Abstract
6β-Hydroxycortisol (6β-OHF) urinary excretion has, for a long time, been considered a marker of drug induction and, more recently, of drug inhibition in humans and in laboratory animals, but its specificity is still under debate. In this work, we review 277 papers devoted to 6β-OHF urinary excretion. We have evaluated factors that could modify 6β-OHF excretion and, thus, could explain contradictory results. We have examined the effect of the analytical techniques on physiological values. Intra- and inter-individual variability and the effect of circadian rhythms on urinary excretion of 6β-OHF as well as cortisol and 17-hydroxycorticosteroids have been evaluated. We also give an overview of drugs that induce, inhibit or have no effect on 6β-OHF. For inducing and inhibiting drugs, we calculated the ranges of variation of 6β-OHF excretion from the results indicated in the different papers. This work was done for well-known inducers, such as anticonvulsants, but also for other inducing or inhibiting drugs found in the literature. The time-course of variation in 6β-OHF excretion when different drugs are co-administered was also investigated. The potential relationship between cytochrome P 450 3A4 (CYP3A4) polymorphism and 6β-OHF excretion was studied. Finally, the interest of 6β-OHF urinary excretion was compared with that of other tests proposed to measure CYP3A4 activity. This review demonstrates that 6β-OHF urinary excretion is a good test to evaluate drug-metabolising enzyme inducing or inhibiting properties of drugs when the subjects are their own controls, but this test is not reliable enough to measure actual CYP3A4 activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The activity of many enzymes that are involved in drug or pollutant metabolism can be increased after exposure to these substances in humans as well as in animals. This induction can have beneficial (protective) effects, but can also be at the origin of drug–drug interactions. Clinical consequences of the induction or the inhibition of drug-metabolising enzymes have been largely reviewed in the past [1, 2, 3, 4, 5].
In vivo assessment of enzyme induction in humans has been performed by the measurement of the plasma half-life of probe drugs. Antipyrine has been widely used for this purpose. Although a decreased plasma half-life of antipyrine may often reflect induction of drug-metabolising enzymes, many other factors may alter the absorption, distribution, metabolism and elimination of antipyrine. Several non-invasive procedures for measuring enzyme induction in humans have been proposed. Among these procedures, CO2 breath tests have become the more commonly used. After administration of drugs, usually labelled with the stable isotope 13C, the rate of exhalation of 13CO2 is measured by mass spectrometry. Erythromycin N-demethylation has been demonstrated to be mediated by cytochrome P 450 3A4 (CYP3A4) [6] and a breath test using erythromycin as substrate has been suggested to be a marker of cytochromeP 450 3A (CYP3A) activity [7]. However, these techniques are time consuming and expensive, and, therefore, enzyme induction has also been studied indirectly by measuring certain potential markers of drug-metabolising enzymes in urine. Among these markers, 6β-hydroxycortisol (6β-OHF: 6β, 11β, 17α, 21-tetrahydroxypregn-4-ene-3,20-dione) has been widely used, since its discovery in human urine after cortisol loading by Burstein et al. in 1954 [8]. However, its usefulness as a non-invasive marker of microsomal CYP3A activity is still under debate [9].
The aim of this review was to report what is known about the variations of urinary 6β-OHF and its ratio to free cortisol. This ratio is considered a safe and simple test to evaluate induction [5, 10, 11, 12] or inhibition [13, 14] due to drug treatment or pollutant exposure in humans and in animals, as no probe is administered.
Metabolism
Cortisol is metabolised by reduction of the A ring, reduction of the 20-ketone function and by 6β-hydroxylation. The latter reaction leads to the formation of 6β-OHF, essentially in the liver [15, 16, 17], but also in the adrenal glands [16, 17, 18, 19], kidney [16] and placenta [16]. These two last organs represent only very low metabolic capacities in humans [16]. 6β-OHF is excreted in urine by the kidney in a polar unconjugated form [20, 21]. It represents about 1% of the total cortisol metabolites in urine [22]. Ged et al. [23], using human liver microsomes, were the first to demonstrate that the transformation of cortisol to 6β-OHF is catalysed by CYP3A. The CYP3A subfamily is the most abundant cytochrome P 450 in the liver. It consists of at least three isoforms, CYP3A4, CYP3A5, and CYP3A7. CYP3A4 accounts for approximately 30–40% of total cytochrome P 450 content in human adult liver and small intestine. CYP3A5 presents 83% homology with CYP3A4. It is also expressed in human adult liver, but usually at a much lower level than CYP3A4 [24]. However, relatively high levels of metabolically active CYP3A5 are expressed in the liver of 30–40% of Caucasians [25]. CYP3A7 is expressed in fetal liver and is undetectable in most individuals older than 1 year [26]. Cortisol is a substrate for CYP3A4, which is also responsible for the metabolism of a large variety of drugs—approximately half of all in use today [27]. Using human livers, Abel et al. [28] demonstrated that the human metabolism of cortisol is very complex (Fig. 1) and highly variable among individuals. There was considerable inter-individual variation in metabolic profiles obtained after incubation with liver microsomes. 6β-OHF varied from 2.8% to 31.7% of the total metabolites produced, and this could explain the large inter-individual variability in 6β-OHF excretion. The same authors, using various inhibitors, confirmed that 6β-OHF was produced by CYP3A [29]. The specificity of the measurement of CYP3A4 activity is mainly provided by the use of the ratio 6β-OHF/cortisol. Another confirmation came from Lemoine et al. [30], who demonstrated that a patient grafted with a liver with no CYP3A4 activity excreted very low amounts of 6β-OHF after transplantation. CYP3A4 (as well as CYP3A5) is also present in human intestine [31] and in the kidney, but only in 14% of human adults [32], and their contribution to cortisol metabolism is not completely elucidated.
Proposed metabolic pathways of cortisol in human liver microsomes [28]
Analytical methods
Many techniques have been described for the determination of 6β-OHF in urine. The earliest ones used paper chromatography [18, 20, 33], thin layer chromatography [34, 35, 36] or column chromatography [37, 38]. The detection of 6β-OHF was done using the Porter and Silber colorimetric reaction [18, 20, 35, 36, 39] or the blue tetrazolium reaction [40, 41]. However, these techniques lack specificity, and values were generally largely higher than those obtained with other techniques (Table 1). They are now completely abandoned and replaced by more specific methods.
Since 1977, three radio immunoassays (RIA) have been published, all using the same technique [42, 43, 44]. In each laboratory, rabbit polyclonal antibodies were raised according to the method of Park et al. [45]. 6β-OHF −21-hemisuccinate conjugated to bovine serum albumin was used, except by Nahoul et al. [44], who did not remove the acetate group at C-21. They used the 3 (O-carboxymethyl) oxime derivative coupled to bovine serum albumin as immunogen. 3H-6β-OHF was used as the competitive ligand. Separation of free and bound 6β-OHF was performed by the addition of dextran-coated charcoal. The analytical characteristics of the three techniques were very similar. A protein-binding assay was developed in 1981 by Bowler-Wong et al. [46].
The first technique using high performance liquid chromatography (HPLC) for the measurement of 6β-OHF in urine was reported in 1979 by Roots et al. [47]. Since that date, several other HPLC techniques have been published. The oldest ones allowed only to measure 6β-OHF by HPLC, the other steroids being determined by various other techniques such as colorimetry [Porter and Silber reaction for total 17-hydroxycorticosteroids (17-OHCSFootnote 1)] or RIA (for free urinary cortisol). Most HPLC methods necessitated a preliminary extraction step, and separation of 6β-OHF from other steroids was achieved either by liquid–liquid partitioning [47, 48] or by reverse phase chromatography [49, 50]. Dumont et al. [51] used the true first internal standard (Δ4-pregnene-tetrol-3one), gradient elution and ultraviolet (UV) detection. Recently, Homma et al. [52] have proposed a new HPLC method for measuring 6β-OHF in the urine of pregnant women. Goto et al. [53] proposed a HPLC technique in which 6β-OHF was quantitatively transformed into the 21-(9-anthroyl) derivative and then chromatographed in a normal phase column. Detection was achieved by fluorescence. Thereafter, some techniques allowing for the simultaneous determination of 6β-OHF and cortisol, either with UV detection [54, 55, 56] or fluorescence [57] have appeared. In this last method, 6β-OHF, cortisol and fludrocortisone (internal standard) were extracted and dissolved in methanol and then oxidised by cupric acetate. The resulting compounds were converted into fluorescent derivatives with 1,2-diamino-4,5-methylenedioxybenzene. Then, the derivatives were separated on a reversed-phase column and detected by fluorimetry. Simultaneous determination of six urinary glucocorticoids is now possible using HLPC [58]. The intra-assay and inter-assay coefficients of variation were less than 5% and 10%, respectively. Different protocols have been applied to the determination of 6β-OHF in different studies.
The simultaneous detection of 6β-OHF and cortisol permitted the reduction of the fluctuations observed during the course of the day for these two compounds [59].The daily excretions of 6β-OHF as a function of the different methods are presented in Table 1. In spot urine, Lykkesfeldt et al. [56] found a 6β-OHF/cortisol ratio of 10.09±6.89 (mean±SD). This value is very similar to that obtained by Bienvenu et al. (9.34±4.50) [54].
In 1981, Nambara’s team [60] developed a direct competitive enzyme immunoassay in order to measure 6β-OHF in urine. The hapten was 6β-OHF hemisuccinate conjugated to bovine serum albumin, and polyclonal antiserum was raised in rabbits. Competition was performed using 6β-OHF conjugated to β galactosidase. This technique was highly specific for 6β-OHF. 6β-hydroxycortisone was the only interfering steroid among those tested (1.4% for 50% inhibition). Subsequently, Zhiri et al. [61] and Patel et al. [62] developed competitive enzyme-linked immunosorbent assays (ELISAs). They used the antiserum raised in Nambara’s laboratory, but the competitive ligands were 6β-OHF conjugated to horseradish peroxidase and to penicillinase, respectively. These three techniques showed the same analytical performances in terms of sensitivity, specificity and precision. More recently, new ELISAs have been developed by Yeung et al., using a polyclonal [63] or a monoclonal antibody [64]. This last technique had a lower sensitivity than the three techniques using polyclonal antibodies (200 ng/ml versus 1 ng/ml), which can be a problem when investigating decreased levels of 6β-OHF, in case of CYP3A4 inhibition. A ready-to-use kit based on the technique developed by Zhiri et al. [61] is now commercially available (Stabiligen, 54600 Villers-Les-Nancy, France). It has been used in several studies [65, 66, 67, 68, 69, 70, 71, 72, 73, 74].
As early as in 1988, a first technique using gas chromatography/mass spectrometry (GC/MS) (selected ion monitoring) was developed by Ishibashi et al. [75] for the simultaneous determination of 6β-OHF and free cortisol in urine. [2H3] cortisol was used as an internal standard. Palermo et al. [76] proposed another GC/MS technique for the measurement of cortisol and related 3-oxo-4-ene steroids (particularly 6β-OHF) in urine. Furuta et al. [77] have published a new GC/MS method for the determination of 6β-OHF in urine, and Luceri et al. [78] have proposed a new quantitative GC/MS method with isotope dilution. In all these methods, steroids are derivatised in methoxime-trimethylsilyl analogues. The specificity and sensitivity of these techniques are very good. Liquid chromatography/atmospheric pressure chemical ionisation–mass spectrometry has been applied to the simultaneous determination of cortisol and 6β-OHF in human [79] and monkey urine [80]. Normal values determined by HPLC or GC/MS are generally lower than those found by other techniques (Table 1). Among all these techniques, only specific ones should be recommended, i.e. ELISA, HPLC and GC/SM.
Biological variations
Intra-individual and inter-individual variations
6β-OHF excretion has been found to be variable from one day to another in the same subject. For instance, Ohnhaus et al. [81] found that 6β-OHF excretion varied from 297±43 µg/day to 341±60 µg/day in seven adults tested on three different days. Zhiri et al. [82] measured 6β-OHF daily excretion in six and eight subjects during two or three different days. In these studies, the observed variations were not statistically significant. In contrast, Gerber-Taras et al. [83] found a highly significant variation when they measured 6β-OHF excretion at two separate occasions in six subjects. More recently, Ohno et al. [84] measured 6β-OHF and cortisol excretion with a very specific LC/MS technique in ten subjects during a 2-week period (daily urinary collection for 9 days). They showed that intra-individual variations in 6β-OHF (5.8–23.3%) and cortisol (7.1–22.2%) excretion were relatively low, which indicated that 6β-OHF/cortisol ratios are constant for a single individual. Similarly, Lee [85] did not find any significant variation when the ratio 6β-OHF/cortisol was measured during six consecutive days.
As 6β-OHF formation has been related to CYP3A4 activity, this inter-individual variability in 6β-OHF excretion is the consequence of the variability in the level of expression of CYP3A4, which has been shown to vary up to 60-fold in human adult livers [86]. Yamamoto et al. [87] hypothesised that if a considerable amount of exogenous cortisol is administered, the inter-individual variability of measuring 6β-OHF would be estimated more precisely. This precision is necessary when drugs with a narrow therapeutic index are metabolised through CYP3A4. Indeed, an excellent correlation (r=0.867; P<0.001) between 24h-excretion of 6β-OHF after the administration of exogenous cortisol and doxetaxel clearance was obtained. This indicated that inter-patient variability of CYP3A4 activity could be estimated by this method [88].
Variations due to gender
Fifteen studies have reported comparison of 6β-OHF excretion in adult males and females (Table 2). For the studies published before 1990, the results are controversial; some authors found higher excretion in males than in females [43, 44, 61], and others found the opposite [18], but the variations were generally not statistically significant. The only statistically significant results were those obtained by Pal et al. [38], who found an 11% higher excretion (P<0.001) in 100 women compared with 100 men. More recent studies, performed after 1990 and which used HPLC [85, 89], ELISA [70] or GC/MS [76], found 6β-OHF excretion slightly lower in females than in males. However, these differences were statistically significant in only three studies [52, 70, 90]. The study of Inagaki et al. [90] presents a very significant difference between the 6β-OHF/cortisol ratio of males and females in Japanese subjects. It is the first study demonstrating such a high difference in 6β-OHF/cortisol urinary excretion according to gender. Additional studies should be performed in order to verify these data in other groups of populations.
