Abstract
Objective
To evaluate the appropriate prescription of antiplatelets according to patients’ global cardiovascular risk level in everyday practice.
Methods
In a cross-sectional study, general practitioners (GPs) identified a random sample of 10% of patients at cardiovascular risk among all subjects coming to the surgery and collected data on cardiovascular risk factors and history of atherosclerotic cardiovascular diseases (CVD). GPs were asked to do a physical examination and record the results of laboratory tests to define the global cardiovascular risk. The use of antiplatelet drugs in patients with established CVD and in healthy subjects at high risk of developing symptomatic atherosclerotic disease was evaluated.
Results
A total of 162 GPs from all over Italy recruited 3,120 subjects (51% female, mean age 64 years). Of the 949 with an indication for antiplatelet treatment for secondary prevention of CVD, 442 (47%) were receiving it. Among the 2,071 without CVD, 11% were taking an antiplatelet drug. In this group, antiplatelets were prescribed in 6, 10, 16 and 23%, respectively, of patients perceived by GPs to be at mild, moderate, high and very high cardiovascular risk.
Conclusions
Prescription of antiplatelets still seems to be far from what is recommended in virtually all patients with a history of CVD. In subjects with cardiovascular risk factors but without CVD antiplatelet prescription increases in relation to global cardiovascular risk but is still low in patients at high or very high risk of cardiovascular events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefit of antiplatelet treatment for patients with atherosclerotic cardiovascular disease (CVD) is well established and it has long been widely recommended in the “secondary” prevention of cardiovascular events. Systematic reviews [1–3] show that the benefits of antiplatelet drugs largely outweigh the risk of major bleeding in patients with prior myocardial infarction (MI), stroke, transient ischaemic attack (TIA), coronary artery bypass graft (CABG) or percutaneous transluminal coronary angioplasty (PTCA), or with angina pectoris and peripheral artery disease (PAD). Many studies suggest that antiplatelet drug use among patients with CVD is still inadequate and that prescription patterns are far from what is recommended [4–11], although some studies [12–14] reported an increase in the last few years.
During the second half of the 1990s, evidence accumulated of a benefit of aspirin in patients at high risk of developing symptomatic atherosclerotic disease [15–17]. It has subsequently become increasingly clear that the net benefit of aspirin increases with the level of cardiovascular risk [18, 19], and antiplatelet treatment is now considered worthwhile and recommended in asymptomatic patients at high coronary risk [20].
Studies focusing on antiplatelet use in primary prevention are few [21, 22], and none has considered prescriptions in everyday practice in relation to the overall cardiovascular risk. As part of the feasibility phase for a large intervention study on cardiovascular prevention in patients at high cardiovascular risk, we launched a pilot epidemiological study to evaluate how patients at cardiovascular risk are usually treated in general practice. The analyses reported here assess whether antiplatelets are appropriately prescribed according to patients’ global cardiovascular risk.
Methods
A network of general practitioners (GPs) from all over Italy was invited to enter a cross-sectional study on the cardiovascular preventive strategies adopted in everyday practice. GPs were members of research working parties who had participated in previous collaborative studies with our Institute. Among all subjects coming to the surgery for any reasons from May to December 2000, each GP identified a random sample of patients aged 40–80 years perceived as being at cardiovascular risk because of at least one known risk factor or established atherosclerotic disease. All patients who met these criteria were consecutively entered in a register in which a random sequence picked out 1 in 10 for inclusion in the study, for up to 20 patients. GPs had to collect data on known cardiovascular risk factors (history of hypertension, diabetes, hyperlipidaemia, if patients were obese, current smokers or had a family history of premature MI) and on the history of CVD (MI, stroke, TIA, CABG or PTCA, angina pectoris and PAD). GPs were also asked to carry out a physical examination [including measurement of blood pressure (BP), height and weight] and record the results of recent laboratory tests (plasma lipids and glucose in all patients and HbA1c in diabetics). On the basis of all the data, GPs were asked to subjectively estimate for each patient the overall level of cardiovascular risk, rating it as mild, moderate, high or very high. The 10-year overall risk of lethal cardiovascular events for each patient was also calculated according to the SCORE Risk Chart for people living in low-risk countries [23].
