Abstract
Objective
Rifampicin greatly reduces the plasma concentrations of many drugs. Our aim was to characterise the inducibility of cytochrome P450 (CYP) 1A2 by rifampicin, using tizanidine and caffeine as probe drugs for presystemic and systemic CYP1A2-mediated metabolism.
Methods
In a randomised, 2-phase crossover study, ten healthy volunteers were given a 5-day pretreatment with 600 mg rifampicin or placebo once daily. On day 6, a single 4-mg dose of tizanidine was administered orally. Plasma and urine concentrations of parent tizanidine and several of its metabolites (M-3, M-4, M-5, M-9, M-10) and pharmacodynamic variables were measured up to 24 h. A caffeine test was performed in both phases.
Results
Rifampicin moderately reduced the peak plasma concentration (by 51%; P=0.002) and area under the plasma concentration-time curve [AUC(0–∞)] (by 54%; P=0.009) of parent tizanidine, and had no effect on its half-life. The tizanidine/M-3 and tizanidine/M-4 AUC(0–∞) ratios were slightly (by 30%; P=0.014; and by 38%; P=0.007) decreased by rifampicin. Also, the excretion of metabolites M-3, M-4 and M-5 into urine was reduced (P<0.005), but that of M-10 was increased (P=0.008) by rifampicin. Rifampicin reduced the tizanidine/M-10 ratio (by 55%; P=0.047) but had no significant effect on the other tizanidine/metabolite ratios in urine. The caffeine/paraxanthine ratio was reduced by 23% (P=0.081) by rifampicin. The effect of rifampicin on the caffeine/paraxanthine ratio correlated significantly with the effect of rifampicin on, for example, the AUC(0–∞) of tizanidine and the tizanidine/M-3 AUC(0–∞) ratio. The pharmacodynamic effects of tizanidine were reduced by rifampicin.
Conclusions
Rifampicin moderately decreases the plasma concentrations of tizanidine. The strong inducing effects of rifampicin on other CYP enzymes, e.g. CYP3A4, may have contributed to the findings, and the inducibility of CYP1A2-mediated presystemic (tizanidine) and systemic (tizanidine, caffeine) metabolism by rifampicin is weak at the most. Compared to CYP3A4 substrate drugs, substrates of CYP1A2 are much less susceptible to drug interactions caused by enzyme inducers of the rifampicin type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The rifamycin antibiotic rifampicin is a potent inducer of many drug-metabolising enzymes and transport proteins [1–3]. In particular, it can greatly (more than 10-fold) reduce the plasma concentrations and effects of drugs with significant presystemic metabolism, such as the cytochrome P450 3A4 (CYP3A4) substrates midazolam [4], triazolam [5], buspirone [6] and simvastatin [7]. Rifampicin also induces the expression of some drug transporters, e.g. the efflux transporters P-glycoprotein [8] and canalicular multispecific organic anion transporter (cMOAT, or MRP2) [9].
There have been only a few studies on the possible inducing effect of rifampicin on CYP1A2 in vivo. Rifampicin has been shown to modestly reduce the area under the concentration-time curve (AUC) of orally administered theophylline (by 18–45%) [3, 10, 11] and caffeine (by about 40%) [12, 13], and that of intravenously administered ropivacaine (by 52% in nonsmokers and by 38% in smokers) [14]. However, theophylline, caffeine and ropivacaine are metabolised to some extent also by other enzymes, including CYP2C9, CYP2E1 and CYP3A4, and theophylline is a substrate for organic anion transporter 2 [15–25]. CYP3A4 can be especially strongly induced by rifampicin; since the basic mechanisms of regulation and induction of CYP1A2 differ from those of CYP3A4 [26, 27], the inducibility of CYP1A2 by rifampicin in humans still remains uncertain. Moreover, the studied CYP1A2 substrates are low clearance drugs with no significant presystemic metabolism, and the effect of rifampicin on the pharmacokinetics of orally administered probe drugs, which have a significant CYP1A2 mediated presystemic metabolism, is not known.
Caffeine has been used widely as an in vivo probe of hepatic CYP1A2 activity [28–31]. Different caffeine-based indices, e.g. the ratio of caffeine and paraxanthine in plasma, reflect mainly systemic elimination by CYP1A2 [32]. Tizanidine, a centrally acting skeletal muscle relaxant, is eliminated from the body principally by CYP1A2-mediated biotransformation into several metabolites (Fig. 1) [33–35]. However, tizanidine differs pharmacokinetically from caffeine by its extensive presystemic metabolism and shorter elimination half-life [32, 33, 35]. Fluvoxamine and ciprofloxacin, inhibitors of CYP1A2 [36, 37], strongly increase the plasma concentrations and effects of tizanidine in vivo [35, 38]. Accordingly, tizanidine is a very sensitive CYP1A2 probe drug, which can be used to measure presystemic CYP1A2 mediated metabolism in humans.
