Abstract
Objective
To investigate the prevalence of current use of benzodiazepines (BZDs) and related drugs in the French general population and factors associated with this use.
Methods
National cross-sectional telephone survey conducted between 25 April 2001 and 8 May 2001 in a representative sample of non-institutionalized adults of BZD use and duration, prescriber specialty, socio-demographic data and mood and anxiety disorders, using a structured diagnostic interview.
Results
The prevalence of current use of BZD was 7.5%. It was higher among women (9.7%) than men (5.2%). It increased with age and was higher in the jobless (10.9). Duration of BZD use was more than 6 months in 75.9% of users and increased with age. Of the 711 (17.7%) subjects with at least one mood or anxiety disorder, 122 (17%) used BZD compared with180 (5.5%) of the 3296 subjects without mood or anxiety disorders. In multivariate analysis, factors associated with BZD use were age [odds ratio (OR): 3.6; 95% confidence interval (CI) 2.0–5.6], 6.5 (4.1–10.3) and 10.9 (6.9–17.1), respectively, for ages 35–44 years, 45–59 years and over 60 years compared with below 34 years, female gender (OR: 1.7; 95% CI 1.3–2.1), anxiety only (OR: 2.2; 95% CI 1.5–3.2), mood disorder only (OR: 4.4; 95% CI 2.7–7.1) or both mood and anxiety disorders (OR: 8.8; 95% CI 5.9–12.6).
Conclusion
Despite precautions, warnings and attempts to limit use, there remains a high proportion of long-term BZD users in the general French population, especially in the elderly. Our findings add to the weight of opinion that messages concerning proper use of BZDs certainly need to be clarified and amplified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benzodiazepines (BZDs) are among the most widely used drugs in the general population [1–6]. They have been a focus of concern in recent years, not only because of the extent of their use but also because of their association with dependence and withdrawal reaction upon discontinuation [7–9], as well as a range of possible consequences, such as a higher risk of traffic accidents [10], falls [11] and cognitive impairment [12], particularly among elderly users. Their effect on hip fracture remains disputed [13–16]. Many epidemiological studies have found increasing use of BZDs with age and the female gender. BZD use has always been thought to be especially high in France [6, 17] but without clear quantification or estimation of the weight of various factors such as age, gender, socio-professional status or concomitant psychiatric disorders. Moreover, drug utilization is variable over time [18] and space [19], justifying regular monitoring of usage patterns to guide possible interventions. In addition, there have been many recommendations to limit the use of BZDs, especially in the elderly, including limiting the duration of prescription to 4 weeks for the hypnotics and 12 weeks for BZDs used in anxiety since 1991 [20]. The results of these interventions have not been quantified recently.
To answer these points, in April–May, 2001, we conducted a cross-sectional survey of the patterns of anxiolytic–hypnotic medication use in a representative sample of the French population assessing prevalence, type of medication, prescriber speciality and concomitant mood or anxiety disorders that could justify the use of these drugs.
Population and methods
Study design and population
This was a cross-sectional telephone survey conducted between 25 April 2001 and 8 May 2001 in France, where 80% of all households are fixed-line telephone subscribers. The target population was non-institutionalized residents 18 years of age or over. Sampling of the study population was done by IPSOS France (http://www.ipsos.com), a company that routinely does marketing and political polls and surveys, using telephone sampling techniques based on a stratified random sampling: a list of random fixed-line telephone numbers was provided by France telecom; at that time, France telecom was the only provider of fixed phone numbers. Fixed phone numbers start by 01 to 05 according to geographic areas, whereas mobile phone numbers all start with 06, so that they are easy to separate. Numbers were stratified by geographic area and size of town. Telephone numbers were randomly selected in each stratum. Within each stratum, a quota sampling procedure was carried out [21] so that the age and gender structure of our population was representative of the age and gender structure of the entire population based on the 1999 population census provided by Institut National de la Statistique et des Etudes Economiques (INSEE, Paris—http://www.insee.fr).