In order to take into account the diurnal variation in both 6β-OHF and cortisol excretion, it has been recommended to measure these two compounds in each urine sample. For example, Palermo et al. [76] found the excretion of cortisol clearly higher in males (35.2±12.6 µg/day) than in females (23.2±13.2 µg/day) and Ng et al. [70] obtained similar results. The urinary ratio 6β-OHF/creatinine was slightly higher in women (median = 47 µg/mmol) than in men (median = 29 µg/mmol) [91]. Before phenytoin dosing, no difference in the ratio 6β-OHF/17-OHCS was observed between males and females. After the administration of phenytoin, the increase of this ratio was more pronounced in females than in males [92].
In children, several authors [36, 93, 94, 95] have found no effect of sex on the urinary excretion of 6β-OHF, but Nakamura and Yakata [96] found 6β-OHF excretion higher in boys (5–10 years) than in girls. This difference disappeared when 6β-OHF/cortisol ratios were considered. Palermo et al. [76] found that young females (before the age of 12 years) excreted more urinary 6β-OHF (+23%) than males of the same age. Inversely, after the age of 13 years, females excreted lower quantities (−22%) than males. These variations according to gender are generally low and not statistically significant. Thus, it does not appear necessary to separate populations as a function of gender in further studies.
Variations due to age
In adults, all studies comparing young and old subjects found a decrease in urinary excretion of 6β-OHF in elderly (Table 3). These decreases were comprised between 17% and 46%. Nakamura and Yakata [96] found the same trend of decreasing excretion with age. In males and in females, the differences (calculated on mean values) between groups aged 14–20 years and 50–67 years were −34% and −40%, respectively. In contrast, Yamagi et al. [35] did not find any decrease between the age of 20 and 29 years and 50 and 59 years in males or in females. Similarly, Dolara et al. [97] did not find any difference in the 6β-OHF/17-OHCS ratio in control subjects before and after the age of 40 years.
In children aged 7–12 years, 6β-OHF excretion was largely lower than in adults, in males as well as in females [76]. Similar results were found by Thrasher et al. [36], but the difference was not significant when the ratio 6β-OHF/17-OHCS was taken into account. On the contrary, Nakamura and Yakata [96] found the 6β-OHF/cortisol excretion ratio higher in children than in adults.
In newborns, it is quite impossible to collect 24-h urine, so the results have been expressed in ng/ml. Kishida and Fukushima [42] found a very high urinary excretion of 6β-OHF in neonates (530±156 ng/ml). Patel et al. [98] found the lowest values in children aged between 15 days and 90 days (31.67±6.55 ng/ml). These values increased with age by 52% when comparing babies aged 90 days and 195 days [99]. In breast-fed infants whose mothers had been taking anti-tuberculosis drugs (ethambutol and isoniazid), 6β-OHF excretion was lower than in control infants. These drugs, thus, significantly inhibited 6β-OHF excretion in infants [99]. Vauzelle-Kervroedan et al. [100] found higher 6β-OHF/cortisol ratios in premature and in full-term neonates (1–15 days after birth) than in 30- to 359-day-old infants (7.2±3.8; 7.9±5.6 and 5.0±4.7, respectively). However, Nakamura et al. [101] obtained the opposite results. In premature neonates (less than 37 weeks gestational age), the mean 6β-OHF/cortisol ratio was 5.3, and, in mature infants, it was 16.5. They found no difference due to gender in neonates and no effect of the mode of delivery—caesarean section or vaginal delivery—on the 6β-OHF/cortisol ratio, but they did observe a correlation between 6β-OHF/cortisol and gestational age and also birth weight. In addition, in premature neonates, the ratio was relatively stable between the day of birth and 14 days after. In contrast, in mature neonates, this ratio decreased until day 5 and then stabilised. No relationship between 6β-OHF/cortisol ratio in mature neonates on the day of birth and the ratio measured in their mothers was found [102]. These variations could, at least in part, explain contradictory results found in literature.
In conclusion, in adults 6β-OHF/cortisol excretion decreases after the age of 50–60 years. Therefore, this variation factor must be taken into account in studies of 6β-OHF/cortisol excretion. In children and neonates, the results are controversial, which obviates the need for additional studies.
Effect of hormonal status
In a limited number of healthy children, Palermo et al. [76] demonstrated that 6β-OHF and cortisol excretions were increased with puberty both in males and in females compared with younger children, but the excretion of both 6β-OHF and cortisol remained lower than in adults. The ratio 6β-OHF/cortisol did not vary with age nor with puberty [76].
Katz et al. [18], and Burstein et al. [103] did not find any significant variation in the 6β-OHF/cortisol ratio in 13 healthy females during the four different weeks of their menstrual cycle. Similarly, Lin et al. [104] did not find any significant difference in the ratio 6β-OHF/cortisol in Caucasian nor in Asian women during the different periods of their menstrual cycle.
In healthy menopausal women, the 6β-OHF/cortisol ratio (measured more than 1 year after the last menstruation) did not significantly vary from the values obtained in non-menopausal women, and there was no variation during the different periods of the month [103].
Frantz et al. [105] were the first to demonstrate that 6β-OHF excretion increased during pregnancy—results confirmed by Nahoul et al. [44] and Bowler-Wong et al. [46]. Compared with non-pregnant women, 6β-OHF excretion was increased by about a factor of two (P<0.001) during the third trimester of pregnancy [41, 44, 46, 52]. The amount of daily urinary excreted 6β-OHF and the ratio 6β-OHF/17-OHCS was studied previously, 1 week and 3 months after parturition in a group of nine healthy pregnant women. The values observed before delivery were largely higher (6β-OHF: +212%; 6β-OHF/17-OHCS: +299%) than those obtained in non-pregnant women [106]. The values for 6β-OHF as well as for the ratio 6β-OHF/cortisol returned to control values 3 months after delivery [106]. Pregnant women in true premature labour who were spontaneously delivered less than 24 h after admission had significantly higher 6β-OHF levels (1144±210 ng/ml) than subjects in false premature labour (544±88 ng/ml) [107]. However, Hunter et al. [108] found a too-high diurnal variation to distinguish false from true premature labour with a single urine sample.
Circadian rhythm
Cortisol is well known to be excreted according to a circadian rhythm. Saenger [109] was, in 1983, the first to demonstrate that 6β-OHF excretion paralleled cortisol excretion and was the highest between 0800 hours and 1200 hours and was the lowest around midnight. He demonstrated in non-treated controls, as well as in phenobarbital-treated patients, that the excretions of 6β-OHF and cortisol varied throughout the day, reflecting the changes in adrenal secretion. However, there was no significant diurnal variation when the 6β-OHF/cortisol ratio was taken into account. Since this first report, several authors have obtained similar results with 6β-OHF/cortisol [59, 61, 85, 108] or with 6β-OHF/17-OHCS [109]. 6β-OHF/cortisol ratios are relatively stable around a 24-h period. Similar results have been obtained in 32-week pregnant women [110]. But Ohno et al. [84] and McCune et al. [111] have demonstrated that diurnal variations of 6β-OHF and of cortisol were not really parallel, and, therefore, the ratio varied from 4.3 between 0900 hours and 1300 hours to 12.6 between 1800 hours and 2200 hours. These results are in disagreement with those obtained by other authors who found a good correlation between morning and 24-h 6β-OHF/cortisol ratios [49, 54, 112, 113].
In conclusion, 24-h urine would be the optimal sampling, but it is difficult to collect qualitatively and quantitatively. It could, therefore, be recommended to use a single-spot morning urine sample to measure both 6β-OHF and cortisol and to calculate the ratio 6β-OHF/cortisol. This, indeed, is the usual way of practice in most studies.
Other variations
Obesity
Mean urinary excretion of 6β-OHF, cortisol and 17-OHCS are not different in obese and in non-obese subjects [114].
Genetic factors
Geographic origin
In healthy non-smoking and non-alcohol consuming Chinese subjects, 6β-OHF and cortisol output was similar to those reported for healthy Caucasians [71].
Polymorphism of CYP3A4
The ratio 6β-OHF/17-OHCS was measured in the urine of 102 healthy volunteers. There was a wide distribution ranging from 17 to 233.3. No clear bimodality was observed [66]. Rifampicin treatment of these healthy subjects increased 6β-OHF excretion, and, again, there was a wide distribution for the ratio (91.3–917.9). However, here again, no clear bimodality was observed. Moreover, the mean 6β-OHF level was higher in women than in men. These observations do not indicate the existence of a CYP3A4 genetic polymorphism reflected by 6β-OHF excretion, but evoke a sexual dimorphism [66], which is not really confirmed when variations of 6β-OHF excretion according to gender are considered. These results do not mean that CYP3A4 is not polymorphic, but rather that, as some polymorphisms do exist on this gene, they have no influence on 6β-OHF excretion. A recent study in 487 healthy Japanese individuals obtained the same results [90]. Collecting the results obtained between 1966 and 1999 by the use of repeated drug administration, Özdemir et al. [115] suggested that approximately 90% of inter-individual variability in hepatic CYP3A4 might be of genetic origin.
It has now been demonstrated that CYP3A4 presents several polymorphisms. Rebbeck et al. [116] found a point mutation (A290 → G) on the 5′-flanking region of the human CYP3A4 gene with an allele frequency in the U.S. Caucasian population estimated to be 9.6%. It was significantly higher in African Americans (53%) and absent in Taiwanese [117]. The allele frequency for this polymorphism was found to be 5.3% in 199 healthy Dutch Caucasians [118]. This mutation seemed to be associated with higher clinical stage and grade in men with prostatic cancer [116]. Wandel et al. [119] observed a lower CYP3A4 activity associated with this variant allele designated CYP3A*1B (systemic clearance in G/G lower by about 30% than in A/A, tested in vivo using midazolam), but Rivory et al. [120] did not find any association between this polymorphism and cyclosporin clearance in liver transplant patients. On the other hand, Sata et al. [121] found that 2.7% of a white population presented another variant allele (CYP3A*2 : Ser222Pro). In these subjects, the intrinsic clearance for nifedipine was lower than in the wild-type enzyme carriers, but there was no difference for testosterone β-hydroxylation. In addition, Weslind et al. [122] did not find any influence of this polymorphism on microsomal testosterone hydroxylation in vitro. Another rare allele, designated CYP3A4*3 (Met445Thr), was discovered in a single Chinese individual by the same team [121]. The allelic frequency of CYP3A4*3 was 1.1% in Caucasians [123]. Lamba et al. [124] studied the genetic variability of CYP3A4 in 82 individuals. They found 28 single nucleotide polymorphisms in different regions of the CYP3A4 gene. None of these polymorphisms was associated with a low in vivo CYP3A4 activity evaluated through midazolam hydroxylation rate. However, Hsieh et al. [74] demonstrated the presence of three novel mutations on the CYP3A4 gene. CYP3A4*4 (Ile118Val) and CYP3A4*5 (Pro218Arg) mutations were present in respectively 3 and 2 of 102 Chinese subjects. Another allele was found in a single heterozygous Chinese individual (CYP3A4*6: A17776, which causes frameshift and an early codon stop in exon 9). These three gene modifications seem to be associated with decreased CYP3A4 activity, measured using the urinary 6β-OHF/cortisol ratio. These results need confirmation in further studies.
Effects of other polymorphisms of drug metabolising enzymes:
Park et al. [125] and Eichelbaum et al. [126] did not find any significant difference between extensive and poor metabolisers of sparteine (CYP2D6). In 1989, Leclercq et al. [127] found the same results using debrisoquine as probe drug. 6β-OHF excretion was also very similar in extensive and in poor metabolisers of S-mephenytoin (CYP2C19) [68].
After isoniazid treatment alone or in combination with rifampicin, there was no difference in 6β-OHF/17-OHCS excretion between slow and rapid acetylors [128].
Effects of drugs
Since early studies, the excretion of 6β-OHF has been used as an endogenous marker of drug-inducing effects on CYP450 activity in vivo [129, 130, 131], but not of cytochrome P 448 Footnote 2 [132].
Effects of classical inducing drugs
6β-OHF excretion has been demonstrated to be increased by a large number of drugs. Antipyrine was able to induce 6β-OHF excretion as well as the ratio 6β-OHF/17-OHCS, but the induction was quite moderate (maximum twofold) [10, 11, 81, 126, 130, 131, 133, 134, 135, 136, 137, 138].
Carbamazepine increased 6β-OHF excretion in adults by 1.5 to 3.0 times (P<0.001) as a function of the dosage and of the duration of the treatment [71, 139, 140, 141, 142, 143]. In six children (6–14 years old), a treatment with this drug for 4 weeks provoked a statistically significant mean increase of 2.5 times [144].
Phenobarbital also induced 6β-OHF excretion but the increases were quite low (7–88%). They were a function of the dosage and of the duration of treatment [10, 11, 81, 126, 127, 129, 130, 131, 134, 138, 145, 146, 147, 148, 149, 150, 151, 152]. No significant change in the cortisol production rate and its excretion was observed after phenobarbital treatment [22]. Phetharbital (N-phenylbarbital) presented larger inducing properties (161–291%) on 6β-OHF excretion [153, 154]. Pentobarbital is also a good inducer of 6β-OHF [37, 155]. Phenytoin has been demonstrated to largely increase 6β-OHF excretion (2 to 7 times) [40, 42, 71, 93, 139, 145, 156, 157, 158, 159]. Valproic acid, another anticonvulsant, was a slight inhibitor of urinary 6β-OHF excretion [140]. Rifampicin has been shown as the best inducer of 6β-OHF excretion. McColl et al. [160] observed an increase in 6β-OHF excretion by 6 times in patients treated with a dose of 600 mg/day for 30 days (P<0.001). Several other studies found an increase in 6β-OHF excretion [43, 47, 64, 67, 126, 131, 137, 138, 161, 162, 163, 164, 165, 166] as well as in the 6β-OHF/cortisol excretion ratio [23, 167, 168, 169, 170, 171] or in the 6β-OHF/17-OHCS ratio [10, 11, 47, 81, 127, 134, 172, 173, 174, 175]. Reichel et al. [176] observed that the induction of cytochrome P 450 by rifampicin was associated with a less than 10% increase in liver volume and with no variation of portal perfusion. It kept its inducing properties in patients with primary biliary cirrhosis [177]. Rifampicin treatment increased the hepatic clearance of cortisol to 6β-OHF from 13±15 ml min−1 to 72±5 ml min−1, which corresponded to the observed rise in 6β-OHF excretion [178]. Some other anti-tubercular agents, derivatives of rifampicin, such as rifabutine [164] or rifapentine [175, 179], are also inducers, but to a lesser extent than rifampicin. The induction due to rifapentine was dose dependent [175].
