Abstract
Objective
To determine whether pharmacogenetic tests such as N-acetyltransferase 2 (NAT2) and cytochrome P450 2E1 (CYP2E1) genotyping are useful in identifying patients prone to antituberculosis drug-induced hepatotoxicity in a cosmopolite population.
Methods
In a prospective study we genotyped 89 patients treated with isoniazid (INH) for latent tuberculosis. INH-induced hepatitis (INH-H) or elevated liver enzymes including hepatitis (INH-ELE) was diagnosed based on the clinical diagnostic scale (CDS) designed for routine clinical practice. NAT2 genotypes were assessed by fluorescence resonance energy transfer probe after PCR analysis, and CYP2E1 genotypes were determined by PCR with restriction fragment length polymorphism analysis.
Results
Twenty-six patients (29%) had INH-ELE, while eight (9%) presented with INH-H leading to INH treatment interruption. We report no significant influence of NAT2 polymorphism, but we did find a significant association between the CYP2E1 *1A/*1A genotype and INH-ELE (OR: 3.4; 95% CI:1.1-12; p=0.02) and a non significant trend for INH-H (OR: 5.9; 95% CI: 0.69–270; p=0.13) compared with other CYP2E1 genotypes. This test for predicting INH-ELE had a positive predictive value (PPV) of 39% (95% CI: 26–54%) and a negative predictive value (NPV) of 84% (95% CI: 69–94%).
Conclusion
The genotyping of CYP2E1 polymorphisms may be a useful predictive tool in the common setting of a highly heterogeneous population for predicting isoniazid-induced hepatic toxicity. Larger prospective randomized trials are needed to confirm these results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycobacterium tuberculosis was responsible for two million deaths and eight million newly infected patients in 1999 [1]. As its incidence increases world-wide, a greater number of patients may be at risk for severe adverse drug reactions (ADRs) when treated with antituberculosis chemotherapy. Clinically important ADRs induced by antituberculous agents include liver toxicity [2], neurotoxicity (polyneuropathy, optical neuritis, seizure) [3, 4], and skin (cutaneous eruption), arthritic and gastrointestinal toxicity [5, 6] with an overall incidence of approximately 5%. The occurrence of ADRs related to INH, particularly hepatotoxicity, has been well-defined [5] and shown to increase as a result of drug-drug pharmacokinetic or pharmacodynamic interactions [7–11].
INH is mainly inactivated by N-acetyltransferase 2 (NAT2)-mediated acetylation, resulting in acetylisoniazid (Fig 1), which is hydrolyzed to acetylhydrazine. The latter is further oxidized by cytochrome P4502E1 (CYP2E1) to form hydroxylamines, which are intermediates in the formation of established hepatotoxic metabolites [12–15]. There are large variations in the metabolism of the antituberculous drug isoniazid, suggesting a pharmacogenetic polymorphism of NAT. This enzyme is markedly decreased in livers of slow acetylators (SA). The official nomenclature of the NAT2 polymorphism can be found on the official website: http://louisville.edu/medschool/ pharmacology/NAT2.html. The elimination of INH has been described to follow a bimodal and even a trimodal distribution consisting of slow (SA), intermediate (IA) and rapid actetylators (RA), and there is a strong correlation (from 0.93 to 1 in the Caucasian population) between these phenotypes and NAT2 genotypes [13, 16–18]. The main clinical interest in the NAT2 polymorphism is the presumed association of the phenotype with the therapeutic response and the occurrence of ADRs. The SA polymorphism has been suspected to be a risk factor for INH-induced hepatotoxicity but despite numerous studies, the controversy still remains [13, 14, 16–21].
