Abstract
Objective
Although alpha-blockers are effective in lowering blood pressure, they may increase heart rate, an unwanted effect that could negatively affect outcome. However, the alpha-blocker urapidil might not increase heart rate due to its additional effect on 5-HT1A receptors. Therefore, we compared the effects of urapidil on heart rate with those of another alpha-blocker, doxazosin.
Methods
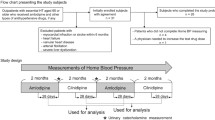
We performed a randomised, double-blind, placebo-controlled, cross-over study in 12 healthy males who received single oral doses of 60 mg urapidil, 4 mg doxazosin and placebo. Four hours following drug intake, heart rate and blood pressure were measured at rest and during exercise.
Results
Both doxazosin and urapidil decreased blood pressure to the same extent. Compared to placebo, resting heart rate was significantly increased by doxazosin (+25%, P < 0.05) but not by urapidil (+12%, n.s.). Resting heart rate with doxazosin was significantly higher than with urapidil (P < 0.05). Similarly, the rate pressure product (RPP) at rest was increased by doxazosin (+17%, P < 0.05) but not by urapidil (+6%, n.s.).
Conclusions
We conclude that the increase in heart rate caused by urapidil is less pronounced than that with doxazosin, a property that might favour urapidil in the treatment of arterial hypertension. In addition, only doxazosin (but not urapidil) increased the RPP at rest, a finding that might be helpful to explain why this drug was never shown to improve outcome in the treatment of arterial hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alpha-blockers are effective in the treatment of arterial hypertension and have been recommended in recent guidelines with certain restrictions [1, 2]. However, it has been shown that the alpha-blocker doxazosin may increase heart rate [3], an unwanted effect, and the doxazosin arm of the ALLHAT trial was discontinued prematurely since doxazosin (compared to chlorthalidone) caused a significant increase in heart failure, stroke, and combined cardiovascular disease [4].
Urapidil is a peripheral postsynaptic alpha-adrenergic antagonist with additional central stimulating effects at 5-HT1A receptors. It has been postulated that urapidil does not increase heart rate due to this effect [5]. However, it has never been shown in a direct comparison that the influence of urapidil on heart rate might differ from that of other alpha-blockers.
Therefore, we performed a randomised, double-blind, placebo-controlled, cross-over study comparing the effects of urapidil, doxazosin and placebo on heart rate and blood pressure in healthy males both at rest and during exercise in order to determine whether or not there might be differences in the effects of urapidil and doxazosin on heart rate.
Methods
The study was performed according to a randomised, double-blind, placebo-controlled, cross-over protocol in 12 healthy males, age 25 ± 4 years, height 179 ± 7 cm, body weight 76 ± 9 kg. Subjects received single oral doses of 60 mg urapidil, 4 mg doxazosin (one-half of the maximum daily doses of these drugs recommended for arterial hypertension in order to obtain similar effects on blood pressure) or placebo together with 50 ml of water in the morning following an overnight fast. The investigations were separated by drug-free intervals of at least 4 days. Four hours after drug intake, exercise on a bicycle ergometer (mean 158 ± 15 W, i.e., 70% of mean individual work load) was performed for 10 min, followed by 15 min of recovery in a supine position. Both heart rate (by continuous ECG monitoring) and blood pressure (by sphygmomanometry) were measured at rest immediately prior to exercise, during the last minute of exercise, and during the last minute of the following 15 min of recovery.
Results are given as means ± SD unless indicated otherwise. Significances of differences were calculated by repeated measures ANOVA (repeated measures ANOVA on ranks when applicable), post-hoc analyses were performed using the Student-Newman-Keuls test, and P < 0.05 was considered statistically significant.
We hypothesized a minimum detectable difference of 0.15, an expected standard deviation of 0.1, a number of groups of 3, a desired power of 0.9 and an alpha of 0.05, thus giving a required sample size of 12 subjects, i.e., the number we used in the present study. Using these data, the present study had a calculated power of 0.903 to detect differences.
The investigation conformed to the principles outlined in the Declaration of Helsinki, was approved by the Ethics Committee of the Medical University of Graz, Austria, and all participants gave written informed consent.
Results
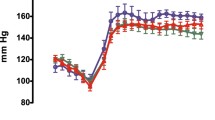
Haemodynamic results are given in Table 1. Both urapidil and doxazosin reduced systolic blood pressure significantly and to the same extent. At rest, doxazosin significantly increased heart rate whereas urapidil did not, and heart rate with urapidil was significantly lower than with doxazosin (Fig. 1). Furthermore, doxazosin significantly increased the rate pressure product (RPP) (i.e., the product of heart rate and systolic blood pressure, also called the “double product”) at rest and at recovery, whereas the RPP was not affected by urapidil, and the RPP at recovery obtained with urapidil was significantly (P < 0.05) lower than that with doxazosin.
Systolic blood pressure (upper panel) and heart rate (lower panel) obtained at rest 4 h following intake of 4 mg doxazosin, placebo, or 60 mg urapidil. Effects of doxazosin on heart rate appear more pronounced than those on systolic blood pressure, and the increase in heart rate with doxazosin is significantly more pronounced than that with urapidil (n = 12). n.s. Not significant
Discussion
Urapidil and doxazosin were equally effective in lowering blood pressure, and both drugs tended to increase heart rate. However, doxazosin significantly increased heart rate at rest, during exercise and at recovery, whereas urapidil did not, with the effect of urapidil on heart rate being significantly less pronounced than that of doxazosin both at rest and during exercise. In addition, the effect of urapidil on heart rate at rest failed to reach statistical significance compared to placebo, whereas the increasing effect of doxazosin on heart rate appeared more pronounced than its lowering effect on systolic blood pressure. Thus, our data provide evidence that urapidil increases heart rate significantly less than doxazosin. This difference might be caused by an agonist action of urapidil on 5-HT1A receptors, an effect lacking with doxazosin. However, this clinical study cannot determine whether this effect of urapidil on 5-HT1A receptors is the one and only reason for these different effects of urapidil and doxazosin on heart rate.