The person who answered the phone was interviewed, not necessarily the line holder. If the person who answered was not within the quota needed for the stratum, the pollster asked whether there was anyone else in the home who could answer and who would be within a quota with free space.
Of the list of phone numbers provided by the phone company, 6358 were wrong numbers (fax, corporate, non-existing numbers) or could not be reached during the study period, 1221 were outside the quotas, 3906 refused to answer from the very start of the phone call, 60 refused to continue during the interview and 4007 completed the interview. Thus, of the 7973 persons who could be contacted and were eligible for the study, 50.3% participated, and only 0.7% refused to continue once they knew the subject of the study.
The age, gender and residence structure of the responder population was the same as that of the general French population according to a national census done in March 1999 (http://www.insee.fr).
Data collection
Interviews
Each subject answered a standardized phoned questionnaire, using a computer-assisted telephone interview system. There was no paper based data collection. Interviewers (n=24) from IPSOS, a company specializing in nation-wide telephone surveys, participated in the study. They received a special one-day training course on the use of the questionnaire, including the mini international neuropsychiatric interview (MINI) [22]. A supervisor monitored the interviewer team to ensure that questions were asked correctly, and the data was properly collected.
BZD use
Subjects were first asked if they currently took any medication, and any answer was noted and qualified as to the name of the drug(s) used. They were then asked specifically about the use of anxiolytics or hypnotics: “Are you currently taking medication to help you sleep or to reduce anxiety?”, using a structured oriented drug utilization questionnaire derived from previously studied and validated questionnaires [23, 24].
A positive response to the above prompted further questions as to the name of the medication used, its dosage and duration of intake and prescriber if the drug was a BZD or similar drug (zolpidem, zopiclone), identified from a list of these drugs. The term BZD in this paper refers indistinctly to BZD as such and to zolpidem or zopiclone.
Patients who declared the use of one or more BZD at the time of interview were considered current users of BZDs. BZDs were classified according to their elimination half-life, i.e., long (>24 h) or short (≤24 h). Drugs with long-elimination half-lives included chlordiazepoxide, clobazam, clonazepam, clorazepate, diazepam, loflazepate, nitrazepam, nordazepam and prazepam, while the drugs with short-elimination half-lives included alprazolam, bromazepam, clotiazepam, estazolam, flunitrazepam, loprazolam, lormetazepam, oxazepam, temazepam, tofizopam, triazolam, zolpidem and zopiclone.
Evaluation of anxiety and depression
After drug use had been recorded and irrespective of possible drug use or its nature, all subjects were explored using the MINI (MINI, French version 5.0.0) [22]. The MINI is an abbreviated structured psychiatric interview using decision tree logic to assess the major adult Axis I disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10). It elicits all the symptoms listed in the symptom criteria for DSM-IV and ICD-10 for 15 major Axis I diagnostic categories, one Axis II disorder and for suicidality. The diagnostic algorithms are consistent with DSM-IV and ICD-10 diagnostic algorithms. The MINI has been validated against the Structured Clinical Interview for DSM-III-R–Patient Edition (SCID-P) and the Composite International Diagnostic Interview (CIDI) 1.0 for ICD.-10 in a study of over 600 subjects at two sites, 300 in Tampa, Florida, USA and 300 at the Hôpital de la Salpêtrière in Paris, France [22]. In the present study, we used the seven sections of the MINI exploring major current or past depressive disorder, dysthymia, panic disorder, agoraphobia, social phobia, obsessive compulsive disorder and generalized anxiety. These disorders were then classified into three main categories including: (1) mood disorder only (depressive disorder or dysthymia), (2) anxiety disorder only (panic disorder, agoraphobia, social phobia, obsessive compulsive disorder and generalized anxiety) and (3) concomitant depressive and anxiety disorder (at least one diagnostic of each category).