Pathways of isoniazid metabolism. Scheme illustrating the metabolism of isoniazid through multiple pathways. The main (confirmed) pathways are indicated by continuous arrows, while a hypothetical alternative pathway is shown with a dotted arrow. The two enzymes involved in these pathways and genotyped in the present study are located within boxes
On the other hand, CYP2E1 is a major ethanol-induced microsomal enzyme expressed in the liver and in other organs such as the kidney, lung, nasal mucosa, brain and lymphocytes [22]. Because of its wide range of substrates (aromatic and halogenated hydrocarbons, halogenated anaesthetics, alcohols, nitrosamines…), this cytochrome plays an important role in the field of clinical toxicology [23]. Several CYP2E1 genetic polymorphisms are currently detectable applying techniques involving the RsaI, TaqI, DraI and PstI restriction enzymes, but the clinical significance of these polymorphisms remains unclear, partly because no convincing association between CYP2E1 catalytic activities and their genotypes has been demonstrated [24–26].
In the study reported here, we found that CYP2E1 was involved in INH metabolism and that its c1/c1 genotype (RsaI polymorphism) was an independent risk factor for antituberculous agents-induced hepatitis after adjustment for NAT2 acetylator status and age in the Asian population [27, 28].
Patients and methods
The protocol was approved by the local ethics committee and written informed consent was obtained from all participants.
Patients
Between October 2001 and March 2003, 103 consecutive outpatients (53 men and 50 women) with primary tuberculosis were asked to participate in this prospective study. Inclusion criteria consisted of the patients having latent tuberculosis as defined by the American Thoracic Society [29] with normal plasma aspartate transaminase (AST) and alanine transaminase (ALT) levels prior to the beginning of INH monotherapy. Exclusion criteria consisted of a history of alcohol consumption, positive serology for the hepatitis A virus (HAV), hepatitis B virus (HBV) or hepatitis C virus (HCV), poor chemotherapy compliance (negative urine INH three times during the follow-up), loss during the follow-up or if the patients had to receive supplementary antituberculosis agents or other potentially hepatotoxic drugs.
Of the initial sample of 103 patients, three (two women, one man) were excluded because of active B hepatitis (positive HBs antigen). During follow-up, 11 additional patients (seven women, four men) had to be excluded: five patients because they had to receive supplementary antituberculosis chemotherapy, four were lost during the follow-up and two were excluded because of poor compliance. At the end of the study period, 89 patients were evaluated. Among these, 40 (45%) were women, Median age was 31 years (range: 17–73 years), with a value between the first and the third quartile ranging from 24 to 41 years of age. Thirty eight patients (43%) were Caucasians, eight (9%) were Hispanic, 22 (25%) were African, 15 (17%) were South Americans, five (6%) were Asians and one (1%) was native to the Middle East.
Before treatment, each patient was emphatically requested to refrain from any alcohol consumption and self-medication without first reporting it. Five patients (6%) were taking various medications before being enrolled in the study: one was treated with omeprazole 40 mg for a gastritis, one with ciprofloxacine for 5 days because of an urinary tract infection, one took losartan and simvastatine because of hypertension and dyslipidemia, one was treated with metformin, omeprazole and venlafaxine because of diabetes, gastroesophageal reflux disease and depression and one patient was treated with glibenclamide, metformin, nifedipin, furosemid, enalapril and aspirin because of diabetes and hypertension. All of the patients participating in the study were treated with isoniazid (INH) 300 mg daily and vitamin B6 40 mg per day for a period of 6 months. Liver function, chemotherapy compliance (positive urine INH test), response to rechallenge (when performed) and risk factors such as alcohol use, pregnancy or concomitant use of drugs were assessed twice a month by an independent investigator.
Criteria for the diagnosis of INH-induced hepatitis (INH-H) consisted of elevation in AST and/or ALT levels fourfold above the upper reference limit (168 UI/l) with or without symptoms. These criteria are routinely used by our institution pneumologists and gastroenterologists and are in accordance with the recommendations of Ozick et al. [31] and consistent with the recommendations of the American Thoracic Society (ATS) [43]. In the case of INH-induced hepatitis, INH was withdrawn and replaced by rifampicin. INH-induced elevated liver enzymes (INH-ELE) was defined as serum ALT and/or AST values above URL (42 UI/l) with or without INH-H. Clinical Diagnostic Scales (CDS) were used to assess the likelihood of drug involvement when INH-H or INH-ELE were suspected [32]. Based on the CDS, causality assessment of INH-H and INH-ELE was then categorized as definite (score >17), probable (14–17), possible (10–13), unlikely (6–9) or excluded (<6). INH-H and INH-ELE with possible to probable scores (≥10–17) were considered for statistical analysis; unlikely scores were still considered when no other factor (see above) was identifiable.
