Abstract
Objective
To document the effect of systematic evaluation of pain in neonates on prescription of intravenous analgesics in a level-III neonatal intensive care unit (NICU) as a marker of increased awareness of treating and preventing pain.
Methods
Retrospective analysis of the number of yearly prescribed vials of intravenous analgesics in a level-III NICU during a period before (1996–1999) and after (2000 to August 2002) introduction of a multidimensional pain scale. Correction was carried out by multiple regression analysis for clinical co-variables (admissions, days on parenteral nutrition, days on respiratory support, surgical procedures), which also might explain changes in prescription of analgesics. Postoperative length (hours) of administration of analgesics was calculated in a group of infants (1996–2001) who all received cryotherapy for threshold retinopathy of prematurity (ROP) before (1996–1999) and since (2000–2001) introduction of pain evaluation.
Results
The number of yearly prescribed vials increased from 3140±619 (mean±SD) to 5915±675 (P<0.005). There is also a significant increase in the number of surgical interventions (P<0.05) but not in days on respiratory support, days on parenteral nutrition or in number of admissions. After correction for the number of surgical procedures, the increase in prescribed vials remained significant (P<0.05). In infants who received cryotherapy, a significant increase in length of postoperative analgesia (65–107 h, P<0.01) was documented. Even after correction for the increased postoperative length of ventilation, duration of postoperative analgesia remained significantly (P<0.05) longer.
Conclusions
Systematic evaluation of pain increased awareness of treating and preventing pain in neonates, even after correction for clinical co-variables. This increase was not associated with an increase in potential side-effects (length of respiratory support, length of parenteral nutrition).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recognition and treatment of pain is an important indicator of quality of care delivered to patients [1]. Since the landmark publications of Anand in the late 1980s, the impact of adequate treatment of pain in neonates has also been well acknowledged [2, 3, 4, 5].
Systematic evaluation of pain likely improves awareness of the medical and nursing staff in optimising treatment, but a specific problem in neonates is objective assessment. We share this challenge in preverbal infants, with professionals taking care of severely mentally retarded, handicapped or comatose patients. Different pain scales have been developed and validated for the neonatal population as reviewed recently by us [6, 7].
To the best of our knowledge, this is the first study to examine the impact of the implementation of systematic evaluation of pain on prescriptive behaviour of analgesics in a level-III neonatal intensive care unit (NICU). Changes in intravenous analgesics (number of vials) and prescription behaviour after cryotherapy (length of postoperative analgesia) before and after the implementation of a pain scale were used as quantitative markers.
Methods
Data collection
The NICU Gasthuisberg is a tertiary neonatal intensive and high care unit, taking care of both premature infants and infants with congenital malformations. Perinatal data of all infants admitted in the unit since 1 January 1996 were available in a prospectively collected database. Clinical variables [total number of admissions, number of extreme low birth weight (ELBW, i.e. <1000 g) infants, days of parenteral nutrition, days on respiratory support and number of surgical interventions] that might influence consumption of analgesics were extracted from this database. Days of respiratory support and days on parenteral nutrition were used as markers of severity of medical disease, at the same time serving as markers of potential side-effects of opioids. Data on the number and type of drugs administered were extracted from the hospital pharmacy database. Intravenous analgesics used and studied during this period (1996 to August 2002) were fentanyl, tramadol, piritramide and propacetamol. There were no major changes in the medical or nursing staff during this period, nor were there changes in the composition of the vials. Data were reported on a yearly basis after extrapolation of the data for 2002 based on the first 8 months.
We also investigated prescription (postoperative hours) of analgesics in a cohort of infants who received cryotherapy for threshold retinopathy of prematurity (ROP) before and since systematic pain evaluation became the standard of care. Data on relevant co-variables (birth weight, weight at surgery, postoperative ventilation) were collected. Since laser therapy was introduced as the preferred treatment for retinal surgery in January 2002, only the period from 1996 to the end of 2001 was analysed [8].