Statistical methods
The main dependent variable was the current use of BZD. Potential correlates were: age, gender, professional activity (yes/no), the place of residence [rural (<25,000 inhabitants) or urban (>25,000 inhabitants)], living alone (yes/no), mood disorder only (present/absent), anxiety disorder only (present/absent) and concomitant depressive and anxiety disorder (present/absent).
Bivariate analyses were carried out with Chi-square statistics. Unconditional stepwise logistic regression was performed to identify risk factors associated with BZD use, with P to exclude set at 0.05 [25]. All the analyses were performed using STATA 7.0 packages, and level of significance was set at 0.05.
Results
Sample characteristics
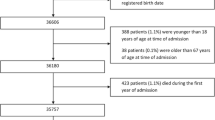
A total of 4007 subjects were interviewed for a target of 4000. Their mean age was 45 years, ranging from 18 years to 98 years. The sample included 2092 (52.2%) women and 1915 (47.8%) men. The socio-demographic characteristics of the study population are shown in Table 1. These were by design representative of the French general population. The description of drug use in this population is reported in Fig. 1.
BZD use
The prevalence of current BZD use was 7.5% (n=302). Most consumers took one BZD: 261 patients (86.4%) used one BZD, 39 (12.9%) used two BZDs and 2 (0.7%) used three BZDs concomitantly. Consumption was higher among women (9.7%) than men (5.2%, P<0.05). BZD use increased with age (Table 2). The prevalence of current use of BZD was not different between residents in urban areas compared with rural areas (7.49 versus 7.55%) but was higher in persons without professional activity compared with persons with professional activity (10.9 versus 4.9%, P<0.05).
Among BZD users, 268 (88.7%) used short half-life BZD and 34 (11.3%) used long half-life BZD. The most frequently reported drugs were bromazepam (33.4%), lorazepam (17.9%), alprazolam (13.9%), zolpidem (11.9%) and zopiclone (11.3%). Doses of BZD reported were within recommended doses. The duration of BZD use was more than 6 months in 76.5% of the users and increased with age (Table 3).
BZDs were prescribed by a general practitioner in 250 cases (82.8%) and a specialist in 50 cases (16.6%), including 26 psychiatrists (8.6%). In two cases, the source of prescription was reported as self-medication.
Mood and anxiety disorders
Among the study population, 711 (17.7%) subjects had at least one mood or anxiety disorder according to the MINI, 122 (17.2%) of whom were taking BZDs, while 180 (5.5%) of 3296 subjects without any mood or anxiety disorder were treated with BZDs. The detail of the diagnoses of mood and anxiety disorders are shown in Tables 4 and 5.
Factors associated with BZD use
The factors associated with BZD use were explored through multivariate logistic regression (Table 6). The use of BZD increased with age and was higher in the female gender. Presence of mood or anxiety disorders was also associated with a higher BZD use: an anxiety disorder alone doubled the rate of BZD use, mood disorders multiplied it by four and both together by eight. Factors such as living alone, professional activity or place of residence (urban/rural) were not associated with increased BZD use.