It has been observed that different drugs have various lag times to switch on their inducing effect on the hepatic microsomal enzyme activities. It is this latent period that allows speculation on the induction property of a drug, rather than a simple direct enzyme activation. It is very important to know exactly the time-course of drug induction or inhibition for the co-administration of drugs.
Latham et al. [148] performed a study in 17 healthy male subjects that were randomly divided into three groups: 6 subjects received placebo or 120 mg phenobarbital and the 5 subjects in the remaining group received 240 mg phenobarbital for 14 days. At the end of day 14, treatment was abruptly terminated. Placebo had no significant effect, but 240 mg phenobarbital per day produced a highly significant increase in the log-normalised values of the urinary excretion of 6β-OHF (P<0.001 during treatment and P<0.01 after treatment) when compared with the mean of the corresponding pre-treatment control values. Two important observations from these studies were the absence of steady-state conditions for 6β-OHF after 7 days of treatment with phenobarbital and the duration to return to steady-state baseline concentrations after the withdrawal of treatment. 6β-OHF started to decrease after termination of treatment and almost reached baseline values in the fifth week after treatment was stopped. Therefore, the time necessary for a return to baseline concentrations, if dependent on the peak 6β-OHF excretion, may be considerably longer than 1 month. A study was conducted by Crowley et al. [156] to correlate 6β-OHF daily excretion levels with age, smoking habits and duration of treatment with phenytoin. 6β-OHF daily excretion was not significantly influenced by age or by smoking, as indicated before. In contrast, depending on the duration of treatment with phenytoin, 6β-OHF excretion was significantly increased (P<0.001). Induction of urinary 6β-OHF excretion due to antipyrine, phenobarbital or rifampicin as a function of time was studied in 71 non-smoker healthy volunteers by Ohnhaus et al. [131]. Drugs were given chronically for either 7 days or 14 days. Significant increases in 6β-OHF excretion occurred only 2 days after start of administration of rifampicin (600 mg/day or 1200 mg/day), 4 days after administration of antipyrine (1200 mg/day), but 13 days after administration of phenobarbital (100 mg/day). When rifampicin was administered for 14 days (1200 mg/day), 6β-OHF excretion reached a maximum between day 11 and day 14, and the excretion was significantly greater than on day 7. After stopping rifampicin treatment in a 7-day study, 6β-OHF excretion decreased over the next 6 days, but still remained significantly elevated compared with the original control values [180]. These studies show that measurement of urinary 6β-OHF provides a simple, non-invasive method for monitoring the time-course of enzyme induction by drugs in man.
Effects of other inducers
It is now well known that enzymatic induction can lead to unexpected effects after drug co-administration, and, therefore, the inducing properties of new candidate drugs are usually tested during their development. Table 4 presents the inducing effects of several drugs on 6β-OHF excretion. Most of them have low-inducing properties, except for enflurane and miconazole, which increased the ratio 6β-OHF/17-OHCS by a factor of two. Pentobarbital, which is structurally very similar to phenobarbital, produced a 2.5-fold induction of this ratio. Induction is dose dependent and it is also dependent on the duration of administration. For example, a derivative of isoquinoleine (52028RP) was highly inducing 6β-OHF excretion after 5–15 days of treatment, but after 20 days, there was no induction [65]. Probenecid [181] as well as phenylbutazone [182] significantly increased 6β-OHF urinary excretion. Saint John’s Wort is an herbal extract (Hypericum perforatum) used in mild to moderate depression. This extract was shown to interact with different variety of drugs. Bauer et al. [183] demonstrated a significant mean increase from 9.9 to 14.3 of 6β-OHF/cortisol ratio in subjects treated with Saint John’s Wort for 14 days. These results confirm those previously obtained by Roby et al. [184].
A first paper published in 1998 by Seidegard et al. [72] demonstrated the inhibitory effect of grapefruit juice. A review [185] confirmed this inhibitory effect on intestinal CYP3A4. The effect of grapefruit juice largely varies from patient to patient, probably because of wide variability in intestinal concentrations of CYP3A4. In a very recent paper, Fuhr et al. [186] considered grapefruit juice as an inducer of hepatic CYP3A4, evaluated by the increase of renal excretion of 6β-OHF in humans. Similar results were obtained in the rat [187]. This example demonstrates the difficulty of such studies, which are dependent upon several factors and among which the treatment conditions are of primary importance. Further studies must be performed in order to evaluate the respective contributions of hepatic and of intestinal CYP3A4 on the excretion of urinary 6β-OHF.
Effects of inhibitors
If there is no contest about the usefulness of 6β-OHF/cortisol ratio in detecting induction, some controversy exists about detection of inhibition. Some drugs inhibit 6β-OHF excretion, but usually their inhibiting properties are fairly low (Table 5).
Inhibitory effects are highly dependent upon the dose administered. For example, ozagrel, a thromboxane inhibitor, did not reduce 6β-OHF/cortisol when 400 mg/day was given, but this ratio was decreased by 15–20% when the dose was 800 mg/day [188]. Stiripentol, a new anticonvulsant, has been demonstrated to inhibit CYP3A4 in vitro and in vivo when dextromethorphan was used as probe drug, but showed no inhibiting properties on 6β-OHF/cortisol [189]. Macrolide antibiotics, such as troleandomycin (2 g/day for 10 days) or josamycin at the same dose, caused a decrease in both urinary 6β-OHF and cortisol excretion, but when the 6β-OHF/cortisol was considered, these variations were not statistically significant [190].
Ketoconazole was the most potent inhibitor of cortisol metabolism by human liver microsomes (IC50=0.6 µM) and itraconazole also showed marked inhibition of cortisol metabolism (IC50=2.4 µM) [191]. However, in a study with tirilazad-ketoconazole co-administration, 6β-OHF/cortisol did not reflect this inhibitory effect [192]. Fluconazole was also a good inhibitor of the 6β-OHF/cortisol ratio [13]. Danazol, a synthetic androgen, has been shown to probably inhibit CYP3A4, as demonstrated by the decrease of the ratios 6β-OHF/cortisol and 6β-OHF/17-OHCS [159]. Certain HIV-protease inhibitors, i.e. indinavir, ritonavir and amprenavir, are known CYP3A4 inhibitors, but none of these drugs caused any significant variation in 6β-OHF/cortisol excretion [193]. Nelfinavir reduced the 24-h urinary excretion of 6β-OHF by an average of 27% [194]. A single dose of methadone administered to healthy volunteers decreased 6β-OHF/cortisol urinary excretion over the first 24 h following drug administration by 33±33% [195]. Amiodarone (800 mg per day for 3 days) significantly decreased 6β-OHF/cortisol [196]. Ushiama et al. [197] demonstrated that clarithromycin (400 mg/day or 800 mg/day for 7 days) led to significant decreases of 6β-OHF/cortisol ratios by 47% and 65%, respectively. They obtained parallel results when using the mean partial cortisol clearance to 6β-OHF, which was supposed to better reflect CYP3A4 activity than 6β-OHF/cortisol urinary excretion.
These different studies demonstrate that only weak correlations exist between in vitro and in vivo inhibition studies. This is probably due to the lack of sensitivity and high inter-individual of in vivo measurements of CYP3A activity. For that reason, some drugs could be presented as inhibitors or as drugs having no effect on 6β-OHF excretion, but for different dosages.
Drugs having no effect
Finally, some drugs have been demonstrated to have no effect on 6β-OHF production. Table 6 gives the list of such drugs having no statistically significant effect on 6β-OHF, 6β-OHF/cortisol or 6β-OHF/17-OHCS excretion at the doses indicated.
Among these drugs, oral contraceptive formulations containing ethinylestradiol and levonorgestrel or gestodene or cyproterone acetate administered to healthy young women did not cause any difference in 6β-OHF/cortisol excretion [82, 198, 199, 200].
Urinary 6β-OHF fluctuation after drug co-administration
In drug monotherapy, the categorisation will be relatively simple to assign, but in drug combination therapy the situation is different, especially when an enzyme inducer and an enzyme inhibitor are administered together. When different inducers were associated, the rise observed was usually higher. For example, various anti-convulsants administered in association gave mean increases of 6β-OHF excretion of 4.9 to 7.6 times, and Zhiri et al. [61] found an increase of 6β-OHF/17-OHCS by more than 10 times.
An enzyme inducer will influence the pharmacokinetics of some co-administered drugs and lead to lowered plasma concentration and half-life. The antipyrine half-life value in eight barbiturate-treated patients was significantly shortened, and the urinary output of 6β-OHF was approximately three times that in a control population [155].
In the case of enzyme inhibitors, the reverse will be observed and the plasma concentration and half-life of the co-administered drug will be increased. However, the results may be different according to the route of administration. For example, the ratio 6β-OHF/cortisol significantly decreased after ketoconazole + oral tirilazad administration, but not after ketoconazole + i.v. tirilazad treatment [192].
The administration of fluconazole for 7 days led to a significant increase in zidovudine half-life and a significant decrease of 6β-OHF excretion (−28%). Inversely, a treatment with zidovudine had no effect on fluconazole half-life and significantly increased 6β-OHF excretion (+56%) [14].
The interaction of ciclosporin A (immunosuppressive agent) and ticlopidine (anti-thrombotic agent) on 6β-OHF excretion was studied in heart-transplant recipients [201]. Urinary 6β-OHF excretion was increased in the ticlopidine-treated patients compared with the placebo group (+32%, P<0.05), suggesting an induction of CYP3A4 possibly leading to a reduced ciclosporin exposure. The 6β-OHF/cortisol ratio did not significantly vary in patients receiving delavirdine mesylate and fluconazole for 1 day to 15 days [202]. After antipyrine administration, a fall in steady-state plasma warfarin concentration in five subjects, a shortening of the plasma warfarin half-life in two subjects and increased urinary excretion of 6β-OHF were observed [133].
Amitriptyline co-administered with atenolol or with metoprolol produced a non-significant reduction of 6β-OHF excretion when compared with atenolol or metoprolol monotherapy [203]. A relatively high dose of lansoprazole did not affect the bioavailability of ethinylestradiol and levonorgestrel, and 6β-OHF excretion was not significantly influenced either [204]. Ranitidine did not impair the hepatic elimination of diazepam, although excretion of 6β-OHF (P=0.029) and 17-OHCS (P=0.041) were significantly increased by ranitidine. However, the ratio did not change [205]. In a study to investigate the effect of sulphinpyrazone on antipyrine metabolism and on the urinary excretion of 6β-OHF, there was no change in the renal clearance of antipyrine after 23 days of sulphinpyrazone treatment, but the renal clearance of each antipyrine metabolite was significantly increased, as was the quantity of urinary 6β-OHF in 24 h urine before and on days 3, 9, and 24 of sulphinpyrazone treatment. The calculated ratio to 17-OHCS excretion also increased significantly in a time-related manner [206]. In another study directed to evaluate the interaction of cimetidine and rifampicin with the β1-selective adrenoceptor antagonist bisoprolol, no significant interaction of bisoprolol with cimetidine, a well-known inhibitor of monooxygenase system in the liver, occurred, but rifampicin, the most potent enzyme inducing drug known, significantly decreased the maximal plasma level and increased the elimination of bisoprolol [207]. In this study, the daily excretion of 6β-OHF was significantly increased, but no effect of bisoprolol on urinary 6β-OHF was reported.
As a conclusion on this section on the effects of various drugs, it can be recommended to pay attention to the conditions of treatment when interpreting the variations of urinary 6β-OHF. It must also be strongly recommended to use the ratio 6β-OHF/cortisol and when possible to test at least two doses for a drug. The results will also depend on the number of subjects included in the study as well as the statistical methodology used.
Effects of xenobiotics
Alcohol intake
Urinary 6β-OHF/cortisol was significantly higher in chronic alcoholics than in control subjects (10.21±2.4 versus 3.97±0.47; P<0.01). Ethanol might have a slight inducing effect on CYP3A4 in humans, as it is the case in cultured hepatocytes. On the contrary, in patients with acute alcohol intoxication, the mean urinary 6β-OHF/cortisol excretion was lower than in controls [78].
Coffee intake
Following 21 days to 52 days of caffeine restriction, no significant variation in the excretion of 6β-OHF/17-OHCS was observed in 11 non-smoker volunteers [208]. The authors observed increases in the ratio in 6 subjects (from 30% to 176%) and decreases in 5 subjects (from −4% to −73%).
Smoking
Vestal et al. [209] demonstrated that smoking had no effect on 6β-OHF excretion in young as well as in old healthy males. In smokers, 6β-OHF was slightly lower than in non-smokers (−24% to −7%, according to age) but these variations were not statistically significant. Similar results were obtained by other authors [91, 156, 213]. In addition, smoking did not influence 6β-OHF/creatinine excretion [91].
Environmental chemicals
Several studies have been undertaken to study the effect of environmental chemicals on the mixed function oxidase enzyme activity on the basis of urinary 6β-OHF excretion. The pesticides dieldrin-aldrin and endrin affected 6β-OHF excretion differently [210]. Dieldrin-aldrin had no effect on the ratio 6β-OHF/17-OHCS (30.7±18.2 versus 30.5±16.2 for exposed and non-exposed workers, respectively), whereas endrin largely influenced 6β-OHF/17-OHCS excretion (91.0±27.6 versus 30.5±16.2 for exposed and non-exposed subjects, respectively). Dichloro-diphenyl-trichloroethane provoked a 57% mean increase in 6β-OHF excretion [39].
Styrene was also found to induce 6β-OHF production as judged by the ratio 6β-OHF/17-OHCS [211], which was 18.8±4.2 in non-exposed and 36.9±15.3 in exposed workers. But Bragt et al. [212] did not confirm this observation on styrene when they analysed 6β-OHF in the 24 h urine from 40 styrene workers and 37 laboratory workers used as controls. They did not find significant alterations in 6β-OHF excretion levels. 6β-OHF levels in exposed workers were 236±83 µg/day versus 256±126 µg/day in controls. Moretti et al. [213] did not observe any induction, but rather an inhibition of 6β-OHF/17-OHCS in workers in the rubber industry. Occupational exposure to cis-1,3-dichloropropene did not affect 6β-OHF/cortisol ratio [214].
A decreased urinary excretion level was observed in lead-intoxicated children [215]. The decrease was all the more important when the lead storage was elevated [216].