Methods
DNA extraction
Genomic DNA was extracted from 200 μl of heparinized frozen whole blood using the the Qiagen (Germantown, Md) DNA Blood Minikit and following the manufacturer’s instructions.
NAT2 genotype
Four major NAT2 polymorphic forms were investigated in the individual samples by real time PCR on LightCycler using fluorescence resonance energy transfer (FRET) with hybridization of allele-specific probes for detection. Briefly, simultaneous analysis of NAT2*5A (C→T at position 481), NAT2*6A (G→A at position 590), NAT2*7A/B (G→A substitution at position 857) and NAT2*14A (G→A substitution at position 191) alleles was achieved by performing a dual color recording as indicated by the manufacturer of the kit (Roche, Basel, Switzerland). At the end of the amplification cycle, unambiguous determination of the different genotypes was achieved by melting curve analysis.
CYP2E1 genotype
For CYP2E1 genotyping, PCR was performed in the GeneAmp 9600 Thermocycler (PerkinElmer, Foster City, Calif.) with an activation step (10 min, 95°C), a two-temperature thermal cycling profile, (35 cycles of 20 min at 94°C and 1 min at 62°C) and a final elongation step (7 min at 72°C). The PCR mixture contained: Taq Gold Dna polymerase (2.5 U/rxn), 25 mM MgCl (1.75 mM), 10× PCR Gold buffer (1×), 10 mM dNTP blend (200 μM each), 10 μM forward and reverse primers (0.5 μM) in a 50 μl rxn volume. The template was approximately 100 ng of genomic DNA . All reagents were purchased from Applied Biosystems (Foster City, Calif.).
The four primer sequences wereRsa forward (CCAGTCGAGTCTACATTGTCA) and reverse (TTCATTCTGTCTTCTAACTGG), and Taq forward (GGGCTTTCATCTTCATTTCGA) and reverse (CAAAATGTGGGCTTTCATCTG).
RsaI and TaqI restriction enzymes were purchased from Biogen (Cambridge, Mass.). Restriction mixtures were prepared with specific buffers (provided) and 1 U/rxn of enzyme. Twenty-microliter aliquots of PCR product were digested either at 37°C for 3 h with the RsaI mixture or at 65°C for 3 h with the the TaqI mixture.
Electrophoretic separation and fragment analysis were achieved on a 2% agarose gel. Restriction fragments were of the expected size: the RsaI+ (C1) wild allele produced two fragments of 351 and 61 bp, respectively, while the RsaI− (C2) mutant allele yielded one single fragment of 413 bp. For TaqI analysis, the TaqI+ (A2) wild type allele was identified from its two fragments, of 80 and 74 bp; while the TaqI− (A1) mutant allele produced one single fragment of 154 bp. The heterozygous mutant showed all the three fragments on the gel. According to the recommended nomenclature of CYP 2E1 (http://www.imm.ki.se/CYPalleles), genotypes were determined by the combination of these RFLP:
-
*1A (wild-type allele) = RsaI+, TaqI+ (C1, A2);
-
*1B = TaqI− (independently of RsaI) (A1);
-
*5 = RsaI− (independently of TaqI) (C2).
Because analyses of the PstI and DraI polymorphisms were not performed, further characterization of the *5 genotype in *5A or *5B were carried out.
Serology and clinical chemistry
Serum liver tests were determined using a LX-20 analyzer (Beckmann-Coulter, Brea, Calif.), and serology for viral hepatitis was assessed using commercially available immunoassays (Abott Laboratories, Chicago, Ill.).