Data on chronic treatments were also gathered, and we focused particularly on antiplatelets. We excluded all patients with atrial fibrillation since they have an indication to antithrombotic drugs for the prevention of embolic complications. At the time of the survey antiplatelets were recommended in all patients with established atherosclerotic disease [24] and two trials had shown benefits of aspirin even in asymptomatic individuals at high cardiovascular risk [15, 16]. Accordingly, we considered the prescription of antiplatelets appropriate in all patients with a history of CVD and those with no history of CVD but at high cardiovascular risk.
Statistical analyses
In patients with established CVD and in asymptomatic individuals at high cardiovascular risk, we examined the association between antiplatelet prescription and age, sex, GPs’ perceptions of patients’ risks and number of other cardiovascular drugs taken. For those who had already experienced a cardiovascular event (MI, TIA, stroke, CABG/PTCA) we analysed the association with time from occurrence. For patients with CVD, we examined the association with the number of previous events or diseases. For patients without CVD, we examined the association with the number of cardiovascular risk factors and, in the 1,672 with complete data for the overall risk assessment, we established their level of risk according to the SCORE Risk Chart. In the latter group of patients, we also analysed antiplatelet prescriptions according to their BP levels.
Descriptive statistics (numbers and percentages for discrete variables) were generated for baseline characteristics and frequencies of treatment. Groups of patients were compared using χ2 tests for differences in proportions of categorical variables; tests were two-sided and P<0.05 was considered significant. In order to assess whether sex, age, number of other risk factors (variable included only in primary prevention analyses) and time from event (variable included only in secondary prevention analyses) were independently associated with antiplatelet prescription, a multivariate logistic regression was undertaken. To evaluate the possible cluster effect due to similar attitudes in prescriptions by GPs, the multivariate analyses were adjusted for the number of physicians in the study. Multivariate analyses were run separately for secondary and primary prevention.
Results
A total of 162 GPs enrolled 3,120 subjects [1,581 women (51%), mean age 64±9.3 years], 949 (31%) with and 2,071 (69%) without a history of CVD; 98 patients (3%) with atrial fibrillation were excluded from the analysis.
Information on the use of antiplatelets was available for all cases. We found 667 prescriptions of an antiplatelet drug; 74% were aspirin, 20% ticlopidine and the remaining 6% other drugs.
Baseline characteristics of the population with CVD are shown in Table 1a. Previous MI was the more common CVD (42%), followed by angina pectoris (34%) and previous CABG/PTCA (28%). A total of 27% and 15%, respectively, had experienced two or three or more cardiovascular events/diseases.
The characteristics of the population with risk factors but no history of CVD are shown in Table 1b. Hypertension and hyperlipidaemia were the most frequent risk factors (83% and 44%). One-third of the subjects had just one major cardiovascular risk factor, 40% had two and 34% three or more. Overall, 16% of subjects were considered at mild risk, 41% at moderate, 34% at high and 9% at very high risk of cardiovascular events.
Antiplatelet treatment in secondary prevention
Of 949 subjects with a history of CVD, 442 (47%) had received a prescription for an antiplatelet drug. Treatment rates varied between 51% in patients with previous TIA or CABG/PTCA and 46% in patients with PAD. Table 2 shows that there was no appreciable difference in the treatment rate according to age and sex. While 43% of patients with only one cardiovascular event or disease were treated, 50% and 54%, respectively, of those with two and three or more were treated.
Antiplatelet prescription was inversely associated with time from the event: patients who had experienced a recent event were more likely to be treated than the others, with the highest treatment rate among those who had had an event in the last year (59%).
