Abstract
Disturbances in mineral and bone metabolism are common in patients with chronic kidney disease (CKD), especially those undergoing dialysis. Renal osteodystrophy, which describes an alteration of bone morphology, is an important component of this systemic disorder and may explain the elevated risk of fracture which adversely affects morbidity and mortality. The most common form of renal osteodystrophy is high-turnover bone disease (osteitis fibrosa), which is induced by secondary hyperparathyroidism (SHPT). During the past decade, there has been considerable advances in the management of SHPT, with the introduction of the calcimimetic agents, the optimized use of nutritional and active vitamin D, and the accumulated experience with surgical parathyroidectomy. Studies supported that these advances could translate into improvement of renal bone disease and fracture prevention, as well as decreasing the risk of cardiovascular events and mortality. In this review, we summarize the available clinical evidence on the effect of old and new drugs on bone disorders in patients with CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
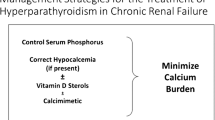
Disturbances in mineral metabolism and bone disease are common in patients with chronic kidney disease (CKD). Declines in kidney function lead to impaired phosphate excretion, positive phosphate balance, and elevated levels of fibroblast growth factor 23 (FGF23) [1]. The elevated FGF23 helps prevent hyperphosphatemia by stimulating urinary phosphate excretion, but it also suppresses biosynthesis of 1,25-dihydroxyvitamin D [1,25(OH)2D], leading to early development of secondary hyperparathyroidism (SHPT) [2, 3]. In advanced CKD, elevated serum phosphorus, decreased serum calcium, and skeletal resistance to PTH further contribute to increased synthesis of parathyroid hormone (PTH) and parathyroid cell proliferation. In the course of parathyroid hyperplasia, there is a progressive reduction in the expression of calcium-sensing receptor (CaSR) [4], vitamin D receptor (VDR) [5], and the Klotho-FGF receptor complex [6], which renders the parathyroid cells less responsive to extracellular calcium, 1,25(OH)2D, and FGF23, respectively, leading to further progression of SHPT [7].
These disorders in mineral metabolism are known as CKD-mineral and bone disorder (CKD-MBD), defined by the Kidney Disease: Improving Global Outcomes (KDIGO) [8]. Renal osteodystrophy (ROD), which describes an alteration of bone morphology in patients with CKD, is one component of the systemic disorder of CKD-MBD and may explain the elevated risk of fracture in these patients. The types of ROD can be defined on the basis of turnover and mineralization as follows: mild, osteitis fibrosa (hyperparathyroid bone disease), osteomalacia (mineralization defect), adynamic (low-turnover bone), and mixed [9]. Among these, the most common form is osteitis fibrosa [10], which is characterized by excessive rates of bone resorption by osteoclasts in response to high levels of PTH. Osteoblastic bone formation is also activated, but the newly formed bone matrix is inadequately mineralized and does not sufficiently compensate for the lost bone mass, leading to progressive bone loss and increased bone fragility. Indeed, the Dialysis Outcomes and Practice Patterns Study (DOPPS) demonstrated that intact PTH levels above 900 pg/ml are associated with an elevated risk for fracture [11], although conflicting results have been reported in smaller studies [12]. Therefore, the main purpose of managing SHPT is, although not limited to, to improve bone disease and ultimately reduce the risk of fracture.
Over the past 15 years, there has been considerable advances in the management of SHPT, with the introduction of the calcimimetic agents [13], the optimized use of nutritional and active vitamin D, and the accumulated experience with surgical parathyroidectomy (PTx). In this review, we summarize the available clinical evidence on the effect of old and new drugs on bone disorders in patients with CKD.
Active Vitamin D
Vitamin D metabolism is progressively altered in CKD. Physiologically, cholecalciferol (D3) [or ergocalciferol (D2)] are first hydroxylized in the liver into 25-hydroxyvitamin D (25(OH)D; calcifediol) which is subsequently hydroxylized in the kidney into 1,25(OH)2D (calcitriol) [14]. Calcitriol can then be regarded as a calcitropic steroid hormone facilitating calcium entry into the body and steering (suppressing) PTH secretion at the parathyroid gland.
In advancing CKD, it was long believed that the pure reduction in kidney mass limits the renal capacity to activate 25(OH)D, but now it is known that increasing serum levels of FGF23 powerfully inhibit renal 1α-hydroxylase activity leading to early and direct suppression of calcitriol synthesis independent of kidney mass [15]. Consequently, transient or sustained hypocalcemia and SHPT may develop.
Therefore, calcitriol or other active vitamin D analogues (alfacalcidol, doxercalciferol, paricalcitol, maxacalcitol etc.) were the mainstay of SHPT management in progressive and end-stage CKD for decades. However, over the last 20 years evidence accumulated that treatment indications must be carefully chosen due to the potential risk of hypercalcemia, extraosseous (especially cardiovascular) calcification and PTH oversuppression associated with the use active vitamin D compounds [16]. Furthermore, the stage of CKD, and SHPT, in which to start active vitamin D therapy are not clearly defined, since moderate elevations of PTH in stages G3a–G4 are probably adaptive in order to overcome bone resistance to PTH and to facilitate phosphate excretion. Accordingly, the KDIGO CKD-MBD guideline update 2017 stated that the “optimal PTH levels are not known” in CKD patients not on dialysis, advised to correct hypocalcemia, hyperphosphatemia and vitamin D deficiency if present, and consider more trends of increasing PTH levels than absolute levels [17].