Statistics
Data were expressed as median with first (Q1) and third (Q3) quartiles. Proportions, odds ratios (OR) and 95% exact confidence intervals (95% CI) were calculated using> StatXact-3 software. Chi-square test, Fisher’s exact test and trend tests were used to compare groups of patients. A two-sided p value was considered to be significant when below 0.05. Clinical sensitivities (SN) and specificities (SP) and negative (NPV) and positive predictive values (PPV) were assessed for association with INH-induced hepatitis (INH-H) and INH-induced elevated liver enzymes (INH-ELE), with or without hepatitis, against different CYP2E1 and NAT2 genotypes.
Results
Of the 89 patients, 26 (29%) had elevated liver enzymes (Table 1). Six of the 8 patients with hepatitis that led to treatment interruption were symptomatic. The ALT values ranged from 177 to 2005 IU/l for INH-H. It is noteworthy that none of the five patients taking other concomitant medications presented with INH-H or INH-ELE.
Overall the analysis of the likelihood of INH involvement in elevated enzymes (CDS score) led to six patients (23%) being classified as having a probable association with INH and 14 (54%) as having a possible association with INH, whereas six patients (23%) were considered unlikely to be related. None were of these classifications are definite (data not shown).
There was a clear, although non-significant, trend showing that increasing age was associated with a higher incidence of INH-ELE and INH-H, but there was no gender difference (Table 1).
Of the 89 patients, nine (10%) were genotyped as RA, 45 (51%) as IA and 35 (39%) as SA. The genotype frequencies reported here were not markedly different from those predicted by the Hardy-Weinberg equation (Table 2) [33]. The risk of having INH-H or INH-ELE was independent of NAT2 acetylator status (Tables 3, 4). In contrast, the risk of having INH-ELE was significantly associated to the CYP2E1 *1A/*1A genotype. and for this genotype, the risk having an INH-ELE was 3.4-fold higher (OR: 3.4; 95% CI:1.1–12; p=0.02) when compared with all other CYP2E1 genotypes (Tables 3, 4). Although nonsignificant, a trend was also identified showing that the CYP2E1 *1A/*1A genotype was associated with a higher incidence of INH-H in comparison to other CYP2E1 genotypes (OR:5.9; 95%CI:0.69–270; p= 0.13).
Among patients that developed an INH-ELE with a CYP2E1*1A/*1A genotype, the distribution of NAT2 genotype was identical to that observed in the general population (data not shown).
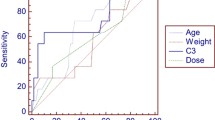
When tested for predicting INH-ELE, the CYP2E1 *1A/*1A genotype yielded a specificity of 51% (95% CI: 35–57%) and a sensitivity of 77% (95% CI: 56–91%) with a PPV of 39% (95% CI: 26–54%) and a NPV of 84% (95% CI:69–94%). For the INH-H group, the SP was 46% (95% CI: 35–57%), the SN reached 87% (95% CI: 47–100%), the PPV was 14% (95% CI: 6–26%) and the NPV was 84% (95% CI: 69–94%), (Table 5).
In order to test a potential allele-allele interaction between NAT2 and CYP2E1 polymorphisms, we performed separate analyses combining the CYP2E1 wild-type and mutant alleles with the NAT2 wild-type and mutant alleles in patients with INH-H and INH-ELE. No significant result was observed.