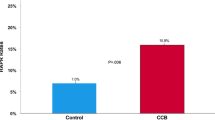
The number of other cardiovascular drugs used did not seem to be related to antiplatelet prescriptions. Those who took one or two other cardiovascular drugs were treated as much as those needing three to four or more than four drugs (47, 47 and 46%, respectively). In these high-risk patients, the antiplatelet prescription rate did not seem to be related to GPs’ perceptions of the level of cardiovascular risk (Fig. 1).
Multivariate analysis confirmed the inverse association between antiplatelet prescription and time from the event (RR=0.78; CI 95% 0.68–0.88; P=0.0001) while age, sex and GPs’ cluster effect were not significant.
Antiplatelet treatment in primary prevention
Among the 2,071 patients with no history of CVD, 225 (11%) were taking an antiplatelet drug. Treatment rates varied from 14% in diabetics and in patients with a family history of premature MI to 13% in hyperlipidaemics, 12% in hypertensives, 11% in obese patients and 9% in smokers.
The variables associated with antiplatelet drug prescription are reported in Table 3. There was a clear relationship between the probability of prescription and advanced age, total number of risk factors and the cardiovascular risk score (obtained by separating the population into the five levels of the SCORE Risk Chart).
The prescription rate did not seem to be related to BP, as we found the same percentage of patients treated with antiplatelets among well-controlled and poor-controlled ones: 11% of prescriptions in patients with a BP less than 140/90 mmHg (81/766), in those with 140–159/90–99 mmHg (110/995) and in those with a BP of 160/100 mmHg or higher (34/310).
Patients treated with a larger number of other cardiovascular drugs were more likely to also receive antiplatelet drugs (24% who took more than four drugs were treated with antiplatelets versus 8% of those who took only one to two drugs, P<0.0001).
The antiplatelet prescription rate was related to the GP’s perception of the level of cardiovascular risk, with a clear pattern from 6% of patients considered at mild risk to 23% of those considered at very high cardiovascular risk; P=0.001 (Fig. 1).
Multivariate analysis confirmed the association between antiplatelet prescription and age (RR=1.06; CI 95% 1.05–1.08; P<0.0001) and number of cardiovascular risk factors (RR=1.43; CI 95% 1.24–1.64; P<0.0001), while sex and GPs’ cluster effect were not significant.
Discussion
Despite a positive pattern of antiplatelet drug prescription in relation to global cardiovascular risk level, antiplatelets still seem under-used, both in patients with established CVD and in asymptomatic subjects at high or very high risk of developing cardiovascular events. While the relatively limited use of these drugs in secondary prevention confirms the sub-optimal treatment rate already reported in many other populations and settings [4–10, 12–14, 25], our data indicate for the first time that, even in patients without CVD, but considered by the GPs at high cardiovascular risk, antiplatelets are seldom used.
Antiplatelet prescription in secondary prevention
Fewer than half of the patients with a history of CVD took antiplatelets, with no appreciable differences among sub-groups with different manifestations of atherosclerotic disease. Although there was a tendency for prescription to reflect the number of cardiovascular events/diseases and the proximity of thrombotic events, the prescription rate was much lower than expected even in patients with multiple diseases or recent cardiovascular events.
Neither the prescription of other antithrombotic drugs such as oral anticoagulants nor polypharmacy seems to explain the low rate of antiplatelet prescription, since oral anticoagulants were prescribed to only 6% of the total population and no association was found between the number of other cardiovascular drugs taken and the use of antiplatelets. Other possible reasons for the low use of antiplatelets might be a history of side effects, the presence of contraindications or poor compliance with treatment. As we did not collect this information, we cannot speculate on these issues. Nevertheless, the high percentage of untreated patients can hardly be explained by these factors alone [17, 26].