Data from the Paricalcitol Capsule Benefits in Renal Failure–Induced Cardiac Morbidity (PRIMO) and Oral Paricalcitol in Stage 3–5 Chronic Kidney Disease (OPERA) trials caused additional caution with regard to the use of active vitamin D analogues in patients in CKD stages G3a–G4 [18, 19]. These two studies were designed to address the question, if paricalcitol could potentially regress or slow the progression of left ventricular hypertrophy in appropriate patient cohorts. This hypothesis was well based on preclinical, biological, and clinical pilot data linking VDRs in the myocardium with re-modeling via the local renin-angiotensin-system [20, 21]. However, over 1-year follow-up periods, no such cardiac benefits could be observed in these randomized controlled trials compared to placebo, while in both studies hypercalcemia occurred quite frequently (23% in PRIMO, 43% in OPERA) in the paricalcitol group and also trends in hyperphosphatemia development were seen versus placebo. Here, and based on these studies, the current KDIGO guideline now states that “calcitriol and vitamin D analogues not be routinely used” in CKD patients not on dialysis, and that it is reasonable to reserve their use “for patients with CKD G4–G5 with severe and progressive hyperparathyroidism” [17]. This change was perceived as quite a paradigm shift compared to past recommendations, but possibly also as a necessary step given the new knowledge of the active vitamin D associated adverse effects (increases in FGF23, progression of vascular calcification etc.).
In dialysis patients (CKD stage G5D), current recommendations are however different, and active vitamin D analogues are considered important in controlling and preventing autonomous progression of SHPT. The KDIGO guideline suggests that “calcimimetics, calcitriol, or vitamin D analogues, or a combination of calcimimetics with calcitriol or vitamin D analogues” can be administered in case PTH-lowering therapies are required, without imposing a hierarchy between these two groups of compounds [17]. Pragmatically, the presence of low calcium levels and well controlled phosphatemia would favor the use of active vitamin D analogues in dialysis patients, while hyperphosphatemia and calcium levels at the higher end would tip the scale towards calcimimetics.
The effects of calcitriol and active vitamin D compounds on bone turnover in CKD patients are quite strongly connected to their effects on PTH levels. More than three decades ago, Baker et al. showed that calcitriol protected against the development of histological evidence of osteitis fibrosa, but not of osteomalacia, in a bone biopsy-guided study of 76 hemodialysis patients [22]. In this instance, insufficient PTH lowering keeps an elevated bone turnover going, however, oversuppression leads to low turnover, the so-called adynamic bone. The latter seems associated with increased extraosseous calcification and calciphylaxis, thus creates a risk scenario, especially in dialysis patients, and should be avoided [23, 24]. What makes it difficult is that there are no definite PTH thresholds that can be given in order to improve guidance on treatment decisions, and there may be substantial differences in PTH target levels among populations (e.g. Japanese vs. Caucasian patients) [17, 25].
Bone mineral density (BMD) data under calcitriol treatment are only available for kidney transplant recipients in their first year after transplantation. Here, calcitriol is well able to protect from glucocorticoid bone loss [26], but no concise comments can be given on its modifying effects on post-transplant CKD-MBD. Systematic analysis of fracture risk or fracture risk prevention, or of bone histomorphometry, under active vitamin D treatment is not available to date in any stage of CKD.
Nutritional Vitamin D
Data on the importance nutritional vitamin D in CKD are unfortunately limited. Traditionally, it had been considered that vitamin D supply may be inconsequential, because the key issue is calcitriol deficiency due to loss of renal function, and if this is therapeutically corrected by calcitriol (or active vitamin D analogue) replacement, no additional supplementation with vitamin D3 (or D2) is required. The latter had even been regarded as ineffective, because it was thought that substrate availability had no impact if 1-alpha-hydroxylation is blocked.
Meanwhile, paradigms shifted into two different and novel directions. First of all, data were generated that there is still some relationship between vitamin D status, calcitriol production, and PTH levels, respectively [27]. Second, autocrine or paracrine (inducible) 1α-hydroxylase activities in non-renal cells (lymphocytes, heart, bone etc.) may serve as targets and be responsible for the so-called pleiotropic effects of vitamin D [28].
Ravani et al. provided data on associations of vitamin D deficiency [low 25(OH)D levels] and impaired calcitriol availability with increased PTH serum levels in 168 CKD patients not on dialysis [27]. Their study further indicated a significant mortality risk in subjects with vitamin D deficiency. Stubbs et al. demonstrated in dialysis patients with vitamin D deficiency that high-dose vitamin D supplementation not only corrected 25(OH)D serum levels, but still also increased calcitriol levels, associated with an improved immune function of circulating monocytes [29]. However, at first glance data on high-dose nutritional vitamin D seem disappointing as an intervention to control SHPT development in CKD patients not on dialysis. Meta-analyses recently demonstrated significant rises of 25(OH)D levels under supplementation, but no changes in PTH serum concentrations [30]. No such change may however alternatively mean still some control, because a further PTH increase was prevented—therefore, these data would not essentially justify ruling out any benefit of nutritional vitamin D on SHPT progression in predialysis stages.
In advanced CKD, while observational studies quite strongly point to associations of vitamin D deficiency with impaired hard outcomes, there are no conclusive prospective data available on the relationship of vitamin D supplementation with outcomes including mortality, morbidity, fracture risk, BMD, bone biomarkers etc. In the absence of such data, the current KDIGO guideline therefore pragmatically decided to apply guidelines recommendations for the normal population to CKD patients [17]. Depending on the source of the guideline (Institute of Medicine or Endocrine Society), 25(OH)D serum levels of ≥ 20 or ≥ 30 ng/ml should thus be targeted [31, 32], and as such levels are frequently not even reached in the normal population, most CKD patients would require some kind of supplementation. On average, doses would vary between 600 and 2000 IU vitamin D3 equivalent per day.
One key question is how to address vitamin D status in the management of SHPT in CKD patients not on dialysis. As outlined above, there are hardly any reliable interventional data on the impact of nutritional vitamin D on SHPT progression. Moe et al. found a PTH lowering effect of high-dose vitamin D3 (4000 IU/day for 1 month, then 2000 IU/day) comparable to doxercalciferol in a short-term study over 3 months in CKD patients not on dialysis, but sustainability remained questionable [33]. A new player is this context may be extended-release calcifediol (ERC), which is already available for treatment in the US. ERC is an especially coated 25(OH)D preparation constantly releasing during intestinal passage over 12 h. This mode of action avoids serum peaks of 25(OH)D and pharmacodynamically seems to prevent from feedback loop interactions getting activated, i.e. catabolizing 24-hydroxylases do not get activated and 1α-hydroxylases stay active [34].