Discussion
On the basis of our study we are able to report a significant association between the CYP2E1 * 1A/*1A genotype and the risk of developing INH-induced hepatotoxicity without hepatitis, with a sensitivity for the CYP2E1 mutant genotype of 77% (95% CI: 56–91%) and a negative predictive value of 84% (95% CI: 69–94%), suggesting a possible protective role of any of the CYP2E1 mutants. These results are consistent with those of Wong et al. who suggested that the A1 allele (*1B, according to the new nomenclature) in the homo- or heterozygous form had a possible protective role in alcoholic liver disease [25] and with those of Huang showing that CYP2E1 RsaI polymorphism was associated with susceptibility to INH-induced hepatotoxicity [27]. Although the role of CYP2E1 might be different for alcoholic liver disease and INH-induced hepatotoxicity, [27] these results are in agreement the current hypothesis depicted in Fig. 1 and emphasise the critical role of CYP2E1 in generating potential hepatotoxic compounds [12–15]. Although our population was small and highly heterogeneous, the possibility that this statistical association might stem from a population stratification can be excluded as we performed our statistical analyses always considering the 89 patients as a unique group, irregardless of their ethnic origin. Although nonsignificant, we also reported a trend between the wild-type CYP2E1 genotype and the likelihood to develop INH-H. The most likely explanation for this lack of statistical signification is a type II error because of the small number of patients enrolled in this study. The other striking finding of our study is that our results failed to show any significant association between NAT2 susceptibility to INH-induced hepatotoxicity in contrast to the recent studies performed with Asian populations [19, 28]. Several explanations of this apparently contradictory observation can be proposed.
First, these discrepancies might well result from a different genotype distribution among Asian and European patients. The NAT2 genotypes and phenotypic (based upon genotype) [13, 16–18] distributions obtained in this study included fewer SA phenotypes than expected. Only 10% RA phenotypes were found, whereas 50% are expected in a Caucasian population [13, 16, 18]. Even if NAT2 allelic distributions were consistent with those predicted by the Hardy-Weinberg equation, they were markedly different from those obtained in Asian populations [27, 28, 34]. Hence, it is likely that the heterogeneity of our population accounts for these differences as important genotype/phenotype prevalences of SA variations occur in accordance to the ethnic group considered (Oriental, 10%; Caucasian, 50%; Egyptian, 80%) [13, 16, 35, 36]. Another explanation could be related to the difference in the treatments between our study and the three Asian ones [19, 27, 28]. Indeed, in our study, patients were treated with 300 mg of INH daily, whereas 600 mg INH was prescribed in the other studies. More importantly, patients in the Asian studies were treated with two to four antituberculosis agents (rifampicin, ethambutol, pyrazinamid and INH) [19, 27, 28]. As rifampicin is known to reduce NAT2 activity [38, 39], as INH is known to have a biphasic effect on CYP2E1 activity (initial inhibition followed by an induction) [40] and because a combination of these drugs is known to increase the incidence of antituberculous drug-induced hepatotoxicity up to 35% [37–41], drug-drug pharmacokinetic and pharmacodynamic interactions certainly did occur. As such, these pharmacodynamic and pharmacokinetic interactions are very likely to represent a major confounding factor impeding proper interpretation of the results obtained in these studies. The patients in the present study were under monotherapy (INH alone) and because none of the five patients receiving other concomitant medications presented INH-hepatitis or INH-elevated liver enzyme, these potential interactions did not occur in our study. A third possible explanation is that in the presence of a highly heterogeneous population, NAT2 genotyping its predictive value. CYP2E1 genotyping could therefore represent the most appropriate test to perform in an ethnically heterogeneous population. Other caveats could be related to methodological issues of our study, such as a type II error because our population was smaller than those evaluated by Huang et al. [27, 28] and Ohno et al. [19].
Finally, the incidence of INH-induced enzyme activity (INH-ELE and INH-H) reported here (26/89; 29%) was higher than any value previously reported (1–5%) and might be related to the fact that most of the earlier studies did not consider the elevation in liver enzymes in their analysis [5, 30, 31, 41]. The incidence of INH-induced hepatitis reported here was also higher (9% versus 1–5%) than reported in the literature [5, 30, 31, 41]. As suggested by Huang et al., the real incidence of INH-induced adverse events, in particular INH-induced hepatitis, could well have been underestimated in previous studies in the absence of systematic assessment [27, 28]. For example, the United States Public Health Service study showed a INH-induced hepatitis incidence of 1% [30], but liver function was controlled only when clinical signs were present and not in a systematic manner as was done in the present study. Furthermore, recent reports show that the prevalence of INH-induced hepatotoxicity is consistently higher than previously thought, with a frequency reaching 13–26% and even 35% in one Japanese study [27, 30, 41–43]. In this perspective, our results support the hypothesis that the frequency of INH-induced hepatotoxicity might have been underestimated.