Discussion
Our population sample was representative of the general French adult population. The selection of this sample was performed according to standard polling methods by a professional polling corporation, IPSOS (http://www.ipsos.com). Persons who were not included were the 20% of the population without a personal fixed telephone line: persons in the lower socio-economic strata or living in communal homes (e.g. students, institutionalized older persons, prisoners) or using only portable phones (students, artists, young urban professionals?), including hospitalized persons. It is not known how this impacts the representability of our sample, so that our results should be seen as applying only to this mainstream population with a fixed telephone line. Use of BZDs was ascertained using a structured questionnaire, including the commercial names of the BZD on the French market, in addition to pathology-oriented questions [24]. This questionnaire has been validated against the presence of the drug in plasma [23], with generally good results. The MINI interview used to ascertain the mood and anxiety disorders is a standard, validated interview based on ICD-10 and DSM-IV [22], so that the positive information in this study is probably reasonably valid and representative of the real situation in the French general population. However, because of constraints in the maximal acceptable duration of the phone call, there are a number of points we could not ascertain with the same degree of confidence and, therefore, will not address. Though the list of concomitant medication, for instance, was asked for and recorded, they were not ascertained to the same degree of precision as BZD, which is the reason why we do not give the rates of, for example, antidepressant use. In the same way, we did not ascertain concomitant somatic diseases, which in any event could probably not have been validated without going back to medical records, an infeasible proposition considering the study design. This study may be thought unusual because it relies only on patient interviews. We did not assess psychiatric disorders other than mood and anxiety disorders. Only MINI was administered, so that there may be a number of false positives and negatives. Nevertheless, we found rates of mood and anxiety disorders quite similar to what was expected. For instance, the rate of major depressive disorder (7.9%) is perfectly in line with studies in the same population (5% and 8% for men and women, respectively) by Lepine and Lellouch [26] . The same consistency was found for anxiety: 14.6% in our study compared with 14% for women and 5% for men [26].
In the French general population, approximately 1 in 13 adults used BZD at the time of interview. This seems coherent with the frequency of use of BZD already reported in the French general population [27–31] from older studies. The French national Healthcare Insurance System, during the year 2000, found that 17.4% of the general population had redeemed at least one prescription for anxiolytics and 8.8% at least one prescription for hypnotics [6]. Considering the distribution of refills over the year, one would expect that between 6.5% and 9% of the users had redeemed a prescription during any given month and would be considered a user during that time.
We found no influence of place of residence or socio-professional status on the use of BZD. Though other authors did find that the local environment and interactions with neighbors could change BZD usage patterns [32], we could not reproduce this finding. Of BZD users, 40% had indications of mood or anxiety disorders. Among these, the largest user group (37%) had agoraphobia, social phobia, panic disorders or obsessive compulsive disorders, indications where BZDs were long thought of little value, although recent data from clinical trials seem to show some effect, at least with alprazolam [33–36] or clonazepam [37, 38]. A total of 23% of the users had major depressive disorder, an indication which may also not be without merit, although only for the first 6–8 weeks [39]. This represents 15–28% of subjects with these disorders. In the same way, only 22% of the patients with signs of generalized anxiety disorder, which one could expect to be a prime indication for BZD use [40, 41], actually took them. Interestingly, the odds of having BZD were doubled when anxiety disorders were present but multiplied by four when moods disorders were found. One would expect the use of BZD to be more often associated with anxiety than with depression, although this separation could be somewhat artificial [42].
A total of 5.5% of subjects without any detected mood or anxiety disorder used BZD, representing 4.5% of the total population or 60% of all BZD users. This would represent overall at least 2 million users in France that take BZDs without any of the psychiatric disorders we looked for, more users than have these disorders. These patients could use them for sleep disorders or have some of the other psychiatric diseases we did not explore, such as psychotic disorders, even though the expected prevalence of these disorders does not exceed 1%, and not all of these patients use BZDs on a routine basis [43]. They could also have other disorders or diseases we did not explore, such as alcohol or substance use disorder.
This high usage of BZD seems stable over time, despite regular warnings on excessive use of BZD. For instance, in a cross-sectional study in 1987–1988 in France, Pariente et al. [27] found respectively 4.6% and 10.2% of users in men and women, in a representative sample of the French population. Though the overall use seems higher in France than in other countries or populations [1, 44–48], a fact already noted over 25 years ago [2], the generally higher use in female and elderly patients (above the age of 60 years) is a constant in all studies. This stability of BZD usage patterns over time and space was recently underlined [49]. As in this study [49], over 75% of our users had been using BZDs for at least 6 months at the time of interview, even though BZDs are generally not effective beyond a few weeks and despite the fact that in France the duration of their prescription is officially limited in the marketing authorization to 4 weeks for use in insomnia and 12 weeks for the treatment of anxiety. Obviously, these instructions are not followed. Perhaps more forcible methods are needed than just information to limit at least the duration of BZD use.