Metabolic pathways of tizanidine according to Koch et al. 1989 [33]
In order to study the inducibility of presystemic and systemic CYP1A2-mediated metabolism by rifampicin in humans, we have investigated the effect of rifampicin on the pharmacokinetics and metabolite profile of tizanidine, and whether these effects parallel changes in the caffeine test. To this end, a carefully controlled rifampicin-tizanidine interaction study was conducted in healthy subjects.
Methods
Subjects
Ten healthy volunteers (six men and four women; age range 19–25 years; weight range 50–85 kg) participated in the study after giving written informed consent (Table 1). The volunteers were ascertained to be healthy by medical history, physical examination and routine laboratory tests before entering the study. For safety reasons, subjects with a systolic blood pressure lower than 110 mmHg were excluded from the study. None of the subjects were tobacco smokers and none used oral contraceptives or other continuous medication. The sample size was chosen so that a possible clinically significant pharmacokinetic drug interaction can be verified statistically without the use of an unnecessarily large group of healthy subjects. The number of subjects was estimated to be sufficient to detect a 30% change in the AUC(0–∞) of tizanidine with a power of 80% (alpha-level 5%).
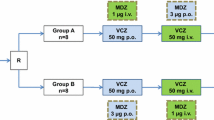
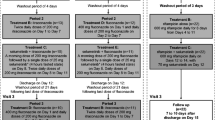
Study design
The study protocol was approved by the Ethics Committee for Studies in Healthy Subjects of the Hospital District of Helsinki and Uusimaa, and the Finnish National Agency for Medicines. A randomised, 2-phase crossover study with a washout period of 4 weeks was carried out. The volunteers received 600 mg rifampicin (one Rimapen 600 mg tablet; Orion Pharma, Espoo, Finland), or placebo once daily at 1600 hours for 5 days. On day 6, after an overnight fast, a single oral dose of 4 mg tizanidine (one Sirdalud 4 mg tablet; Novartis Pharma, Wehr, Germany) was administered with 150 ml water at 0900 hours. A standard meal was served 4 and 7 hours after tizanidine administration. Drinking of grapefruit juice and tobacco smoking were not allowed for 1 week before each study day. Alcohol and drinks containing caffeine were not permitted on the study days.
An oral caffeine test was performed on the 5th day of the pretreatment during both phases [28–31]. The subjects ingested 100 mg caffeine (one Cofi-Tabs 100 mg tablet; Vitabalans, Hämeenlinna, Finland) at 0900 hours, after having abstained from intake of caffeine for at least 18 h, and a blood sample for analysis of plasma caffeine and paraxanthine (1,7-dimethylxanthine) was taken from each subject 6 h after caffeine intake.
The subjects were under direct, close medical supervision for 12 h after administration of tizanidine. Fluids for intravenous infusion were available for immediate use, but were not needed.
Sampling
On the days of tizanidine administration, a forearm vein of each subject was cannulated with a plastic cannula and kept patent with an obturator. Timed blood samples were drawn before the administration of tizanidine and at 20, 40, 60 and 90 min and 2, 3, 4, 5, 7, 9, 12 and 24 h later. Blood samples (10 ml each) were taken into ethylenediaminetetra-acetic acid containing tubes. Plasma was separated within 30 min. Urine was collected cumulatively in two fractions: 0–12 and 12–24 h. Urine aliquots and plasma were stored at −70°C until analysis.
Drug concentrations in plasma and urine
Plasma and urine tizanidine and metabolite (M) concentrations were quantified by use of an API 2000 liquid chromatography-tandem mass spectrometry system (MDS Sciex, Toronto, Ontario, Canada). Chromatography was performed on an XTerra RP C18 column (3.9×100 mm; Waters, Milford, Mass) using gradient elution. The mobile phase consisted of 10 mM ammonium acetate (pH 9.5, adjusted with 25% ammonia solution) and acetonitrile. The mass spectrometer was operated in the atmospheric pressure chemical ionisation (APCI) mode with positive ion detection. The ion transitions monitored were mass-to-charge ratio (m/z) 254 to m/z 44 for tizanidine, m/z 268 to m/z 211 for M-3, m/z 228 to m/z 211 for M-4, m/z 252 to m/z 216 for M-5, m/z 415 to m/z 286 for M-9, m/z 288 to m/z 188 for M-10, and m/z 230 to m/z 44 for the internal standard, clonidine. These transitions represent the product ion of the [M+H]+ ion. The limit of quantification for tizanidine was 0.05 ng/ml and the day-to-day coefficient of variation (CV) was 17.5% at 0.1 ng/ml, 7.3% at 1.2 ng/ml and 13.7% at 12.8 ng/ml (n=5). A signal to noise ratio of 10:1 was used as the limit of detection for tizanidine metabolites, and their concentrations are given in arbitrary units relative to the ratio of the peak height of the metabolite to the peak height of the internal standard. The detector response for each metabolite was confirmed to be linear over the relevant concentration range by means of sample dilution. Rifampicin did not interfere with the determinations.