Variations due to pathological states
Few studies have been conducted to study the variations in 6β-OHF excretion in pathological cases. Nevertheless, 6β-OHF excretion has been reported to be much more increased than cortisol itself in hypercortisolemic patients [20, 41, 42, 114, 156, 217], although Nahoul et al. [44] observed the opposite. Nakamura and Yamata [112, 114] did not find any difference in 6β-OHF excretion between Cushing’s syndrome (overproduction of cortisol by adrenal glands) and Cushing’s disease (overproduction of ACTH by pituitary glands), although both 6β-OHF and cortisol excretion were higher than in control subjects.
Werk et al. [33] found increased excretion of 6β-OHF in terminal illnesses, especially in advanced cancer, but these increases, although very high, were not statistically significant due to the wide scattering of values. In six patients with bronchogenic carcinoma, Kishida and Fukushima [42] did not find any significant rise in 6β-OHF excretion.
Several studies have been performed to evaluate the variation of 6β-OHF excretion in different hepatic diseases. In nine patients with hepatic disease, Borkowski et al. [218] did not find any difference in 6β-OHF excretion compared with control subjects. A slight increase in the ratio 6β-OHF/cortisol was found in healthy HbsAg carriers [219]. In subjects presenting an abnormal liver function profile, Eade et al. [220] found a mean 6β-OHF/17-OHCS increase of 75% (P<0.001). The largest rises were observed in patients suffering from acute hepatitis (+273%; P< 0.05) or hepatic carcinomas (+327%; P< 0.05). However, Wensing et al. [221] did not find any variation in the daily excretion of 6β-OHF in patients with liver cirrhosis. After liver transplantation, 6β-OHF excretion increased by about 4 times, even in a patient where liver biopsy was unable to detect CYP3A4 [29]. Ng et al. [70] did not find any significant variation in the 6β-OHF/cortisol ratio in chronic liver disease, in cirrhosis and in resectable carcinoma. In contrast, in non-resectable carcinoma they found a significant rise (10.55±7.3) compared with control subjects (5.92±2.97). More recently, Wild et al. [222] showed that 6β-OHF/cortisol did not vary in patients with chronic hepatitis B.
A significant increase (P<0.01) in 6β-OHF excretion was observed in five glucose-6 phosphate dehydrogenase deficient patients [218]. In patients suffering from thyrotoxicosis, 6β-OHF excretion was lower than in controls and the opposite was observed in myxedematous patients [35]. In heterozygous familial hypercholesterolemia 6β-OHF as well as cortisol excretion were similar to those observed in control subjects [198, 223].
As mentioned in a previous section, 6β-OHF urinary excretion was increased by about 2 times during the third trimester of normal pregnancy. In toxemia pregnancy, this increase was demonstrated to be much higher (by about 5 times) [105]. 6β-OHF excretion was elevated in traumatic brain injury [224] and did not vary in rheumatoid disease [18].
In a recent case-control study, the risk of breast cancer was increased with increasing levels of 6β-OHF/cortisol urinary excretion [225]. The association 6β-OHF/cortisol and breast cancer was stronger among older women who had a high body mass index, late age at menopause and early age at menarche.
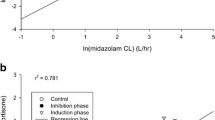
Comparison with the other tests measuring CYP3A activity in humans
Watkins’ team [7, 226] has demonstrated that the erythromycin breath test well reflects the hepatic activity of CYP3A4. It was well correlated with 6β-OHF in some patients, but not in others [168]. Hunt et al. [227] did not find any correlation between erythromycin breath test and 6β-OHF urinary excretion in a small number of patients with hypertension. Kinirons et al. [228] confirmed these results in young healthy men. More recently, the same team failed to find any correlation between erythromycin breath test, 6β-OHF/cortisol excretion and midazolam clearance, all three tests supposed to represent CYP3A liver activity [229]. Similarly, Gotzowsky et al. [230] found a poor correlation between the 24-h urinary 6β-OHF/cortisol molar ratio and midazolam clearance. These results strongly suggest that cortisol 6-β hydroxylation, erythromycin N-demethylation, and midazolam hydroxylation are catalysed by distinct CYP3A4 isoforms, genetically different or other CYP3A forms like CYP3A5. Moreover, overall CYP3A5 protein content accounted for 31% of the variability in hepatic midazolam hydroxylation activity [231]. For Watkins et al. [232], the ideal probe for CYP3A is not discovered yet, and it seems that a single probe would not be appropriate to test CYP3A4 activity.
The use of 6β-OHF as test of induction in different animal species
Hepatic cortisol metabolism is highly variable across species. Rat and mouse liver microsomes produce 6β-OHF as a minor metabolite (2%) [233]. Dog liver is also able to produce small quantities of 6β-OHF from cortisol [17]. In the guinea-pig, 6β-OHF production in vivo is strain-dependent, and two distinct phenotypes exist with high or low urinary excretion of 6β-OHF [234]. In the hamster, 6β hydroxylation is a major pathway of cortisol biotransformation (30%) [233].
Pre-treatment of rats, guinea-pigs or mice with phenobarbital increases the mean rate of in vitro cortisol transformation to 6β-OHF in liver microsomes [235, 236, 237]. Dexamethasone, but not β-naphthoflavone, also induced cortisol 6β hydroxylation in mice [237]. Ethanol was not an inducer of 6β-hydroxylase in the rat [235].
Concerning 6β-OHF excretion, marmoset and rhesus monkeys have been demonstrated to be good animal models of CYP induction due to phenobarbital [57, 238] or rifampicin [80, 239]. These animals represent the best model for estimating drug induction. The 6β-OHF/cortisol ratio was increased approximately 4-fold on the eighth day after the beginning of phenobarbital treatment (30 mg/kg/day) [240].
In guinea-pigs, 6β-OHF excretion was increased by pre-treatment of the animals by phenobarbital or rifampicin, but no variation was observed after 3-methylcholanthrene, pregnenolone-16α-carbonitrile or spironolactone treatment [241]. The induction due to phenobarbital has been demonstrated to be variable with the strain [242].
When mouse liver microsomes were incubated in vitro with gestodene, 6β-OHF formation was inhibited [237]. In rats, Abu-Qare and Abou-Donia [243] found a significant increase in urinary 6β-OHF after a single dermal dose of an insect repellent, N,N-diethyl-m-toluamide (DEET), but permethrin, another insecticide, had no effect on 6β-OHF excretion.
Conclusion
The measurement of 6β-OHF excretion has to be considered as a useful test for estimating CYP3A drug induction or inhibition in human and in laboratory animals, particularly monkeys and guinea pigs. Urinary cortisol must be evaluated in the same patients as the ratio 6β-OHF/cortisol minimises the effect of circadian rhythms. Because of large inter-individual variations in cortisol metabolism, each patient must be his own control for the evaluation of drug induction or inhibition and the time course of induction or inhibition should be followed.
Some limitations appeared in the use of 6β-OHF/cortisol ratio to measure CYP3A4 activity. First, cortisol is a substrate for CYP3A4 and also for CYP3A5, and the contribution of this last enzyme on the metabolism of cortisol to 6β-OHF is poorly understood. Is it possible that CYP3A5 variations should mask changes in CYP3A4? That does not seem very probable, as CYP3A5 is not inducible and is present in much smaller concentrations than CYP3A4 [173], except for those people who are carriers of the CYP3A5*1 allele [25]. Second, 6β-OHF/cortisol ratio reflects liver CYP3A4 activity and also extrahepatic activity. Nevertheless, most authors consider that 6β-OHF/cortisol ratio is useful non-invasive test to evaluate inducing or inhibiting properties of drugs, totally validated for induction, still under debate for some inhibition. The great advantage of this test is that there is no drug to be administered, as cortisol and 6β-OHF are natural metabolites.
Further studies are needed to establish possible correlations between CYP3A4 polymorphisms and 6β-OHF/cortisol urinary excretion. Comparative studies between 6β-OHF/cortisol excretion and other tests supposed to evaluate CYP3A activity must be performed. 6β-OHF/cortisol urinary excretion does not seem to be the appropriate test to measure the actual CYP3A activity, but the ideal probe has not yet been discovered.
Finally, the measurement of 6β-OHF excretion presents also new interest in certain pathologies such as breast cancer, as has been demonstrated very recently. Further studies must be conducted in different pathologies to examine the interest of 6β-OHF as biomarker of disease states.
Notes
Urinary 17-OHCS group: all the urinary steroids possessing a function 17,21 dihydroxy-20 cetone, i.e. di and tetrahydroxy derivatives of cortisol, cortisone and 11 deoxycortisol. This old nomenclature is no more in use as each of these compounds is now specifically measured.
Cytochrome P 448 is the old name of a family of cytochromes whose absorbance peak of the complex with carbon oxide shifted from 450 nm to 448 nm. In modern nomenclature, it refers mainly, but not exclusively, to CYP1A.
References
Conney AH (1967) Pharmacological implications of microsomal enzyme induction. Pharmacol Rev 19:317–366
Breckenridge A (1975) Clinical implications of enzyme induction. In: Parke DV (ed) Enzyme induction. Plenum Press, London, pp 273–301
Park BK, Breckenridge AM (1981) Clinical implications of enzyme induction and enzyme inhibition. Clin Pharmacokin 6:1–24
Okey AB, Roberts EA, Harper PA, Denison MS (1986) Induction of drug-metabolizing enzymes: mechanisms and consequences. Clin Biochem 19:132–141
Park BK, Kitteringham NR (1988) Relevance and means of assessing induction and inhibition of drug metabolism in man. In: Gibson GG (ed) Progress in drug metabolism. Taylor and Francis, London, pp 1–60
Watkins PB, Wrighton SA, Maurel P, Schuetz EG, Mendez-Picon G, Parker GA et al (1985) Protein identification of an inducible form of cytochrome P 450 in human liver. Proc Natl Acad Sci U S A 82:6310–6314
Watkins PB, Murray SA, Winkelman LG, Heuman DM, Wrighton SA, Guzelian PS (1989) Erythromycin breath test as an assay of glucocorticoid-inducible liver cytochromes P 450. Studies in rats and patients. J Clin Invest 83:688–697
Burstein S, Dorfman RI, Nadel EM (1954) 6β-hydroxycortisol—a new steroid in human urine. Arch Biochem Biophys 53:307–308
Thummel KE, Wilkinson GR (1998) In vitro and in vivo drug interactions involving human CYP3A. Annu Rev Pharmacol Toxicol 38:389–430
Ohnhaus EE, Park BK (1979) Measurement of urinary 6-β-hydroxycortisol excretion as an in vivo parameter in the clinical assessment of the microsomal enzyme-inducing capacity of antipyrine, phenobarbitone and rifampicin. Eur J Clin Pharmacol 15:139–145
Park BK (1981) Assessment of urinary 6β-hydroxycortisol as an in vivo index of mixed-function oxygenase activity. Br J Clin Pharmacol 12:97–102
Streetman DS, Bertino JS Jr, Nafziger AN (2000) Phenotyping of drug-metabolizing enzymes in adults: a review of in vivo cytochrome P 450 phenotyping probes. Pharmacogenetics 10:187–216
Morita K, Konishi H, Shimakawa H (1992) Fluconazole: a potent inhibitor of cytochrome P 450-dependent drug-metabolism in mice and humans in vivo. Comparative study with ketoconazole. Chem Pharm Bull (Tokyo) 40:1247–11251
Brockmeyer NH, Tillmann I, Mertins L, Barthel B, Goos M (1997) Pharmacokinetic interaction of fluconazole and zidovudine in HIV-positive patients. Eur J Med Res 2:377–383
Cohn GL, Upton V, Bondy PK (1961) The in vivo conversion of cortisol-4-C14 to 6β-hydroxycortisol-4-C14 by the human cirrhotic liver. J Clin Endocrinol Metab 21:1328–1331
Lipman MM, Katz FH, Jailer JW (1969) An alternate pathway for cortisol metabolism: 6β-hydroxycortisol production by human tissue slices. J Clin Endocrinol Metab 22:268–272
Miyabo S, Kishida S, Hisada T (1973) Metabolism and conjugation of cortisol by various dog tissues in vitro. J Steroid Biochem 4:567–576
Katz FH, Lipman MM, Frantz AG, Jailer JW (1962) The physiologic significance of 6β-hydroxycortisol in human corticoid metabolism. J Clin Endocrinol 22:71–77
Fukushima DK, Bradlow HL, Hellman L (1971) Effects of o,p’-DDD on cortisol and 6β-hydroxycortisol secretion and metabolism in man. J Clin Endocrinol 32:192–200