Conclusion
Telephone surveys using validated structured questionnaires may be a rapid and simple way to obtain data on current medication use directly from patients and possibly some medical information. As is the case elsewhere, BZD usage in France is focused in the elderly and on long-term use, where the risks are highest and the possible benefits lowest [50, 51]. Any intervention to reduce use or at least duration of use should focus on the general practitioners who write over 80% of these prescriptions and on the patients. Present strategies to limit BZD use and duration of use seem quite ineffective.
References
Mellinger GD, Balter MB, Uhlenhuth EH (1984) Prevalence and correlates of the long-term regular use of anxiolytics. JAMA 251(3):375–379
Balter MB, Levine J, Manheimer DI (1974) Cross-national study of the extent of anti-anxiety-sedative drug use. N Engl J Med 290(14):769–774
Edwards C, Bushnell JL, Ashton CH, Rawlins MD (1991) Hospital prescribing and usage of hypnotics and anxiolytics. Br J Clin Pharmacol 31(2):190–192
Morgan K, Dallosso H, Ebrahim S, Arie T, Fentem PH (1988) Prevalence, frequency, and duration of hypnotic drug use among the elderly living at home. BMJ 296(6622):601–602
Olfson M, Pincus HA (1994) Use of benzodiazepines in the community. Arch Intern Med 154(11):1235–1240
Lecadet J, Vidal P, Baris B, Vallier N, Fender P, Allemand H (2003) Médicaments psychotropes: consommations et pratiques de prescription en France métropolitaine. I Données nationales, 2000. Rev Med Ass Maladie 34:75–84
Mattila-Evenden M, Bergman U, Franck J (2001) A study of benzodiazepine users claiming drug-induced psychiatric morbidity. Nord J Psychiatry 55(4):271–278
Lader M (1984) Benzodiazepine dependence. Prog Neuropsychopharmacol Biol Psychiatry 8(1):85–95
Khan A, Hornblow AR, Walshe JW (1981) Benzodiazepine dependence: a general practice survey. N Z Med J 93(687):19–21
Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DG et al (1998) Association of road-traffic accidents with benzodiazepine use. Lancet 352(9137):1331–1336
Herings RM, Stricker BH, de Boer A, Bakker A, Sturmans F (1995) Benzodiazepines and the risk of falling leading to femur fractures. Dosage more important than elimination half-life. Arch Intern Med 155(16):1801–1807
Lagnaoui R, Begaud B, Moore N, Chaslerie A, Fourrier A, Letenneur L et al (2002) Benzodiazepine use and risk of dementia: a nested case-control study. J Clin Epidemiol 55(3):314–318
Pierfitte C, Macouillard G, Thicoipe M, Chaslerie A, Pehourcq F, Aissou M et al (2001) Benzodiazepines and hip fractures in elderly people: case-control study. BMJ 322(7288):704–708
Ensrud KE, Blackwell T, Mangione CM, Bowman PJ, Bauer DC, Schwartz A et al (2003) Central nervous system active medications and risk for fractures in older women. Arch Intern Med 163(8):949–957
Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J (2001) Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. Am J Psychiatry 158(6):892–898
Sgadari A, Lapane KL, Mor V, Landi F, Bernabei R, Gambassi G (2000) Oxidative and nonoxidative benzodiazepines and the risk of femur fracture. The Systematic Assessment of Geriatric Drug Use Via Epidemiology Study Group. J Clin Psychopharmacol 20(2):234–239
Marks J (1980) The benzodiazepines—use and abuse. Arzneimittelforschung 30(5a):898–901
Stewart RB, Marks RG, Padgett PD, Hale WE (1994) Benzodiazepine use in an ambulatory elderly population: a 14-year overview. Clin Ther 16(1):118–124
Marks J (1983) The benzodiazepines an international perspective. J Psychoactive Drugs 15(1–2):137–149
Duneton P (2001) Mise au point sur les troubles du comportement liées à l’utilisation des benzodiazépines et produits apparentés. http://www.afssaps.sante.fr/htm/10/filltrpsc/lp010901.htm; 2001.