Strugnell et al. performed a pivotal placebo-controlled trial in patients in CKD stages G3a–G4 with elevated serum PTH levels demonstrating both significant increases of 25(OH)D and decreases of PTH serum concentrations by ERC treatment, with concomitant decreases in bone turnover biomarkers [35]. Concerning safety, no relevant changes in calcium and phosphate levels were observed. Of note, serum 25(OH)D levels of ≥ 50 ng/ml were needed to see substantial PTH lowering in this cohort, raising the question of how an adequate vitamin D status should become defined in CKD patients not on dialysis. Finally, another question remains: would it potentially be equally effective, if such 25(OH)D levels were reached by high-dose nutritional vitamin D administration, or does the pharmacodynamic specificity of ERC make the difference? The latter issue is currently under investigation.
Calcimimetics
The CaSR was first identified in 1993 as a G protein-coupled receptor sensitive to calcium and other extracellular cations [36]. The principle physiological function of the CaSR is in the control of extracellular fluid calcium concentration, reflected by the location of the receptor in the parathyroid glands and in the renal tubules [36, 37] where it respectively modulates PTH secretion and renal tubular calcium handling. Thus, the CaSR plays a pivotal role in the regulation of calcium homeostasis, achieving very tight control of extracellular calcium within a narrow physiological range. The receptor is expressed in many other tissues including bone, gut, and brain [38]. Unsurprisingly, activating and inactivating mutations of the CaSR may be associated with profound disturbances of calcium metabolism and mineral ion homeostasis, whereas acquired disturbances of the CaSR may be associated with progressive hyperparathyroidism in patients with falling GFR, where failure of the vitamin D-endocrine system and retention of phosphate lead to decreased extracellular calcium and compensatory hyperparathyroidism mediated via the CaSR. Phosphate further augments the drive to hyperparathyroidism by direct actions on the parathyroid cells which increase PTH synthesis and proliferative activity in the parathyroid glands [39, 40]. Of note, recent work has shown that phosphate acts directly on the CaSR, and it thus appears likely that the stimulation of the parathyroids by hyperphosphatemia is mediated via an additional direct mechanism involving the CaSR [41].
The central role of the CaSR in the pathogenesis of SHPT points to the CaSR as an attractive therapeutic target. The rapid development of allosteric modulators of the CaSR, initially NPS 568 and later AMG 073 (cinacalcet), attests to the importance of this therapeutic target [42]. Cinacalcet was the first clinically usable calcimimetic agent and has been in increasingly widespread use since 1993 [13]. Predictably its actions are to lower simultaneously PTH secretion and serum calcium concentration, an action that requires that the drug significantly shifts the normal sigmoid relationship between calcium and PTH to the left [43]. Cinacalcet has proved extremely effective with sustained responses in these patients [44], although with a target receptor so widely expressed, it is not surprising that certain unwanted off-target effects have emerged. Fortunately, these have generally been mild.
A further development in the area of CaSR modulation comes from the development of etelcalcetide, a peptide agonist of the receptor [45]. This peptide, which is administered by intravenous injection, activates the CaSR powerfully, thereby resulting in actions similar to those of cinacalcet. A critical feature of etelcalcetide is its resistance to degradation in plasma—the elimination of etelcalcetide is almost entirely renal and although the half-life in the presence of normal GFR is short, it is greatly prolonged in ESRD. This prolongation enables intermittent intravenous administration of etelcalcetide after dialysis with sustained action on the parathyroids resulting. Placebo-controlled studies using etelcalcetide have attested to its efficacy [46], and so also have comparative studies with cinacalcet where etelcalcetide was seen to be at least as effective as cinacalcet, carrying also the benefits of good tolerability (though are no better than cinacalcet) and very high levels of patient adherence reflecting the parenteral route of administration [47].
The flip side of calcimimetic drug development has been attempts to identify agents that reduce the sensitivity of the CaSR to ambient calcium concentration, thereby stimulating the release of PTH. Calcilytics are small organic molecules that act as negative allosteric modulators and, like calcimimetics, bind the transmembrane domain of the receptor [48]. The main potential therapeutic area is osteoporosis where it had been hoped that intermittent doses of a calcilytic agent would serve to mimic the effects of intermittent exogenous administration of synthetic human PTH, a therapy of proven efficacy in the treatment of osteoporosis [49, 50]. In phase II clinical studies using calcilytic agents, several have been tested and all generated rapid increases of PTH lasting from 8 or 12 h. Unfortunately, accompanying changes in the levels of bone markers were generally small, and there was no discernible effect on bone density [42]. In one study using ronacaleret for osteoporosis in postmenopausal women, despite significant changes in bone markers, comparable to those in patients treated with teriparatide, only very small changes of bone density were seen in the ronacaleret-treated patients, in contrast to those receiving alendronate or teriparatide [51]. Theoretically, calcilytics might be considered as a therapeutic option for adynamic bone disease in CKD patients, but this possibility has not been fully explored.
The pivotal role of PTH in the regulation of bone metabolism, alongside the expression of the CaSR in bone, raises important questions as to the skeletal consequences of CaSR modulating agents (calcimimetic or calcilytics). Clearly, osseous effects of calcimimetic treatment could be direct, mediated via the CaSR in bone, or indirect mediated via calcium, phosphate, PTH, vitamin D or FGF23. The possibility that the CaSR mediates anabolic input to the skeleton is supported by studies of Al-Dujaili et al. in transgenic animals null for CaSR on osteoblasts, but not parathyroid, who found that PTH exerted a reduced bone anabolic effect [52]. Díaz-Tocados et al. infused physiological doses of PTH in parathyroidectomized rats and found that the anabolic effect on bone was increased further by concomitant administration of a calcimimetic [53]. Potentially, this could be therapeutically useful by mitigating the loss of PTH-induced anabolic input in patients overtreated with active vitamin D and/or calcium.