Plasma caffeine and paraxanthine concentrations were determined by HPLC, with β-OH-ethyltheophylline used as the internal standard [39, 40]. The day-to-day CV of caffeine and paraxanthine was less than 6% at relevant concentrations.
Pharmacokinetics
The pharmacokinetics of tizanidine, and metabolites 3 and 4, were characterised by peak concentration in plasma (C max), time to C max (t max), area under the plasma concentration-time curve from 0 to infinity [AUC(0–∞)], and elimination half-life (t ½) using non-compartmental methods as described earlier [35, 38]. In addition, the amount of tizanidine and its metabolites excreted into urine within 24 h (Ae) were calculated. The renal clearance (Clrenal) of tizanidine was calculated as Clrenal = Ae/AUC(0–24).
Pharmacodynamics
Systolic and diastolic blood pressures, heart rate, subjective drowsiness, subjective overall drug effect and the digit symbol substitution test (DSST) were assessed before administration of tizanidine and immediately after each blood sampling, as described earlier [35, 38]. For each pharmacodynamic variable, the area under the effect versus time curve from 0 to 12 h [AUC(0–12 h)] was calculated by use of the trapezoidal rule. In addition, the maximum responses in each pharmacodynamic variable were recorded.
Statistical analysis
Results are expressed as mean values±standard deviation (SD) in the tables and text and, for clarity, as mean values±standard error of the mean (SEM) in the figures. The pharmacokinetic and pharmacodynamic variables and the caffeine/paraxanthine ratio during the placebo and rifampicin phase were compared by repeated-measures ANOVA with treatment sequence as a factor or, in the case of t max with the Wilcoxon signed-rank test. For all variables except t max, 95% confidence intervals (CI) were calculated on the mean differences between the placebo and rifampicin phase. The Pearson correlation coefficient was used to investigate possible relationships of the pharmacokinetic variables of tizanidine, the tizanidine/metabolite AUC(0–∞) ratios and the tizanidine/metabolite urinary excretion (Ae) ratios with the caffeine/paraxanthine ratio during the placebo phase and the possible relationships between their changes caused by rifampicin. All the data were analysed with the statistical program Systat for Windows, version 6.0.1. (SPSS, Chicago, Ill). Differences were considered statistically significant at P<0.05.
Results
Plasma tizanidine
Rifampicin moderately decreased the mean C max of tizanidine (by 51%; P=0.002) and its AUC(0–∞) (by 54%; P=0.009) (Fig. 2, Table 2). There was little variation in the extent of the interaction, but in one of the ten subjects, the C max and AUC(0–∞) were not decreased at all (Fig. 3a,c). Furthermore, the mean t ½ and t max of tizanidine were unaffected by rifampicin (Figs. 2, 3b, Table 2).
Individual values for peak concentration in plasma (C max) (a), elimination half-life (t ½) (b), and area under plasma concentration-time curve from time 0 to infinity [AUC(0–∞)] (c) of tizanidine in ten healthy volunteers after a single oral dose of 4 mg tizanidine after treatment with placebo or 600 mg rifampicin daily for 5 days
Tizanidine metabolites M-3 and M-4 in plasma
Rifampicin slightly reduced the C max of M-3 (17%; P=0.044) and M-4 (10%; P=0.050), and shortened the t max of M-4 (from 2.5 to 1.0 h; P=0.014) (Fig. 4, Table 2). The t ½ for M-3 was shortened from 4.1 to 3.6 h (P=0.031). Rifampicin also decreased the AUC(0–∞) of both M-3 (33%; P=0.003) and M-4 (23%; P<0.001), as well as the tizanidine/M-3 AUC(0–∞) ratio (30%; P=0.014), and the tizanidine/M-4 AUC(0–∞) ratio (38%; P = 0.007). The greatest decrease in plasma tizanidine/metabolite concentration ratio was observed during the absorption phase, about 20–120 min after tizanidine administration (Fig. 4).
Plasma concentrations (mean±SEM) of tizanidine metabolites M-3 (a) and M-4 (b), and the tizanidine/M-3 ratio (c) and tizanidine/M-4 ratio (d), in ten healthy volunteers after a 4 mg oral dose of tizanidine following pretreatment with placebo (open circles) or 600 mg rifampicin (solid circles) daily for 5 days
Excretion of tizanidine and its metabolites into urine
Rifampicin did not change significantly the Ae (P=0.13) or Clrenal of the parent tizanidine (P=0.14) (Fig. 5). The Ae of M-3, M-4 and M-5 was decreased (P<0.005), but that of M-10 was increased by rifampicin (P=0.008). Rifampicin decreased the tizanidine/M-10 urinary excretion ratio by 55% (P=0.047), but had no statistically significant effect on the urinary excretion ratios of tizanidine to the metabolites M-3, M-4, M-5 or M-9.