Development and implementation of the Leuven neonatal pain scale
Based on literature and after discussion within the medical and nursing staff, a multi-dimensional pain scale was developed with seven items (sleep, facial appearance, crying, heart rate, motor tone, movement and consolability). Each variable was graded 0, 1 or 2 points, resulting in a maximal score of 14. After a preliminary trial during the direct postoperative period (n=10), infants admitted to the NICU were scored simultaneously by two caregivers (n=628 observations), blinded for each other. A strong inter-observer correlation (r=0.88) was observed with a cut-off point of 6 or above for infants in pain as used in the algorithm. We further validated this pain score during endotracheal aspiration (n=10), where we could demonstrate marked correlation (r=0.8) between increase in pain score and increase in serum catecholamines. Implementation in daily nursing care was achieved after all caregivers attended a training session during which the pain scale was introduced together with observations in the unit [9].
Standard analgesia protocol (therapeutic algorithm)
Analgesic treatment in post-surgical, ventilated infants was provided by continuous intravenous administration of fentanyl, 3 μg/kg/h (0.3 ml/h) after a loading dose (3–5 μg/kg i.v. bolus) was administered before transfer to the unit. Within 24 h, treatment with intravenous tramadol (5 mg/kg per day; 0.3 ml/h) in combination with propacetamol (4×10–20 mg/kg per day) was initiated to decrease fentanyl needs and to enable weaning. In post-surgical, non-ventilated infants, analgesia was provided by continuous administration of tramadol (5 mg/kg per day; 0.3 ml/h), while propacetamol (an intravenous pro-drug of paracetamol) (4×10–20 mg/kg per day) was administered as additional treatment. Continuous perfusions were increased by 0.1 ml/h if the pain scale was above 5 and decreased by 0.1 ml/h if the pain scale remained below 4 for at least 6 h. All continuous perfusions were changed every 24 h. In non-surgical infants, treatment was initiated if the pain score was above 5 by continuous fentanyl or tramadol administration in the same dose as mentioned above. Perfusions were adapted based on the same step-up/step-down as in surgical infants. The initial dose of fentanyl and propacetamol used in our study were in line with reports in literature while tramadol administration was extrapolated from data in infants and children [5, 10, 11, 12, 13]. Before introduction of the pain scale, administration and adaptation of analgesics were based on the subjective impression of the attending physician, but the same medications were used.
Statistics
All variables are reported on a yearly basis by mean and standard deviation (SD) in the period before (1996–1999) and since (2000 to August 2002) implementation. The student t-test was used in a univariate approach to compare both periods. ANOVA (MedCalc) was used for all clinical variables studied with an additional variable (pain score used or not during a given year) as factor. All significant co-variables were entered in a multiple regression model (MedCalc) to correct the trend in the number of prescribed vials of analgesics. The same approach was used to study prescriptive behaviour after cryotherapy (1996–2001).
Results
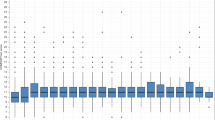
The mean number of yearly prescribed vials of intravenous analgesics before implementation (1996–1999) was 3140±619 (mean±SD). Since introduction of the pain scale, mean number of yearly prescribed vials increased to 5915±675 (P<0.005). Mean yearly number of opioid vials prescribed increased from 1473±395 to 2819±534 (P<0.05), while mean number of propacetamol vials increased from 1667±294 to 3096±434 (P<0.05). Mean yearly number of fentanyl vials increased from 908±241 to 1394±345 (P<0.05). There was no significant increase in days on respiratory support, in the number of admissions or in the number of ELBW infants admitted or in days of parenteral nutrition. There was a significant increase in the number of surgical procedures (P<0.05, Table 1).
Using ANOVA, with presence or absence of the pain scale in a given year as factor, the number of vials (P=0.005) and the number of surgical procedures (P=0.05) were significantly higher during the second period, while all other clinical variables were not. Even after correction for the increase in surgical procedures, the increase in the number of vials prescribed remained significant (P<0.05).