Antiplatelet prescription in primary prevention
In subjects with cardiovascular risk factors but without CVD, antiplatelet prescription is low—one out of ten—but increases in relation to the patient’s level of risk, either “subjectively” estimated by GPs or calculated by two “objective” methods such as risk chart score or the number of concomitant risk factors. Despite this trend, antiplatelet use is still exceptional in patients at high or very high risk of cardiovascular events.
The few studies investigating antiplatelet use in primary prevention reported similar findings in diabetics and other subjects at high risk [21, 22], but none has evaluated prescriptions in relation to the GP’s perception of a patient’s cardiovascular risk level.
Antiplatelet prescription was uniform across patients with different cardiovascular risk factors despite the fact that the literature offers sound positive evidence of benefit in well-controlled hypertensives [15] and, on the contrary, the lack of evidence of benefit in diabetics [27]. On the other end, the low rate of prescription of antiplatelets in the large number of hypertensives was not due to the common condition of uncontrolled hypertension. As in secondary prevention, not even polypharmacy seems to explain the low rate of antiplatelet prescription in primary prevention: in fact GPs seemed more likely to prescribe an antiplatelet drug to patients already taking a larger number of other cardiovascular drugs, very likely reflecting the presence of multiple risk factors.
The low rate of antiplatelet prophylaxis among asymptomatic high-risk patients in our series may have several causes; some indicative of inadequacies of medical management, some related to the patients’ clinical profiles or viewpoint. While for secondary prevention there is long-standing strong evidence that antiplatelet treatment has a clearly favourable risk/benefit profile, in primary prevention the evidence is more recent, the absolute benefit is smaller and there is still some uncertainty about the cardiovascular risk level above which aspirin should be recommended.
In general practice, the decision to start long-term therapy is made jointly with the patient. In asymptomatic individuals, risk perception as well as personal beliefs and values may play an important role in the decision to agree to recommended long-term prophylaxis [28]. Patients’ underestimates of their own risk may lead to a low acceptance rate [29]. The lack of information about patients’ own risk perception and their reluctance to take antiplatelets limit the possibility of assessing the importance of these factors in our population.
One possible limitation of our study is the selection of physicians. This is likely to be a selected sample of physicians more sensitive to the issue of cardiovascular prevention and therefore only partially representative of the whole category. The prescription of antiplatelet drugs in everyday practice may consequently be even lower than indicated by our data. Another possible bias could be due to a cluster effect in the GPs’ attitudes to the prescription of antiplatelets. However, we could reasonably exclude this since, on adjusting the multivariate analyses for the number of GPs, the results did not show any significant cluster effect.
Conclusions
Our findings suggest that, despite all evidence, antiplatelet drugs are still not widely used in daily practice and the majority of patients who would benefit from this effective, safe and cheap treatment (i.e. patients with established CVD and healthy subjects at high risk of developing symptomatic atherosclerotic disease) still remain at risk of cardiovascular events.
There is a need for general practice-based studies to explore the reasons for the gap between recommended behaviour and real practice, including GPs’ and patients’ perspectives. This was a feasibility phase for a large prospective study that is currently ongoing on the optimisation in everyday practice of cardiovascular prevention in high-risk patients. A specific aim of the study is to investigate why evidence-based strategies, in cardiovascular prevention, including antiplatelets, are not implemented in practice.