Frantz AG, Katz FH, Jailer JW (1961) 6β-hydroxycortisol and other polar corticosteroids: measurement and significance in human urine. J Clin Endocrinol Metab 21:1290–1303
Dixon R, Pennington GW (1969) 6β-hydroxycortisol metabolism in man. Steroids 13:529–538
Burstein S, Kimball HL, Klaiber EL, Gut M (1967) Metabolism of 2α- and 6β-hydroxycortisol in man: determination of production rates of 6β-hydroxycortisol with and without phenobarbital administration. J Clin Endocrinol 27:491–499
Ged C, Rouillon JM, Pichard L, Combalbert J, Bressot N, Bories P et al (1989) The increase in urinary excretion of 6β-hydroxycortisol as a marker of human hepatic cytochrome P 450 IIIA induction. Br J Clin Pharmacol 28:373–387
De Wildt SN, Kearns LH, Leeder JS, Van Den Anker JN (1999) Cytochrome P 450 3A: ontogeny and drug disposition. Clin Pharmacokinet 37:485–505
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J et al (2001) Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet 27:383–391
Guenguerich P (1999) Cytochrome P 450 3A4: regulation and role in drug metabolism. Annu Rev Pharmacol Toxicol 39:1–17
Hines RH, McCarver DG (2002) The ontogeny of human drug-metabolizing enzymes: phase I oxidative enzymes. J Pharmacol Exp Ther 300:355–360
Abel SM, Maggs JL, Back DJ, Park BK (1992) Cortisol metabolism by human liver in vitro. I. Metabolite identification and inter-individual variability. J Steroid Biochem Mol Biol 43:713–719
Abel SM, Back DJ (1993) Cortisol metabolism in vitro. III. Inhibition of microsomal 6β-hydroxylase and cytosolic 4-ene-reductase. J Steroid Biochem Mol Biol 46:827–832
Lemoine A, Azoulay D, Dennison A, Kiffel L, Pichard L, Furlan V et al (1994) FK 506 renal toxicity and lack of detectable cytochrome P 450 3A in the liver graft of a patient undergoing liver transplantation. Hepatology 20:1472–1477
Kolars JC, Lown KS, Schmiedlin-Ren P, Ghosh M, Fang C, Wrighton SA et al (1994) CYP3A gene expression in human gut epithelium. Pharmacogenetics 4:247–259
Schuetz EG, Schuetz JD, Grogan WM, Narray-Fejes-Toth A, Fejes-Toth G, Raucy J et al (1992) Expression of cytochrome P 450 3A in amphibian, rat, and human kidney. Arch Biochem Biophys 294:206–214
Werk EE, MacGee J, Sholiton LJ (1964) Altered cortisol metabolism in advanced cancer and other terminal illnesses: excretion of 6-hydroxycortisol. Metabolism 13:1425–1438
Corti P, Murratzu C, Sciarra GF, Corbini GF (1985) Dosaggio densitometrico del 6β-idrossi-cortisolo nelle urine. Boll Chim Farm 124:483–489
Yamaji T, Motohashi K, Murakawa S, Ibayashi H (1969) Urinary excretion of 6β-hydroxycortisol in states of altered thyroid function. J Clin Endocrinol 29:801–806
Thrasher K, Werk EE, Choi Y, Sholiton LJ, Meyer W, Olinger C (1969) The measurement, excretion, and source of urinary 6β-hydroxycortisol in humans. Steroids 14:455–468
Berman ML, Green OC (1971) Acute stimulation of cortisol metabolism by pentobarbital in man. Anesthesiology 34:365–369
Pal SB (1980) A fluorimetric method for the determination of urinary 6β-hydroxycortisol in humans. J Steroid Biochem 13:1373–1377
Poland A, Smith D, Kuntzman R, Jacobson M, Conney AH (1970) Effect of intensive occupational exposure to DDT on phenylbutazone and cortisol metabolism in human subjects. Clin Pharmacol Ther 11:724–732
Werk EE, MacGee J, Sholiton LJ (1964) Effect of diphenylhydantoin on cortisol metabolism in man. J Clin Invest 43:1824–1835
Ghosh PC, Pennington GW (1969) A comparison of gas-liquid chromatography with colorimetric mathods for the estimation of extremely polar unconjugated corticosteroids in urine. Steroids 3:247–255
Kishida S, Fukushima DK (1977) Radioimmunoassay of 6β-hydroxycortisol in human plasma and urine. Steroids 30:741–749
Park BK (1978) A direct radioimmunoassay for 6β-hydroxycortisol in human urine. J Steroid Biochem 9:963–966
Nahoul K, Adeline J, Paysant F, Scholler R (1982) Radioimmunoassay of plasma and urine 6β-hydroxycortisol: levels in healthy adults and in hypercortisolemic states. J Steroid Biochem 17:343–350
Park BK, Rowe PH, Osborne M, Dean PDG (1976) Preparation of antisera specific for 6β-hydroxycortisol. Febs Lett 68:237–239
Bowler-Wong SJ, Hay DM, Lorscheider FL (1981) A protein-binding radioassay for 6 beta-hydroxycortisol: detection in pregnancy urine and amniotic fluid. Am J Obstet Gynecol 139:243–249
Roots I, Holbe R, Hövermann W, Nigam S, Heinemeyer G, Hildebrandt AG (1979) Quantitative determination by HPLC of urinary 6β-hydroxycortisol, an indicator of enzyme induction by rifampicin and antiepileptic drugs. Eur J Clin Pharmacol 16:63–71
Corti P, Lencioni E, Sciarra GF, Murratzu G (1983) Indagini cromatografiche in TLC e HPLC sul 6-β-idrossi-cortisolo in miscela con composti a struttura steroidea. Boll Chim Farm 122:297–307
Ono T, Tanida K, Shibata H, Konishi H, Shimakawa H (1986) High-performance liquid chromatographic determination of 6β-hydroxycortisol in urine. Chem Pharm Bull (Tokyo) 34:2522–2527
Lodovici M, Dolara P, Bavazzano P, Colzi A, Pistolesi V (1981) A new method for the determination of 6-beta-OH-cortisol in human urine. Clin Chim Acta 114:107–110
Dumont E, Sclavons M, Desager JP (1984) Use of an internal standard to assay 6β-hydroxycortisol in urine. J Liquid Chromatogr 7:2051–2057
Homma M, Beckerman K, Hayashi S, Jayewardene AL, Oka K, Gambertoglio JG et al (2000) Liquid chromatographic determination of urinary 6β-hydroxycortisol to assess cytochrome P 450 3A activity in HIV positive pregnant women. J Pharm Biomed Anal 23:629–635
Goto J, Shamsa F, Nambara T (1983) Studies on steroids CLXXXII. Determination of 6β-hydroxycortisol in urine by high-performance liquid chromatography with fluorescence detection. J Liquid Chromatogr 6:1977–1985
Bienvenu T, Rey E, Pons G, D’Athis P, Olive G (1991) A simple non-invasive procedure for the investigation of cytochrome P 450 IIIA-dependent enzymes in humans. Int J Clin Pharmacol Ther Toxicol 29:441–445
Bidart M, Lesgards G (1995) Direct injection analysis of 6β-hydroxycortisol and cortisol in urine by HPLC-UV with on-line ISRP precolumn. J Liquid Chromatogr 18:725–738
Lykkesfeldt J, Loft S, Poulsen HE (1994) Simultaneous determination of urinary free cortisol and 6β-hydroxycortisol by high-performance liquid chromatography to measure human CYP3A activity. J Chromatogr B Biomed Appl 660:23–29
Inoue S, Inokuma M, Harada T, Shibutani Y, Yoshitake T, Charles B et al (1994) Simultaneous high-performance liquid chromatographic determination of 6 β-hydroxycortisol and cortisol in urine with fluorescence detection and its application for estimating hepatic drug-metabolizing enzyme induction. J Chromatogr B Biomed Appl 661:15–23
Shibata N, Hayakawa T, Takata K, Hoshino N, Minouchi T, Yamaji A (1998) Simultaneous determination of glucocorticoids in plasma or urine by high-performance chromatography with precolumn fluorimetric derivatization by 9-anthroyl nitrile. J Chromatogr B Biomed Sci Appl 706:191–199
Joellenbeck L, Qian Z, Zarba A, Groopman JD (1992) Urinary 6β-hydroxycortisol/cortisol ratios measured by high-performance liquid chromatography for use as a biomarker for the human cytochrome P 450 3A4. Cancer Epidemiol Biomarkers Prev 1:567–572
Hosoda H, Sakai Y, Nambara T (1981) A direct enzyme immunoassay of 6β-hydroxycortisol in human urine. Chem Pharm Bull (Tokyo) 29:170–175
Zhiri A, Wellman-Bednawska M, Siest G (1986) ELISA of 6-beta-hydroxycortisol in human urine: diurnal variations and effects of antiepileptic therapy. Clin Chim Acta 157:267–276
Patel SB, Khatkhatay I, Desai MP, Betrabet SS, Toddywalla VS (1994) A sensitive ELISA for 6β-hydroxycortisol in urine using enzyme penicillinase (β-lactamase). J Steroid Biochem Mol Biol 48:293–296
Yeung JHK, Wong JKL, Park BK (1997) Development of a screening method for anti-6β-hydroxycortisol antibody using an enzyme-linked immunosorbent assay (ELISA) and its applications. Meth Find Exp Clin Pharmacol 19:79–86
Yeung JHK, Wong JKL, Park BK (1997) Development of a monoclonal antibody to 6β-hydroxycortisol and its application in an enzyme-linked immunosorbent assay (ELISA) for 6 β-hydroxycortisol in urine. J Pharmacol Toxicol Methods 38:71–79
Freche JP, Decolin D, Siest JP, Batt AM, Panis-Rouzier R, Siest G (1989) Variation chez l’homme de l’excrétion du 6-β-hydroxycortisol après administration d’un nouveau dérivé de l’isoquinoléine, PK-11195 (52028 RP). Thérapie 44:327–330
Horsmans Y, Desager JP, Harvengt C (1992) Absence of CYP3A genetic polymorphism assessed by urinary excretion of 6β-hydroxycortisol in 102 healthy subjects on rifampicin. Pharmacol Toxicol 71:258–261
Schrenzel J, Dayer P, Leeman T, Weidekamm E, Portmann R, Lew DP (1993) Influence of rifampin on fleroxacin pharmacokinetics. Antimicrob Agents Chemother 37:2132–2138
Rost KL, Brösicke H, Heinemeyer G, Roots I (1994) Specific and dose-dependent enzyme induction by omeprazole in human beings. Hepatology 20:1204–1212
Pellizzoni C, Poggesi I, Jorgensen NP, Edwards DMF, Paus E, Strolin Benedetti M (1996) Pharmacokinetics of reboxetine in healthy volunteers. Single against repeated oral doses and lack of enzymatic alterations. Biopharm Drug Dispos 17:623–633
Ng MCY, Young RP, Critchley JAJH, Leung NWY, Lau JWT, Li AKC (1996) Urinary 6β-hydroxycortisol excretion in Hong Kong Chinese patients with hepatocellular carcinoma and other chronic liver diseases. Cancer 77:1427–1433
Tomlinson B, Young RP, Ng MCY, Anderson PJ, Kay R, Critchley JAJH (1996) Selective liver enzyme induction by carbamazepine and phenytoin in Chinese epileptics. Eur J Clin Pharmacol 50:411–415
Seidegard J, Dahlström K, Kullberg A (1998) Effect of grapefruit juice on urinary 6β-hydroxycortisol/cortisol excretion. Clin Exp Pharmacol Physiol 25:379–381
Weber C, Schmitt R, Birnboeck H, Hopfgartner G, Eggers H, Meyers J et al (1999) Multiple-dose pharmacokinetics, safety, and tolerability of bosentan, an endothelin receptor antagonist, in healthy human male volunteers. J Clin Pharmacol 39:703–714
Hsieh KP, Lin YY, Cheng CL, Lai Ml, Lin MS, Siest JP et al (2001) Novel mutations of CYP3A4 in Chinese. Drug Metab Dispos 29:268–273
Ishibashi M, Takayama H, Nakagawa Y, Harima N (1988) Diethylhydrogensilyl-cyclic diethylsilylene derivatives in gas chromatography/mass spectrometry of hydroxylated steroids. V. Analysis of cortisol and 6β-hydroxycortisol in human urine. Chem Pharm Bull (Tokyo) 36:845–848
Palermo M, Gomez-Sanchez C, Roitman E, Shackleton CHL (1996) Quantitation of cortisol and related 3-oxo-4-ene steroids in urine using gas chromatography/mass spectrometry with stable isotope-labeled internal standards. Steroids 61:583–589
Furuta T, Matsuzawa M, Shibasaki H, Kasuya Y (2000) Simultaneous determination of 6β- and 6α-hydroxycortisols and 6β-hydroxycortisone in human urine by stable isotope dilution mass spectrometry. J Chromatogr B 738:367–376
Luceri F, Fattori S, Luceri C, Zorn M, Mannaioni P, Messeri G (2001) Gas chromatography-mass spectrometry measurement of 6beta-OH-cortisol/cortisol ratio in human urine: a specific marker of enzymatic induction. Clin Chem Lab Med 39:1234–1239
Ohno M, Yamaguchi I, Saiki K, Yamamoto I, Azuma J (2000) Specific determination of urinary 6beta-hydroxycortisol and cortisol by liquid chromatography-atmospheric pressure chemical ionization mass spectrometry. J Chromatogr B Biomed Sci Appl 746:95–101
Tang C, Kassahun K, McIntosh IS, Brunner J, Rodrigues AD (2000) Simultaneous determination of urinary free cortisol and 6β-hydroxycortisol by liquid chromatography-atmospheric pressure chemical ionization tandem mass spectrometry and its application for estimating hepatic CYP3A induction. J Chromatogr 742:303–313
Ohnhaus EE, Bürgi H, Burger A, Studer H (1981) The effect of antipyrine, phenobarbitol and rifampicin on thyroid hormone metabolism in man. Eur J Clin Invest 11:381–387
Zhiri A, Mayer HA, Michaux V, Wellman-Bednawska M, Siest G (1986) 6β-hydroxycortisol in serum and urine as determined by enzyme immunoassay on microtitre plates. Clin Chem 32:2094–2097
Gerber-Taras E, Park BK, Ohnhaus EE (1981) The estimation of 6β-hydroxycortisol in urine—a comparison of two methods: high performance liquid chromatography and radioimmunoassay. J Clin Chem Clin Biochem 19:525–527
Ohno M, Yamaguchi I, Ito T, Saiki K, Yamamoto I, Azuma J (2000) Circadian variation of the urinary 6β-hydroxycortisol to cortisol ratio that would reflect hepatic CYP3A activity. Eur J Clin Pharmacol 55:861–865