Cryotherapy for threshold ROP was performed in 42 infants during the studied period (1996–1999=30 and 2000–2001=12). Length of postoperative analgesics was 65±19 h and increased to 107±32 h (P<0.01) after systematic pain evaluation was introduced. The same trend was documented if only opioids were considered: 71±30 h versus 50.5±32 h (P<0.05). There were no significant differences in gestational age at birth and postconceptional age at surgery. Weight at birth (P<0.01) and weight at surgery (P<0.03) were significantly lower, and postoperative ventilation was significantly longer in the second group (P<0.005, Table 2). Using ANOVA, with presence or absence of pain score as factor, length of any analgesic treatment and opioids administered (both P=0.001) and length of postoperative ventilation (P=0.005) increased significantly. After correction for ventilation, weight at surgery and birth weight, pain score remained a significant independent variable (P<0.05) to explain the trend in the number of prescribed vials.
Discussion
To the best of our knowledge, this is the first study to examine the impact of the implementation of systematic evaluation of pain on prescriptive behaviour of analgesics in a level-III neonatal intensive unit.
Change in the number of analgesics prescribed was used as marker of improved awareness to treat and prevent pain. A significant increase in the vials used after introduction of systematic evaluation was documented. This increase was significant for all opioid vials, for fentanyl vials and also for propacetamol vials, reflecting an overall increase in consumption of intravenous analgesics. This change in prescriptive behaviour was also documented in a cohort of infants after a specific surgical procedure (cryotherapy), where a significant increase in duration of postoperative analgesia was documented.
There are overwhelming data in the literature supporting the relevance of adequate analgesia after surgery in neonates [2, 3, 4, 5]. Adequate postoperative analgesia is mandatory, even if this might prolong ventilation while in non-surgical, mostly premature infants, there is still debate whether adequate analgesia and/or sedation are mandatory [12, 13, 14, 15]. In the NOPAIN trial, pre-emptive analgesia by continuous low-dose morphine infusion (loading dose 100 μg/kg, maintenance dose 10–30 μg/kg/h) was well tolerated in ventilated pre-terms [14]. There was a (non-significant) trend in reduction of the incidence of poor neurological outcome in infants on morphine, likely based on reduction of fluctuations of blood pressure, decreased stress hormones, improved oxygenation and improved ventilator synchrony. The same trend was documented in a randomised placebo-controlled trial of fentanyl (0.5–2 μg/kg/h) infusion in pre-term infants with hyaline membrane disease [15]. Based on these and other studies, pre-emptive analgesia in ventilated infants is considered the standard of care in most neonatal units [5]. In this study, we could illustrate that systematic evaluation increased consumption of analgesics, without significant increase in respiratory support, in line with reports in the literature [14, 15]. Systematic evaluation by validated pain scale is mandatory in order to objectify the prescriptive behaviour. In addition to making prescriptions more objective, it might also improve awareness to treat and prevent pain as we illustrated in this study. This might not only be relevant in neonates and infants, but also in other groups of non-verbal (comatose, severely mentally retarded) patients. The risk of undertreatment of pain in non-verbal patients was recently illustrated in an adult intensive care population [16]. If pain is not measured, it's easy to ignore it.
Propacetamol is an intravenous pro-drug of paracetamol. There are still very few data of this specific drug in neonates, although paracetamol itself is frequently used for neonatal analgesia, especially after surgery [17]. During the period studied, doses administered were based on the report of Autret et al. [10]. Bypassing drug absorption variability and better accuracy of dose using an intravenous formula when compared with rectal or oral administration might improve effectiveness and predictability of its effects in ill neonates. Therefore, pharmacokinetics and dynamics of the specific intravenous formula should be studied in neonates.
Although prescription of intravenous analgesics was used as marker in this study, we wish to stress that pharmacological treatment is only part of a more extensive approach of comfort in neonates. An environment that reduces nociceptive stimuli and that enhances comfort is equally important in contemporary neonatal care. The switch in retinal surgery, from cryo- to less invasive laser therapy is an illustration of this integrated approach [6].