Amounts excreted into urine within 24 h (Ae) (mean±SEM) of tizanidine, and its metabolites M-3, M-4, M-5, M-9 and M-10, and urine tizanidine/metabolite ratios, in ten healthy subjects after a 4 mg oral dose of tizanidine following pretreatment with placebo (open bars) or 600 mg of rifampicin (hatched bars) daily for 5 days. *P<0.05, **P<0.01, ***P<0.001
Pharmacodynamic variables
In the placebo phase, tizanidine reduced the systolic and diastolic blood pressures and heart rate from baseline values by −17 mmHg, −13 mmHg and −12 beats/min, respectively (Table 3). During the rifampicin phase, the corresponding reductions were −10 mmHg (P=0.059, versus placebo phase), −9 mmHg (P=0.035) and −7 beats/min (P=0.054), respectively. There were no significant differences between the phases in the effects of tizanidine on subjective drowsiness, overall drug effect, or DSST (Table 3).
Caffeine test
Rifampicin decreased the plasma caffeine/paraxanthine concentration ratio by 23%, but this change was statistically non-significant (P=0.081) (Table 1).
Correlations between tizanidine pharmacokinetics and caffeine/paraxanthine ratio and their changes by rifampicin
The AUC(0–∞), C max and Ae of the parent tizanidine during the placebo phase, and their changes caused by rifampicin, correlated significantly (P<0.05) with the caffeine/paraxanthine ratio during the placebo phase, and with the change of the caffeine/paraxanthine ratio with rifampicin (Table 4). Furthermore, during placebo, the tizanidine/M-3 and tizanidine/M-4 AUC(0–∞) ratios, the Ae of M-3 and M-5, and all tizanidine/metabolite Ae ratios correlated significantly with the caffeine/paraxanthine ratio (P<0.01). Moreover, the changes in the tizanidine/M-3 AUC(0–∞) ratio, Ae of M-5, tizanidine/M-4 Ae ratio, tizanidine/M-5 Ae ratio and tizanidine/M-10 Ae ratio correlated with the change caused by rifampicin in the caffeine/paraxanthine ratio (P<0.05).
Discussion
The results of the present study show that administration of rifampicin 600 mg daily for 5 days only weakly affects the pharmacokinetics of tizanidine, a CYP1A2 substrate with an extensive presystemic metabolism, and the caffeine test, an index of hepatic CYP1A2 activity. Rifampicin decreased the C max and AUC(0–∞) of tizanidine by about 50%, and had no effect on its t ½ or renal clearance. An identical short-term pretreatment with rifampicin has decreased the C max and AUC of several drugs, e.g. midazolam, triazolam, buspirone and simvastatin, which have a considerable CYP3A4-mediated presystemic metabolism, by 10- to 30-fold more than this [4–7].
Induction of several CYP enzymes, e.g. CYP3A4, and of other proteins by rifampicin is mediated by the pregnane X receptor (PXR) [27, 41, 42]. However, induction of CYP1A2 is mediated by the aryl hydrocarbon receptor (Ahr) [26, 27], and there is no direct evidence about the involvement of PXR in the regulation of CYP1A2. The in vitro effects of the PXR ligand rifampicin on CYP1A2 expression have been variable. For example, in cultured human hepatocytes, rifampicin has induced expression of CYP1A2 mRNA much less (0.5-fold reduction to 2-fold increase) than that of CYP3A4 (more than 50-fold increase), CYP2B6 (about 9-fold), CYP2C8 (about 6.5-fold), CYP2C9 (about 4-fold), or CYP3A5 (about 5-fold) [43]. In other in vitro studies, rifampicin has had either no effect [44–47] or it has increased (even several-fold) CYP1A2 expression or activity [48, 49]. In a recent study, rifampicin induced expression of CYP1A2 mRNA by 3- to 26-fold, and that of Ahr 2- to 3-fold in cultured human hepatocytes, suggesting that rifampicin can increase CYP1A2 expression by inducing Ahr [48]. Our present findings are consistent with these in vitro results, and indicate that CYP1A2 is only weakly induced by rifampicin in humans.