References
Antiplatelet Trialists Collaboration (1994) Collaborative overview of randomised trials of antiplatelet therapy, I: prevention of death, myocardial infarction and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 308:82–105
Antiplatelet Trialists Collaboration (2002) Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction and stroke in high risk patients. BMJ 324:71–86
Patrono C, Bachmann F, Baigent C et al (2004) Expert consensus document on the use of antiplatelet agents. The Task Force on the use of antiplatelet agents in patients with atherosclerotic cardiovascular disease of the European Society of Cardiology. Eur Heart J 25:166–181
Svilaas A, Thorensen M, Kristoffersen JE, Hjartaaker J, Westeheim A (2000) How well are patients with atherosclerotic disease treated? Secondary prevention in primary care. Scand J Prim Health Care 18:232–236
Brady AJB, Oliver MA, Pittard JB (2001) Secondary prevention in 24,431 patients with coronary heart disease: survey in primary care. BMJ 322:1463
Welton M, Croft P, Welton J (1999) General practitioners’ use of aspirin in the secondary prevention of vascular events: knowledge, attitudes, and current practice. Br J Gen Pract 49:607–610
Campbell NC, Thain J, Deans HG, Ritchie LD, Rawles JM (1998) Secondary prevention in coronary heart disease: baseline survey of provision in general practice. BMJ 316:1430–1434
Brown JB, Delea TE, Nichols GA, Edelsberg J, Elmer PJ, Oster G (2002) Use of oral antithrombotic agents among health maintenance organization members with atherosclerotic cardiovascular disease. Arch Intern Med 162:193–199
Bradley F, Morgan S, Smith H, Mant D (1997) Preventive care for patients following myocardial infarction. Fam Pract 14:220–226
Harder S, Thurmann P, Thierolf C, Klepzig H (1998) Prescription of cardiovascular drugs in outpatient care: a survey of outpatients in a German University Hospital. Int J Clin Pharmacol Ther 36:195–201
Euroaspire II Group (2001) Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries. Principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J 22:554–572
Stafford RS (2000) Aspirin use is low among United States outpatients with coronary artery disease. Circulation 101:1097–1101
Martinez M, Agustí A, Arnau JM, Vidal X, Laporte JR (1998) Trends of prescribing patterns for the secondary prevention of myocardial infarction over a 13-year period. Eur J Clin Pharmacol 54:203–208
Stafford RS, Radley DC (2003) The underutilization of cardiac medications of proven benefit, 1990 to 2002. J Am Coll Cardiol 41:56–61
Hanson L, Zanchetti A, Carruthers SG, et al (1998) Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 351:1755–1762
Thrombosis prevention trial (1998) randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The Medical Research Council’s General Practice Research Framework. Lancet 351:233–241
Collaborative Group of the Primary Prevention Project (PPP) (2001) Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Lancet 357:89–95
Sanmugananathan PS, Gharamani P, Jackson PR et al (2001) Aspirin for primary prevention of coronary heart disease: safety and absolute benefit related to coronary risk derived from meta-analysis of randomised trials. Heart 85:265–271
Hayden M, Pignone M, Phillips C, Mulrow C (2002) Aspirin for the primary prevention of cardiovascular events: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 136:161–172
De Backer G, Ambrosioni E, Borch-Johnsen K et al (2003) European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur J Cardiovasc Prev Rehabil 10(Suppl1):S1–S78
Rolka DB, Fagot-Campagna A, Venkat Narayan KM (2001) Aspirin use among adults with diabetes. Diabetes Care 24:197–201
Stafford R, Ma J (2004) Continued suboptimal use of aspirin in patients at high and moderate risk for CHD events. J Gen Intern Med (Suppl1):133
Conroy RM, Pyörälä K, Fitzgerald AP, et al (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24:987–1003
Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyorala K (1998) Prevention of coronary heart diseases in clinical practice: recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. Atherosclerosis 140:199–270
Filippi A, Bignamini AA, Sessa E, et al (2003) Secondary prevention of stroke in Italy. A cross-sectional survey in family practice. Stroke 34:1010–1014
Collaborative Group of the Primary Prevention Project (1995) Epidemiological feasibility of cardiovascular primary prevention in general practice: a trial of vitamin E and aspirin. J Cardiovasc Risk 2:137–142
ETDRS Investigators (1992) Aspirin effects on mortality and morbidity in patients with diabetes mellitus: Early Treatment Diabetic Retinopathy Study report 14. J Am Med Assoc 268:1292–1300
Short D, Frischer M, Bashford J, Ashcroft D (2003) Why are eligible patients not prescribed aspirin in primary care? A qualitative study indicating measures for improvement. BMC Fam Pract 4(1):9
Ferrario G, Alkhimovitch O, Avanzini F, et al (2004) People’s perception of their overall coronary risk: an Italian experience. Ital Heart J 5(1):16–21
Acknowledgements
We would like to thank Dr. Vittorio Bertele’ for helpful comments on the manuscript, Fiorenza Clerici, Guya Sgaroni and Angela Palumbo for careful secretarial assistance in the management of the study and in preparing the paper, and Judith Baggott for editorial assistance. An educational grant was provided by Pharmacia Upjohn and Società Prodotti Antibiotici (SPA) for the coordination expenses.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors wrote this article on behalf of the Collaborative Group Risk and Prevention Study. A full list of investigators is reported in the Appendix.