Lee C (1995) Urinary 6β-hydroxycortisol in humans: analysis, biological variations, and reference ranges. Clin Biochem 28:49–54
Forrester LM, Henderson CJ, Glancey MJ, Back DJ, Park BK, Ball SE et al (1992) Relative expression of cytochrome P 450 isozymes in human liver and association with the metabolism of drugs and xenobiotics. Biochem J 281:359–368
Yamamoto N, Tamura T, Kamyia Y, Sekine I, Kunitoh H, Saijo N (2000) Correlation between docetaxel clearance and estimated cytochrome P 450 activity by urinary metabolite of exogenous cortisol. J Clin Oncol 18:2301–2308
Yamamoto N, Kamiya Y, Nakamura Y, Onodera R, Ito R, Sekine I et al (1999) Good correlation of docetaxel pharmacokinetics (PK) with cytochrome P 450 (CYP3A4) activity, evaluated by exogenous cortisol metabolite in urine (abstract). Am Assoc Clin Oncol 18
Barton RN, Horan MA, Weijers JWM, Sakkee AN, Roberts NA, Van Bezooijen CFA (1993) Cortisol production rate and the urinary excretion of 17-hydroxycorticosteroids, free cortisol, and 6β-hydroxycortisol in healthy elderly men and women. J Gerontol 48:M213–M218
Inagaki K, Inagaki M, Kataoka T, Sekido I, Gill MA, Nishida M (2002) A wide interindividual variability of urinary 6beta-hydroxycortisol to free cortisol in 487 healthy Japanese subjects in near basal condition. Ther Drug Monit 24:722–727
Beyeler C, Frey BM, Bird HA (1997) Urinary 6β-hydroxycortisol excretion in rheumatoid arthritis. Br J Rheumatol 36:54–58
Frey FJ, Frey BM (1983) Urinary 6β-hydroxyprednisolone excretion indicates enhanced prednisolone catabolism. J Lab Clin Med 101:593–604
Saenger P, Forster E, Kream J (1981) 6β-hydroxycortisol: a noninvasive indicator of enzyme induction. J Clin Endocrinol Metab 52:381–384
Voccia E, Saenger P, Peterson RE, Rauh W, Gottesdiener K, Levine LS et al (1979) 6β-hydroxycortisol excretion in hypercortisolemic states. J Clin Endocrinol Metab 48:467–471
Saenger P, Voccia E, Gunczler P, Rauh W, New MI (1978) 6β-hydroxycortisol (6OHF) as indicator of altered cortisol (F) metabolism. Ped Res 12:1092
Nakamura J, Yakata M (1985) Age- and sex-related differences in urinary excretion of 6β-hydroxycortisol in humans. Clin Chim Acta 152:193–197
Dolara P, Lodovici M, Salvadori M, Zaccara G, Muscas GC (1987) Urinary 6-beta-OH-cortisol and paracetamol metabolites as a probe for assessing oxidation and conjugation of chemicals in humans. Pharmacol Res Commun 19:261–273
Patel SB, Toddywalla VS, Betrabet SS, Kulkarni RD, Kombo I, Saxena BN (1996) Age-related changes in urinary 6β-hydroxycortisol in normal infants. Indian Pediatr 33:398–401
Toddywalla VS, Patel SB, Betrabet SS, Kulkarni RD, Kombo I, Saxena BN (1995) Can chronic maternal drug therapy alter the nursing infant’s hepatic drug metabolizing enzyme pattern? J Clin Pharmacol 35:1025–1029
Vauzelle-Kervroedan F, Rey E, Pariente-Khayat A, Bienvenu T, Badoual J, Olive G et al (1996) Non-invasive in vivo study of the maturation of CYP IIIA in neonates and infants. Eur J Clin Pharmacol 51:69–72
Nakamura H, Hirai M, Ohmori S, Ohsone Y, Obonai T, Sugita K et al (1998) Changes in urinary 6β-hydroxycortisol/cortisol ratio after birth in human neonates. Eur J Clin Pharmacol 53:343–346
Nakamura H, Hasegawa A, Kimura M, Yamagata SI, Nakasa H, Osada H et al (1999) Comparison of urinary 6β-hydroxycortisol/cortisol ratio between neonates and their mothers. Br J Clin Pharmacol 47:31–34
Burstein AH, Reiss WG, Kantor E, Anderson GD (1998) Cytochrome P 450 3A4 activity in premenopausal and postmenopausal women based on 6β-hydroxycortisol:cortisol ratios. Pharmacotherapy 18:1271–1276
Lin Y, Anderson GD, Kantor E, Ojemann LM, Wilensky AJ (1999) Differences in the urinary excretion of 6β-hydroxycortisol/cortisol between Asian and Caucasian women. J Clin Pharmacol 39:578–582
Frantz AG, Katz FH, Jailer JW (1960) 6β-hydroxycortisol: high levels in human urine in pregnancy and toxemia. Proc Soc Exp Biol Med 105:41–43
Ohkita C, Goto M (1990) Increased 6β-hydroxycortisol excretion in pregnant women: implication of drug-metabolizing enzyme induction. DICP Ann Pharmacother 24:814–816
Cumming DC, Love EJ, Lorscheider FL (1981) 6β-hydroxycortisol levels in maternal urine of pregnancies complicated by prematurity. Am J Obstet Gynecol 139:250–253
Hunter DJS, Keane P, Walker WHC, YoungLai EV (1984) Variations in urinary levels of free 6β-hydroxycortisol, cortisol, and estrogens in late pregnancy. Gynecol Obstet Invest 18:83–87
Saenger P (1983) 6β-hydroxycortisol in random urine samples as an indicator of enzyme induction. Clin Pharmacol Ther 34:818–821
YoungLai EV, Hunter DJS (1987) Diurnal variation in the excretion of 6β-hydroxycortisol and estriol at 32 weeks gestation. Gynecol Obstet Invest 23:157–159
McCune J, Lindley C, Sawyer W, Williamson K, Kashuba A, Pieper J (1998) Comparison of 24-hour and morning 6βOHcortisol: cortisol ratio in men, women on oral contraceptives (OC) and women not on OC. Clin Pharmacol Ther 63:219
Nakamura J, Yakata M (1989) Assessing adrenocortical activity by determining levels of urinary free cortisol and urinary 6β-hydroxycortisol. Acta Endocrinol (Copenh) 120:277–283
Tran JQ, Kovacs SJ, McIntosh TS, Davis HM, Martin DE (1999) Morning spot and 24-hour urinary 6β-hydroxycortisol to cortisol ratios: intraindividual variability and correlation under basal conditions and conditions of CYP3A4 induction. J Clin Pharmacol 39:487–494
Nakamura J, Yakata M (1985) Determination of urinary cortisol and 6β-hydroxycortisol by high performance liquid chromatography. Clin Chim Acta 149:215–224
Özdemir V, Kalow W, Tang BK, Paterson AD, Walker SE, Endrenyi L et al (2000) Evaluation of the genetic component of variability in CYP3A4 activity: a repeated drug administration method. Pharmacogenetics 10:373–388
Rebbeck TR, Jaffe JM, Walker AH, Wein AJ, Malkowicz SB (1998) Modification of clinical presentation of prostate tumors by a novel genetic variant in CYP3A4. J Natl Cancer Inst 90:1225–1229
Walker AH, Jaffe JM, Gunasegaram S, Cummings SA, Huang CS, Chern HD et al (1998) Characterization of an allelic variant in the nifedipine-specific element CYP3A4: ethnic distribution and implications for prostate cancer risk. Hum Mutat 12:289
Van Schaik RHN, De Wildt SN, Van Iperen NM, Uitterlinden AG, Van der Anker JN, Lindemans J (2000) CYP3A4-V polymorphism detection by PCR-restriction fragment length polyporphism analysis and its allelic frequency among 199 Dutch Caucasians. Clin Chem 46:1834–1836
Wandel C, Witte JS, Hall JM, Stein CM, Wood AJJ, Wilkinson GR (2000) CYP3A activity in African American an European American men: population differences and functional effect of CYP3A4*1B5’-promoter region polymorphism. Clin Pharmacol 68:82–91
Rivory LP, Qin H, Clarke SJ, Eris J, Duggin G, Ray E et al (2000) Frequency of cytochrome P 450 3A4 variant genotype in transplant population and lack of association with ciclosporin clearance. Eur J Clin Pharmacol 56:395–398
Sata F, Sapone A, Elizondo G, Stocker P, Miller VP, Zheng W et al (2000) CYP3A4 allelic variants with amino acid substitutions in exons 7 and 12: evidence for an allelic variant with altered catalytic activity. Clin Pharmacol Ther 67:48–56
Weslind A, Lofberg L, Tindberg N, Andersson TB, Ingelman-Sundberg M (1999) Interindividual differences in hepatic expression of CYP3A4: relationship to genetic polymorphism in the 5’-upstream regulatory region. Biochem Biophys Res Commun 259:201–205
Van Schaik RHN, De Wildt SN, Brosens R, Van Fessem M, Van der Anker JN, Lindemans J (2001) The CYP3A4*3 allele: is it really rare? Clin Chem 47:1104–1106
Lamba JK, Lin YS, Thummel K, Daly A, Watkins PB, Strom S et al (2002) Common allelic variants of cytochrome P 450 3A4 and their prevalence in different populations. Pharmacogenetics 12:121–132
Park BK, Eichelbaum M, Ohnhaus EE (1982) 6β-hydroxycortisol excretion in relation to polymorphic N-oxidation of sparteine. Br J Clin Pharmacol 13:737–740
Eichelbaum M, Mineshita S, Ohnhaus EE, Zekorn C (1986) The influence of enzyme induction on polymorphic sparteine oxidation. Br J Clin Pharmacol 22:49–53
Leclercq V, Desager JP, Horsmans Y, Van Nieuwenhuyze Y, Harvengt C (1989) Influence of rifampicin, phenobarbital and cimetidine on mixed function monooxygenase in extensive and poor metabolizers of debrisoquine. Int J Clin Pharmacol Ther Toxicol 27:593–598
Timbrell JA, Park BK, Harland SJ (1985) A study of the effects of rifampicin on isoniazid metabolism in human volunteer subjects. Hum Toxicol 4:279–285
Price DE, Mehta A, Park BK, Hay A, Feely MP (1986) The effect of low-dose phenobarbitone on three indices of hepatic microsomal enzyme induction. Br J Clin Pharmacol 22:744–747
Desager JP, Dumont E, Harvengt C (1987) The urinary 6β-hydroxycortisol excretion in man on inducers and inhibitors of the hepatic mixed function oxidase. Pharmacol Ther 33:197–199
Ohnhaus EE, Breckenridge AM, Park BK (1989) Urinary excretion of 6β-hydroxycortisol and the time course measurement of enzyme induction in man. Eur J Clin Pharmacol 36:39–46
Challiner M, Park BK, Odum J, Orton TC (1981) The effect of 3-methylcholanthrene on urinary 6β-hydroxycortisol excretion and hepatic enzyme activity in the marmoset monkey (Callithrix jacchus). Biochem Pharmacol 30:2131–2134
Breckenridge A, Orme M, Thorgeirsson S, Davies DS, Brooks RV (1971) Drug interactions with warfarin: studies with dichloralphenazone, chloral hydrate and phenazone (antipyrine). Clin Sci 40:351–364
Ohnhaus EE, Kirchhof B, Peheim DVM (1979) Effect of enzyme induction on plasma lipids using antipyrine, phenobarbital, and rifampicin. Clin Pharmacol Ther 25:591–597
Ohnhaus EE, Park BK, Colombo JP, Heizmann P (1979) The effect of enzyme induction on diazepam metabolism in man. Br J Clin Pharmacol 6:557–563
Ohnhaus EE, Noelpp UB, Ramos MR (1985) Liver blood flow and enzyme induction in man. Hepato-gastroenterol 32:61–64
Ohnhaus EE, Brockmeyer N, Dylewicz P, Habicht H (1987) The effect of antipyrine and rifampin on the metabolism of diazepam. Clin Pharmacol Ther 42:148–156
Bammel A, Van der Mee K, Ohnhaus EE, Kirch W (1992) Divergent effects of different enzyme-inducing agents on endogenous and exogenous testosterone. Eur J Clin Pharmacol 42:641–644
Rapeport WG, McInnes GT, Thompson GG, Forrest G, Park BK, Brodie MJ (1983) Hepatic enzyme induction and leucocyte delta-aminolaevulinic acid synthase activity: studies with carbamazepine. Br J Clin Pharmacol 16:133–137
Wietholtz H, Zysset Th, Kreiten K, Kohl D, Büchsel R, Matern S (1989) Effect of phenytoin, carbamazepine, and valproic acid on caffeine metabolism. Eur J Clin Pharmacol 36:401–406
Pirmohamed M, Allott R, Green VJ, Kitteringham NR, Chadwick D, Park BK (1994) Lymphocyte microsomal epoxide hydrolase in patients on carbamazepine therapy. Br J Clin Pharmacol 37:577–581
Lucas RA, Gilfillan DJ, Bergstrom RF (1998) A pharmacokinetic interaction between carbamazepine and olanzapine: observations on possible mechanism. Eur J Clin Pharmacol 54:639–643
Brämswig S, Kerksiek A, Sudhop T, Luers C, Von Bergmann K, Berthold HK (2002) Carbamazepine increases atherogenic lipoproteins: mechanism of action in male adults. Am J Physiol Heart Circ Physiol 282:H704–H716
Moreland TA, Park BK, Rylance GW (1982) Microsomal enzyme induction in children: the influence of carbamazepine treatment on antipyrine kinetics, 6β-hydroxycortisol excretion and plasma γ-glutamyltranspeptidase activity. Br J Clin Pharmacol 14:861–865
Conney AH, Jacobson M, Schneidman K, Kuntzman R (1965) Induction of liver microsomal cortisol 6β-hydroxylase by diphenylhydantoin or phenobarbital: an explanation for increased excretion of 6-hydroxycortisol in humans treated with these drugs. Life Sci 4:1091–1098
Brooks SM, Werk EE, Ackerman SJ, Sullivan I, Thrasher K (1972) Adverse effects of phenobarbital on corticosteroid metabolism in patients with bronchial asthma. N Engl J Med 286:1125–1128
Hildebrandt AG, Roots I, Speck M, Saalfrank K, Kewitz H (1975) Evaluation of in vivo parameters of drug metabolizing enzyme activity in man after administration of clemastine, phenobarbital or placebo. Eur J Clin Pharmacol 8:327–336
Latham AN, Turner P, Franklin C, Maclay W (1976) Phenobarbitone-induced urinary excretions of D-glucaric acid and 6β-hydroxycortisol in man. Can J Physiol Pharmacol 54:778–782
Park BK, Wilson AC, Kaatz G, Ohnhaus EE (1984) Enzyme induction by phenobarbitone and vitamin K1 disposition in man. Br J Clin Pharmacol 18:94–97