In conclusion, this study shows for the first time that the CYP2E1 *1A/*1A polymorphism may confer a greater risk of INH-induced hepatotoxicity in the setting of a heterogeneous ethnic population. Because of the acceptable NPV of any CYP2E1 mutant allele obtained in the present study, this test could be of clinical utility in the setting of a cosmopolite population. Because ethnic heterogeneity represents the daily reality most clinicians have to deal with, we thought it important to test the potential predictive value of genotyping in this common setting. However, due to the small number of patients enrolled in this study, these results must be considered as preliminary and need to be replicated in a larger sample. Nevertheless, our results do suggest that the CYP2E1 genotype could be a much more robust and independent predictive parameter when evaluating the risk of experiencing hepatic adverse effects with antituberculosis drugs than the NAT2 genotype when applied to an ethnically heterogeneous population.
Abbreviations
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- CDS:
-
Clinical diagnostic scale
- CI:
-
Confidence interval
- FN:
-
False negative
- FP:
-
False positive
- IA:
-
Intermediate acetylator
- INH:
-
Isoniazid
- INH-ELE:
-
Isoniazid-induced elevated liver enzymes
- INH-H:
-
Isoniazid-induced hepatitis
- NAT2:
-
N-acetyltransferase type 2
- NPV:
-
Negative predictive value
- OR:
-
Odds ratio
- PPV:
-
Positive predictive value
- RA:
-
Rapid acetylator
- RFLP:
-
Restriction fragment length polymorphism
- SA:
-
Slow acetylator
- SP:
-
Specificity
- SN:
-
Sensitivity
- TN:
-
True negative
- TP:
-
True positive
- ∞:
-
infinity
- URL:
-
Upper reference limit
References
Dye C (1999) Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA 282:677–686
Durant F, Jebrak G, Pessayre D, Fournier M, Bernau J (1996) Hepatotoxicity of antitubercular treatments. Rationale for monitoring liver status. Drug Saf 16:394–405
Martinjak-Dvorsek I, Gorjup V, Horvat M, Noc M (2000) Acute isoniazid neurotoxicity during preventive therapy. Crit Care Med 28:567–568
Watkins RC, Hambrick EL, Benjamin G, Chavda SN (1990) Isoniazid toxicity presenting as seizures and metabolic acidosis. J Natl Med Assoc 82:57–64
Schaberg T, Rebhan K, Lode H (1996) Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J 9:2026–2030
Morant J, Ruppaner H (2003) Compendium Suisse des Médicaments, 24th edn. Documed, Geneva
Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D (2003) Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med 167:1472–1477
Steele MA, Burk RF, DesPrez RM (1991) Toxic hepatitis with isoniazid and rifampin a meta-analysis. Chest 99:465–471
Saram GR, Imanuel C, Kailasam S, Narayana ASL, Venkatesan P (1986) Rifampin –induced release of hydrazine from isoniazid. A possible cause of hepatitis during treatment of tuberculosis with regiments containing isoniazid and rifampin. Am Rev Dis 133:1072–1075
Mitchell JR, Thorgeisson UP, Black M et al (1975) Increased incidence of isoniazid hepatitis in rapid acetylators : possible relation to hydralazine metabolites. Clin Pharmacol Ther 18:70–79
Black M, Mitchell JR, Zimmerman HJ, Ishak KG, Elper GR (1975) Isoniazid-associated hepatitis in 114 patients. Gastroenterology 69:289–302