Levy PS, Lemeshow S (1999) Sampling of populations. Wiley, New York, p 21
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E et al (1998) The mini-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59[Suppl 20]:22–33
Moore N, Pierfitte C, Pehourcq F, Lagnaoui R, Begaud B (2001) Comparison of patient questionnaires, medical records, and plasma assays in assessing exposure to benzodiazepines in elderly subjects. Clin Pharmacol Ther 69(6):445–450
Moore N, Masson H, Noblet C, Joannidès R (1993) What medicines do patients really take? A comparison of free form vs. oriented questionnaires. Post Marketing Surveillance 7:355–362
Hosmer DW, Lemeshow S (1989) Applied logistic regression. Wiley, New York
Lepine JP, Lellouch J (1993) Etude épidémiologique des troubles dépressifs et anxieux dans une population générale. Ann Med Psychol 151:618–623
Pariente P, Lepine JP, Lellouch J (1992) Self-reported psychotropic drug use and associated factors in a French community sample. Psychol Med 22(1): 181–190
Ohayon MM, Caulet M (1996) Psychotropic medication and insomnia complaints in two epidemiological studies. Can J Psychiatry 41(7):457–464
Ohayon M, Caulet M, Lemoine P (1996) The elderly, sleep habits and use of psychotropic drugs by the French population. Encephale 22(5):337–350
Guignon N, Mormiche P, Sermet C (1994) Epidemiological aspects of chronic use of psychotropic drugs. In: La consommation régulière de psychotropes. Institut National des Statistiques et des Etudes Economiques—INSEE Premiere, Paris, p 310
Ohayon MM, Lader MH (2002) Use of psychotropic medication in the general population of France, Germany, Italy, and the United Kingdom. J Clin Psychiatry 63(9):817–825
Johnell K, Merlo J, Lynch J, Blennow G (2004) Neighbourhood social participation and women’s use of anxiolytic-hypnotic drugs: a multilevel analysis. J Epidemiol Community Health 58(1):59–64
Ravaris CL, Friedman MJ, Hauri PJ, McHugo GJ (1991) A controlled study of alprazolam and propranolol in panic-disordered and agoraphobic outpatients. J Clin Psychopharmacol 11(6):344–350
Ballenger JC (1990) Efficacy of benzodiazepines in panic disorder and agoraphobia. J Psychiatr Res 24[Suppl 2]:15–25
Ballenger JC, Burrows GD, DuPont RL Jr, Lesser IM, Noyes R Jr, Pecknold JC et al (1988) Alprazolam in panic disorder and agoraphobia: results from a multicenter trial. I. Efficacy in short-term treatment. Arch Gen Psychiatry 45(5):413–422
Liebowitz MR, Fyer AJ, Gorman JM, Campeas R, Levin A, Davies SR et al (1986) Alprazolam in the treatment of panic disorders. J Clin Psychopharmacol 6(1):13–20
Moroz G, Rosenbaum JF (1999) Efficacy, safety, and gradual discontinuation of clonazepam in panic disorder: a placebo-controlled, multicenter study using optimized dosages. J Clin Psychiatry 60(9):604–612
Beauclair L, Fontaine R, Annable L, Holobow N, Chouinard G (1994) Clonazepam in the treatment of panic disorder: a double-blind, placebo-controlled trial investigating the correlation between clonazepam concentrations in plasma and clinical response. J Clin Psychopharmacol 14(2):111–118
Furukawa TA, Streiner DL, Young LT (2002) Antidepressant and benzodiazepine for major depression. Cochrane Database Syst Rev (1):CD001026
Gorman JM (2002) Treatment of generalized anxiety disorder. J Clin Psychiatry 63[Suppl 8]:17–23
Davidson JR (2001) Pharmacotherapy of generalized anxiety disorder. J Clin Psychiatry 62[Suppl 11]:46–50
Shorter E, Tyrer P (2003) Separation of anxiety and depressive disorders: blind alley in psychopharmacology and classification of disease. BMJ 327(7407):158–160