The oral bioavailability of tizanidine is only about 10–30% due to extensive presystemic metabolism [33, 38, 50], with CYP1A2 being crucial to its metabolism [34, 35]. Fluvoxamine and ciprofloxacin, inhibitors of CYP1A2 [36, 37], have drastically increased the AUC (33-fold and 10-fold, respectively) of tizanidine [35, 38], suggesting that the contribution of CYP1A2 to the total elimination of tizanidine would be at least 90–97%. The main metabolites of tizanidine found in human plasma are M-3, M-4 and M-10 [33]. In addition to these, significant amounts of M-5 and M-9 were excreted into urine. The enzymes responsible for the formation of tizanidine metabolites have not been fully characterised. However, preliminary in vitro results (M.J. Karjalainen et al., unpublished data) from our laboratory indicate that CYP1A2 mediates the formation of M-3, M-4 and M-5. In our present study, the AUC(0–∞) and C max of the parent tizanidine, and the different tizanidine/metabolite ratios correlated significantly with the caffeine/paraxanthine ratio during the placebo phase, supporting the role of CYP1A2 in the formation of tizanidine metabolites [51].
In the present study, rifampicin reduced the tizanidine/M-3 and tizanidine/M-4 ratios in plasma and shortened the t max of M-4, consistent with induction of the formation of M-3 and M-4 by rifampicin. The rate of biotransformation of tizanidine to M-3 and M-4 was increased by rifampicin especially during the absorption phase, as seen in the ascending portions of the plasma M-3 and M-4 concentration-time curves, and the over 50% reduction in the plasma tizanidine/metabolite ratios at 20 min–2 h after tizanidine intake (Fig. 4). The effect of rifampicin on the AUC of tizanidine and the tizanidine/M-3 and tizanidine/M-4 AUC-ratios with its effect on the caffeine/paraxanthine ratio, strongly suggesting that the increase in M-3 and M-4 formation by rifampicin was due to induction of CYP1A2. It seems that rifampicin also induced the further metabolism of M-3, M-4 and M-5, which probably explains the reduced AUC values and urinary excretions (Ae) of these metabolites and the shortened t ½ of M-3. Rifampicin had no statistically significant effect on the tizanidine/M-3, tizanidine/M-4, tizanidine/M-5 and tizanidine/M-9 Ae ratios (Fig. 5), which may be explained by variability in the renal clearance of tizanidine and its metabolites. However, rifampicin markedly reduced the tizanidine/M-10 Ae ratio. Thus, it is possible that the formation of M-10 is partially mediated by a CYP-enzyme that is strongly induced by rifampicin, such as CYP3A4 [3, 4]. However, as rifampicin only slightly increased the Ae of M-10 and as only about 12% of the tizanidine dose is normally excreted in urine as M-10 [33], this finding alone cannot explain the 50% reduction in the AUC of tizanidine. However, it is possible that the reduction in the AUC of tizanidine by rifampicin was partially due to strong induction of an enzyme (e.g. CYP3A4) and metabolic pathway(s) with a minor contribution to the metabolism of tizanidine in non-induced subjects. This hypothesis could be tested by investigating the effects of selective CYP1A2 and CYP3A4 inhibitors on the pharmacokinetics of tizanidine in rifampicin-induced subjects.
In the present study, rifampicin reduced the AUC of tizanidine by about 50%, mainly by inducing its first-pass metabolism (no effect on t ½), and had only a minor, statistically non-significant effect (23%) on the caffeine test; rifampicin reduced the caffeine/paraxanthine ratio in eight of the ten subjects studied. The caffeine/paraxanthine ratio reflects mainly the systemic CYP1A2-mediated elimination of caffeine, since caffeine lacks presystemic metabolism [28–32]. The effect of rifampicin on the pharmacokinetics of tizanidine was, although small, still stronger than its effect on the caffeine test. Accordingly, it is possible that tizanidine could be more sensitive than caffeine as an indicator of CYP1A2 induction. It is also worth noting that the effects of CYP1A2 inhibitors on the AUC and C max of tizanidine were greater than their effects on the caffeine test [35, 38, 51].
Only a 5-day pretreatment with rifampicin was used in the present study, and therefore hepatic enzyme induction was not necessarily maximal at the time of tizanidine intake [3]. However, an identical 5-day pretreatment with rifampicin has been shown to cause a very strong induction of CYP3A4-mediated metabolism [4–7]. Furthermore, Branch et al. [52] reported only a 16% increase in the paraxanthine-to-caffeine ratio in healthy subjects after a long, 28-day, treatment with 600 mg rifampicin daily. In other studies, rifampicin has modestly reduced the AUC of CYP1A2 substrates: orally administered theophylline (by 18–45%) [3, 10, 11] and caffeine (by about 40%) [12, 13], and intravenously administered ropivacaine (by 38–52%) [14]. Taken together, on the basis of the present results and previous findings, it seems obvious that rifampicin is at most only a weak inducer of CYP1A2-mediated presystemic and systemic metabolism in humans. Accordingly, drugs metabolised by CYP1A2 only are much less susceptible than substrates of CYP3A4 to drug interactions caused by enzyme inducers of the rifampicin type.