References
Philips DM (2000) JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA 284:428–429
Anand KJ, Hickey PR (1987) Pain and its effects in the human neonate and fetus. N Engl J Med 317:1321–1329
Anand KJ, Sippell WG, Aynsley-Green A (1987) randomised trial of fentanyl anaesthesia in preterm infants undergoing surgery: effects on stress response. Lancet 1:62–66
Anand KJS (1998) Clinical importance of pain and stress in preterm newborn infants. Biol Neonate 73:1–9
Anand KJ (2001) Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med 155:173–180
Stevens BJ, Johnston CC, Petryshen P, Taddio A (1996) Premature infant pain profile: development and initial validation. Clin J Pain 12:13–22
van Dijk M, Peters J, Bouwmeester J, Tibboel D (2002) Are postoperative pain instruments useful for specific groups of vulnerable infants? Clin Perinatol 29:469–491
Mc Gregor ML, Wherley AJ, Fellows RR, Bremer DL, Rogers GL, Letson AD (1998) A comparison of cryotherapy versus diode laser retinopexy in 100 consecutive infants treated for threshold retinopathy of prematurity. J AAPOS 2:360–364
Allegaert K, Tison D, De Jonge A, Naulaers G, Cossey V, Debeer A et al (2002) Measures to assess and to treat: the development of a neonatal pain scale (in Dutch). Ned Tijdschr Geneesk 58:155–161
Autret E, Dutertre JP, Breteau M, Jonville AP, Furet Y, Laugier J (1993) Pharmacokinetics of paracetamol in the neonate and infant after administration of propacetamol chlorhydrate. Dev Pharmacol Ther 20:129–134
Dayer P, Collart L, Desmeules J (1994) The pharmacology of tramadol. Drugs 47[Suppl 1]:3–7
Ambalavanan N, Carlo WA (1999) Analgesia for ventilated neonates: where do we stand? J Pediatr 135:403–405
Kennedy KA, Tyson JE (1999) Narcotic analgesia for ventilated newborns: are placebo-controlled trials ethical and necessary? J Pediatr 134:127–129
Anand KJ, Barton BA, McIntosch N, Lagercrantz H, Pelausa E, Young TE, Vasa R (1999) Analgesia and sedation in preterm neonates who require ventilatory support: results form the NOPAIN trial. Neonatal Outcome and Prolonged Analgesia in Neonates. Arch Pediatr Adolesc Med 153:331–338
Lago P, Benini F, Agosto C, Zacchello F (1998) Randomized controlled trial of low dose fentanyl infusion in preterm infants with hyaline membrane disease. Arch Dis Child Fetal Neonatal Ed 79:F194–F197
Bertolini G, Minelli C, Latronico N, Cattaneo A, Mura G, Melotti RM, Iapichino G (2002) The use of analgesic drugs in postoperative patients: the neglected problem of pain control in intensive care units. An observational, prospective, multicenter study in 128 Italian intensive care units. Eur J Clin Pharmacol 58:73–77
Anderson BJ, Van Lingen RA, Hansen TG, Lin YC, Holford NH (2002) Acetaminophen developmental pharmacokinetics in premature neonates and infants. Anesthesiology 96:1336–1345
Acknowledgements
G. Naulauers was supported by the Fund for Scientific Research, Flanders (Belgium), clinical doctoral grant A6/5 CM. D 11.354.
Author information
Authors and Affiliations
Corresponding author
Additional information
These results were partially presented at the biannual congress of the European Society of Developmental Pharmacology (ESDP, Liège, 25–28 October 2002) and at the annual meeting of the Belgian Society of Anesthesia and Resuscitation (BSAR, Brussels, 30 November 2002).
Rights and permissions
About this article
Cite this article
Allegaert, K., Tibboel, D., Naulaers, G. et al. Systematic evaluation of pain in neonates: effect on the number of intravenous analgesics prescribed. Eur J Clin Pharmacol 59, 87–90 (2003). https://doi.org/10.1007/s00228-003-0585-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0585-3