suicide: ecological findings confirmed in population based cohort study. Br Med J 7:741–745
Brunner J, Parhofer KG, Schwandt P, Bronisch T (2002) Cholesterol, essential fatty acids, and suicide. Pharmacopsychiatry 35:1–5
Gasse C, Derby LE, Vasilakis C, Jick H (2000) Risk of suicide among users of calcium channel blockers: population based, nested case-control study. Br Med J 320:1251
Sorensen HT, Mellemkjaer L, Olsen JH (2001) Risk of suicide in users of beta-adrenoceptor blockers, calcium channel blockers and angiotensin converting enzyme inhibitors. Br J Clin Pharmacol 52:313–318
Yang CC, Jick SS, Jick H (2003) Lipid-lowering drugs and the risk of depression and suicidal behavior. Arch Intern Med 163:1926–1932
Andersen UA, Andersen M, Rosholm JU, Gram LF (2000) Contacts to the health care system prior to suicide: a comprehensive analysis using registers for general and psychiatric hospital admissions, contacts to general practitioners and practising specialists and drug prescriptions. Acta Psychiatr Scand 102:126–134
Andersen UA, Andersen M, Rosholm JU, Gram LF (2001) Psychopharmacological treatment and psychiatric morbidity in 390 cases of suicide with special focus on affective disorders. Acta Psychiatr Scand 104:458–465
Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM (2003) Long-term statin use and psychological well-being. J Am Coll Cardiol 42:690–697
Bergman U, Isacsson G (1998) Use of calcium channel blockers and risk of suicide. Independent studies are needed before causality is established. Br Med J 317:1076
Chen YT, Makuch RW (1998) Use of calcium channel blockers and risk of suicide. Prescriptions for particular drug are influenced by numerous factors. Br Med J 317:1077
Wiholm BE, Sundstrom A, Alfredsson L (1998) Use of calcium channel blockers and risk of suicide. Drug prescriptions over longer period should have been followed up. Br Med J 317:1076–1077
Conant J, Engler R, Janowsky D, Maisel A, Gilpin E, LeWinter M (1989) Central nervous system side effects of beta-adrenergic blocking agents with high and low lipid solubility. J Cardiovasc Pharmacol 13:656–661
Ullrich H, Passenberg P, Agelink MW (2003) Episodes of depression with attempted suicide after taking valsartan with hydrochlorothiazide. Dtsch Med Wochenschr 128:2534–2536
Gard PR, Mandy A, Sutcliffe MA (1999) Evidence of a possible role of altered angiotensin function in the treatment, but not etiology, of depression. Biol Psychiatry 45:1030–1034
Golomb BA, Kane T, Dimsdale JE (2004) Severe irritability associated with statin cholesterol-lowering drugs. Q J Med 97:229–235
Acknowledgements
The study was supported by the Danish Medical Research Council (grant no. 22-02-0395).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Callréus, T., Agerskov Andersen, U., Hallas, J. et al. Cardiovascular drugs and the risk of suicide: a nested case-control study. Eur J Clin Pharmacol 63, 591–596 (2007). https://doi.org/10.1007/s00228-007-0293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0293-5