While there is no doubt that calcimimetic agents (cinacalcet is the best evaluated) are capable of improving the metabolic profile of patients with CKD and SHPT, as well as those with primary hyperparathyroidism and autonomous hyperparathyroidism following renal transplantation, effects on bone are much less clear. Even more problematic is the matter of patient-level outcomes in relation to the skeleton, as well as in other tissues. Thus, a major focus has been on the effect of these agents on cardiovascular events, as well as parathyroid- and skeletal-related events of this type—parathyroidectomy/fracture are also very important.
Because over treatment with calcium and vitamin D compounds has been associated with the development of low-turnover (adynamic) bone disease, the possibility of a similar problem in relation to overzealous treatment with cinacalcet is relevant. In addition to the experimental studies discussed above, this has been approached by investigators looking at biochemical bone markers and also bone histology and fracture. Several small studies have been undertaken to examine this and will be described now. Malluche et al. [54] examined bone markers (bone-specific alkaline phosphatase—BSAP and N-telopeptide—NTx) in 32 dialysis patients with mild-to-moderate hyperparathyroidism. Both biochemical markers were elevated at baseline and fell in cinacalcet-treated patients while increasing further in placebo-treated patients over the one year period of observation. In the Bone Histomorphometry Assessment for Dialysis Patients with Secondary Hyperparathyroidism of End Stage Renal Disease (BONAFIDE) study, BSAP, NTx, osteocalcin, and tartrate resistant acid phosphatase (TRAP) were followed in 40 patients treated with cinacalcet [55]. The resorption markers (NTx and TRAP) decreased significantly from the elevated baseline levels, as did the bone formation marker, osteocalcin. BSAP did not change significantly.
More recently biochemical bone markers have been examined in etelcalcetide-treated patients. In a comparative study between cinacalcet and etelcalcetide, BSAP and C-terminal telopeptide both decreased following calcimimetic treatment, with effects on etelcalcetide slightly greater than those seen with cinacalcet [47]. Similar results were obtained by Shigematsu et al. with TRACP-5b levels decreasing in etelcalcetide-treated patients though with less change in BSAP—indeed, there was transient increase of BSAP followed by decrease in etelcalcetide-treated patients in the early phase after initiation [56].
Bone histology was examined by Malluche et al. in 19 cinacalcet-treated patients and compared with results from 13 receiving placebo [54]. Bone turnover was elevated in the majority at baseline. Cinacalcet treatment decreased PTH and also activation frequency, bone formation rate/bone surface, and fibrosis surface/bone surface. Three cinacalcet-treated patients developed adynamic bone disease (in two of these PTH was over suppressed to less than 100 pg/ml). These histomorphometric changes broadly correlated with the changes in BASP and NTx.
In the single-arm BONAFIDE study [55], 110 patients with PTH at least 300 pg/ml underwent a baseline biopsy and a further 77 underwent second bone biopsy after 6–12 months of cinacalcet treatment. Evidence of cinacalcet effect was seen by PTH reduction from 785 to 480 pg/ml with significant reductions of bone turnover parameters in most patients—mean rate/tissue area from 728 to 336 µm2/mm2/day, osteoblast perimeter/osteoid perimeter from 17.4 to 13.9%, and eroded perimeter/bone perimeter from 12.7 to 8.3%. No patient was defined by normal bone histology at baseline with 20 normal at 12 months. Only two patients developed adynamic bone disease, both with PTH under 150 pg/ml. Most patients at the end of the study had persisting mild hyperparathyroidism or mixed uremic osteodystrophy. Thus, when used in this way, the risk of the unintended induction of low turnover/adynamic bone disease by cinacalcet appears to be low. One can surmise that this potential benefit of PTH control using a calcimimetic, rather than a vitamin D compound, may be a CaSR mediated phenomenon [52].
The first evidence that cinacalcet might have a favorable effect on fracture rate in hemodialysis patients came from a post hoc analysis of data from four similarly designed randomized studies comprising a total of 1184 subjects [57]. Randomization to cinacalcet resulted in the anticipated biochemical responses, accompanied by substantial reduction of fracture risk (RR 0.46, 95% CI 0.22–0.95). Subsequently in the much larger Evaluation of Cinacalcet Hydrochloride Therapy to Lower Cardiovascular Events (EVOLVE) trial, fracture was part of a pre-specified secondary analysis in which the relative hazard for fracture after adjustment of baseline characteristics and multiple fractures, was less impressive at 0.83 (95% CI 0.72–0.98). In fact, in the unadjusted comparison the difference in fracture rate just failed to reach statistical significance [58]. The overall reduction of fracture rate by cinacalcet appeared to be more pronounced in older patients. To date, no evidence exists to demonstrate an effect of etelcalcetide on fracture rates in hemodialysis patients, despite data from studies in CKD rats demonstrating better preservation of bone structure and strength in animals treated with etelcalcetide [59]. Further studies will be needed to elucidate the potential of etelcalcetide in relation to this important clinical outcome.
Evocalcet is a relatively new oral calcimimetic widely used in Japan from where most of the clinical data have emerged. Evocalcet appears similarly effective to cinacalcet in respect of biochemical control in patients with SHPT, with the apparent advantage of a higher level of gastrointestinal tolerability than cinacalcet [60]. These clinical observations are consistent with earlier studies showing a favorable profile on gastric emptying in rats and the interaction with CYPs in liver microsomes [61].
Mindful of the plethora of new compounds capable of modifying the CaSR (only three of them used in clinical practice so far), this field is likely to continue its advance [42]. Perhaps the most intriguing possibilities lie in the area of organ specific agents targeting the CaSR where mitigation of unwanted side effects and/or exploitation of localized functions of the CaSR would be exciting developments.
Parathyroidectomy
Despite the advances in the medications for treating SHPT, a subset of patients with severe SHPT do not respond to PTH-lowering therapy, potentially leading to the development of high-turnover bone disease. PTx is the definitive therapy for treating such uncontrolled SHPT. This procedure drastically lowers PTH levels and simultaneously lowers serum calcium, phosphorus, and FGF23 levels [62, 63].