The effects of tizanidine on systolic and diastolic blood pressure and heart rate were weaker during the rifampicin phase than during the placebo phase, i.e. the reduced plasma concentrations of tizanidine had pharmacodynamic consequences. It is likely that the therapeutic effects of tizanidine are also similarly reduced during treatment with rifampicin, which may be of clinical significance in some patients. Notably, the main metabolites of tizanidine in plasma (M-3, M-4, M-10) lack pharmacological activity and have no clinical relevance [33].
In conclusion, treatment with 600 mg rifampicin daily moderately decreases the plasma concentrations of tizanidine, and slightly reduces its cardiovascular effects. The inducibility of CYP1A2-mediated presystemic (tizanidine) and systemic (tizanidine and caffeine) metabolism by usual therapeutic doses of rifampicin is weak at the most. Compared to CYP3A4 substrate drugs, substrates of CYP1A2 are much less susceptible to drug interactions caused by enzyme inducers of the rifampicin type.
References
Combalbert J, Fabre I, Fabre G, Dalet I, Derancourt J, Cano JP, Maurel P (1989) Metabolism of cyclosporin A. IV. Purification and identification of the rifampicin-inducible human liver cytochrome P-450 (cyclosporin A oxidase) as a product of P450IIIA gene subfamily. Drug Metab Dispos 17:197–207
Kolars JC, Schmiedlin-Ren P, Schuetz JD, Fang C, Watkins PB (1992) Identification of rifampin-inducible P450IIIA4 (CYP3A4) in human small bowel enterocytes. J Clin Invest 90:1871–1878
Niemi M, Backman JT, Fromm MF, Neuvonen PJ, Kivistö KT (2003) Pharmacokinetic interactions with rifampicin: clinical relevance. Clin Pharmacokinet 42:819–850
Backman JT, Olkkola KT, Neuvonen PJ (1996) Rifampin drastically reduces plasma concentrations and effects of oral midazolam. Clin Pharmacol Ther 59:7–13
Villikka K, Kivistö KT, Backman JT, Olkkola KT, Neuvonen PJ (1997) Triazolam is ineffective in patients taking rifampin. Clin Pharmacol Ther 61:8–14
Lamberg TS, Kivistö KT, Neuvonen PJ (1998) Concentrations and effects of buspirone are considerably reduced by rifampicin. Br J Clin Pharmacol 45:381–385
Kyrklund C, Backman JT, Kivistö KT, Neuvonen M, Laitila J, Neuvonen PJ (2000) Rifampin greatly reduces plasma simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther 68:592–597
Greiner B, Eichelbaum M, Fritz P, Kreichgauer HP, von Richter O, Zundler J, Kroemer HK (1999) The role of intestinal P-glycoprotein in the interaction of digoxin and rifampin. J Clin Invest 104:147–153
Fromm MF, Kauffmann HM, Fritz P, Burk O, Kroemer HK, Warzok RW, Eichelbaum M, Siegmund W, Schrenk D (2000) The effect of rifampin treatment on intestinal expression of human MRP transporters. Am J Pathol 157:1575–1580
Robson RA, Miners JO, Wing LM, Birkett DJ (1984) Theophylline-rifampicin interaction: non-selective induction of theophylline metabolic pathways. Br J Clin Pharmacol 18:445–448
Straughn AB, Henderson RP, Lieberman PL, Self TH (1984) Effect of rifampin on theophylline disposition. Ther Drug Monit 6:153–156
Wietholtz H, Zysset T, Marschall HU, Generet K, Matern S (1995) The influence of rifampin treatment on caffeine clearance in healthy man. J Hepatol 22:78–81
Soto J, Sacristan JA, Alsar MJ (1996) Use of salivary caffeine tests to assess the inducer effect of a drug on hepatic metabolism. Ann Pharmacother 30:736–739
Jokinen MJ, Olkkola KT, Ahonen J, Neuvonen PJ (2001) Effect of rifampin and tobacco smoking on the pharmacokinetics of ropivacaine. Clin Pharmacol Ther 70:344–350
Sarkar MA, Hunt C, Guzelian PS, Karnes HT (1992) Characterization of human liver cytochromes P-450 involved in theophylline metabolism. Drug Metab Dispos 20:31–37
Rasmussen BB, Mäenpää J, Pelkonen O, Loft S, Poulsen HE, Lykkesfeldt J, Brøsen K (1995) Selective serotonin reuptake inhibitors and theophylline metabolism in human liver microsomes: potent inhibition by fluvoxamine. Br J Clin Pharmacol 39:151–159
Tjia JF, Colbert J, Back DJ (1996) Theophylline metabolism in human liver microsomes: inhibition studies. J Pharmacol Exp Ther 276:912–917