Pinquier JL, Joseph X, Delaforge M, Lejus C, Boucher Jl, De Lauture D et al (1993) Lack of effect of phenobarbital on ex vivo leukocyte oxydative metabolism in healthy volunteers. Fundam Clin Pharmacol 7:311–317
Goldberg MR, Lo MW, Deutsch PJ, Wilson SE, McWilliams EJ, McCrea JB (1996) Phenobarbital minimally alters plasma concentrations of losartan and its active metabolite E-3174. Clin Pharmacol Ther 59:268–274
Thompson GA, St Peter JV, Heise MA, Horowitz ZD, Salyers GC, Charles TT et al (1996) Assessment of doxylamine influence on mixed function oxidase activity upon multiple dose oral administration to normal volunteers. J Pharm Sci 85:1242–1247
Southren AL, Gordon GG, Tochimoto S, Krikun E, Krieger D, Jacobson M et al (1969) Effect of N-phenylbarbital (phetharbital) on the metabolism of testosterone and cortisol in man. J Clin Endocrinol 29:251–256
Kuntzman R, Jacobson M, Levin W, Conney AH (1968) Stimulatory effect of N-phenobarbital (phetharbital) on cortisol hydroxylation in man. Biochem Pharmacol 17:565–571
Ballinger B, Browning M, O’Malley K, Stevenson IH (1972) Drug-metabolizing capacity in states of drug dependence and withdrawal. Br J Pharmacol 45:638–643
Crowley JJ, Cusack BJ, Jue SG, Koup JR, Park BK, Vestal RE (1988) Aging and drug interactions. II. Effect of phenytoin and smoking on the oxidation of theophylline and cortisol in healthy men. J Pharmacol Exp Ther 245:513–523
Fleishaker JC, Pearson LK, Peters GR (1995) Phenytoin causes a rapid increase in 6 β-hydroxycortisol urinary excretion in humans—a putative measure of CYP3A induction. J Pharm Sci 84:292–294
Fleishaker JC, Pearson LK, Peters GR (1998) Induction of tirilazad clearance by phenytoin. Biopharm Drug Dispos 19:91–96
Konishi H, Takenaka A, Minouchi T, Yamaji A (2001) Impairment of CYP3A4 capacity in patients receiving danazol therapy: examination on oxidative cortisol metabolism. Horm Metab Res 33:628–630
McColl KE, Thompson GG, El Omar E, Moore MR, Park BK, Brodie MJ (1987) Effect of rifampicin on haem and bilirubin metabolism in man. Br J Clin Pharmacol 23:553–559
Ohnhaus EE, Studer H (1983) A link between liver microsomal enzyme activity and thyroid hormone metabolism in man. Br J Clin Pharmacol 15:71–73
Scott AK, Haynes BP, Schinkel KD, Ohnhaus EE, Park BK (1987) Hepatic enzyme induction and vitamin K1 elimination in man. Eur J Clin Pharmacol 33:93–95
Schulte HM, Mönig H, Benker G, Pagel H, Reinwein D, Ohnhaus EE (1987) Pharmacokinetics of aldosterone in patients with Addison’s disease: effect of rifampicin treatment on glucocorticoid and mineralocorticoid metabolism. Clin Endocrinol 27:655–662
Perucca E, Grimaldi R, Frigo GM, Sardi A, Mönig H, Ohnhaus EE (1988) Comparative effects of rifabutin and rifampicin on hepatic microsomal enzyme activity in normal subjects. Eur J Clin Pharmacol 34:595–599
Wietholtz H, Zysset T, Marschall HU, Generet K, Matern S (1995) The influence of rifampin treatment on caffeine clearance in healthy man. J Hepatol 22:78–81
Kovarik JM, Hartmann S, Figueiredo J, Rouilly M, Port A, Rordorf C (2002) Effect of rifampin on apparent clearance of everolimus. Ann Pharmacother 36:981–985
Apseloff G, Hilligoss DM, Gardner MJ, Henry EB, Inskeep PB, Gerber N et al (1991) Induction of fluconazole metabolism by rifampin: in vivo study in humans. J Clin Pharmacol 31:358–361
Watkins PB, Turgeon DK, Saenger P, Lown KS, Kolars JC, Hamilton T et al (1992) Comparison of urinary 6β-hydroxycortisol and the erythromycin breath test as measures of hepatic P 450 IIIA (CYP3A) activity. Clin Pharmacol Ther 52:265–273
Borin MT, Chambers JH, Carel BJ, Gagnon S, Freimuth WW (1997) Pharmacokinetic study of the interaction between rifampin and delavirdine mesylate. Clin Pharmacol Ther 61:544–553
Saima S, Furuie K, Yoshimoto H, Fukuda J, Hayashi T, Echizen H (2002) The effects of rifampicin on the pharmacokinetics and pharmacodynamics of orally administered nilvadipine to healthy subjects. Br J Clin Pharmacol 53:203–206
Spaans E, Van Den Heuvel MW, Schnabel PG, Peeters PA, Chin-Kon-Sung UG, Colbers EP et al (2002) Concomitant use of mirtazapine and phenytoin: a drug–drug interaction study in healthy male subjects. Eur J Clin Pharmacol 58:423–429
Birmingham AT, Coleman AJ, Orme M, Parl BK, Pearson NJ, Short AH et al (1978) Antibacterial activity in serum and urine following oral administration in man of DL473 (a cyclopentyl derivative of rifampicin). Br J Clin Pharmacol 6:455P–456P
Ohnhaus EE, Gerber-Taras E, Park BK (1983) Enzyme-inducing drug combinations and their effects on liver microsomal enzyme activity in man. Eur J Clin Pharmacol 24:247–250
Kovacs SJ, Martin DE, Everitt DE, Patterson SD, Jorkasky DK (1998) Urinary excretion of 6β-hydroxycortisol as an in vivo marker for CYP3A induction: applications and recommendations. Clin Pharmacol Ther 63:617–622
Keung A, Reith K, Eller MG, McKenzie KA, Cheng L, Weir SJ (1999) Enzyme induction observed in healthy volunteers after repeated administration of rifapentine and its lack of effect on steady-state rifapentine pharmacokinetics: part I. Int J Tuberc Lung Dis 3:426–436
Reichel C, Block W, Skodra T, Traber F, Schiedermaier P, Spengler U et al (1997) Relationship between cytochrome P 450 induction by rifampicin, hepatic volume and portal blood flow in man. Eur J Gastroenterol Hepatol 9:975–979
Hoensch HP, Balzer K, Dylewizc P, Kirch W, Goebell H, Ohnhaus EE (1985) Effect of rifampicin treatment on hepatic drug metabolism and serum bile acids in patients with primary biliary cirrhosis. Eur J Clin Pharmacol 28:475–477
Hoener BA (1994) Predicting the hepatic clearance of xenobiotics in humans from in vitro data. Biopharm Drug Dispos 15:295–304
Vital Durand D, Hampden C, Boobis AR, Park BK, Davies DS (1986) Induction of mixed function oxidase activity in man by rifapentine (MDL 473), a long-acting rifamycin derivative. Br J Clin Pharmacol 21:1–7
Park BK (1987) In vivo methods to study enzyme induction and enzyme inhibition. Pharmacol Ther 33:109–113
Bammel A, Monig H, Zurborn KH, Ohnhaus EE, Kirch W (1989) Probenecid affects liver metabolism. Schweiz Med Wochenschr 118:1831–1834
Kuntzman R, Jacobson M, Conney AH (1966) Effect of phenylbutazone on cortisol metabolism in man. Pharmacologist 8:195
Bauer S, Stormer E, Kerb A, Brockmöller J, Roots I (2002) Differential effects of Saint John’s Wort (hypericum perforatum) on the urinary excretion of D-glucaric acid and 6beta-hydroxycortisol in healthy volunteers. Eur J Clin Pharmacol 58:581–585
Roby CA, Anderson GD, Kantor E, Dryer DA, Burstein AH (2000) St. John’s Wort: effect on CYP3A4 activity. Clin Pharmacol Ther 67:451–457
Kane GC, Lipsky JJ (2000) Drug-grapefruit juice interactions. Mayo Clin Proc 75:933–942
Fuhr U, Müller-Peltzer H, Kern R, Lopez-Rojas P, Jünemann M, Harder S et al (2002) Effects of grapefruit juice and smoking on verapamil concentrations in steady state. Eur J Clin Pharmacol 58:45–53
Mohri K, Uesawa Y, Sagawa KI (2000) Effects of long-term grapefruit juice ingestion on nifedipine pharmacokinetics: induction of rat hepatic P 450 by grapefruit juice. Drug Metab Dispos 28:482–486
Morita K, Yamakawa M, Minouchi T, Hayashi Y, Hoshino N, Konishi H et al (1989) Ozagrel hydrochloride monohydrate, a thromboxane synthase inhibitor, and its metabolites as inhibitors of hepatic microsomal drug metabolism. Chem Pharm Bull (Tokyo) 37:3351–3354
Tran A, Rey E, Pons G, Rousseau M, D’Athis P, Olive G et al (1997) Influence of stiripentol on cytochrome P 450-mediated metabolic pathways in humans: in vitro and in vivo comparison and calculation of in vivo inhibition constants. Clin Pharmacol Ther 62:490–504
Uzzan B, Nicolas P, Perret G, Vassy R, Tod M, Petitjean O (1991) Effects of troleandomycin and josamycin on thyroid hormone and steroid serum levels, liver function tests and microsomal monooxygenases in healthy volunteers: a double blind placebo-controlled study. Fundam Clin Pharmacol 5:513–526
Back DJ, Tjia JF, Abel SM (1992) Azoles, allylamines and drug metabolism. Br J Dermatol 126:14–18
Fleishaker JC, Pearson PG, Wienkers LC, Pearson LK, Peters GR (1996) Biotransformation of tirilazad in humans: 2. Effect of ketoconazole on tirilazad clearance and oral bioavailability. J Pharmacol Exp Ther 277:991–998
Gass RJ, Gal J, Fogle PW, Detmar-Hanna D, Gerber JG (1998) Neither dapsone hydroxylation nor cortisol 6beta-hydroxylation detects the inhibition of CYP3A4 by HIV-1 protease inhibitors. Eur J Clin Pharmacol 54:741–747
Lillibridge JH, Liang BH, Kerr BM, Webber S, Quart B, Shetty BV et al (1998) Characterization of the selectivity and mechanism of human cytochrome P 450 inhibition by the human immunodeficiency virus-protease inhibitor nelfinavir mesylate. Drug Metab Dispos 26:609–616
Boulton DW, Arnaud P, DeVane CL (2001) A single dose of methadone inhibits cytochrome P 450 3A activity in healthy volunteers as assessed by the urinary cortisol ratio. Br J Clin Pharmacol 51:350–354
Micuda S, Hodac M, Sispera L, Parisek P, Pleskot M, Zimova G et al (2001) Influence of amiodarone on urinary excretion of 6β-hydroxycortisol in humans. Physiol Res 50:191–196
Ushiama H, Echizen H, Nachi S, Ohnishi A (2002) Dose-dependent inhibition of CYP3A activity by clarithromycin during Helicobacter pylori eradication therapy assessed by changes in plasma lansoprazole levels and partial cortisol clearance to 6beta-hydroxycortisol. Clin Pharmacol Ther 72:33–43
Karayalçin U, Takeda Y, Miyamori T, Morise T, Takeda R (1991) Effect of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor pravastatin on urinary 6β-hydroxycortisol excretion: a preliminary study. Steroids 56:598–600
Kuhnz W, Lofberg B (1995) Urinary excretion of 6β-hydroxycortisol in women during treatment with different oral contraceptive formulations. J Steroid Biochem Mol Biol 55:129–133
Hammerstein J, Daume E, Simon A, Winkler UH, Schindler AE, Back DJ et al (1993) Influence of gestodene and desogestrel as components of low-dose oral contraceptives on the pharmacokinetics of ethinyl estradiol (EE2), on serum CBG and on urinary cortisol and 6β-hydroxycortisol. Contraception 47:263–281
Boissonnat P, De Lorgeril M, Perroux V, Salen P, Batt AM, Barthelemy JC et al (1997) A drug interaction study between ticlopidine and cyclosporin in heart transplant recipients. Eur J Clin Pharmacol 53:39–45
Borin MT, Cox SR, Herman BD, Carel BJ, Anderson RD, Freimuth WW (1997) Effect of fluconazole on the steady-state pharmacokinetics of delavirdine in human immunodeficiency virus-positive patients. Antimicrob Agents Chemother 41:1892–1897
Kirch W, Spahn H, Kitteringham NR, Hutt HJ, Mutschler E, Ohnhaus EE (1984) Interaction between the beta-adrenoceptor blockers metoprolol and atenolol with amitriptyline and their effects on oxidative liver metabolism. Br J Clin Pharmacol 17:65S–68S
Fuchs W, Sennewald R, Klotz U (1994) Lansoprazole does not affect the bioavailability of oral contraceptives. Br J Clin Pharmacol 38:376–380
Klotz U, Reimann IW, Ohnhaus EE (1983) Effect of ranitidine on the steady state pharmacokinetics of diazepam. Eur J Clin Pharmacol 24:357–360
Staiger C, Schlicht F, Walter E, Gundert-Remy U, Hildebrandt R, De Vries J et al (1983) Effect of single and multiple doses of sulphinpyrazone on antipyrine metabolism and urinary excretion of 6β-hydroxycortisol. Eur J Clin Pharmacol 25:797–801
Kirch W, Rose I, Klingmann I, Pabst J, Ohnhaus EE (1986) Interaction of bisoprolol with cimetidine and rifampicin. Eur J Clin Pharmacol 31:59–62
Caraco Y, Zylber-Katz E, Granit L, Levy M (1990) Does restriction of caffeine intake affect mixed function oxidase activity and caffeine metabolism? Biopharm Drug Dispos 11:639–643
Vestal RE, Cusack BJ, Mercer GD, Dawson GW, Park BK (1987) Aging and drug interactions. I. Effect of cimetidine and smoking on the oxidation of theophylline and cortisol in healthy men. J Pharmacol Exp Ther 241:488–500
Chamberlain J (1971) The determination of urinary 6-oxygenated cortisol in evaluating liver function. Clin Chim Acta 34:269–271
Dolara P, Lodovici M, Salvadori M, Santoni G, Caderni G, Buiatti E et al (1983) Enzyme induction in humans exposed to styrene. Ann Occup Hyg 27:183–188
Bragt PC, Poppema A (1985) Excretion of 6β-hydroxycortisol (6β-OHF) by workers exposed to styrene. In: Abstracts of the International symposium on clinical and basic aspects of enzyme induction and inhibition. Essen, p 43
Moretti M, Villarini M, Scassellati-Sforzolini G, Monarca S, Libraro M, Fatigoni C et al (1996) Biological monitoring of genotoxic hazard in workers of the rubber industry. Environ Health Perspect 104:543–545