The effect of PTx on bone histology has been evaluated only in a few studies, probably because of the practical difficulty of performing bone biopsy before and after PTx in the same patient. These studies demonstrated that osteoclast bone resorption was markedly suppressed immediately after PTx, and this effect persisted in the long term. By contrast, osteoblast bone formation was further increased after PTx, but this effect was transient and was followed by a subsequent gradual decline [64, 65]. These findings indicate that there is an uncoupling of bone formation and bone resorption in the early postsurgical period, which corresponds to the rapid uptake of calcium and phosphate by the skeleton following PTx (a condition known as hungry bone syndrome). In accordance with the increased bone formation and mineralization following PTx, observational studies have consistently reported increased bone mineral density (BMD) following PTx [66, 67]. Of note, recent clinical studies reported the utility of BMD testing to predict fracture risk in dialysis patients [68, 69]. Thus, the improvement in BMD after PTx may have important implications in terms of fracture prevention.
As clinical fractures are not a common event even in the dialysis population, with the incidence being several-fold lower than mortality rates [70], evaluating whether PTx reduces the risk of fracture in patients with severe SHPT requires a large sample size. Until date, this question was explored only in one epidemiological study by Rudser et al. [71] using the United States Renal Database System (USRDS). This study compared incidence rates of fractures among 5,918 patients who underwent PTx with 16,328 control patients who were matched by age, race, sex, year of dialysis initiation, primary cause of kidney failure, and the dosage of intravenous vitamin D. The investigators demonstrated that PTx was associated with a lower risk for hip fracture (HR 0.68; 95% CI, 0.54–0.86) and combined fracture (hip, vertebral, distal radius, or wrist fracture; HR 0.69; 95% CI, 0.57–0.83). Although this observational study could not infer causality, their findings, in combination with the reported increase in BMD after PTx, support the possibility that PTx may reduce the risk of fracture in patients with severe SHPT [72].
The major concern with PTx is extremely low PTH levels after surgery because this condition has been linked with adynamic bone disease. However, it is still unknown whether the extremely low level of PTH, as a result of therapeutic intervention, actually contributes to increased bone fragility. One study reported that intact PTH levels less than 195 pg/ml were associated with an increased risk of hip fracture [12], but similar relationships were not observed in the much larger DOPPS analysis [11]. Importantly, patients with low PTH levels often have multiple risk factors for fracture, including aging, diabetes, malnutrition, and cardiovascular comorbidities that potentially contribute to falls [73, 74]. Thus, the associations of low PTH with elevated fracture risk reported in few previous studies could be attributed to residual confounding and may not be explained by low-turnover bone disease per se. In this regard, it is worth noting that in the USRDS study by Rudser et al. the risk reduction for fracture was pronounced among those who underwent total PTx versus subtotal PTx [71], suggesting that more aggressive PTH reduction may provide benefit in terms of bone strength. Interestingly, one bone biopsy study reported an activation of ‘minimodeling’ long after total PTx, which is characterized by enhanced de novo osteoid formation and mineral apposition without signs of previous bone resorption, suggesting that PTH is not indispensable for maintaining bone volume after PTx [65]. These observations support the potential benefit of PTx on bone metabolism and might argue against the current belief that low PTH should be avoided for maintaining bone strength. However, additional studies are needed to address this possibility.
Phosphate Binders
While management of hyperphosphatemia is mainly intended to prevent vascular calcification and reduce the risk of cardiovascular disease, abnormal phosphate metabolism has been historically linked to the development of SHPT and high-turnover bone disease [75]. As such, control of PTH levels and management of bone metabolism have long been the therapeutic objective of phosphate binder therapy.
In the 1970s and 1980s, aluminum-based binders were the mainstay of therapy for hyperphosphatemia. They are highly effective, but their use was largely abandoned because of systemic aluminum toxicity, manifested as encephalopathy, anemia, and bone disease characterized by mineralization defect and suppressed bone turnover [76, 77].
As an alternative to aluminum salts, calcium-based binders have been used for the treatment of hyperphosphatemia. They are effective and inexpensive, but their administration results in elevations in serum calcium levels, especially in combinations with active vitamin D. The elevated serum calcium can cause suppression of PTH, which, theoretically, could reduce bone turnover [75]. If so, calcium-based binders might be used to help improve high-turnover bone disease. However, no placebo-controlled trials have evaluated the effect of calcium-based binders on bone histology. In a randomized trial comparing sevelamer hydrochloride and calcium carbonate, there were no changes from baseline in bone histomorphometric parameters in patients receiving calcium carbonate [78]. However, almost all of these patients have already been treated with calcium carbonate at study enrollment, which limited the ability to examine the effect of starting calcium carbonate on bone histology. Several studies have also shown increased BMD with calcium-based binders compared to placebo [79, 80], which might suggest improved bone strength. However, these effects could be achieved at the expense of accelerated vascular calcification, so the current KDIGO guideline suggests restricting the dose of calcium-based binders regardless of underlying bone disease or the presence of vascular calcification [17].
Sevelamer hydrochloride is a calcium-free, resin-based phosphate binder. Since this binder can cause metabolic acidosis, sevelamer carbonate has become available in several countries. The major characteristic of sevelamer is that it does not cause calcium overload. Compared with calcium-based binders, the use of sevelamer has been associated with lower serum calcium levels and higher levels of PTH and bone turnover markers [81]. In line with this, previous studies have reported that sevelamer-treated patients showed increased bone formation rate compared with those receiving calcium-based binders [78, 82]. These results may suggest that sevelamer is preferable to calcium-based binders for patients with adynamic bone disease, but additional studies are required to address this possibility.
Lanthanum carbonate is another calcium-free binder that effectively lowers serum phosphorus levels. In the same as sevelamer, lanthanum treatment has been associated with lower serum calcium levels, higher PTH levels, and a tendency towards higher bone turnover compared with calcium-based binders [83,84,85]. Thus, it could be assumed, but not proved, that lanthanum is preferable for patients with low bone turnover. In light of the experience with aluminum-induced bone disease, there has been a concern regarding the long-term safety of lanthanum, particularly with regard to bone toxicity. Indeed, studies reported a progressive increase in the concentrations of lanthanum in bone up to three years [83,84,85,86]. However, these concentrations were still very low, and no patients have developed aluminum-like effects on bone so far in previous studies [83,84,85,86]. Furthermore, in a recent analysis of post-marketing observational study, lanthanum prescription was not associated with increased risk of fracture during the 5 years of follow-up [87]. These data suggest that lanthanum does not accumulate to clinically relevant levels in bone, but additional studies would be required to fully confirm the safety of this binder.