Fourrier A, Gasquet I, Allicar MP, Bouhassira M, Lepine JP, Begaud B (2000) Patterns of neuroleptic drug prescription: a national cross-sectional survey of a random sample of French psychiatrists. Br J Clin Pharmacol 49(1):80–86
Dunbar GC, Perera MH, Jenner FA (1989) Patterns of benzodiazepine use in Great Britain as measured by a general population survey. Br J Psychiatry 155:836–841
Ohayon MM, Caulet M, Priest RG, Guilleminault C (1998) Psychotropic medication consumption patterns in the UK general population. J Clin Epidemiol 51(3):273–283
Rayon P, Serrano-Castro M, del Barrio H, Alvarez C, Montero D, Madurga M et al (1996) Hypnotic drug use in Spain: a cross-sectional study based on a network of community pharmacies. Spanish Group for the Study of Hypnotic Drug Utilization. Ann Pharmacother 30(10):1092–1100
Mayer-Oakes SA, Kelman G, Beers MH, De Jong F, Matthias R, Atchison KA et al (1993) Benzodiazepine use in older, community-dwelling southern Californians: prevalence and clinical correlates. Ann Pharmacother 27(4):416–421
Koenig W, Ruther E, Filipiak B (1987) Psychotropic drug utilization patterns in a metropolitan population. Eur J Clin Pharmacol 32(1):43–51
van Hulten R, Isacson D, Bakker A, Leufkens HG (2003) Comparing patterns of long-term benzodiazepine use between a Dutch and a Swedish community. Pharmacoepidemiol Drug Saf 12(1):49–53
Zandstra SM, Furer JW, van de Lisdonk EH, Bor JH, Zitman FG, van Weel C (2002) Differences in health status between long-term and short-term benzodiazepine users. Br J Gen Pract 52(483):805–808
Cumming RG, Le Couteur DG (2003) Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 17(11):825–837
Acknowledgements
This study was funded by an unconditional grant from Merck & Co., USA. The authors gratefully thank the subjects who agreed to participate in this study. This study was done in accordance with all the laws and regulations governing such studies in France. All data were collected anonymously.
Conflict of interest and authorship statement: none of the authors or their families have any direct financial ties with any of the producers of any of the drugs cited in this study, or with Merck & Co., or own any shares in any of these companies. Several of them (mainly NM, HV and BB) have been invited to give lectures by pharmaceutical companies in this and other fields and have consulted for most pharmaceutical companies in the field of psychopharmacology and other fields of pharmacology, the proceeds going to the university or to non-profit organizations. RL, BB, HV, NM are employees of Université Victor Segalen, Bordeaux; FD and AA are employees of Naturalia & Biologia, a non-profit organization. Their salaries are financed by research contracts with pharmaceutical companies and public organisms. AF was at the time of the study. an employee of ARME-Pharmacovigilance, a non-profit research organization funded by equal donations from eleven pharmaceutical companies and by grants from the French Ministry of Health to conduct fundamental research on methods in pharmacovigilance. NM, HV, AF and BB had the original idea, RL, HV and FD designed the study and the study material and organized the survey, AA, AF, FD and RL did the data analysis. The first draft of the paper was written by RL and reviewed by all authors, who approved the final draft. NM is the guarantor of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lagnaoui, R., Depont, F., Fourrier, A. et al. Patterns and correlates of benzodiazepine use in the French general population. Eur J Clin Pharmacol 60, 523–529 (2004). https://doi.org/10.1007/s00228-004-0808-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0808-2