conflict of interest: none
Appendix
Appendix
General practitioners
Adinolfi D. (Pozzuoli); Agneta A. (Montalbano Jonico); Alberino S. (Chiusdino); Alexanian A. (Milano); Anglano B. (Parona-Verona); Aronica A. (Milano); Bagagli F. (Torino); Balzan C. (Trichiana); Barba G. (Talsano); Baron P. (Palmanova); Barone A. (Albano di Lucania); Bedon R. (Casale Monferrato); Benetti R. (Casale sul Sile); Berton G. (Castelfranco Veneto); Besozzi E. (Castelletto sopra Ticino); Bevilacqua S. (Viterbo); Bizzarri G. (Cannara); Boldini L. (Torbole Casaglia); Bonzi G. (Ostiano); Bosisio Pioltelli M. (Monza); Bozzetto R.M. (Breganze); Brocchi A. (Cortona); Brizzi A. (Terlizzi); Bruno B. (Montereale); Burbi M. (Cortona); Buzzatti A. (Sedico); Cadioli T. (Carpi); Caimi V. (Monza); Calciano F.P. (Grassano); Calienno S. (Monza); Caltagirone P. (Castelnuovo di Isola Vic.); Capelli O. (Montefiorino); Casella M. (Caserta); Casella P. (Caserta); Caso C. (Mercato San Severino); Cassanelli M. (Castelfranco Emilia); Catalano A. (San Leucio del Sannio); Ciociano C. (Sarno); Coazzoli E. (Milano); Colecchia G. (Massa); Colombo I. (Boffalora sul Ticino); Conti M. (Castiglion Fiorentino); Corti N. (Scandiano); Corvino P. (Caserta); Cotroneo S. (Villa San Giovanni); Cozzani L. (Ponte di Arcola); Cuffari A. (Marino); Cuozzo E. (Napoli); Cusmai L. (Foggia); D’Anna M.A. (Milano); Danti G. (Buttapietra); De Cesare G. (Caserta); De Maria E. (Napoli); De Maria R. (Milano); De Matteis D. (Belvedere Spinello); Del Carlo A. (Viareggio); Dell’Aquila A.M. (Caserta); De Sire G. (Caserta); Di Giovambattista E. (Magnano in Riviera); Di Giuseppe M. (Carnate); Dionette M.G. (Scano di Montiferro); Ermacora T. (Maiano); Fastidio M. (Milano); Ferrari V. (Parabita); Ferreri A. (Cigoli San Miniato Basso); Filippi S. (Pontremoli); Fortunato S. (Montoro Inferiore); Fossati B. (Monza); Fumagalli M.A. (Senago); Galimberti G. (Como); Galli G. (Licciana Nardi); Galopin T. (Verona); Gambarelli L. (Scandiano); Gangi F. (Pasian di Prato); Gardinale E. (Milano); Gasparin A. (Pordenone); Gasparri R. (Mansue’); Gelardi M. (Urbino); Gentile M. (Terni); Germano S. (Avola); Germini F. (Perugia); Giugliano R. (Pozzuoli); Guerra C. (Aprilia); Guerrini A. (Piangipane); Idone A. (Catona); Lattuada G. (Uboldo); Lippa L. (Avezzano); Lombardi P. (Milano); Longoni P. (Milano); Lorello M. (Napoli); Maggioni A. (Ala); Malavasi P. (Carpi); Manni A. (Scandiano); Mao M. (Torino); Marazzi M. (Mirandola); Mariangeloni A. (Terontola); Maruzzi G. (Cantù); Masperi