Shimada T, Gillam EM, Sutter TR, Strickland PT, Guengerich FP, Yamazaki H (1997) Oxidation of xenobiotics by recombinant human cytochrome P450 1B1. Drug Metab Dispos 25:617–622
Butler MA, Iwasaki M, Guengerich FP, Kadlubar FF (1989) Human cytochrome P-450PA (P-450IA2), the phenacetin O-deethylase, is primarily responsible for the hepatic 3-demethylation of caffeine and N-oxidation of carcinogenic arylamines. Proc Natl Acad Sci USA 86:7696–7700
Tassaneeyakul W, Mohamed Z, Birkett DJ, McManus ME, Veronese ME, Tukey RH, Quattrochi LC, Gonzalez FJ, Miners JO (1992) Caffeine as a probe for human cytochromes P450: validation using cDNA-expression, immunoinhibition and microsomal kinetic and inhibitor techniques. Pharmacogenetics 2:173–183
Tassaneeyakul W, Birkett DJ, McManus ME, Veronese ME, Andersson T, Tukey RH, Miners JO (1994) Caffeine metabolism by human hepatic cytochromes P450: contributions of 1A2, 2E1 and 3A isoforms. Biochem Pharmacol 47:1767–1776
Ha HR, Chen J, Krähenbühl S, Follath F (1996) Biotransformation of caffeine by cDNA-expressed human cytochromes P-450. Eur J Clin Pharmacol 49:309–315
Ekström G, Gunnarsson UB (1996) Ropivacaine, a new amide-type local anesthetic agent, is metabolized by cytochromes P450 1A and 3A in human liver microsomes. Drug Metab Dispos 24:955–961
Arlander E, Ekström G, Alm C, Carrillo JA, Bielenstein M, Böttiger Y, Bertilsson L, Gustafsson LL (1998) Metabolism of ropivacaine in humans is mediated by CYP1A2 and to a minor extent by CYP3A4: an interaction study with fluvoxamine and ketoconazole as in vivo inhibitors. Clin Pharmacol Ther 64:484–491
Kobayashi Y, Sakai R, Ohshiro N, Ohbayashi M, Kohyama N, Yamamoto T (2005) Possible involvement of organic anion transporter 2 on the interaction of theophylline with erythromycin in the human liver. Drug Metab Dispos 33:619–622
Poland A, Glover E, Kende AS (1976) Stereospecific, high affinity binding of 2,3,7,8-tetrachlorodibenzo-p-dioxin by hepatic cytosol. Evidence that the binding species is receptor for induction of aryl hydrocarbon hydroxylase. J Biol Chem 251:4936–4946
Tirona RG, Kim RB (2005) Nuclear receptors and drug disposition gene regulation. J Pharm Sci 94:1169–1186
Fuhr U, Rost KL (1994) Simple and reliable CYP1A2 phenotyping by the paraxanthine/caffeine ratio in plasma and in saliva. Pharmacogenetics 4:109–116
Fuhr U, Rost KL, Engelhardt R, Sachs M, Liermann D, Belloc C, Beaune P, Janezic S, Grant D, Meyer UA, Staib AH (1996) Evaluation of caffeine as a test drug for CYP1A2, NAT2 and CYP2E1 phenotyping in man by in vivo versus in vitro correlations. Pharmacogenetics 6:159–176
Spigset O, Hägg S, Söderström E, Dahlqvist R (1999) The paraxanthine:caffeine ratio in serum or in saliva as a measure of CYP1A2 activity: when should the sample be obtained? Pharmacogenetics 9:409–412
Faber MS, Jetter A, Fuhr U (2005) Assessment of CYP1A2 activity in clinical practice: why, how, and when? Basic Clin Pharmacol Toxicol 97:125–134
Dollery C (1999) Caffeine. In: Dollery C (ed) Therapeutic drugs. Churchill Livingstone, Edinburgh, pp C4–C6
Koch P, Hirst DR, von Wartburg BR (1989) Biological fate of sirdalud in animals and man. Xenobiotica 19:1255–1265
Granfors MT, Backman JT, Laitila J, Neuvonen PJ (2004) Tizanidine is mainly metabolized by cytochrome p450 1A2 in vitro. Br J Clin Pharmacol 57:349–353
Granfors MT, Backman JT, Neuvonen M, Ahonen J, Neuvonen PJ (2004) Fluvoxamine drastically increases concentrations and effects of tizanidine: a potentially hazardous interaction. Clin Pharmacol Ther 75:331–341
Brøsen K, Skjelbo E, Rasmussen BB, Poulsen HE, Loft S (1993) Fluvoxamine is a potent inhibitor of cytochrome P4501A2. Biochem Pharmacol 45:1211–1214
Harder S, Fuhr U, Staib AH, Wolff T (1989) Ciprofloxacin-caffeine: a drug interaction established using in vivo and in vitro investigations. Am J Med 87:89S–91S
Granfors MT, Backman JT, Neuvonen M, Neuvonen PJ (2004) Ciprofloxacin greatly increases concentrations and hypotensive effect of tizanidine by inhibiting its cytochrome P450 1A2-mediated presystemic metabolism. Clin Pharmacol Ther 76:598–606