Verplanke AJ, Bloemen LJ, Brouwer EJ, Van Sitter NJ, Boogaard PJ, Herber RF et al (2000) Occupational exposure to cis-1,3-dichoropropene: biological effect monitoring of kidney and liver function. Occup Environ Med 57:745–751
Saenger P, Rosen JF (1981) 6β-hydroxycortisol excretion is a non-invasive and sensitive index of chelatable lead stores in children. In: Brown SS, Davies DS (eds) Organ-directed toxicity. Chemical indices and mechanisms. Pergamon Press, London, pp 297–303
Saenger P, Markowitz ME, Rosen JF (1984) Depressed excretion of 6β-hydroxycortisol in lead-toxic children. J Clin Endocrinol Metab 58:363–367
Touchstone JC, Blakemore WS (1961) Urinary 6β-hydroxycortisol in adrenocortical hyperfunction. J Clin Endocrinol Metab 21:263–270
Borkowski AJ, Marks PA, Katz FH, Lipman MM, Christy NP (1962) An abnormal pathway of steroid metabolism in patients with glucose-6-phosphate dehydrogenase deficiency. J Clin Invest 41:1346–1347
Geubel AP, Pauwels S, Buchet JP, Dumont E, Dive C (1985) Increased cyt P 450-dependent function in healthy HBsAg carriers. Abstracts of the international symposium on clinical and basic aspects of enzyme induction and inhibition. Essen, p 45
Eade OE, Maddison A, Leonard PJ, Wright R (1977) Ratio of urinary 6β-hydroxycortisol to 17-hydroxycorticosteroids in patients with liver disease. Digestion 16:169–174
Wensing G, Mönig H, Ohnhaus EE, Hoensch HP (1991) Pharmacokinetics of encainide in patients with cirrhosis. Cardiovasc Drugs Ther 5:733–739
Wild CP, Yin F, Turner PC, Chemin I, Chapot B, Mendy M et al (2000) Environmental and genetic determinants of aflatoxin-albumin addducts in the Gambia. Int J Cancer 86:1–7
Takeda Y, Miyamori I, Karayalçin U, Takeda R (1991) Influence of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, pravastatin, on corticosteroid metabolism in patients with heterozygous familial hypercholesterolemia. Horm Res 36:75–77
Anderson GD, Awan AB, Adams CA, Temkin NR, Winn HR (1998) Increases in metabolism of valproate and excretion of 6β-hydroxycortisol in patients with traumatic brain injury. Br J Clin Pharmacol 45:101–105
Zheng W, Jin F, Dunning LA, Shu XO, Dai Q, Wen WQ et al (2001) Epidemiological study of urinary 6beta-hydroxycortisol to cortisol ratio and breast cancer risk. Cancer Epidemiol Biomarkers Prev 10:237–242
Lown K, Kolars J, Turgeon K, Merion R, Wrighton SA, Watkins PB (1992) The erythromycin breath test selectively measures P 450 IIIA in patients with severe liver disease. Clin Pharmacol Ther 51:229–238
Hunt CM, Watkins PB, Saenger P, Stave GM, Barlascini N, Watlington TO et al (1992) Heterogeneity of CYP3A isoforms metabolizing erythromycin and cortisol. Clin Pharmacol Ther 51:18–23
Kinirons MT, O’Shea D, Downing TE, Fitzwilliam AT, Joellenbeck L, Groopman JD et al (1993) Absence of correlations among three putative in vivo probes of human cytochrome P 450 3A activity in young healthy men. Clin Pharmacol Ther 54:621–629
Kinirons MT, O’Shea D, Kim RB, Groopman JD, Thummel KE, Wood AJJ et al (1999) Failure of erythromycin breath test to correlate with midazolam clearance as a probe of cytochrome P 450 3A. Clin Pharmacol Ther 66:224–231
Gotzkowsky SK, Kashuba ADM, Hall W, Kulaway RW, Beck DJ, Rocci ML et al (1999) Poor correlation between 24-hour urinary 6β-hydroxycortisol: cortisol molar ratios (CMR) and plasma midazolam clearance (MDZ CL) as measures of hepatic CYP3A activity (abstract). Clin Pharmacol Ther 65:167
Lin YS, Dowling ALS, Quigley SD, Farin FM, Zhang J, Lamba J et al (2002) Co-regulation of CYP3A4 and CYP3A5 and contribution to hepatic and intestinal midazolam metabolism. Mol Pharmacol 62:162–172
Watkins PB (1994) Noninvasive tests of CYP3A enzymes. Pharmacogenetics 4:171–184
Abel SM, Back DJ, Maggs JL, Park BK (1993) Cortisol metabolism in vitro—II. Species difference. J Steroid Biochem Mol Biol 45:445–453
Burstein S, Kimball HL, Bhavnani BR (1963) Urinary corticosteroid excretion patterns in guinea pigs: 2 main phenotypes. Steroids 2:195
Kiernan TW, Luisada-Opper A, Ertel NH (1981) Hepatic microsomal induction in rat liver: heterogeneity of response. J Clin Pharmacol 21:280–283
Burstein S, Bhavnani BR (1967) Effect of phenobarbital administration on the in vitro hydroxylation of cortisol and on overall substrate and product metabolism in the guinea pig and rat. Endocrinology 80:351–356
Pirmohamed M, Kitteringham NR, Breckenridge AM, Park BK (1992) The effect of enzyme induction on the cytochrome P 450-mediated bioactivation of carbamazepine by mouse liver microsomes. Biochem Pharmacol 44:2307–2314
Challiner MR, Park BK, Odum J, Orton TC, Parker GL (1980) The effects of phenobarbitone on urinary 6β-hydroxycortisol excretion and hepatic enzyme activity in the marmoset monkey (Callithrix jacchus). Biochem Pharmacol 29:3319–3324
Totsuka S, Watanabe T, Koyanagi F, Tanaka K, Yasuda M, Manabe S (1999) Increase in urinary excretion of 6β-hydroxycortisol in common marmosets as a marker of hepatic CYP3A induction. Arch Toxicol 73:203–207
Huber R, Hartmann M, Bliesath H, Luhmann R, Steinijans VW, Zech K (1996) Pharmacokinetics of pantoprazole in man. Int J Clin Pharmacol Ther 34:185–194
Roots I, Ley B, Hildebrandt AG (1977) In vivo parameters of drug metabolism—differences in specificity towards inducing agents. In: Ullrich V, Roots E, Hildebrandt AG, Estabrook RW, Conney AH (eds) Microsomes and drug oxidations. Pergamon Press, Oxford, pp 581–588
Park BK, Challiner MR, Newby S (1983) The effects of phenobarbitone on urinary 6β-hydroxycortisol excretion and hepatic enzyme activity in the guinea-pig. J Steroid Biochem 18:453–457
Abu-Qare AW, Abou-Donia MB (2001) DEET (N,N-diethyl-m-toluamide) alone and in combination with permethrin increased urinary excretion of 6beta-hydroxycortisol in rats, a marker of hepatic CYP3A induction. J Toxicol Environ Health 64:373–384
Krause W, Träger H, Kühne G, Sauerbrey N, Gräf KJ, Dorow R (1990) Pharmacokinetics and endocrine effects of terguride in healthy subjects. Eur J Clin Pharmacol 38:609–615
Heller FR, Desager JP, Harvengt C (1988) Changes in plasma activities of lipolytic enzymes and lipids of normolipidemic subjects given phenobarbital, a strong microsomal inducer, alone or in combination with fenofibrate. Int J Clin Pharmacol Ther Toxicol 26:138–142
Goldberg DM (1980) Selected aspects of microsomal enzyme induction. In: Goldberg DM, Werner M (eds) Progress in clinical enzymology, Masson Publishing, USA, Inc., New York, pp 20–31
Morita K, Ono T, Shimakawa H (1988) Effects of antimycotics on hepatic steroid metabolism. J Pharmacobiodyn 11:808–815
Walter E, Staiger Ch, De Vries J, Weber E, Bitzer W, Degott M et al (1982) Enhanced drug metabolism after sulfinpyrazone treatment in patients aged 50 to 60 years. Klin Wochenschr 60:1409–1413
Koup JR, Anderson GD, Loi CM (1998) Effect of troglitazone on urinary excretion of 6β-hydroxycortisol. J Clin Pharmacol 38:815–818
Stevenson IH, Browning M, Crooks J, O’Malley K (1972) Changes in human drug metabolism after long-term exposure to hypnotics. Br Med J 4:322–324
Berman ML, Green OC, Calverley RK, Smith NT, Eger EI (1976) Enzyme induction by enflurane in man. Anesthesiology 44:496–500
Morita K, Shibata H, Ono T, Shimakawa H (1986) Inducing effect of feprazone on hepatic drug-metabolizing enzymes in man. Eur J Clin Pharmacol 31:117–118
Heinemeyer G, Roots I, Lestau P, Klaiber HR, Dennhardt R (1986) D-glucaric acid excretion in critical care patients—comparison with 6β-hydroxycortisol excretion and serum γ-glutamyltranspeptidase activity and relation to multiple drug therapy. Br J Clin Pharmacol 21:9-18
O’Malley K, Browning M, Stevenson I, Turnbull MJ (1973) Stimulation of drug metabolism in man by tricyclic antidepressants. Eur J Clin Pharmacol 6:102–106
Horsmans Y, Desager JP, Van den Berge V, Abrassart M, Harvengt C (1993) Effects of simvastatin and pravastatin on 6β-hydroxycortisol excretion, a potential marker of cytochrome P 450 3A Pharmacol Res 28:243–248
Morita K, Konishi H, Ono T, Shimakawa H (1987) A comparison of the inhibitory effects of roxatidine acetate hydrochloride and cimetidine on cytochrome P 450-mediated drug-metabolism in mouse hepatic microsomes and in man in vivo. J Pharmacobiodyn 10:287–295
Feely J, Robertson D, Island DP, Wood AJJ (1982) Cimetidine alters plasma catecholamine levels and cortisol and aldosterone excretion. N Engl J Med 306:1054
Macphee GJ, Thompson GG, Scobie G, Agnew E, Park BK, Murray T et al (1984) Effects of cimetidine on carbamazepine auto- and hetero-induction in man. Br J Clin Pharmacol 18:411–419
Orme M, Breckenridge A, Brooks RV (1972) Interactions of benzodiazepines with warfarin. Br Med J 3:611–614
Orme M, Back DJ, Ward S, Green S (1991) The pharmacokinetics of ethynylestradiol in the presence and absence of gestodene and desogestrel. Contraception 43:305–316
Rost KL, Mansmann U, Roots I (1997) Urinary 6β-hydroxycortisol and D-glucaric acid excretion rates are not affected by lansoprazole treatment. Int J Clin Pharmacol Ther 35:14–18
Larkin JG, McKee PJW, Forrest G, Beastall GH, Park BK, Lowrie JI et al (1991) Lack of enzyme induction with oxcarbazepine (600 mg daily) in healthy subjects. Br J Clin Pharmacol 31:65–71
Brocks DR, Upward JW, Georgiou P, Stelman G, Doyle E, Allen E et al (1996) The single and multiple dose pharmacokinetics of pranlukast in healthy volunteers. Eur J Clin Pharmacol 51:303–308
Dammann HG, Burkhardt F, Wolf N (1999) The effects of oral rabeprazole on endocrine and gastric secretory function in healthy volunteers. Aliment Pharmacol Ther 13:1195–1203
Ohnhaus EE, Gerber-Taras E (1984) The effect of spironolactone on the liver microsomal enzyme system in patients. Br J Clin Pharmacol 17:485–486
Thompson GG, Small M, Lowe GDO, Forbes CD, Park BK, Scobie G et al (1984) Effect of stanozolol on δ-aminolaevulinic acid synthase and hepatic monooxygenase activity in man and rat. Eur J Clin Pharmacol 26:587–950
Macphee GJ, Mitchell JR, Wiseman L, McLellan AR, Park BK, McInnes GT et al (1988) Effect of sodium valproate on carbamazepine disposition and psychomotor profile in man. Br J Clin Pharmacol 25:59–66
Horsmans Y, Desager JP, Pauwels S, Harvengt C (1991) Lack of effect by nifedipine on hepatic mixed function oxidase in man. Fundam Clin Pharmacol 5:193–201
Back DJ, Purba HS, Park BK, Ward SA, Orme ML (1983) Effect of chloroquine and primaquine on antipyrine metabolism. Br J Clin Pharmacol 16:497–502
Mönig H, Hoffman K, Ohnhaus EE, Schulte HM (1992) Ranitidine treatment and cortisol metabolism in man. Eur J Drug Metab Pharmacokinet 17:9–12
Yasui-Furukori N, Kondo T, Kubota T, Otake H, Ohkubo T, Nagasaki T et al (2001) No correlations between the urinary ratio of 6β-hydroxycortisol to free cortisol and pharmacokinetics of alprazolam. Eur J Clin Pharmacol 57:285–288
Svensson US, Ashton M, Trinh NH, Bertilsson L, Dinh XH, Nguyen Nguyen TN et al (1998) Artemisinin induces omeprazole metabolism in human beings. Clin Pharmacol Ther 64:160–167
Lefevre G, Bindschedler M, Ezzet F, Schaeffer N, Meyer I, Thomsen MS (2000) Pharmacokinetic interaction trial between co-artemether and mefloquine. Eur J Pharm Sci 10:141–151
Pichard-Garcia L, Hyland R, Baulieu J, Fabre JM, Milton A, Maurel P (2000) Human hepatocytes in primary culture predict lack of cytochrome P 450 3A4 induction by eletriptan in vivo. Drug Metab Dispos 28:51–57
Pageaux GP, Le Bricquir Y, Berthou F, Bressot N, Picot MC, Blanc F et al (1998) Effects of interferon-alpha on cytochrome P 450 isoforms 1A2 and 3A activities in patients with chronic hepatitis C. Eur J Gastroenterol Hepatol 10:491–495
Nowak SN, Edwards DJ, Clarke A, Anderson GD, Jaber LA (2002) Pioglitazone: effect on CYP3A4 activity. J Clin Pharmacol 42:1299–1302
Bartoli A, Gatti G, Cipolla G, Barzaghi N, Veliz G, Fattore C et al (1997) A double-blind, placebo-controlled study on the effect of vigabatrin on in vivo parameters of hepatic microsomal enzyme induction and on the kinetics of steroid oral contraceptives in healthy female volunteers. Epilepsia 38:702–707
Acknowledgement
We would like to warmly thank G. Sanderink, Aventis, for his help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galteau, M.M., Shamsa, F. Urinary 6β-hydroxycortisol: a validated test for evaluating drug induction or drug inhibition mediated through CYP3A in humans and in animals. Eur J Clin Pharmacol 59, 713–733 (2003). https://doi.org/10.1007/s00228-003-0690-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0690-3