Conclusions
During the past decade, the introduction of calcimimetics, the optimized use of nutritional and active vitamin D, and the accumulated experience with PTx have expanded the treatment options for SHPT in patients with CKD. Our current knowledge on the effects of these interventions on bone disorders are summarized in Table 1. Studies supported that these advances could translate into improvement of renal bone disease and fracture prevention, as well as decreasing the risk of cardiovascular events and mortality. Nonetheless, patients with advanced CKD, especially those receiving dialysis, still have unacceptably high risk of fracture, which adversely impacts morbidity and mortality. Clearly, additional studies are needed to establish the optimal treatment of CKD-MBD for preventing fractures and other adverse clinical outcomes.
References
Isakova T, Wahl P, Vargas GS et al (2011) Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int 79:1370–1378
Shigematsu T, Kazama JJ, Yamashita T et al (2004) Possible involvement of circulating fibroblast growth factor 23 in the development of secondary hyperparathyroidism associated with renal insufficiency. Am J Kidney Dis 44:250–256
Gutierrez O, Isakova T, Rhee E et al (2005) Fibroblast growth factor-23 mitigates hyperphosphatemia but accentuates calcitriol deficiency in chronic kidney disease. J Am Soc Nephrol 16:2205–2215
Fukuda N, Tanaka H, Tominaga Y et al (1993) Decreased 1,25-dihydroxyvitamin D3 receptor density is associated with a more severe form of parathyroid hyperplasia in chronic uremic patients. J Clin Invest 92:1436–1443
Kifor O, Moore FD Jr, Wang P et al (1996) Reduced immunostaining for the extracellular Ca2þ-sensing receptor in primary and uremic secondary hyperparathyroidism. J Clin Endocrinol Metab 81:1598–1606
Komaba H, Goto S, Fujii H et al (2010) Depressed expression of Klotho and FGF receptor 1 in hyperplastic parathyroid glands from uremic patients. Kidney Int 77:232–238
Komaba H, Fukagawa M (2012) The role of FGF23 in CKD—with or without Klotho. Nat Rev Nephrol 8:484–490
Moe S, Drueke T, Cunningham J et al (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int 69:1945–1953
Sherrard DJ, Hercz G, Pei Y et al (1993) The spectrum of bone disease in end-stage renal failure: an evolving disorder. Kidney Int 43:436–442
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl 113:S1–S130
Jadoul M, Albert JM, Akiba T et al (2006) Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int 70:1358–1366
Coco M, Rush H (2000) Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36:1115–1121
Block GA, Martin KJ, de Francisco AL et al (2004) Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med 350:1516–1525
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Wolf M (2012) Update on fibroblast growth factor 23 in chronic kidney disease. Kidney Int 82:737–747
Wolisi GO, Moe SM (2005) The role of vitamin D in vascular calcification in chronic kidney disease. Semin Dial 18:307–314
Kidney Disease: Improving Global Outcomes (KDIGO) CKD–MBD Update Work Group (2017) KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl 7:1–59
Thadhani R, Appelbaum E, Pritchett Y et al (2012) Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. JAMA 307:674–684
Wang AY, Fang F, Chan J et al (2014) Effect of paricalcitol on left ventricular mass and function in CKD: the OPERA trial. J Am Soc Nephrol 25:175–186
Xiang W, Kong J, Chen S et al (2005) Cardiac hypertrophy in vitamin D receptor knockout mice: role of the systemic and cardiac renin-angiotensin systems. Am J Physiol Endocrinol Metab 288:E125–E132
Bodyak N, Ayus JC, Achinger S et al (2007) Activated vitamin D attenuates left ventricular abnormalities induced by dietary sodium in Dahl salt-sensitive animals. Proc Natl Acad Sci USA 104:16810–16815
Baker LR, Muir JW, Sharman VL et al (1986) Controlled trial of calcitriol in hemodialysis patients. Clin Nephrol 26:185–191
London GM, Marty C, Marchais SJ et al (2004) Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15:1943–1951
Brandenburg VM, Kramann R, Rothe H et al (2017) Calcific uraemic arteriolopathy (calciphylaxis): data from a large nationwide registry. Nephrol Dial Transplant 32:126–132
Fukagawa M, Yokoyama K, Koiwa F et al (2013) Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial 17:247–288
Torres A, Garcia S, Gomez A et al (2004) Treatment with intermittent calcitriol and calcium reduces bone loss after renal transplantation. Kidney Int 65:705–712
Ravani P, Malberti F, Tripepi G et al (2009) Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int 75:88–95
Biggar PH, Liangos O, Fey H et al (2011) Vitamin D, chronic kidney disease and survival: a pluripotent hormone or just another bone drug? Pediatr Nephrol 26:7–18
Stubbs JR, Idiculla A, Slusser J et al (2010) Cholecalciferol supplementation alters calcitriol-responsive monocyte proteins and decreases inflammatory cytokines in ESRD. J Am Soc Nephrol 21:353–361
Agarwal R, Georgianos PI (2016) Con: Nutritional vitamin D replacement in chronic kidney disease and end-stage renal disease. Nephrol Dial Transplant 31:706–713
Ross AC, Manson JE, Abrams SA et al (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–58
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Moe SM, Saifullah A, LaClair RE et al (2010) A randomized trial of cholecalciferol versus doxercalciferol for lowering parathyroid hormone in chronic kidney disease. Clin J Am Soc Nephrol 5:299–306