It is well known that the levels of both blood pressure [1, 2] and heart rate [6–12] are directly correlated with morbidity and mortality. In this context, the present study revealed an additional finding that might deserve further attention, namely the fact that doxazosin significantly increased the rate pressure product (RPP), both at rest and at recovery, although the drug significantly lowered systolic blood pressure. In contrast, urapidil did not significantly affect the RPP, although the RPP showed a slight tendency to increase rather than to decrease. Obviously, the tendency of doxazosin to increase heart rate was more pronounced than its tendency to decrease blood pressure; the potentially harmful increase in heart rate might outweigh the potentially beneficial decrease in blood pressure. This fact might explain why doxazosin was never shown to decrease morbidity and mortality in patients with arterial hypertension despite its excellent ability to lower blood pressure—this behaviour is similar to that repeatedly discussed with calcium antagonists of the dihydropyridine type [13–16]. Furthermore, this finding might help to explain (at least in part) why doxazosin may increase the incidence of heart failure and stroke in comparison to chlorthalidone as shown in the ALLHAT trial [4].
It has to be emphasised that the present study is a trial in the field of basic clinical cardiovascular pharmacology investigating the effects of single doses of urapidil and doxazosin on heart rate in healthy subjects; this is its main limitation. However, the authors believe that, based on the present results, a study on the effects of long-term treatment with urapidil and doxazosin on heart rate, RPP and clinical outcome in patients with arterial hypertension is warranted in order to find out whether or not the findings of the present study carried out in healthy subjects are the same in patients with arterial hypertension.
In conclusion, our data show that the increasing effect of urapidil on heart rate and RPP is significantly less pronounced than that of doxazosin, a property which might be beneficial in the treatment of arterial hypertension with alpha-blockers.
According to these results, we hypothesize that understanding the influence of a drug on RPP might be helpful for predicting outcome in antihypertensive drug therapy. Unfortunately, it is actually impossible even to speculate on this hypothesis since the effects of the drugs on heart rate are not given in most outcome trials in arterial hypertension. Therefore, the authors suggest the results of large-scale clinical trials in patients with arterial hypertension be re-analysed in order to determine the predictive value of the influence of antihypertensive drugs on resting heart rate and RPP with regard to morbidity and mortality in order to further optimise drug treatment in arterial hypertension.
References
European Society of Hypertension Guidelines Committee (2003) 2003 European Society of Hypertension—European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertension 21:1011–1053
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ, The National High Blood Pressure Education Program Coordinating Committee (JNC VII) (2003) Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42:1206–1252
Stoschitzky K, Koshucharova G, Zweiker R, Lercher P, Maier R, Watzinger N, Kraxner W, Klein W, Donnerer J (2003) Different effects of propranolol, bisoprolol, carvedilol and doxazosin on heart rate, blood pressure, and plasma concentrations of epinephrine and norepinephrine. J Clin Basic Cardiol 6:69–72
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) (2000) Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlortalidone. JAMA 283:1967–1975
Dooley M, Goa KL (1998) Urapidil: a reappraisal of its use in the management of hypertension. Drugs 56:929–955
Palatini P, Julius S (1997) Heart rate and the cardiovascular risk. J Hypertension 15:3–17
Levine HJ (1997) Rest heart rate and life expectancy. J Am Coll Cardiol 30:1104–1106
Palatini P, Casiglia E, Julius S, Pessina AC (1999) High heart rate-a risk factor for cardiovascular death in elderly men. Arch Intern Med 159:585–592
Palatini P, Thijs L, Staessen JA, Fagard RH, Bulpitt CJ, Clement DL, de Leeuw PW, Jaaskivi M, Leonetti G, Nachev C, O’Brien ET, Parati G, Rodicio JL, Roman E, Sarti C, Tuomilehto J, for the Syst-Eur Trial Investigators (2002) Predictive value of clinic and ambulatory heart rate for mortality in elderly subjects with systolic hypertension. Arch Intern Med 162:2313–2321
Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetière P (2005) Heart-rate profile during exercise as a predictor of sudden death. New Engl J Med 352:1951–1958
Palatini P (2005) Heart rate: a strong predictor of mortality in subjects with coronary artery disease. Eur Heart J 26:943–945
Diaz A, Bourassa MG, Guertin MC, Tardif JC (2005) Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J 26:967–974
Furberg CD, Psaty BM, Meyer JV (1995) Dose-related increase in mortality in patients with coronary heart disease. Circulation 92:1068–1073
Pahor M, Guralnick JM, Corti MC, Foley DJ, Carbonin P, Havlik RJ (1995) Long-term survival and use of antihypertensive medications in older persons. J Am Geriatric Soc 43:1191–1197
Epstein M (1996) Calcium antagonists: still appropriate as first line antihypertensive agents. Am J Hypertens 9:110–121
Furberg CD, Psaty BM (1996) Calcium antagonists: not appropriate as first line antihypertensive agents. Am J Hypertens 9:122–125
Acknowledgements
The authors acknowledge the support of this study by an unrestricted scientific grant of Altana Pharma, Vienna, Austria. We also wish to thank Lannacher Heilmittel GmbH, Lannach, Austria, for providing doxazosin.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stoschitzky, K., Stoschitzky, G., Wonisch, M. et al. Differential effects of urapidil and doxazosin on heart rate. Eur J Clin Pharmacol 63, 259–262 (2007). https://doi.org/10.1007/s00228-006-0256-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0256-2