M. (Abbiategrasso); Massa E. (Cittadella); Mastella M. (Foza); Mezzacapo G. (Veroli); Mingarelli C. (Aprilia); Mingione F. (Puccianiello); Minotta F. (Pozzuoli); Misiani V. (Reggio Calabria); Montecchio G. (Abbiategrasso); Moretti S. (Caserta); Morini M. (Cotignola); Moro A. (Preganziol); Nasorri R. (Terontola); Nicoli S. (Borgo di Terzo); Nicolosi M. (Torino); Orlando V. (Caserta); Paci C. (Gioia del Colle); Palatella A. (Foggia); Panigada M. (Bergamo); Panza E.G. (Bollate); Parini P.C. (Vittuone); Paroli G. (Galleno); Patafio M. (Scilla); Pedroni M. (Scandiano); Perone V. (Caserta); Perugini I. (Capranica); Petrera L. (Castellaneta); Piazza G. (Santorso); Piccolo F. (Bisceglie); Pignatti M. (S. Giovanni in Persiceto); Pinto D. (Monopoli); Pirovano E. (Milano); Pirrotta D. (Scilla); Pulcino Lupo G. (Caserta); Rafanelli P. (Firenze); Ramunni A. (Conversano); Recusani A. (Parma); Ribetto Bruno M. (Villar Perosa); Ricciarini P. (Lucignano); Rinchi F. (Cortona); Riva M.G. (Monza); Rossi C. (Casagiove); Rossi R. (Urbino); Rossitto A. (Taranto); Russo V. (Pozzuoli); Sagnelli C. (Maddaloni); Savignano L.C. (Casagiove); Scattolari G. (Urbino); Sissa F. (Virgilio); Sizzano E. (Trivero); Sproviero A.M. (Pozzuoli); Sproviero S. (Pozzuoli); Stranges M. (Caserta); Talia R. (Villa San Giovanni); Tedesco A. (Guradavalle); Titta G. (Torino); Tomba A. (Valdagno); Tosetti C. (Porretta Terme); Uberti M. (Torino); Vece R. (Eboli); Vincenti G. (Sarzana); Visentini E. (Sant’Angelo di Piove di Sacco); Vitali F. (Castiglione del Lago); Vitaloni E. (Abbiategrasso); Zannier P. (San Giuliano Milanese); Zappone P. (Palmi); Ziccardi F. (San Clemente); Zitiello V. (San Marco Evangelista); Zizzo F. (Lissone); Zorzi C. (Ziano di Fiemme).
Data management and statistics
Clerici F.1, Colombo F.1, Barlera S.1, Palumbo A.1, Sgaroni G.1
Scientific committee
Aronica A.2, Avanzini F.1, Caimi V.3, Lauri D.1, Longoni P.2, Marchioli R.4, Monesi L.1, Roccatagliata D.1, Roncaglioni MC.1, Tognoni G.1, Tombesi M.3, Visconti M.2
1 Istituto di Ricerche Farmacologiche “Mario Negri”, Milano; 2 CoS, Milano; 3 CSeRMEG, Monza; 4 Consorzio “Mario Negri Sud”, Santa Maria Imbaro.
Rights and permissions
About this article
Cite this article
Monesi, L., Avanzini, F., Barlera, S. et al. Appropriate use of antiplatelets: is prescription in daily practice influenced by the global cardiovascular risk?. Eur J Clin Pharmacol 61, 595–601 (2005). https://doi.org/10.1007/s00228-005-0948-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-005-0948-z