Sprague SM, Strugnell SA, Bishop CW (2017) Extended-release calcifediol for secondary hyperparathyroidism in stage 3–4 chronic kidney disease. Expert Rev Endocrinol Metab 12:289–301
Strugnell SA, Sprague SM, Ashfaq A et al (2019) Rationale for raising current clinical practice guideline target for serum 25-hydroxyvitamin D in chronic kidney disease. Am J Nephrol 49:284–293
Brown EM, Gamba G, Riccardi D et al (1993) Cloning and characterization of an extracellular Ca(2+)-sensing receptor from bovine parathyroid. Nature 366:575–580
Aida K, Koishi S, Tawata M et al (1995) Molecular cloning of a putative Ca(2+)-sensing receptor cDNA from human kidney. Biochem Biophys Res Commun 214:524–529
Alfadda I, Saleh AMA, Houillier P et al (2014) Calcium-sensing receptor 20 years later. Am J Physiol Cell Physiol 307:C221–C231
Nielsen PK, Feldt-Rasmussen U, Olgaard K (1996) A direct effect in vitro of phosphate on PTH release from bovine parathyroid tissue slices but not from dispersed parathyroid cells. Nephrol Dial Transplant 11:1762–1768
Almaden Y, Canalejo A, Hernandez A et al (1996) Direct effect of phosphorus on PTH secretion from whole rat parathyroid glands in vitro. J Bone Miner Res 11:970–976
Centeno PP, Herberger A, Mun HC et al (2019) Phosphate acts directly on the calcium-sensing receptor to stimulate parathyroid hormone secretion. Nature Commun 10:4693
Nemeth EF, Goodman WG (2016) Calcimimetic and calcilytic drugs: feats, flops, and futures. Calcif Tissue Int 98:341–358
Valle C, Rodriguez M, Santamaría R et al (2008) Cinacalcet reduces the set point of the PTH-calcium curve. J Am Soc Nephrol 19:2430–2436
Moe SM, Cunningham J, Bommer J et al (2005) Long-term treatment of secondary hyperparathyroidism with the calcimimetic cinacalcet HCl. Nephrol Dial Transplant 20:2186–2193
Walter S, Baruch A, Dong J et al (2013) Pharmacology of AMG 416 (Velcalcetide), a novel peptide agonist of the calcium-sensing receptor, for the treatment of secondary hyperparathyroidism in hemodialysis patients. J Pharmacol Exp Ther 346:229–240
Block GA, Bushinsky DA, Cunningham J et al (2017) Effect of etelcalcetide vs placebo on serum parathyroid hormone in patients receiving hemodialysis with secondary hyperparathyroidism: two randomized clinical trials. JAMA 317:146–155
Block GA, Bushinsky DA, Cheng S et al (2017) Effect of etelcalcetide vs cinacalcet on serum parathyroid hormone in patients receiving hemodialysis with secondary hyperparathyroidism: a randomized clinical trial. JAMA 317:156–164
Gowen M, Stroup GB, Dodds RA et al (2000) Antagonizing the parathyroid calcium receptor stimulates parathyroid hormone secretion and bone formation in osteopenic rats. J Clin Invest 105:1595–1604
Silve BC, Bilezikian JP (2015) Parathyroid hormone: anabolic and catabolic actions on the skeleton. Curr Opin Pharmacol 22:41–50
Riccardi D (2012) Antagonizing the calcium-sensing receptor: towards new bone anabolics? Curr Mol Pharmacol 5:182–188
Fitzpatrick LA, Dabrowski CE, Cicconetti G et al (2011) The effects of ronacaleret, a calcium-sensing receptor antagonist, on bone mineral density and biochemical markers of bone turnover in postmenopausal women with low bone mineral density. J Clin Endocrinol Metab 96:2441–2449
Al-Dujaili SA, Koh AJ, Dang M et al (2016) Calcium sensing receptor function supports osteoblast survival and acts as a co-factor in PTH anabolic actions in bone. J Cell Biochem 117:1556–1567
Díaz-Tocados JM, Rodríguez-Ortiz ME, Almadén Y et al (2019) Calcimimetics maintain bone turnover in uremic rats despite the concomitant decrease in parathyroid hormone concentration. Kidney Int 95:1064–1078
Malluche HH, Monier-Faugere MC, Wang G et al (2008) An assessment of cinacalcet HCl effects on bone histology in dialysis patients with secondary hyperparathyroidism. Clin Nephrol 69:269–278
Behets GJ, Spasovski G, Sterling LR et al (2015) Bone histomorphometry before and after long-term treatment with cinacalcet in dialysis patients with secondary hyperparathyroidism. Kidney Int 87:846–856
Shigematsu T, Fukagawa M, Yokoyama K et al (2018) Long-term effects of etelcalcetide as intravenous calcimimetic therapy in hemodialysis patients with secondary hyperparathyroidism. Clin Exp Nephrol 22:426–436
Cunningham J, Danese M, Olson K et al (2005) Effects of the calcimimetic cinacalcet HCl on cardiovascular disease, fracture, and health-related quality of life in secondary hyperparathyroidism. Kidney Int 68:1793–1800
Moe SM, Abdalla S, Chertow GM et al (2015) Effects of cinacalcet on fracture events in patients receiving hemodialysis: the EVOLVE trial. J Am Soc Nephrol 26:1466–1475
Li X, Yu L, Asuncion F et al (2017) Etelcalcetide (AMG 416), a peptide agonist of the calcium-sensing receptor, preserved cortical bone structure and bone strength in subtotal nephrectomized rats with established secondary hyperparathyroidism. Bone 105:163–172
Fukagawa M, Shimazaki R, Akizawa T (2018) Head-to-head comparison of the new calcimimetic agent evocalcet with cinacalcet in Japanese hemodialysis patients with secondary hyperparathyroidism. Kidney Int 94:818–825
Kawata T, Tokunaga S, Murai M et al (2018) A novel calcimimetic agent, evocalcet (MT-4580/KHK7580), suppresses the parathyroid cell function with little effect on the gastrointestinal tract or CYP isozymes in vivo and in vitro. PLoS ONE 13:e0195316
Wetmore JB, Liu J, Do TP et al (2016) Changes in secondary hyperparathyroidism-related biochemical parameters and medication use following parathyroidectomy. Nephrol Dial Transplant 31:103–111