Mitchell JR, Zimmerman HJ, Ishak KG, Thorgeisson UP, Timbrell JA, Snodgrass WR, Nelson SD (1976) Isoniazid Liver injury: clinical spectrum, pathology and probable pathogenesis. Ann Intern Med 84:181–192
Spielberg SP (1996) N-acetyltransferases: Pharmacogenetics and clinical consequences of polymorphism drug metabolism. J Pharmacokinet Biopharm 509–19
Singh J, Garg PK, Thakur VS, Tandon RK (1995) Anti-tubercular treatment induced hepatotoxicity: does acetylator status matter? Indian J Physiol Pharmacol 39:43–46
Ryan DE, Ramanathan L, Iilda S, Thomas PE, Hainu M, Shively JE, Lieber CS et al (1985) Characterisation of a major form of rat hepatic microsomal cytochrome P-450 induced by isoniazid. J Biol Chem 260:6385–6393
Cascorbi I, Drakoulis N, Brockmöller J, Maurer A, Sperling K, Roots I (1995) Arylamine N-acetyl transferase (NAT2) mutations and their allelic linkage in unrelated Caucasian individual: correlation with phenotypic activity. Am J Hum Gen 57:581–592
Parkin PD, VandenPlas S, Botha FJH (1997) Trimodality of isoniazid elimination. Phenotype and genotype in patients with tuberculosis. Am J Respir Crit Care Med 155:1717–1722
Smith CAD, Wadelius M, Gough AC, Harrison DJ, Wolf CR, Rane A (1997) A simplified assay for the arylamine N-acetyltransferase 2 polymorphism validated by phenotyping with isoniazid. J Med Genet 34:758–760
Ohno M, Yamaguchi I, Yamamoto I, Fukuda T, Yokota S, Maekura R, Ito M, Yamamoto Y, et al (2000) Slow N-acetyltransferase 2 genotype affects the incidence of isoniazid and rifampicin-induced hepatotoxicity. Int J Tuberc Lung Dis 4:256–261
Gurumutry P, Krishnamurthy MS, Nasareth O (1984) Parthasarthy R, Samara GR, Somasundaram PR, Tripathy SP et al (1984) Lack of relationship between hepatotoxicity and acetylator phenotype in three thousand south Indian patients during treatment with isoniazid for tuberculosis. Am Rev Respir Dis 129:58–61
Dickinson DS, Bailey WC, Hirschowitz BI, Soong SJ, Eidus L, Hodgkin MM (1981) Risk factors for isoniazid (INH)-induced liver dysfunction. J Clin Gastroenterol 3:271–279
Lieber CS (1997) Cytochrome P-4502E1: its physiological and pathological role. Physiol Rev 77:517–544
Tanaka E, Terarda M ,Misawa S (2000) Cytochrome P4502E1.Its clinical and toxicological role. J Clin Pharm Ther 25:165–175
Lucas D, Ferrara R, Gonzales E, Albores A, Manno M, Berthou F (2001) Cytochrome CYP2E1 phenotyping and genotyping in the evaluation of health risks from exposure to polluted environments. Toxicol Lett 124:71–81
Wong NACS, Rae F, Simpson KJ, Murray GD, Harrison DJ (2000) Genetic polymorphism of cytochrome p4502E1 and susceptibility to alcoholic liver disease and hepatocellular carcinoma in a white population: a study and literature review, including meta analysis. J Clin Pathol Mol Pathol 53:88–93
Haufroid V, Buchet JP, Gardinal S, Lison D (2002) Cytochrome P4502E1 phenotyping by the measurement of the chlorzoxazone metabolic ratio: assessment of its usefulness in workers exposed to styrene. Int Arch Occup Environ Health 75:453–458
Huang YS, Chern HD, Su WJ, Wu JC, Lai SL, Yang SY, Chang FY et al (2003) Cytochrome P450 2E1 genotype and the susceptibility to antituberculous drug-induced hepatitis. Hepatology 37:924–930