Pickard CE, Stewart AD, Hartley R, Lucock MD (1986) A rapid HPLC method for monitoring plasma levels of caffeine and theophylline using solid phase extraction columns. Ann Clin Biochem 23:440–446
Holland DT, Godfredsen KA, Page T, Connor JD (1998) Simple high-performance liquid chromatography method for the simultaneous determination of serum caffeine and paraxanthine following rapid sample preparation. J Chromatogr B Biomed Sci Appl 707:105–110
Lehmann JM, McKee DD, Watson MA, Willson TM, Moore JT, Kliewer SA (1998) The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions. J Clin Invest 102:1016–1023
Honkakoski P, Sueyoshi T, Negishi M (2003) Drug-activated nuclear receptors CAR and PXR. Ann Med 35:172–182
Rae JM, Johnson MD, Lippman ME, Flockhart DA (2001) Rifampin is a selective, pleiotropic inducer of drug metabolism genes in human hepatocytes: studies with cDNA and oligonucleotide expression arrays. J Pharmacol Exp Ther 299:849–857
Morel F, Beaune PH, Ratanasavanh D, Flinois JP, Yang CS, Guengerich FP, Guillouzo A (1990) Expression of cytochrome P-450 enzymes in cultured human hepatocytes. Eur J Biochem 191:437–444
Li AP, Reith MK, Rasmussen A, Gorski JC, Hall SD, Xu L, Kaminski DL, Cheng LK (1997) Primary human hepatocytes as a tool for the evaluation of structure-activity relationship in cytochrome P450 induction potential of xenobiotics: evaluation of rifampin, rifapentine and rifabutin. Chem Biol Interact 107:17–30
Mills JB, Rose KA, Sadagopan N, Sahi J, de Morais SM (2004) Induction of drug metabolism enzymes and MDR1 using a novel human hepatocyte cell line. J Pharmacol Exp Ther 309:303–309
Roymans D, Van Looveren C, Leone A, Parker JB, McMillian M, Johnson MD, Koganti A, Gilissen R, Silber P, Mannens G, Meuldermans W (2004) Determination of cytochrome P450 1A2 and cytochrome P450 3A4 induction in cryopreserved human hepatocytes. Biochem Pharmacol 67:427–437
Maglich JM, Stoltz CM, Goodwin B, Hawkins-Brown D, Moore JT, Kliewer SA (2002) Nuclear pregnane x receptor and constitutive androstane receptor regulate overlapping but distinct sets of genes involved in xenobiotic detoxification. Mol Pharmacol 62:638–646
Madan A, Graham RA, Carroll KM, Mudra DR, Burton LA, Krueger LA, Downey AD, Czerwinski M, Forster J, Ribadeneira MD, Gan LS, LeCluyse EL, Zech K, Robertson P, Jr., Koch P, Antonian L, Wagner G, Yu L, Parkinson A (2003) Effects of prototypical microsomal enzyme inducers on cytochrome P450 expression in cultured human hepatocytes. Drug Metab Dispos 31:421–431
Wagstaff AJ, Bryson HM (1997) Tizanidine. A review of its pharmacology, clinical efficacy and tolerability in the management of spasticity associated with cerebral and spinal disorders. Drugs 53:435–452
Granfors MT, Backman JT, Laitila J, Neuvonen PJ (2005) Oral contraceptives containing ethinyl estradiol and gestodene markedly increase plasma concentrations and effects of tizanidine by inhibiting cytochrome P450 1A2. Clin Pharmacol Ther 78:400–411
Branch RA, Adedoyin A, Frye RF, Wilson JW, Romkes M (2000) In vivo modulation of CYP enzymes by quinidine and rifampin. Clin Pharmacol Ther 68:401–411
Acknowledgements
This study was supported by grants from the Helsinki University Central Hospital Research Fund, the National Technology Agency, and the Sigrid Jusélius Foundation, Finland. None of the authors has any financial or personal relationships that could be perceived as influencing the research described. The experiments comply with the current laws of Finland, and the study protocol was approved by the Ethics Committee for Studies in Healthy Subjects and Primary Care of the Hospital District of Helsinki and Uusimaa and the Finnish National Agency for Medicines.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Backman, J.T., Granfors, M.T. & Neuvonen, P.J. Rifampicin is only a weak inducer of CYP1A2-mediated presystemic and systemic metabolism: studies with tizanidine and caffeine. Eur J Clin Pharmacol 62, 451–461 (2006). https://doi.org/10.1007/s00228-006-0127-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0127-x