Takahashi H, Komaba H, Takahashi Y et al (2014) Impact of parathyroidectomy on serum FGF23 and soluble Klotho in hemodialysis patients with severe secondary hyperparathyroidism. J Clin Endocrinol Metab 99:E652–E658
Yajima A, Ogawa Y, Takahashi HE et al (2003) Changes of bone remodeling immediately after parathyroidectomy for secondary hyperparathyroidism. Am J Kidney Dis 42:729–738
Yajima A, Inaba M, Tominaga Y et al (2008) Bone formation by minimodeling is more active than remodeling after parathyroidectomy. Kidney Int 74:775–781
Abdelhadi M, Nordenström J (1998) Bone mineral recovery after parathyroidectomy in patients with primary and renal hyperparathyroidism. J Clin Endocrinol Metab 83:3845–3851
Chou FF, Chen JB, Lee CH et al (2001) Parathyroidectomy can improve bone mineral density in patients with symptomatic secondary hyperparathyroidism. Arch Surg 136:1064–1068
Iimori S, Mori Y, Akita W et al (2012) Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients–a single-center cohort study. Nephrol Dial Transplant 27:345–351
Nakagawa Y, Komaba H, Hamano N et al (2020) Metacarpal bone mineral density by radiographic absorptiometry predicts fracture risk in patients undergoing maintenance hemodialysis. Kidney Int 98:970–978
Tentori F, McCullough K, Kilpatrick RD et al (2014) High rates of death and hospitalization follow bone fracture among hemodialysis patients. Kidney Int 85:166–173
Rudser KD, de Boer IH, Dooley A et al (2007) Fracture risk after parathyroidectomy among chronic hemodialysis patients. J Am Soc Nephrol 18:2401–2407
Komaba H, Nakamura M, Fukagawa M (2017) Resurgence of parathyroidectomy: evidence and outcomes. Curr Opin Nephrol Hypertens 26:243–249
Floege J, Kim J, Ireland E et al (2011) Serum iPTH, calcium and phosphate, and the risk of mortality in a European haemodialysis population. Nephrol Dial Transplant 26:1948–1955
Komaba H, Taniguchi M, Wada A et al (2015) Parathyroidectomy and survival among Japanese hemodialysis patients with secondary hyperparathyroidism. Kidney Int 88:350–359
Drüeke TB, Massy ZA (2016) Changing bone patterns with progression of chronic kidney disease. Kidney Int 89:289–302
Alfrey AC, LeGendre GR, Kaehny WD (1976) The dialysis encephalopathy syndrome. Possible aluminum intoxication. N Engl J Med 294:184–188
Wills MR, Savory J (1983) Aluminium poisoning: dialysis encephalopathy, osteomalacia, and anaemia. Lancet 2:29–34
Ferreira A, Frazão JM, Monier-Faugere MC et al (2008) Effects of sevelamer hydrochloride and calcium carbonate on renal osteodystrophy in hemodialysis patients. J Am Soc Nephrol 19:405–412
Rudnicki M, Hyldstrup L, Petersen LJ et al (1994) Effect of oral calcium on noninvasive indices of bone formation and bone mass in hemodialysis patients: a randomized double-blind placebo-controlled study. Miner Electrolyte Metab 20:130–134
Block GA, Wheeler DC, Persky MS et al (2012) Effects of phosphate binders in moderate CKD. J Am Soc Nephrol 23:1407–1415
Qunibi W, Moustafa M, Muenz LR et al (2008) A 1-year randomized trial of calcium acetate versus sevelamer on progression of coronary artery calcification in hemodialysis patients with comparable lipid control: the Calcium Acetate Renagel Evaluation-2 (CARE-2) study. Am J Kidney Dis 51:952–965
Barreto DV, Barreto Fde C, de Carvalho AB et al (2008) Phosphate binder impact on bone remodeling and coronary calcification: results from the BRiC study. Nephron Clin Pract 110:c273–c283
D’Haese PC, Spasovski GB, Sikole A et al (2003) A multicenter study on the effects of lanthanum carbonate (Fosrenol) and calcium carbonate on renal bone disease in dialysis patients. Kidney Int Suppl 85:S73–S78
Malluche HH, Siami GA, Swanepoel C et al (2008) Improvements in renal osteodystrophy in patients treated with lanthanum carbonate for two years. Clin Nephrol 70:284–295
Spasovski GB, Sikole A, Gelev S et al (2006) Evolution of bone and plasma concentration of lanthanum in dialysis patients before, during 1 year of treatment with lanthanum carbonate and after 2 years of follow-up. Nephrol Dial Transplant 21:2217–2224
Shigematsu T, Tokumoto A, Nakaoka A et al (2011) Effect of lanthanum carbonate treatment on bone in Japanese dialysis patients with hyperphosphatemia. Ther Apher Dial 15:76–184
Hutchison A, Whelton A, Thadhani R et al (2018) Long-term mortality and bone safety in patients with end-stage renal disease receiving lanthanum carbonate. Nephron 140:265–274
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Hirotaka Komaba has received honoraria, consulting fees, and/or grant support from Bayer Yakuhin, Chugai Pharmaceutical, Japan Tobacco, Kyowa Kirin, Novartis, and Ono Pharmaceutical. Markus Ketteler has received honoraria for consulting and lecture fees from Amgen, Bayer, Kyowa Kirin, Medice, Ono Pharmaceutical, Sanofi, and Vifor Pharma. John Cunningham has receive honoraria, consulting fees, and/or grant support from Vifor Pharma, Amgen, Merck, and Opko Pharma. Masafumi Fukagawa has received honoraria, consulting fees, and/or grant support from Bayer Yakuhin, Fresenius Kabi, Kissei Pharmaceutical, Kyowa Kirin, Ono Pharmaceutical, and Torii Pharmaceutical.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Komaba, H., Ketteler, M., Cunningham, J. et al. Old and New Drugs for the Management of Bone Disorders in CKD. Calcif Tissue Int 108, 486–495 (2021). https://doi.org/10.1007/s00223-020-00788-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00788-y