Huang YS, Chern HD, Su WJ, Wu JC, Lai SL, Yang SY, Chang FY et al (2002) Polymorphism of the N-acetyltransferase 2 gene as a susceptibility risk factor for antituberculosis drug-induced hepatitis. Hepatology 35(4):883–889
American Thoracic Society (2000) Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recommendation Rep 49:1–51
Kopanoff DE, Snider DE, Caras GJ (1978) Isoniazid related hepatitis : A US public health service cooperative surveillance study. Am Rev Resp Dis 117:991–1001
Ozick LA, Jacob L, Comer GM, Lee TP, Ben-Zvi J, Donelson SS, Felton CP (1995) Hepatotoxicity from isoniazid and rifampin in inner-city AIDS patients. Am J Gastroenterol 90:1978–1980
Guruprasad P. Aithal GP, Rawlins MD, Day CP (2000) Clinical diagnostic scale: a useful tool in the evaluation of suspected hepatotoxic adverse drug reactions. J Hepatol 33:949–952
Guo SW, Thompson EA (1992) Performing the exact test of Hardy-Weinberg proportion for multiple alleles. Biometrics 48:361–372
Xie HG, Xu ZH, Ou-Yang DS, Shu Y, Yang DL, Wang JS, Yan XD et al (1997) Metaanalysis of phenotype and genotype of NAT2 deficiency in Chinese population. Pharmacogenetics 7:503–514
Cascorbi I, Roots I (1999) Pitfalls in N-acetyltransferase-2 genotyping. Pharmcogenetics 9:123–127
Aynacioglu AS, Cascorbi I, Mrozikiewics PM, Roots I (1997) Arylamine N-acetyltransferase (NAT2) genotypes in a Turkish population. Pharmacogenetics 7:327–331
Mandell GL, Petri WA (1996) Antimicrobial agents. In: Goodman G (eds) The pharmacological basis of therapeutics 9th edn. Donnelley and Sons, Chicago, Ill., pp 1155–1174
Branch RA, Adedoyin A, Frye RF, Wilson JW, Romkes M (2000) In vivo modulation of CYP enzymes by quinidine and rifampin. Clin Pharmacol Ther 68:401–411
Zand R, Nelson SD, Slaterry JT, Thummel KE, Kalhorn TF, Adams SP, Wright JM (1993) Inhibition and induction of cytochrome P4502E1-catalysed oxidation by isoniazid in humans. Clin Pharmacol Ther 54:142–149
Hwang SJ, Wu JC, Lee CN, Yen FS, Lu CJ, Lin TP, Lee SD (1997) A prospective clinical study of isoniazid-rifampicin-pyrazinamid-induced liver injury in an area endemic for hepatitis B. J Gastroenterol Hepatol 12:87–91
Wong WM, Wu PC, Yuen MF, Cheng CC, Yew WW, Wong PC, Tam CM et al (2000) Antituberculosis drug-related liver dysfunction in chronic hepatitis B infection. Hepatology 31:201–206
Yamamoto T, Suou T, Hirayama C (1986) Elevated serum amino-transferase induced by isoniazid in relation to isoniazid acetylator phenotype. Hepatology 6:295–298
American Thoracic Society (1994) Treatment of tuberculosis and tuberculosis infection in adults and children. Am J Resp Crit Care Med 149:1359–1374
Acknowledgements
We are indebted to Dr, J.-D. Graf for the resolution of Hardy-Weinberg equation, to Dr. V. Rollason for the revision of the manuscript, to the nurses of the Anti-tuberculosis Centre and the staff of the Central Laboratory of Chemistry for their technical support. This experiment complies with the current laws of Switzerland in which it was performed inclusive of ethics approval.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vuilleumier, N., Rossier, M.F., Chiappe, A. et al. CYP2E1 genotype and isoniazid-induced hepatotoxicity in patients treated for latent tuberculosis. Eur J Clin Pharmacol 62, 423–429 (2006). https://doi.org/10.1007/s00228-006-0111-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0111-5